Abstract
Erythropoietin (Epo) is the central regulator of red blood cell production and acts primarily by inducing proliferation and differentiation of erythroid progenitor cells. Because a sufficient supply of iron is a prerequisite for erythroid proliferation and hemoglobin synthesis, we have investigated whether Epo can regulate cellular iron metabolism. We present here a novel biologic function of Epo, namely as a potential modulator of cellular iron homeostasis. We show that, in human (K562) and murine erythroleukemic cells (MEL), Epo enhances the binding affinity of iron-regulatory protein (IRP)-1, the central regulator of cellular iron metabolism, to specific RNA stem-loop structures, known as iron-responsive elements (IREs). Activation of IRP-1 by Epo is associated with a marked increase in transferrin receptor (trf-rec) mRNA levels in K562 and MEL, enhanced cell surface expression of trf-recs, and increased uptake of iron into cells. These findings are in agreement with the well-established mechanism whereby high-affinity binding of IRPs to IREs stabilizes trf-rec mRNA by protecting it from degradation by a specific RNase. The effects of Epo on IRE-binding of IRPs were not observed in human myelomonocytic cells (THP-1), which indicates that this response to Epo is not a general mechanism observed in all cells but is likely to be erythroid-specific. Our results provide evidence for a direct functional connection between Epo biology and iron metabolism by which Epo increases iron uptake into erythroid progenitor cells via posttranscriptional induction of trf-rec expression. Our data suggest that sequential administration of Epo and iron might improve the response to Epo therapy in some anemias.
ERYTHROPOIETIN (Epo) is a 30-kD glycoprotein that is primarily produced in the kidney and to a lesser extent in liver cells in response to reduced oxygen tension. Epo then enhances red blood cell mass by stimulating proliferation and differentiation of relatively mature red blood progenitor cells, such as colony-forming units (for review see Krantz,1 Jelkmann,2 and Spivak3 ). The effects of Epo on these cells are transduced by a specific cell surface receptor, the Epo receptor.4 Besides ongoing erythropoiesis, an adequate supply of iron is a prerequisite for achieving a normal oxygen supply, because iron is a central component of heme and essential for oxygen binding by hemoglobin. However, little information is available as to whether Epo, besides promoting erythropoiesis, may also affect iron metabolism, because tight regulation of both mechanisms is a prerequisite for achieving optimal oxygen transport capacity.1-3,5 Maintenance of cellular iron homeostasis is largely exerted posttanscriptionally by the interaction of RNA stem loop structures, termed iron-responsive elements (IREs), with specific cytoplasmic proteins, known as iron-regulatory protein (IRP)-1 and IRP-2. IRP-1 is a bifunctional protein that can act either as a cytoplasmic aconitase or as an IRE-binding protein.6-8 Conversion of IRP-1 to its IRE-binding form occurs during cellular iron deprivation, during oxidative stress, and in the presence of nitric oxide (NO). This is probably due to removal of the central iron-sulfur cluster of the protein, thus causing allosteric changes in protein conformation.9-13 Under these conditions, IRPs bind with high affinity to IREs present at the 5′-untranslated regions of the mRNAs for H-and L-chain ferritin and erythroid-5-aminolevulinic acid synthase (e-ALAS), thus causing repression of translation of these proteins.14-17 In contrast, IRP binding to IREs present within the 3′-untranslated region of transferrin receptor (trf-rec) mRNA enhances the stability of this mRNA by protecting it from digestion by an as yet unidentified RNase, leading to enhanced trf-rec expression and cellular iron uptake.18-20 On the other hand, increased supply of intracellular metabolically active iron reconstitutes aconitase activity of IRP-1 and degrades IRP-2, thus fully obliterating their IRE-binding function. The suppressive effect of IRPs on ferritin and e-ALAS translation and the enhanced trf-rec mRNA stability are then reversed, causing iron storage and consumption while iron uptake via trf-rec is reduced.6-8
In this report, we show a new regulatory pathway by which Epo causes an increase in IRE-binding activity of IRP-1 in human (K562) and murine erythroleukemic cells (MEL), but not in human myelomonocytic cells (THP-1). We show that this Epo-induced increase of IRE-binding activity results in an increase of trf-rec mRNA levels, cell surface expression of the protein, and subsequent iron uptake into these cells.
MATERIALS AND METHODS
Cell culture techniques.THP-1 and K562 cells were grown in RPMI 1640 medium supplemented 10% heat-inactivated fetal calf serum (FCS), 100 U/mL penicillin, and 0.1 mg/mL streptomycin at 37°C in humidified air containing 5% CO2. MEL cells were maintained in minimum Eagle's medium (MEM) with supplements as detailed above. Cells were seeded at a density of 5 × 105/mL medium and 50 μmol/L ferric nitrate nonahydrate, 100 μmol/L desferrioxamine (both from Sigma, Munich, Germany), 0.5 U/mL of murine recombinant erythropoietin (Boehringer Mannheim, Mannheim, Germany), varying concentrations of human recombinant erythropoietin (CILAG, Schaffhausen, Switzerland), or 1.5% dimethylsulphoxide (DMSO) were added. After up to 24 hours of incubation at 37°C, cells were harvested, washed twice with phosphate-buffered saline, and subjected to further procedures as indicated below. Induction of differentiation by DMSO in MEL cells was tested by scoring the percentage of hemoglobin-producing cells after staining with benzidine. After a incubation period of 96 hours, more than 90% of cells were positively stained.
Generation of a 32P-labeled IRE probe and gel retardation assay.Cells were grown in the appropriate medium plus additives and treated as described above. After harvesting and washing, detergent cell extracts were prepared as described previously.21 A 32P-labeled IRE probe was generated as described by Milligan et al22 using T7 RNA polymerase and purified by gel electrophoresis (15% of 20:1 acrylamide/bisacrylamide; 6 mol/L urea), followed by probe elution, phenol/chloroform extraction, and ethanol precipitation. The DNA template had the sequence 5′-GGGATCCGTC CAAGCACTGT TGAAGCAGGA TCCCTATAGT GAGTCGTATT A-3′.
Approximately 15,000 cpm of this transcript was incubated with 10 to 20 μg of protein of each cellular extract at room temperature. After 20 minutes, heparin (final concentration, 3 mg/mL) was added for 10 minutes and analysis of RNA/protein complexes was performed by nondenaturating gel electrophoresis and subsequent autoradiography as described.9 Autoradiographs were densitometrically scanned using the Bio-Profil system for image analysis (Vilber Lourmat, Marne La Vallée, France).
RNA extraction and Northern blot analysis.Cells were stimulated for up to 24 hours as described above. Preparation of total RNA and Northern hybridization were then performed as detailed elsewhere.23 Briefly, RNA was prepared by the acid guanidinium thiocyanate-phenol-chloroform extraction.24 Ten micrograms of total RNA was separated on 1% agarose/2.2 mol/L formaldehyde gels, and RNA was blotted on to Duralon-UV membranes (Stratagene, La Jolla, CA). After UV cross-linking and prehybridization at 65°C, blots were hybridized overnight in 3× SSC, 0.1% sodium dodecyl sulfate, 0.1% sodium pyrophosphate, 10% dextran sulfate, 10× Denhardt's solution (0.2% Ficoll 400, 0.2% polyvinylpyrrolidone, 0.2% bovine serum albumin), and 1 mg/mL of denatured salmon sperm DNA. After washing, filters were exposed for up to 4 days to XRP-5 x-ray films (Kodak, X-OMAT RP; Sigma) with intensifying screens at −80°C. Human transferrin receptor cDNA was kindly provided by Dr M.W. Hentze (EMBL, Heidelberg, Germany).25 For Northern hybridization, the 800-bp Acc I insert was used. For hybridization with murine trf-rec cDNA (in pUC 9), a 2.2-kb fragment was used. Hybridization with the rat cDNA of the housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH; in PBR322; 1.4-kb Pst I/Pst I insert) and with chicken β-actin cDNA (in pBR322; 1.9-kb HindIII/HindIII insert) were used as a control. Probes were labeled with [α-32P]dCTP (DuPont New England Nuclear, Boston, MA) using the oligoprimer procedure.26
Transferrin binding studies.These investigations were performed essentially as described elsewhere.27 Briefly, cells were incubated for 24 hours in serum-free RPMI containing human serum albumin and 50 μg/mL of transferrin (30% iron saturated) and desferrioxamine (100 μmol/L), Epo (5 or 50 U/mL), or no further additives. Cells were then harvested and washed twice and 5 × 106 cells were incubated with 2 μg of 125I-transferrin on ice for 30 minutes in 100 μL of phosphate-buffered saline containing 1 mg/mL bovine serum albumin (Sigma). After rapid separation of cells from the supernatant and five consecutive washing steps, the cell-associated 125I activity was determined. In some experiments, cells were incubated with varying amounts of 125I-transferrin, and the number and affinity of transferrin binding sites was determined by the Scatchard method as described,28 after correction for nonspecific binding in the presence of a 200-fold excess of unlabeled transferrin.
Iron uptake studies.Cells were incubated for 24 hours with the appropriate additives as described for transferrin binding and then incubated with 59 Fe-labeled transferrin for 2 hours as described.27 Radioactivity in cells and supernatants was determined, and uptake was expressed as nanograms of Fe taken up per 106 cells per hour.
Protein determination.Protein concentration of cell lysates was estimated according to Bradford,29 using the protein dye reagent from BioRad (Richmond, CA) and bovine serum albumin as a standard.
Statistical analysis.Calculation of statistical significance was performed using the Student's t-test. Only P values less than .05 were considered significant.
RESULTS
Epo stimulates IRE binding of IRP.To investigate a possible effect of Epo on intracellular iron regulation, we first explored IRE-binding activity of IRP in human erythroleukemic (K562) and myelomonocytic cells (THP-1). Figures 1 and 2 show the results of a gel retardation assay with extracts prepared from untreated cells (C), iron-perturbed cells, and cell treated with Epo (50 U/mL). In untreated K562, only 1 RNA/protein complex is found, because IRP-1 and IRP-2 cannot be distinguished in extracts of these cells, at least by this method. Treatment of K562 cells with iron caused reduced IRE-binding activity as compared with control cells, whereas the addition of the iron chelator desferrioxamine led to the induction of IRE-binding activity of IRP, which is in accordance with previous data.10,12 21 Treatment of K562 cells with 50 U/mL Epo for 24 hours strongly induced IRE-binding activity to levels equal to or exceeding those of desferrioxamine treatment (Fig 1).
Activation of IRE-binding activity of IRP by Epo in K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), 50 U/mL human recombinant Epo (Epo), or 1.5% DMSO or remained untreated (control [C]). Fifteen micrograms of detergent cell extracts was assayed for IRE-binding activity of IRP by means of gel shift assay in the absence (upper panel) or presence of 2% 2-mercaptoethanol. After fixation, gels were exposed for 6 to 48 hours to x-ray films. The IRE/IRP complex and the nonbound IRE-probe (free probe) are shown in the upper panel, whereas in the lower panel only RNA-protein complexes are pictured. The results of one of seven similar experiments are shown.
Activation of IRE-binding activity of IRP by Epo in K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), 50 U/mL human recombinant Epo (Epo), or 1.5% DMSO or remained untreated (control [C]). Fifteen micrograms of detergent cell extracts was assayed for IRE-binding activity of IRP by means of gel shift assay in the absence (upper panel) or presence of 2% 2-mercaptoethanol. After fixation, gels were exposed for 6 to 48 hours to x-ray films. The IRE/IRP complex and the nonbound IRE-probe (free probe) are shown in the upper panel, whereas in the lower panel only RNA-protein complexes are pictured. The results of one of seven similar experiments are shown.
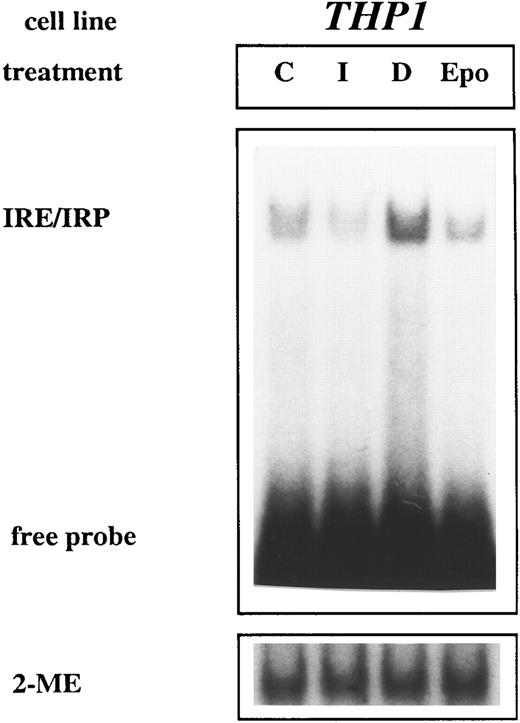
IRE/IRP interaction is not modulated by Epo in THP-1 cells. THP-1 cells were treated with various additives, and gel retardation assay was performed exactly as described in the legend to Fig 1. The results of one of five representative experiments are shown.
IRE/IRP interaction is not modulated by Epo in THP-1 cells. THP-1 cells were treated with various additives, and gel retardation assay was performed exactly as described in the legend to Fig 1. The results of one of five representative experiments are shown.
In contrast, supplementation with DMSO (1.5%) for 24 hours did not significantly alter IRE-binding activity as compared with untreated control cells (Fig 1).
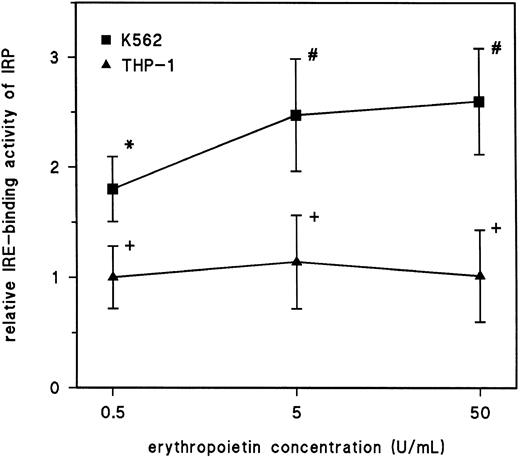
In THP-1 cells, exposure to Epo (50 U/mL) did not significantly alter the IRE-binding activity of IRPs in comparison to untreated cells, although changes in the IRP affinity by iron perturbation were the same as expected from previous investigations, ie, activation of IRP activity by withdrawal of iron upon addition of the iron chelator desferrioxamine and deactivation of IRP binding upon supplementation of iron (Fig 2). The Epo-induced high-affinity binding of IRP to IRE in human erythroleukemic cells (K562) showed a dose-response relationship with maximum effects between 5 and 50 U/mL. Densitometric scanning showed that these conditions caused an up to threefold increase in high-affinity binding of IRP to the radiolabeled IRE-probe in the gel retardation assays in comparison to untreated control cells (P < .01; Fig 3).
Dose-response curve of IRE-binding activity of IRP upon treatment with Epo. THP-1 or K562 cells were treated with increasing concentrations of human recombinant Epo (Epo) for 24 hours. After this treatment, detergent cell extracts were prepared and RNA-protein interaction was assayed by gel retardation assay as described in the Materials and Methods. The IRE/IRP complexes were then densitometrically quantified and related to the amount of RNA-protein interaction in untreated cells (control), which was set at 1 (ie, 100%). The results are plotted as means ± SD for four (K562) or three (THP-1) independent experiments. The calculation of statistical differences from the control was performed using the Student's t-test. #P < .01; *P < .05; +P < .05, not significant.
Dose-response curve of IRE-binding activity of IRP upon treatment with Epo. THP-1 or K562 cells were treated with increasing concentrations of human recombinant Epo (Epo) for 24 hours. After this treatment, detergent cell extracts were prepared and RNA-protein interaction was assayed by gel retardation assay as described in the Materials and Methods. The IRE/IRP complexes were then densitometrically quantified and related to the amount of RNA-protein interaction in untreated cells (control), which was set at 1 (ie, 100%). The results are plotted as means ± SD for four (K562) or three (THP-1) independent experiments. The calculation of statistical differences from the control was performed using the Student's t-test. #P < .01; *P < .05; +P < .05, not significant.
To see whether Epo-induced changes of IRP activity are specific for K562 cells or apply also to other erythroid cells, we investigated MEL cells. As can be seen from Fig 4, iron and desferrioxamine treatment cause the same regulatory changes of IRP activity as observed in K562 and THP-1 cells. Moreover, in desferrioxamine-treated cells, 2 RNA/protein complexes were found corresponding to murine IRP-1 (upper complex) and IRP-2 (lower complex), although the amount of IRP-2 was extremely low. Treatment of MEL cells with murine recombinant erythropoietin for 24 hours clearly increased IRP-1 activity as compared with untreated control cells (Fig 4, compare lanes 1 and 9). Interestingly, IRE-binding by IRP-2 appeared not be affected by Epo treatment in the same way as observed in response to desferrioxamine supplementation (Fig 4, compare lanes 1, 3, and 9), although caution must be taken in account that, in our experimental approach, IRP-2 expression was hardly detectable. To further characterize the induction mechanism of IRPs by Epo, time course experiments were performed. As evident from Fig 4, an optimal concentration of murine Epo (0.5 U/mL) requires approximately 4 hours to stimulate IRP-1 and 12 to 24 hours to reach maximum induction (Fig 4). Moreover, treatment of MEL cells with DMSO (1.5%) for 24 hours, a procedure that induces differentation in this cell line, did not cause obvious alterations in IRE-binding activity by IRPs as observed in untreated control cells (Fig 4, compare first and last lane).
Induction kinetics of IRPs by Epo in MEL cells. Cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), with 100 μmol/L desferrioxamine (D), and, for the indicated times, with murine recombinant Epo (0.5 U/mL) or remained untreated (control [C]). Gel retardation assays were performed exactly as described in the legend to Fig 1. The results of one of three representative experiments are shown.
Induction kinetics of IRPs by Epo in MEL cells. Cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), with 100 μmol/L desferrioxamine (D), and, for the indicated times, with murine recombinant Epo (0.5 U/mL) or remained untreated (control [C]). Gel retardation assays were performed exactly as described in the legend to Fig 1. The results of one of three representative experiments are shown.
As with iron regulation,21 Epo-mediated responses in all cell lines appear to occur posttranslationally, because IRE-binding activity can be fully activated by treatment of extracts with 2% 2-mercaptoethanol (Figs 1, 2, and 4, lower panels).
Increase in trf-rec mRNA in response to Epo.To investigate whether Epo-induced activation of IRE-binding activity of IRP in human erythroleukemic cells results in similar alterations to trf-rec mRNA concentrations, as shown previously for cellular iron starvation, we next performed Northern blots for trf-rec mRNA. As shown in Fig 5, treatment of K562 cells with desferrioxamine for 24 hours caused an increase in cytoplasmic trf-rec mRNA levels as compared with an untreated control. This is due to posttranscriptional stabilization of trf-rec mRNA via interaction of IRP with the IREs present at the 3′-untranslated region of its mRNA.18,19 In contrast, supplementation of cells with iron salts resulted in reduced amounts of trf-rec mRNA, reflecting the decreased stability of the mRNA under these conditions.18 19 Treatment of K562 cells with increasing concentrations of Epo caused a dose-dependent increase in trf-rec mRNA in K562 cells (Fig 5) that was comparable to or even greater than trf-rec mRNA levels observed after treatment with desferrioxamine. Densitometric evaluation of Northern blots more clearly showed the significant increase in trf-rec mRNA concentration upon supplemtentation of Epo (1.7 ± 0.3 [increase of the trf-rec/β-actin mRNA ratio relative to the control, in which the ratio is set 1 corresponding to 100%] for 0.5 U/mL Epo [n = 3], 2.2 ± 0.4 for 5 U/mL Epo [n = 5], and 2.4 ± 0.4 for 50 U/mL Epo [n = 5], respectively; P < .05 for 0.5 U/mL Epo; P < .01 for 5 U/mL and 50 U/mL Epo).
Increase of trf-rec mRNA concentration upon Epo-treatment of K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or the indicated concentrations of human recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a human trf-rec cDNA or a rat GAPDH probe. The results of one of three similar experiments are shown.
Increase of trf-rec mRNA concentration upon Epo-treatment of K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or the indicated concentrations of human recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a human trf-rec cDNA or a rat GAPDH probe. The results of one of three similar experiments are shown.
Moreover, perturbation of MEL cells with iron caused the same relative changes in trf-rec mRNA concentrations as observed in K562 cells (Fig 6). Treatment of MEL cells with murine Epo increased cytoplasmic trf-rec mRNA concentrations after approximately 8 hours, which is 4 hours after the induction of IRP-binding activity (compare Figs 4 and 6). Trf-rec mRNA concentrations remained high for at least 24 hours after stimulation with Epo. The changes in trf-rec mRNA levels are specific, because GAPDH mRNA levels were not altered by either treatment (Fig 6, lower panel).
Modulation of Trf-rec mRNA concentration upon treatment of MEL cells with EPO. MEL cells were treated for 16 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or, for the indicated times, with 0.5 U/mL of murine recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a murine trf-rec cDNA or a rat GAPDH probe. The results of one of four similar experiments are shown.
Modulation of Trf-rec mRNA concentration upon treatment of MEL cells with EPO. MEL cells were treated for 16 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or, for the indicated times, with 0.5 U/mL of murine recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a murine trf-rec cDNA or a rat GAPDH probe. The results of one of four similar experiments are shown.
Transferrin binding and trf-rec expression on K562 cells exposed to Epo.Because Epo increased the level of trf-rec mRNA in K562 erythroleukemic cells, it was of interest to determine if this resulted in an enhanced expression of cell-surface trf-rec. Binding studies showed that total transferrin binding was markedly increased by incubation with Epo at both 24 and 72 hours of incubation (Table 1). As with mRNA levels, similar effects were obtained with either 5 or 50 U/mL of Epo for transferrin binding.
Increased Binding of Transferrin by K562 Cells in Reponse to Epo
| Treatment . | Transferrin Binding (ng/106 cells) . | |
|---|---|---|
| . | 24 h . | 72 h . |
| None (control) | 2.6 ± 0.4 | 2.7 ± 1.1 |
| Desferrioxamine (100 μmol/L) | 7.9 ± 1.4* | 14.2 ± 2.5 |
| Epo (5 U/mL) | 4.2 ± 1.4† | 5.3 ± 1.1* |
| Epo (50 U/mL) | 4.9 ± 1.4* | 7.4 ± 2.3* |
| Treatment . | Transferrin Binding (ng/106 cells) . | |
|---|---|---|
| . | 24 h . | 72 h . |
| None (control) | 2.6 ± 0.4 | 2.7 ± 1.1 |
| Desferrioxamine (100 μmol/L) | 7.9 ± 1.4* | 14.2 ± 2.5 |
| Epo (5 U/mL) | 4.2 ± 1.4† | 5.3 ± 1.1* |
| Epo (50 U/mL) | 4.9 ± 1.4* | 7.4 ± 2.3* |
Cells were preincubated for 24 and 72 hours with human recombinant erythropoietin (Epo), desferrioxamine, or left untreated (control); were washed; and were incubated on ice with 125I-transferrin (2 μg) for 30 minutes. After consecutive washing steps, cell-bound 125I-transferrin was determined. Means ± SD for six independent experiments are shown. Calculation of statistical differences in relation to the control were performed using the Student's t-test.
P < .01.
P < .05.
To show that these changes were due to modification of the number of receptor sites rather than to an altered affinity of the interaction between transferrin and trf-rec, binding was analyzed by the Scatchard procedure, after correcting for nonspecific binding. As can be seen in Fig 7, Epo (50 U/mL) more than doubled the number of binding sites for transferrin on K562 cells, whereas exposure to desferrioxamine also caused the expected increase in transferrin binding sites. Neither treatment greatly affected the binding affinity (Fig 7), indicating that the enhanced binding of transferrin by K562 cells after Epo treatment was due to an increase in the number of receptors and not to a change in their affinity. Thus, Epo appears to be able to upregulate the expression of trf-rec on a responsive cell line such as K562.
Scatchard analysis of transferrin binding to K562 cells. Cells were preincubated for 24 hours with 50 U/mL human recombinant Epo (Epo), 100 μmol/L desferrioxamine (Dfo), or no addition (C) and were then incubated for 30 minutes on ice with 125I-transferrin. Nonspecific binding was determined by incubating with a 200-fold excess of unlabeled transferrin. The number of bindings sites per cell after correcting for nonspecific binding were, for control, n = 0.45 × 105 (dissociation constant [kd] = 41 nmol/L); for Epo-treated cells, n = 1.11 × 105 (kd = 43 nmol/L); and for desferrioxamine-treated cells, n = 2.92 × 105 (kd = 43 nmol/L). The results of one of three similar experiments are shown.
Scatchard analysis of transferrin binding to K562 cells. Cells were preincubated for 24 hours with 50 U/mL human recombinant Epo (Epo), 100 μmol/L desferrioxamine (Dfo), or no addition (C) and were then incubated for 30 minutes on ice with 125I-transferrin. Nonspecific binding was determined by incubating with a 200-fold excess of unlabeled transferrin. The number of bindings sites per cell after correcting for nonspecific binding were, for control, n = 0.45 × 105 (dissociation constant [kd] = 41 nmol/L); for Epo-treated cells, n = 1.11 × 105 (kd = 43 nmol/L); and for desferrioxamine-treated cells, n = 2.92 × 105 (kd = 43 nmol/L). The results of one of three similar experiments are shown.
Stimulation of cellular iron uptake by Epo.Incubation of K562 cells with Epo (5 U/mL) resulted in a small but significant (P < .05) increase in iron uptake (0.49 ± 0.03 [n = 4] v 0.40 ± 0.02 ng Fe/106 cells/h for controls). Desferrioxamine caused a significant but still relatively modest increase in iron uptake (0.55 ± 0.04 ng Fe/106 cells/h). Although the increase of iron uptake by Epo was relatively modest, it was reproducibly observed, and the effect of desferrioxamine was likewise small but consistent.
DISCUSSION
The study presented here describes a novel functional pathway by which Epo influences regulation of cellular iron metabolism via modulation of the interaction between IRE and IRP. We have shown that, in human (K562) and MEL cells, Epo activates presumably IRP-1, the central regulatory protein for orchestrating cellular iron metabolism via posttranscriptional and translational modulation of the expression of the proteins involved in cellular iron uptake, storage, and consumption. Activation of IRE-binding by IRP-1 via Epo was followed by increased concentrations of trf-rec mRNA in these cells. It is well established that activation of IRE-binding function of IRP increases trf-rec mRNA expression via posttranscriptional mRNA stabilization.18-20 This is achieved by interaction of activated IRP with IREs in the 3′-untranslated region of trf-rec mRNA, thus preventing degradation of this mRNA by a specific RNase. It therefore seems very likely that the same mechanism accounts for increased trf-rec mRNA expression in response to Epo treatment. This notion is further supported by our kinetic studies showing that IRP-1 activation precedes the increase of trf-rec mRNA levels (Figs 4 and 6).
We have also shown that the increased trf-rec mRNA levels after Epo treatment of K562 cells led to enhanced expression of trf-rec, as reflected by a significant increase in cell-surface transferrin binding sites.
The Epo-induced changes in IRP-binding affinity to IREs appear to quantitatively account for the changes in levels of trf-rec mRNA, further indicating that posttranscriptional regulation of iron metabolism via IRP activation may be primarily responsible for the Epo-induced increase in trf-rec expression. However, whereas Epo produced an effect equal to or even greater than that of desferrioxamine at the level of IRP activation and the amount of trf-rec mRNA, its effect on surface trf-rec expression and iron uptake was less than that of desferrioxamine. The reason for this difference is unclear, but may relate to the fact that desferrioxamine causes iron starvation and presumably a general decrease in metabolic activity, whereas the effect of Epo, as discussed below, is primarily a stimulatory one on cell metabolism. This may result in different rates of endocytosis of the trf-rec/transferrin complex and in different ratios of surface to intracellular receptors.30 Maturation of erythroid cells results in exocytic loss of trf-rec,31 which would cause a decrease in the number of trf-rec relative to mRNA levels. The rather modest effects of both Epo and desferrioxamine on iron uptake may be due to the fact that some iron taken up by K562 cells in vitro is subsequently released, thus reducing net uptake.32
The effects of Epo on activation of IRE-binding by IRP were not observed in a human myelomonocytic cell line (THP-1). In contrast to erythroleukemic and erythroid progenitor cells, human macrophages and macrophage-like cell lines do not express Epo receptors.2,4,33 Because MEL and K562 cells express Epo receptors, the later one albeit to a lesser extent,34 one could speculate whether this receptor-ligand interaction may in part account for modulation of IRP activity by Epo in erythroid cells.
Activation of IRE-binding of IRP in erythroid cells appears not to be due to induction of differentiation by Epo, because treatment of cells with DMSO, a known inducer of differentiation especially in MEL cells, did not significantly alter IRE-binding by IRPs as compared with control cells (Fig 4). Treatment of MEL and Friend erythroleukemic cells with DMSO has previously been shown to increase trf-rec expression via an as yet not fully elucidated transcriptional mechanism.35,36 Our observation that DMSO did not alter IRE-binding by IRP is confirmed by results previously made.36 This indicates that the effects of Epo and DMSO on iron metabolism are of a different nature.
Our observations of an effect of Epo on trf-rec expression via IRP activation agrees well with previous results showing increased numbers of plasma trf-rec during erythroid hyperplasia,37 a condition dependent on the action of Epo.1-3 Furthermore, the reported increase in synthesis of trf-rec in Friend virus-infected erythroid cells isolated from the spleen of infected mice after induction of maturation by Epo38 is in good accordance with our data, although the effect of viral infection must be taken in account.38 Moreover, increased uptake of iron after administration of Epo, observed in vivo in healthy volunteers39 or during erythroid hyperplasia,40 may from the results of this study be due to Epo-induced increase of trf-rec expression; uptake of iron by erythroid cells occurs exclusively via the interaction of iron-loaded transferrin with trf-rec, followed by cellular uptake of the transferrin/trf-rec complex via endocytosis and subsequent release of iron into the cytoplasm.41 42
Finally, there remains the question of how Epo regulates IRP. It seems unlikely to be due to a direct effect of Epo on the conformation of IRP, because activation of IRE/IRP interaction was not observed in THP-1 cells. Instead, Epo may induce a signal transduction cascade that could lead to activation of the IRE-binding function of IRP, as occurs with activation of IRP by H2O2 , which involves stress-induced kinase/phosphatase pathways.13 Based on our results, this pathway appears not to be very likely, because the induction kinetics of IRP-1 by Epo and H2O213 are different. Alternatively, the effect of Epo on IRP could be mediated indirectly via alteration of the availability of iron from the so-called regulatory iron pool that is thought to be responsible for IRP activity due to iron perturbation.10,12,20 This theory would be favored by our time course experiments (Fig 4) showing similar activation kinetics of IRP-1 by Epo and by iron perturbations.13,19 21 Nevertheless, the effects of Epo and desferrioxamine towards activation of IRP-2 appear to be different (Fig 4), which could point to an alternative, yet not eluciadated mechanism by which Epo modulates activation of IRPs.
In context with our results, the stimulatory effect of Epo on protoporphyrin IX synthesizing enzymes, without change in heme oxygenase activity, in human bone marrow cell culture is of interest.43 Increased synthesis of protoporphyrin IX after Epo administration could result in increased heme formation and thus a reduction of iron in the regulatory pool that, in turn, would cause a conformational change of IRP, thus enhancing its IRE-binding affinity.6-8 This would then lead to increased trf-rec expression and uptake of iron into cells to obtain sufficient iron supply for hemoglobin synthesis. Moreover, because the key enzyme of heme biosynthesis, e-ALAS, is also subjected to translational regulation via IRE/IRP interaction,6-8,16,17, 44 Epo could effect heme biosynthesis also via stimulation of transferrin/trf-rec mediated iron uptake. According to the metabolic pathway described herein, treatment with Epo would progressively increase intracellular iron concentrations, which would then reduce IRE-binding by IRP, thus unblocking e-ALAS translation44 and promoting heme biosynthesis. Undoubtedly, future studies will have to definitely prove the impact of Epo on the various biochemical aspects of heme biosynthesis.
These mechanisms could also be of clinical interest, eg, in patients with anemia of chronic disease, who present with low serum iron and hemoglobin concentrations, whereas their serum levels of ferritin and porphyrins are increased.45,46 The blunted response to Epo in such patients could be due not only to the inhibitory effects of cytokines on erythropoiesis,45-47 but also to the decreased uptake of iron by erythroid progenitors as a results of withdrawal and sequestration of iron by the reticuloendothelial system.45-47 Therefore, our data may provide some useful indications for improving the response to Epo therapy. It is possible that sequential administration of Epo and iron might more effectively stimulate erythropoiesis via an enhanced trf-rec–mediated uptake of iron into erythroid progenitor cells.
Supported by the Austrian Research Funds FWF (Project No. 10603-MED) and by the Scottish Office Home and Health Development.
Address reprint requests to Günter Weiss, MD, Department of Internal Medicine, University Hospital, Anichstr. 35, A-6020 Innsbruck, Austria.

![Fig. 1. Activation of IRE-binding activity of IRP by Epo in K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), 50 U/mL human recombinant Epo (Epo), or 1.5% DMSO or remained untreated (control [C]). Fifteen micrograms of detergent cell extracts was assayed for IRE-binding activity of IRP by means of gel shift assay in the absence (upper panel) or presence of 2% 2-mercaptoethanol. After fixation, gels were exposed for 6 to 48 hours to x-ray films. The IRE/IRP complex and the nonbound IRE-probe (free probe) are shown in the upper panel, whereas in the lower panel only RNA-protein complexes are pictured. The results of one of seven similar experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/2/10.1182_blood.v89.2.680/4/m_bl_0026f1.jpeg?Expires=1767737993&Signature=z-m~daDNYSBaNTjJ7Cw9~SRyRXptpjUfzJ9O1zW7-M0N38vTDnCa-8Hh~-RBi1MCOashmudhPrmTAApPGLNyS-yVR2YkoSvAbqXLNI5L9lGrW0NWwejUH89UX9Mv4A3b9377Wx9kdx7b8rbCxWcKdN5KVWDTTHzDLm8hMFxbATvewGpf7zg8OxIANf4KF2bUQau-Z7Z~RxdK1gwWSXnB-sX6XJtqn4SVy1KgdmQI7QdNiClw843fHCFhEQlSPmI0jrHqACNGSKnpZaZD9XZsaX8z33Mr04AQnhBQqbiM~fIz2fB3a7HmMZfQPlfTXT0b8nNKdTC~7rZtfZcUKXIIYQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 4. Induction kinetics of IRPs by Epo in MEL cells. Cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), with 100 μmol/L desferrioxamine (D), and, for the indicated times, with murine recombinant Epo (0.5 U/mL) or remained untreated (control [C]). Gel retardation assays were performed exactly as described in the legend to Fig 1. The results of one of three representative experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/2/10.1182_blood.v89.2.680/4/m_bl_0026f4.jpeg?Expires=1767737993&Signature=DCmb~fVh5fJjb1hLRNZMDG82umJnjMOtJNGQ1Z9OiZJFd6sVGCy6lnHCWYBWVE8UIBzHY1MevmbvxpWUyMQYRSAfJYY0s8aGojanHJdjCxMdw2zfBuTQmMX8-JFt33I8SrJVNOhwQ7t1J7PALwFNiOtevx36ASqscJdwdv34BhreuBsXt9jZvyBV8akS-Rqhs6zR4ju-KwjOpRpBUsP9sTofOqIUeB8jSMeuIPt2c48mNwFGS-ulkG0aScfyxcGCUXqHOCSxem0J4P7F5hSCOIZkPCGooYOO1~nfrb4QvIxf~c73PrWeuOLAABdVgKh61aBJ~975firHoldQCiZhSw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Increase of trf-rec mRNA concentration upon Epo-treatment of K562 cells. K562 cells were treated for 24 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or the indicated concentrations of human recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a human trf-rec cDNA or a rat GAPDH probe. The results of one of three similar experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/2/10.1182_blood.v89.2.680/4/m_bl_0026f5.jpeg?Expires=1767737993&Signature=ULBj2tzTUoURrX13bdbo8vI6fmcQK5we0tjeTq2v-eFvTfJEQn7GByFwHuyIrc04nsTvX3-IiHUhsf-6Ntsc-rVuEZ-HZCoSlfPZHeZQsp4lfUx1v2IUkQ8Kgcz8O2JsgwNF3GnrhjzMhRkbs5yCu5euDMY7oVBNzGgagsaSdispE4P9GmyBHPNJ-hSyLVGgJAui6dZosbDEtlKSffTzoJ8FPuF4rfWzCNksfVXm2JqS5urJX83B520qeRxZQHtVAFghBmIFhR9OcQwjL6~nkT5mPSmBKUgaSvM01h8BH6ygZLT4pRJnBKzzbIkL-XbthIpEUIv2geyU~TR1nxv6xQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 6. Modulation of Trf-rec mRNA concentration upon treatment of MEL cells with EPO. MEL cells were treated for 16 hours with 50 μmol/L Fe(NO3 )3 (I), 100 μmol/L desferrioxamine (D), or, for the indicated times, with 0.5 U/mL of murine recombinant Epo (Epo) or remained untreated (control [C]). The total RNA was then extracted and 10 μg was subjected to Northern blotting with a murine trf-rec cDNA or a rat GAPDH probe. The results of one of four similar experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/2/10.1182_blood.v89.2.680/4/m_bl_0026f6.jpeg?Expires=1767737993&Signature=SMFIZ8WJWUpCWStnEaYFeRJ1yWRchpcgkJroXo0X6jOn9AhJGi4xdqPL2Bz1sg-FNrR2EwcExIL6qbaeF4rcuq8UWcOyGIGQonRrZzxOBuTt6hPIKGQzrsHfYAPjLdKc-P3Mb2xBXSkxYX7dPmnyhPGHyYfMIRDcLF1Kysy~umnlPlcc0IkLux1OKtC1U~WjtzESxfk--lF3PivISgcX6kQquXauh7RHmEAEo1HFM75~nSYm~0l0OwvUMxveGemYebe0WsQD3HCkFHqDZmPjz6MTkFPVK81tkq6PaCtKFtm77W80ZEwZDIJb40gzfSYXOmrcIL4-fsp4xQHeuAyziw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 7. Scatchard analysis of transferrin binding to K562 cells. Cells were preincubated for 24 hours with 50 U/mL human recombinant Epo (Epo), 100 μmol/L desferrioxamine (Dfo), or no addition (C) and were then incubated for 30 minutes on ice with 125I-transferrin. Nonspecific binding was determined by incubating with a 200-fold excess of unlabeled transferrin. The number of bindings sites per cell after correcting for nonspecific binding were, for control, n = 0.45 × 105 (dissociation constant [kd] = 41 nmol/L); for Epo-treated cells, n = 1.11 × 105 (kd = 43 nmol/L); and for desferrioxamine-treated cells, n = 2.92 × 105 (kd = 43 nmol/L). The results of one of three similar experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/89/2/10.1182_blood.v89.2.680/4/m_bl_0026f7.jpeg?Expires=1767737993&Signature=PXHIe3rNTchrK3NLxmItkHD8-Hr1lxJFUL8bfA5ZZ9NtDQy1fHZmcN1ZBc6U7gRnkdK2xsKz0ovh-61lFrXSKm68drg0ll22h~4eEA3ASco9xjsEw~itwXYJP9jx6YJZqeuiguXMP9xV48v~lY7x3v9oexNoG2rlu8PuAWAoh4dLT04yAI2R~r~LaZxO0gFpZKxZNRk~wxonylDh5vytu821lPa~xjBSuNkQpWbCHJ1l6k7MWuqQmYIYygyuGXX2vMyUKuHjp-TnwBpYFBZIw0oDcdceWYCuaU53CFiL46vgWHk-X-OOIsLVe~2nmtu7~N1VgVBdEoK-6tqKqUVS3Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal