Abstract
Activation of the contact and complement systems in C1-inhibitor deficiencies is thought to contribute to the pathogenesis of angioedema attacks by releasing kinins. Trigger stimuli of attacks may also activate coagulation. This is particularly important because experimental data suggest that thrombin, the main enzyme of the coagulation cascade, increases vascular permeability and can thus influence edema formation. We have studied 19 patients with hereditary angioedema (HAE) during remission, 5 HAE patients during acute attacks, and 6 patients with acquired angioedema (AAE) during remission and during seven attacks. Thirty normal subjects, matched for sex and age, served as controls. Generation of thrombin was measured by enzyme-linked immunosorbent assay (ELISA) as plasma levels of the prothrombin fragment 1 + 2 (F1 + 2); the initiators of the tissue factor and contact coagulation pathways were investigated by measuring plasma levels of activated factor VII (FVIIa) coagulometrically and activated factor XII (FXIIa) by ELISA. Cleavage of high molecular weight kininogen (HK) was evaluated by immunoblotting analysis. F1 + 2 was slightly increased during remission and further significantly increased during attacks in both HAE (P = .0115) and AAE. FVIIa and FXIIa, normal during remission, increased strikingly during attacks in both HAE (P = .0022 and P = .0044) and AAE. During remission, cleaved HK was normal in HAE and high in AAE; during attacks it increased in HAE (P = .0008) and remained elevated in AAE. Our data indicate that in C1-inhibitor deficient patients there is increased generation of thrombin during attacks, with signs of activation of both the contact and tissue factor coagulation pathways. In conclusion, C1-inhibitor deficiency, whether hereditary or acquired, has demonstrable activation of the coagulation and kinin-forming cascades during attacks and that thrombin should be considered a possible contributing factor in the pathogenesis of edema in HAE and AAE.
THE INHIBITOR OF THE first component of complement (C1-INH) is also the main regulatory protein of the contact system, inhibiting activated factor XII (FXIIa), kallikrein, and activated factor XI (FXIa).1 Deficiency of C1-INH, which can be inherited (hereditary angioedema, [HAE]) or acquired (acquired angioedema, [AAE]), results in self-limiting swelling of subcutaneous tissues, bowel walls, and upper airways.2 Symptoms are episodic despite continuously defective C1-INH levels. Their pathogenesis is at present unknown, although candidate mediators are bradykinin,3,4 which is released by the action of kallikrein on high molecular weight kininogen (HK) during contact system activation,5 and/or a kinin-like peptide released from C2 during complement activation.6,7 Evidence for contact system involvement in C1-INH deficiency comes from in vivo studies that have demonstrated its activation in plasma of HAE patients during attacks8-11 and from in vitro studies in which bradykinin was generated by incubating plasma from patients during remission at 37°C.3,4 Physical trauma and surgery frequently act as triggers of attacks,12 perhaps because of their ability to activate the contact system. These stimuli are also important activators of the coagulation cascade through the expression of tissue factor and the activation of factor VII. There are very few data in C1-INH deficiency on activation of coagulation factors downstream from the contact system.
The in vivo importance of contact system activation in hemostasis is questioned (patients who have deficiencies of the contact system components FXII, prekallikrein, and HK do not have a hemostatic defect) and increasing evidence indicates a pivotal role of activated factor VII and tissue factor.5,13,14 Recently a small degree of activation of factor VII in patients with C1-INH deficiency was reported,15 but the activation of coagulation factors downstream was not investigated. Whether or not such activation occurs is particularly interesting because experimental data indicate that thrombin, the final enzyme of the coagulation cascade, increases vascular permeability and thus could influence edema formation.16,17 This action of thrombin has a unique mechanism, cleavage, and activation of a receptor at the endothelial cell surface, which induces intercellular gap formation.18 The prothrombin fragment F1 + 2, an inactive fragment released from the amino terminus of the prothrombin molecule by factor Xa in the presence of factor Va and calcium ions, is considered to be a reliable marker of thrombin generation in vivo.19
With this background, we have evaluated thrombin generation by measuring prothrombin fragment F1 + 2 and the contact and tissue factor pathways that initiate blood coagulation by measuring FVIIa and FXIIa, in patients with hereditary and acquired deficiency of C1-INH. Our findings indicate that thrombin is generated during edema attacks and thus might participate in the formation of edema in these patients.
MATERIALS AND METHODS
Patients.We studied 19 HAE patients (8 men and 11 women; age range, 20 to 60 years) during remission, 5 HAE patients during acute attacks (3 men and 2 women; age range, 20 to 48 years), and 6 AAE patients (4 men and 2 women; age range, 58 to 76 years). Ten HAE patients studied during remission and 3 during attacks had type I C1-inhibitor deficiency (low levels of functional and antigenic C1-inhibitor), whereas type II deficiency (low levels of functional C1-inhibitor only) was observed in 9 patients studied during remission and in 2 patients during attacks. Nine of these patients were on long-term treatment with minimal effective doses of anabolic steroids (danazol 100 to 200 mg/d) and 15 were not being treated. Four patients with AAE had not been treated prophylactically and 2 were taking tranexamic acid (3 g/d); all 6 patients had an autoimmune form of AAE, with autoantibodies to C1-inhibitor of different classes (3 IgG, 2 IgM, and 1 IgA); 4 of them had a monoclonal gammopathy and 2 had no associated disease. Three of the 6 AAE patients were also studied during acute attacks for a total of 7 episodes (4 in the first patient, 2 in the second, and 1 in the third). Eleven of 12 attacks of edema observed in our patients involved the upper airways and the subcutaneous tissues of face or neck and 1 involved the intestinal tract. Thirty normal subjects (15 men and 15 women; age range, 20 to 76 years) served as normal controls.
Blood sampling.Blood was drawn by clean venipuncture with minimal stasis and collected in siliconized Vacutainer tubes (Becton Dickinson, Plymouth, UK) containing 0.13 mol/L trisodium citrate. For the assessment of high molecular weight kininogen, we used tubes containing ethylene-diaminetetraacetic acid (EDTA) (10 mmol/L) and hexadimethrine bromide (Polybrene) (0.05% wt/vol), which has been shown to prevent in vitro activation of contact system,20 although some degree of HK cleavage may occur. Tubes were centrifuged at 2,000g for 10 minutes at room temperature, and plasma aliquots were stored in polystyrene tubes at −80°C until tests were performed.
Methods.Prothrombin fragment 1 + 2 was assessed in citrated plasma with a sandwich enzyme-linked immunosorbent assay (ELISA) (Enzygnost F1 + 2, Behringwerke Ag, Marburg, Germany). The method uses a rabbit antibody to human F1 + 2 as capture antibody and a rabbit peroxidase-conjugated antiprothrombin as second antibody. Intraassay and interassay coefficients of variation are ≈8%.
Factor VIIa was measured in trisodium citrated plasma with a one-stage prothrombin-time–based assay using a truncated soluble form of recombinant tissue factor (kindly supplied by Dr Y. Nemerson, Mount Sinai Medical School, New York, NY) that, upon relipidation, reacts with FVIIa, but not with one-chain factor VII.21 The results were expressed as ng/mL referring to a standard of recombinant FVIIa (Novo Nordisk, Gentofte, Denmark). Intraassay and interassay coefficients of variation are 2.2% and 8.1%.
Factor XIIa was measured in citrated plasma with a sandwich ELISA (Shield Diagnostic Ltd, Dundee, UK) which uses a specific mouse monoclonal antibody for human FXIIa (2/215) as capture antibody and a sheep polyclonal anti-FXII antibody conjugated to alkaline phosphatase as second antibody. The method detects both forms of FXIIa: the 80-kD protein known as αFXIIa or simply FXIIa and the 28- to 30-kD fragment known as βFXII or FXIIf, without cross-reactivity with human factor XII zymogen.22 Intra- and inter-assay coefficients of variation are 5.1% and 8.2%.
Cleavage of high molecular weight kininogen (HK) was assessed on EDTA-Polybrene plasma by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and immunoblotting analysis, using a method based on that described by Berrettini et al.10 After electrophoretic transfer of proteins from gel onto a polyvinylidene difluoride membrane (Immobilon; Millipore Corp, Milford, MA), HK was identified with goat polyclonal antilight-chain HK (Nordic, Tilburg, the Netherlands) and visualized with a biotinylated rabbit antigoat antibody (Sigma Chemical Co, St Louis, MO). The apparent molecular masses of the proteins were estimated by comparison with the high molecular weight protein markers from Bio-Rad Laboratories, Hercules, CA. With this method, native HK appears as a band with Mr 130,000, and cleaved HK is represented by two bands with Mr 107,000 and 98,000. Density of the bands was evaluated by computerized image analysis (Image Master; Pharmacia, Uppsala, Sweden). The amount of cleaved HK (bands with Mr 107,000 and 98,000) was expressed as percentage of total HK (sum of the three bands).
Statistical analysis.The significance of differences between groups was assessed by the nonparametric test of Wilcoxon-Mann-Whitney. A P value of less than .05 was considered to indicate a statistically significant difference.
RESULTS
Complement measurements in patients with HAE and AAE during remission are reported in Table 1. No significant change of any measurement from that during remission was observed during acute attacks.
Complement Measurements in 24 Patients With HAE and 6 Patients With AAE
| . | C1-Inhibitor . | C1-Inhibitor . | C4 Antigen % . |
|---|---|---|---|
| . | Function % . | Antigen % . | . |
| HAE Type I (n = 13) | 22 (<10-42) | 19 (<10-39) | 20 (<10-56) |
| HAE Type II (n = 11) | 19 (<10-32) | 185 (54-205) | 16 (<10-51) |
| AAE (n = 6) | <10 | 25 (<10-39) | <10 |
| Normal ranges | (70-130) | (70-130) | (60-140) |
| . | C1-Inhibitor . | C1-Inhibitor . | C4 Antigen % . |
|---|---|---|---|
| . | Function % . | Antigen % . | . |
| HAE Type I (n = 13) | 22 (<10-42) | 19 (<10-39) | 20 (<10-56) |
| HAE Type II (n = 11) | 19 (<10-32) | 185 (54-205) | 16 (<10-51) |
| AAE (n = 6) | <10 | 25 (<10-39) | <10 |
| Normal ranges | (70-130) | (70-130) | (60-140) |
HAE patients are divided into type I (low levels of both antigenic and functional C1-inhibitor) and type II (low levels of functional C1-inhibitor only). Data are reported as median values (ranges in parenthesis). Results are expressed as percent of a normal human pooled plasma.
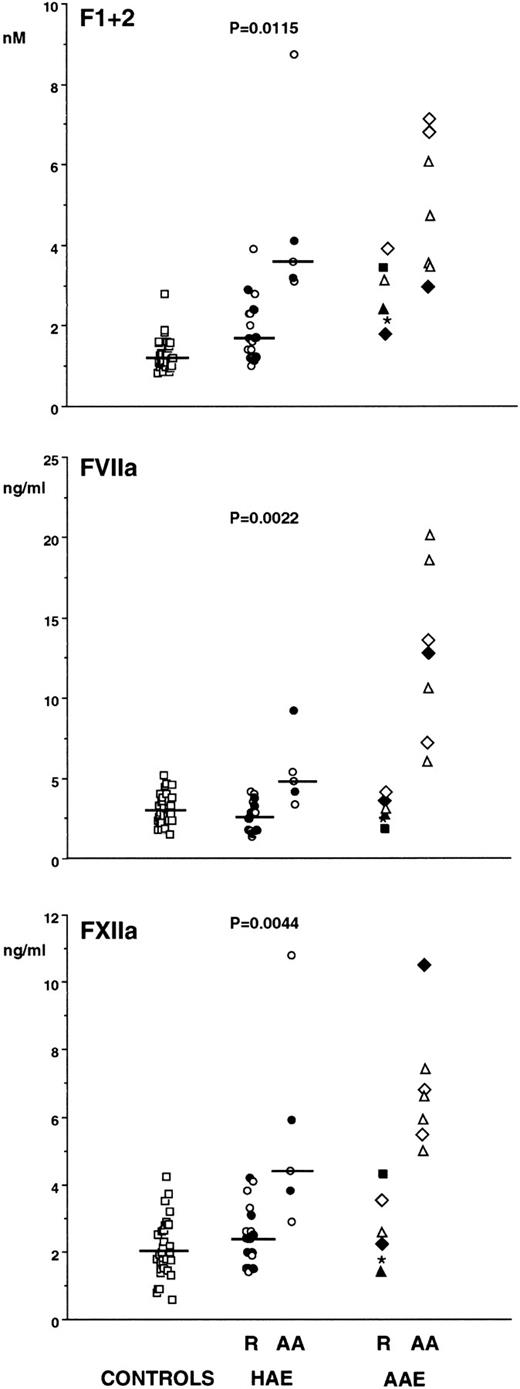
F1 + 2 in HAE patients during remission was slightly higher (1.69 nmol/L [1.00 to 3.90 nmol/L]) (median [range]) than in normal controls (1.24 nmol/L [0.82 to 2.80 nmol/L]) (P = .0025) and increased significantly during attacks (3.50 nmol/L [3.00 to 8.75 nmol/L]) (P = .0115). Patients with AAE had a similar pattern, with high F1 + 2 plasma levels during remission and a further increase during acute attacks (Fig 1, top panel). To rule out the possibility of plasma protein concentration due to the formation of edema, we measured total plasma proteins with the biuret method in samples from 10 of 12 patients during attacks and 24 to 48 hours after remission of the attack. The median values of attack samples (6.11 g/dL; range, 5.76 to 6.94 g/dL) did not differ significantly from those of remission samples (6.14; range, 5.50 to 7.05).
Plasma levels of prothrombin fragment F1 + 2 (top panel), activated factor VII (FVIIa) (middle panel), and activated factor XII (FXIIa) (bottom panel) in 30 normal subjects (□), in 19 patients with HAE during remission (R), in five patients with HAE during acute attacks (AA) (type I = ○; type II = •) and in six patients with AAE. AAE patients (individuals identified by different symbols) were observed during R and three of them also during seven episodes of AA. Horizontal lines represent medians.
Plasma levels of prothrombin fragment F1 + 2 (top panel), activated factor VII (FVIIa) (middle panel), and activated factor XII (FXIIa) (bottom panel) in 30 normal subjects (□), in 19 patients with HAE during remission (R), in five patients with HAE during acute attacks (AA) (type I = ○; type II = •) and in six patients with AAE. AAE patients (individuals identified by different symbols) were observed during R and three of them also during seven episodes of AA. Horizontal lines represent medians.
Plasma levels of FVIIa during remission were normal in both HAE (2.60 ng/mL [1.10 to 4.20 ng/mL]) and in AAE. They were increased significantly during attacks in HAE (4.80 ng/mL [3.30 to 9.20 ng/mL]) (P = .0022) and to a higher extent in AAE (Fig 1, middle panel). During 10 of 12 attacks, we also measured FVII antigen with an ELISA method23 and calculated the relative amount of FVIIa. Plasma levels of FVII antigen during acute attacks (428 ng/mL [range, 260 to 555 ng/mL]) did not differ from those during remission (400 ng/mL [270 to 635 ng/mL]), whereas FVIIa expressed as percent of total FVII, both in HAE and in AAE, was strikingly higher during attacks (2.3% [0.9% to 5.0%]) than during remission (0.5% [0.4% to 1.2%]).
FXIIa, normal during remission, significantly increased during attacks in both HAE (from 2.40 ng/mL [1.40 to 4.20 ng/mL] to 4.30 ng/mL [2.80 to 10.70 ng/mL]) (P = .0044) and AAE (Fig 1, bottom panel).
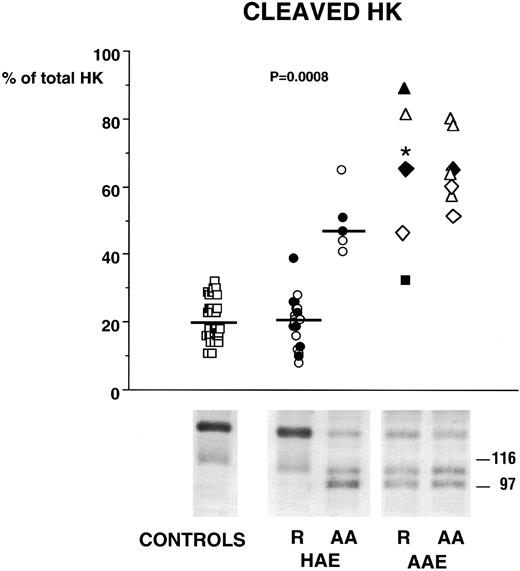
SDS-PAGE followed by immunoblotting analysis of HK showed in normal plasma a major band of Mr 130,000, which represents native HK and a faint one of Mr 107,000, which represents a catabolic product. After in vitro activation of the contact system with kaolin, normal plasma showed a diminution of the band of Mr 130,000, an increase of the band of Mr 107,000 and the appearance of a band of Mr 98,000. Similar patterns were evident in both HAE and AAE during attacks and only in AAE during remission (Fig 2).
Plasma levels of cleaved high molecular weight kininogen (HK) in 30 normal subjects (□), in 19 patients with HAE during remission (R), in five patients with HAE during AA (type I = ○; type II = •) and in six patients with AAE. AAE patients (individuals identified by different symbols) were observed during R and three of them also during seven episodes of AA. Horizontal lines represent medians. In HAE, cleaved HK is normal during remission and significantly increased during attacks, while it is increased in AAE during both remission and attacks. Immunoblots of HK forms illustrating the profiles for each group are presented at the bottom of the figure.
Plasma levels of cleaved high molecular weight kininogen (HK) in 30 normal subjects (□), in 19 patients with HAE during remission (R), in five patients with HAE during AA (type I = ○; type II = •) and in six patients with AAE. AAE patients (individuals identified by different symbols) were observed during R and three of them also during seven episodes of AA. Horizontal lines represent medians. In HAE, cleaved HK is normal during remission and significantly increased during attacks, while it is increased in AAE during both remission and attacks. Immunoblots of HK forms illustrating the profiles for each group are presented at the bottom of the figure.
Plasma levels of cleaved HK during remission were normal in HAE (21% [8% to 39%]) and high in AAE; during attacks they increased in HAE (47% [41% to 65%]) (P = .0008) and remained elevated in AAE (Fig 2).
DISCUSSION
Donaldson24 stated in 1983 that, in view of the broad spectrum of regulatory actions of C1-INH, there is no reason to propose that a single substance causes the symptoms in C1-INH deficiency. Several lines of evidence indicate that complement,25,26 the contact system,8-11and fibrinolysis11 are activated during attacks. There has been little investigation of whether or not the coagulation system, whose activating stimuli (trauma or surgery) also trigger attacks, is also involved. The recent experimental demonstration that thrombin, the final enzyme of the coagulation cascade, induces vasopermeability16-18 prompted us to investigate whether or not this enzyme is generated during angioedema attacks, thus becoming a new candidate mediator of symptoms in C1-INH deficiency.
In this study we demonstrated that in both HAE and AAE the prothrombin fragment F1 + 2 is significantly increased during attacks. The release of F1 + 2 can result from activation of factor X (FXa) by the complex formed by activated factor VII (FVIIa) and tissue factor.27 The increase of FVIIa in our patients during attacks supports the hypothesis that the increase of F1 + 2 results from in vivo generation of active thrombin. We also found that FXIIa is increased during attacks, probably as a consequence of contact system activation. Our method detects both forms of FXIIa: FXIIf, which has been demonstrated able to activate FVII,28 29 and FXIIa (kD 80), whose role in FVII activation is not completely known. We do not know which of the two forms is increased in our patients, but it is possible that FXIIf, which is slightly increased in normal plasma on contact system activation, in this case (due to C1-inhibitor deficiency), becomes important and thus can activate FVII and enhance thrombin generation.
In the scenario of C1-INH deficiency, we believe that the possibility of an involvement of thrombin in the pathogenesis of symptoms must be considered. An obvious concern with this view comes from the observation that F1 + 2 is increased in several pathological conditions such as disseminated intravascular coagulation,30 deep venous thrombosis,31 and endotoxinemia32 that are not characterized by angioedema symptoms. Therefore, thrombin activation per se is not enough to generate angioedema, but in the presence of C1-inhibitor deficiency, it might enhance the effects of other vasoactive substances released by the concomitant activation of complement6,7 and contact system.8-11 In fact, the vasoactive effect of bradykinin can be potentiated by the effect of thrombin, as the two substances represent two distinct classes of endothelial cell agonists that increase vascular permeability by different mechanisms.33,34 In addition to its direct action on endothelial cells, thrombin could also contribute to increased vasopermeability by releasing from fibrinogen fibrinopeptides, which enhance the effects of kinins.35
It is apparently contradictory that patients with deficiency of C1-INH, although they have increased levels of F1 + 2 that indicate a state of hypercoagulability, do not have an increased prevalence of thrombotic events, as would be expected in such a condition. We previously demonstrated an increase of fibrinolytic activity in HAE during attacks11 and also in AAE during remission.36 Our data are too few to define whether hyperfibrinolysis is sufficient to counteract hypercoagulability or whether other as yet unidentified factors may protect these patients from thrombosis. Because there is no intravascular coagulation in our patients, thrombin inhibition by antithrombin III appears to be effective. The observation that HAE patients have normal plasma levels of antithrombin III37 further supports this view.
In this study, we confirmed our previous observations that HK is cleaved only during attacks in HAE11 and during both remission and attacks in AAE.36 In addition, by measuring FXIIa, we found that FXII, the initiator of the contact system, is activated only during attacks. Both kallikrein (generated by the activation of contact system) and plasmin (generated by the activation of fibrinolysis) are able to cleave HK, but the vasoactive peptide bradykinin is released only when HK is cleaved by kallikrein. The enzymatic action of plasmin on HK does not result in bradykinin release, but increases its susceptibility to kallikrein.38 The increase of FXIIa only during attacks supports the view that the activation of the contact system creating the conditions for the release of bradykinin is a critical step for the appearance of symptoms in HAE and in AAE. In the latter, continuous hyperfibrinolytic activity during remission accounts for a plasmin-dependent HK cleavage without effects on vasopermeability. On the other hand, plasmin is also able to activate FXII,39 particularly with the formation of FXIIf, and it may further contribute to contact system activation during attacks.
We conclude from our data that C1-INH–deficient patients have increased generation of thrombin during attacks. Because there is experimental proof that thrombin increases vascular permeability and can potentiate the effects of bradykinin, it is possible that the activation of the coagulation cascade in the presence of C1-INH deficiency could participate in edema formation.
Address reprint requests to Professor Angelo Agostoni, Institute of Internal Medicine, University of Milan, Via Pace, 9-20122 Milano, Italy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal