Abstract
CD95 antigen (also known as Fas or Apo-1) and Fas ligand play key roles in apoptosis of cells of the immune system, function as effector molecules of cytotoxic T lymphocytes, and function in the elimination of activated lymphocytes during the downregulation of the immune response. The critical roles of the Fas-Fas ligand system in apoptosis suggest that its inactivation may be involved in malignant transformation. We analyzed the expression of Fas antigen on adult T-cell leukemia (ATL) cells by flow cytometry and found that Fas antigen expression was absent in a case of ATL and markedly decreased in another case among 47 cases examined. Apoptosis could not be induced in the Fas-negative ATL cells by antibody against Fas antigen. Sequencing of reverse transcription-polymerase chain reaction products of the Fas genes in the Fas negative cells showed two types of aberrant transcripts: one had a 5-bp deletion and a 1-bp insertion in exon 2, and the other transcript lacked exon 4. These mutations caused the premature termination of both alleles, resulting in the loss of expression of surface Fas antigen. These aberrant transcripts were not detected in a nonleukemic B-cell line from the same patient. An RNase protection assay of the Fas gene showed mutations in 2 additional cases with Fas-positive ATL cells of 35 cases examined: 1 case lacked exon 4 and the other was a silent mutation. In the Fas antigen-negative case, leukemic cells were resistant to anticancer drugs in vivo, indicating that the loss of expression of Fas antigen may be associated with a poor response to anticancer drugs. Indeed, Fas-negative ATL cells were resistant to adriamycin-induced apoptosis in vitro, which is consistent with the finding that ATL in this case was resistant to chemotherapy. These findings indicate that mutation of the Fas gene may be associated with the progression of ATL and with resistance to anticancer drugs.
ADULT T-CELL LEUKEMIA (ATL) is an aggressive neoplasm of activated T-lymphocytes which was established as a distinct clinical entity in 1977.1,2 Human T-lymphotropic virus type I (HTLV-I) was found to be the causative virus of ATL.3-5 Thereafter, a number of investigators have studied the clinical, epidemiologic, immunologic, and virologic aspects of ATL.6-8 HTLV-I has a unique genome region, the pX region, between env and the 3′-long terminal repeat (LTR). The pX region contains at least four open reading frames and encodes several gene products, Tax, Rex, p21x, p12I, p13II, and p30II.9-12 Tax can trans-activate not only the LTR but also cellular genes, such as the interleukin-2 receptor gene, certain oncogenes, and the parathyroid hormone-related protein gene.13-16 Such trans-activation of genes by Tax is thought to be one of the mechanisms of leukemogenesis by HTLV-I. However, the presence of tax gene expression is not clearly established in freshly isolated ATL cells; moreover, defective viruses, which cannot produce Tax, have been observed in ATL cells, suggesting that the tax gene is necessary for the initial stages of leukemogenesis, but not essential for the late stage of leukemia.17,18 As suggested by the multistep model of tumorigenesis,19 mutations of various genes are considered to contribute to leukemogenesis; indeed, mutation or deletion of the p53 and p16 genes was detected in an aggressive form of ATL, namely acute or lymphoma-type ATL, indicating that inactivation of these genes was associated with the progression of disease.20 21
Fas antigen (also known as Apo-1 or CD95) is associated with apoptosis, because antibody against Fas antigen can induce apoptosis.22-24 Expression of Fas antigen is ubiquitous, but its ligand, Fas ligand, is expressed in limited cell types, particularly T lymphocytes and natural killer cells, which can induce apoptosis of Fas positive cells.25 Mice with Fas (lpr) and Fas ligand (gld) gene mutations have an abnormality of mature T-cell deletion in the peripheral tissues, resulting in proliferation of T lymphocytes and autoimmune disease, whereas thymic selection is normal in these mutant mice.26,27 Thus, the Fas-Fas ligand system is crucial for the elimination of autoreactive T lymphocytes in the peripheral tissues.28,29 Mutation of the Fas gene in humans also causes an increase in double-negative T lymphocytes and autoimmune diseases, as observed in mice.30,31 Antigen-stimulated T lymphocytes express Fas ligand as well as Fas antigen and commit suicide by this mechanism. Thus, the Fas-Fas ligand system also functions as a regulator of antigen-stimulated T cells.32
We previously demonstrated that ATL cells in some cases proliferated in response to stimulation by autologous cell lines, showing that ATL cells in these cases were derived from autoreactive T cells.33 The fact that the Fas-Fas ligand system is crucial in the apoptosis of autoreactive T cells suggests that an impaired Fas-Fas ligand system in ATL cells may be involved in the leukemogenesis of ATL, leading to leukemic changes of autoreactive T cells.
In this report, we describe defects of Fas genes of ATL cells. In one case, Fas antigens were not detected on ATL cells, and molecular analysis identified mutations in this case. In other cases, RNase protection assays detected Fas gene mutations on single alleles in ATL cells. These observations suggest that mutation of the Fas gene may be associated with the progression of ATL.
MATERIALS AND METHODS
Patients.
Diagnosis was made based on the criteria of Shimoyama et al.34 Genomic DNA was extracted from peripheral blood mononuclear cells (PBMCs) or lymph node cells, and monoclonal integration of HTLV-I provirus was identified by Southern blot analysis using an HTLV-I probe. To establish Epstein-Barr virus (EBV)-transformed B-cell lines, PBMCs were cultured in the presence of B95-8 supernatant as a source of EBV.
Case history.
A 78-year-old man (case no. 2) visited the clinic with the complaint of palpitation; at that time, an increased number of atypical lymphocytes was detected. He was then referred to our hospital. His white blood cell count (WBC) was 11.4 × 109/L, with 80% atypical lymphocytes. Morphologic characteristics and positivity of antibody against HTLV-I suggested the diagnosis of ATL, and the monoclonal integration of HTLV-I provirus was detected in PBMCs by Southern blot analysis. The diagnosis of chronic ATL was established. Thereafter, he attended the outpatient department of our hospital for regular checkups. Three months later, laboratory tests showed a WBC of 21.8 × 109/L and a lactic dehydrogenase (LDH) level of 790 U/L, so VP-16 (50 mg/d) was administrated orally, but it had little effect on the number of ATL cells. The patient then stopped attending the hospital. After 8 months, he was admitted to our hospital because of high fever with chills. Physical examination found systemic lymphadenopathy and hepatosplenomegaly. His WBC was 73.4 × 109/L (atypical lymphocytes, 73%). These data showed that he had an acute crisis of ATL. The oral administration of VP-16 was restarted, but the WBC did not change, and the serum calcium level increased to 12.5 mg/mL. Therefore, 640 mg of cyclophosphamide, 50 mg of adriamycin, 1.5 mg of vincristine, and 125 mg of prednisone were administrated. However, his WBC did not decrease much (63.1 × 109/L, with 87% atypical lymphocytes). Herpes simplex virus infection occurred, and acyclovir was administered as a treatment. Two months after the chemotherapy, the WBC increased to 95.5 × 109/L, with 74% atypical lymphocytes, and the LDH level was 944 U/L. Then, 0.9 mg/d of vincristine, 14 mg/d of adriamycin, and 50 mg of VP-16 were continuously infused for 5 days, but again had little effect. Despite combination therapy with interferon-α and azidothymidine, the number of ATL cells increased. Seven months after the patient's admission, systemic varicella-zoster virus infection and multiple organ failure occurred. Despite salvage chemotherapy, he deteriorated and died.
Expression of Fas antigen.
Expression of Fas antigen was studied by flow cytometry. Tumor cells and neutrophils of ATL patients were incubated at 4°C for 30 minutes with mouse anti-Fas antibody (clone ZB4, 10 μg/mL final concentration; MBL Hiteclone, Nagoya, Japan) or control mouse IgG (10 μg/mL final concentration; DAKO, Carpinteria, CA). This step was followed by two washes with phosphate-buffered saline (PBS)-fetal calf serum (FCS)-azide and incubation at 4°C for 30 minutes with fluorescein isothiocyanate (FITC)-conjugated goat antimouse IgG (1:200 final dilution; Cosmo Co Ltd, Tokyo, Japan). After two washes, cells were analyzed with a FACScan flow cytometer (Becton Dickinson Immunocytometry Systems, Mountain View, CA). The resulting histograms correspond to cell number (y-axis) versus fluorescence intensity (x-axis) plotted on a logarithmic scale.
cDNA synthesis and polymerase chain reaction (PCR).
Total RNA was prepared from PBMCs and tumor cells from 36 ATL patients using Trizol reagent (GIBCO BRL, Paisley, UK), and cDNAs were made from 5 μg of total RNAs using the Superscript Preamplification System (GIBCO BRL) according to the manufacturer's protocol. Oligo dT primers were used to prime first-strand synthesis for all the reactions. In the first round of PCR, 2 μL of the reverse transcriptase reaction mixture was diluted with 50 μL of PCR buffer containing 0.2 mmol/L each of dNTP, 1.5 mmol/L MgCl2, 1.25 U of Taq DNA polymerase (GIBCO BRL), and 20 pmol each of the sense primer (5′-TACGGAGTTGGGGAAGCT-3′) and the antisense primer (5′-GGGTACTTAGCATGCCAC-3′). PCR was performed in a Robo Cycler (Stratagene, La Jolla, CA) for 30 cycles under the following conditions: 30 seconds at 94°C, 30 seconds at 57°C, and 1 minute at 72°C.
RNase protection assays.
This assay was performed using the MisMatch Detect II kit (Ambion Inc, Austin, TX) according to the manufacturer's protocol. In the second round of PCR, the primers were designed to incorporate T7 and SP6 phage promoters into the products: 5′-TAATACGACTCACTATAGGATTGCTCAACAAC-3′ and 5′-ATTTAGGTGACACTATAGGAGGCAGAATCATG-3′. Using 1 μL of the first-round PCR product as the template, we performed the second round of PCR under the same conditions as the first round. Sense and antisense RNA probes were made from the second-round PCR products by in vitro transcription. Briefly, 1 μL of the second-round PCR product was diluted with transcription buffer containing 0.25 mmol/L of each rNTP and 10 U of T7 or SP6 RNA polymerase and the reaction mixture was incubated at 37°C for 1 hour. An equal volume of hybridization buffer was added to each reaction. SP6 transcripts from ATL cells were added to T7 transcripts from normal PBMCs, and T7 transcripts from ATL cells were added to SP6 transcripts from normal PBMCs. To make the no-mismatch control duplex, we mixed T7 transcripts and SP6 transcripts from normal PBMCs. All reactions were heated at 95°C for 3 minutes and cooled to room temperature. The hybridized mixtures were treated with RNase A, and RNase cleavage products were then analyzed on a 2.5% agarose gel.
Subcloning and sequencing.
We cloned the first-round PCR products of the samples in which RNase cleavage products were detected into the pCR2.1 vector using the TA cloning kit (Invitrogen Corp, San Diego, CA). All sequencing experiments were performed with an Applied Biosystems 373 DNA sequencer (Perkin Elmer/Applied Biosystems Division, Foster City, CA) using dye terminators.
Detection of apoptosis.
Apoptosis was assessed by determination of plasma membrane integrity (uptake of propidium iodide [PI]). Cells were plated at 1 × 106/mL in 12-well plates with 2 mL of RPMI1640 media supplemented with 10% FCS and incubated with or without adriamycin at a concentration of 4 μmol/L. Cells were collected 2 and 6 hours later and washed twice with cold PBS/5 mmol/L EDTA. Cells were fixed with ethanol and stained with PI as described.35 Spontaneous PI uptake in the control culture was about 10% to 30% among ATL cells. The percentage of specific cell death was calculated as described elsewhere32: 100 × (Experimental PI Uptake [%] − Spontaneous PI Uptake in Medium [%])/(100% − Spontaneous PI Uptake [%]).
For detection of fragmentation of DNA, cells were plated at 5 × 105/mL in 12-well plates with 2 mL of culture media and incubated with or without anti-Fas antibody (clone CH11, 100 ng/mL final concentration; MBL Hiteclone) at 37°C for 2, 6, or 24 hours. Cells were then collected and washed with PBS and lysed in 100 μL of cell lysing buffer (10 mmol/L Tris-HCl, pH 7.4, 10 mmol/L EDTA, 0.5% Triton X-100). After incubation at 4°C for 10 minutes, samples were centrifuged at 13,000 rpm for 15 minutes. Supernatant fluid was transferred to a fresh tube, mixed with 2 μL of 10 mg/mL RNase A, and incubated at 37°C for 1 hour. To precipitate fragmented DNA, we mixed each sample with 20 μL of 5 mol/L NaCl and 120 μL of isopropanol and centrifuged it at 13,000 rpm. DNA pellets were dissolved in TE buffer and electrophoresed on a 2% agarose gel.
RESULTS
Expression of Fas antigen on ATL cells.
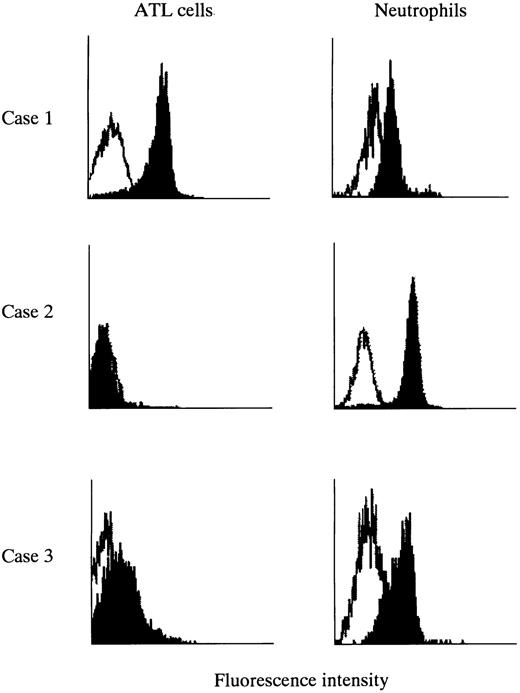
We analyzed expression of Fas/APO-1 (CD95) antigens on fresh ATL cells by flow cytometry using an anti-Fas monoclonal antibody (clone ZB4). In this study, cases in whom the percentage of leukemic cells was greater than 90% were used for analysis. Most ATL cells expressed Fas antigens on their surfaces (Fig 1, case no. 1) as reported previously.36 The fluorescence intensity of Fas antigens was higher on ATL cells than on neutrophils in the same patients.
Expression of Fas antigens on ATL cells and neutrophils from patients with ATL. Heparinized blood was incubated with monoclonal antibody ZB4 (against Fas antigen) or control mouse IgG. Expression of Fas antigen on ATL cells and neutrophils was examined simultaneously by flow cytometry. Shadowed peaks represent Fas antigen and open peaks represent control mouse Ig. Case no. 1, Fas-positive ATL cells; case no. 2, Fas-negative ATL cells; case no. 3, ATL cells with decreased expression of Fas antigen.
Expression of Fas antigens on ATL cells and neutrophils from patients with ATL. Heparinized blood was incubated with monoclonal antibody ZB4 (against Fas antigen) or control mouse IgG. Expression of Fas antigen on ATL cells and neutrophils was examined simultaneously by flow cytometry. Shadowed peaks represent Fas antigen and open peaks represent control mouse Ig. Case no. 1, Fas-positive ATL cells; case no. 2, Fas-negative ATL cells; case no. 3, ATL cells with decreased expression of Fas antigen.
Among 47 cases examined, Fas antigen was not detected in 1 case. In contrast to ATL cells, the neutrophils of this patient expressed normal levels of Fas antigen on their surfaces, indicating that the defect in expression of Fas antigen was specific to leukemic cells (Fig 1, case no. 2). The clinical findings and history of this case were summarized in the Materials and Methods. The ATL cells stored in liquid nitrogen when the patient was first diagnosed as having chronic ATL were examined by flow cytometry. Fas antigen on ATL cells was already negative at this chronic phase. Anticancer drugs had little effect on the number of ATL cells in this case.
In another case, the expression of Fas antigen on ATL cells, which were derived from a tumor in the breast, was markedly decreased when compared with that on neutrophils (Fig 1, case no. 3).
Apoptosis of Fas-negative ATL cells.
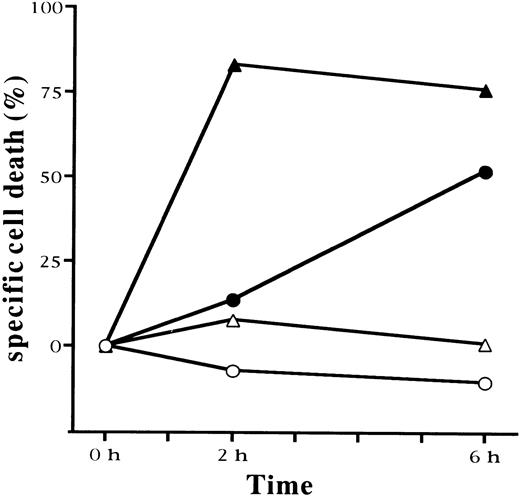
Apoptosis of ATL cells was reported to be induced by the addition of anti-Fas antibody. We analyzed whether apoptosis could be induced in Fas-negative and Fas-positive ATL cells by anti-Fas antibody and adriamycin using the uptake of propidium iodide. As shown in Fig 2, apoptosis was strongly induced in Fas-positive ATL cells by anti-Fas antibody. Most cells underwent apoptosis within 2 hours. On the other hand, the antibody could not induce apoptosis in Fas-negative ATL cells, confirming that Fas antigen was not expressed on these ATL cells and that signaling via Fas antigen was not functional in these cells. Adriamycin can also induce apoptosis of various cells, and the Fas-negative phenotype has been reported to be associated with drug resistance in vitro.37 Therefore, we analyzed apoptosis of Fas-positive and Fas-negative ATL cells induced by adriamycin. In Fas-positive ATL cells, apoptosis could be induced by adriamycin (4 μmol/L) within 6 hours; however, it had no effect on Fas-negative ATL cells. Thus, Fas-negative ATL cells were resistant to not only Fas-mediated apoptosis, but also adriamycin-induced apoptosis. To confirm that apoptosis had occurred, we also studied DNA ladder formation in these cells (data not shown).
Apoptosis of Fas-positive and Fas-negative ATL cells induced by monoclonal antibody against Fas antigen and adriamycin. Fas-positive (•, ▴) and Fas-negative (○, ▵) ATL cells were cultured with antibody against Fas antigen (CH11; ▴, ▵) or adriamycin (4 μmol/L; •, ○). Apoptosis was detected by uptake of propidium iodide at 0, 2, and 6 hours after incubation. Specific cell death was calculated as described in the Materials and Methods.
Apoptosis of Fas-positive and Fas-negative ATL cells induced by monoclonal antibody against Fas antigen and adriamycin. Fas-positive (•, ▴) and Fas-negative (○, ▵) ATL cells were cultured with antibody against Fas antigen (CH11; ▴, ▵) or adriamycin (4 μmol/L; •, ○). Apoptosis was detected by uptake of propidium iodide at 0, 2, and 6 hours after incubation. Specific cell death was calculated as described in the Materials and Methods.
Because viable cells were not available, apoptosis induced by antibody or adriamycin could not be analyzed in the ATL cells of case no. 3, which showed decreased expression of Fas antigen.
Analysis of Fas genes in Fas-negative ATL cells.
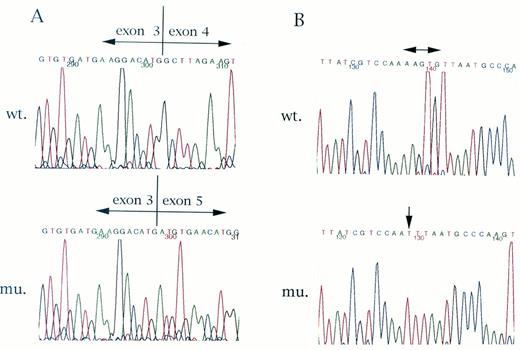
The complete defect in Fas antigen expression in case no. 2 prompted us to examine Fas gene transcripts. Reverse transcription-PCR (RT-PCR) detected transcripts of the Fas gene in case no. 2. The RT-PCR products of the whole Fas gene from case no. 2 were subcloned into plasmid DNA and a total of 11 clones were sequenced. The entire sequence of the Fas transcript was determined for each of the clones. As shown in Fig 3A, exon 4 was missing in 5 clones, resulting in premature termination. To clarify whether any mutations in the splicing junctions existed to generate aberrant transcript, we determined the genomic sequences and found no mutation around the splicing signals (data not shown). In the remaining 6 clones of case no. 2, a 5-bp deletion (AAGTG) and a 1-bp insertion (T) were found at exon 2 (Fig 3B), which again caused premature termination. These abnormalities caused the complete defect in expression of Fas antigens on ATL cells of case no. 2. On the other hand, these mutations were not present in an EBV-transformed B-cell line that was established from this case, as determined both by sequencing and by RNase protection assay (described below). This clearly showed that the mutations causing a defect in Fas antigen expression were specific to ATL cells.
Sequences of Fas gene cDNA clones derived from Fas-negative ATL cells. Sequences of Fas gene cDNA from Fas-negative ATL cells were determined as described in the Materials and Methods. In the clones sequenced, four clones lacked exon 4 (A). The other five clones showed a 5-bp deletion and a 1-bp insertion in exon 2 (B). Both mutations caused premature termination of Fas gene translation.
Sequences of Fas gene cDNA clones derived from Fas-negative ATL cells. Sequences of Fas gene cDNA from Fas-negative ATL cells were determined as described in the Materials and Methods. In the clones sequenced, four clones lacked exon 4 (A). The other five clones showed a 5-bp deletion and a 1-bp insertion in exon 2 (B). Both mutations caused premature termination of Fas gene translation.
In case no. 3, semiquantitative RT-PCR (30 cycles of amplification) showed a decreased level of Fas gene transcripts, suggesting that decreased transcription was the cause of decreased expression of Fas antigens on the surface (data not shown). Southern blot analysis using a Fas gene probe showed no difference between the genomic DNA of ATL cells and that of neutrophils from the same patient (data not shown), demonstrating that there was no rearrangement to interrupt the gene.
Detection of Fas gene mutations by RNase protection assay.
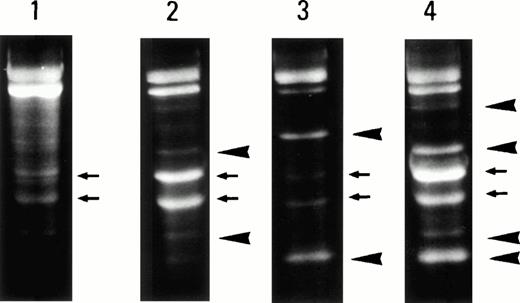
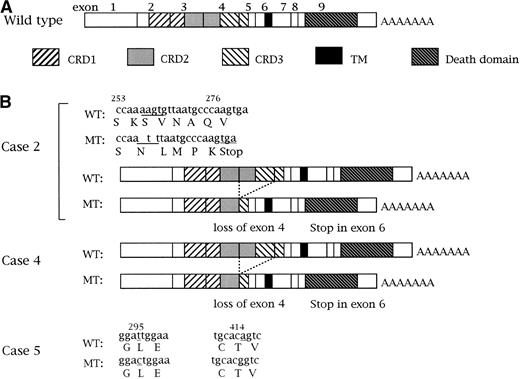
The mutation of both Fas gene alleles identified in case no. 2 suggested that mutation of a single allele might be frequent in ATL cells. Therefore, we analyzed RNA samples from 34 cases of Fas-positive ATL using an RNase protection assay. Because this assay can detect mutations even in genes that are more than 1 kb in length, whole Fas genes can be analyzed with this assay. The typical pattern obtained in an RNase protection assay is shown in Fig4. In normal PBMCs, three different bands were observed (Fig 4, lane 1), one of which represents the intact Fas gene transcript and two of which correspond to the spliced form of the Fas gene identified previously.38 This spliced form encodes the soluble form of the Fas antigen. In case no. 2, four additional bands could be detected (lane 4), which were derived from two mutations as described above. Of 34 cases, mutations could be detected in two cases in addition to case no. 2 (Fig 4, lanes 2 and 3). Sequencing experiments showed aberrant transcripts, which lacked exon 4, in 1 case (case no. 4; lane 2), as identified in case no. 2, and silent mutations in position 295 and 414 were found in the other case (case no. 5; lane 3; Fig 5), one of which has been described previously.39 It is important to note that the results obtained from an RNase protection assay could underestimate the frequency of Fas gene mutations, because the sensitivity of this assay is not 100%.
RNase protection assay of Fas gene transcripts. The reaction mixtures were digested with ribonuclease and electrophoresed in a 2.5% agarose gel. In normal PBMCs, the intact and spliced Fas gene transcripts (small arrowheads) were detected (lane 1). In cases no. 4 and 5 (lanes 2 and 3, respectively), additional bands (big arrowheads) could be found. In the Fas-negative ATL case, multiple bands were identified (lane 4, case no. 2), two of which corresponded to bands in case no. 4.
RNase protection assay of Fas gene transcripts. The reaction mixtures were digested with ribonuclease and electrophoresed in a 2.5% agarose gel. In normal PBMCs, the intact and spliced Fas gene transcripts (small arrowheads) were detected (lane 1). In cases no. 4 and 5 (lanes 2 and 3, respectively), additional bands (big arrowheads) could be found. In the Fas-negative ATL case, multiple bands were identified (lane 4, case no. 2), two of which corresponded to bands in case no. 4.
Abnormalities of the Fas gene in ATL cells. (A) Structure of the human Fas gene. The three cysteine-rich domains (CRDs), transmembrane domain (TM), and death domain are shown. (B) Mutations of the Fas genes in cases no. 2, 4, and 5. Detected Fas gene mutations are shown.
Abnormalities of the Fas gene in ATL cells. (A) Structure of the human Fas gene. The three cysteine-rich domains (CRDs), transmembrane domain (TM), and death domain are shown. (B) Mutations of the Fas genes in cases no. 2, 4, and 5. Detected Fas gene mutations are shown.
In case no. 4, both intact and truncated (without exon 4) Fas gene transcripts could be detected. It is interesting that case no. 4 was again a case of chronic ATL, similar to case no. 2. Because viable cells were not available in this case, we could not study apoptosis in this case.
To study whether mutation of the Fas gene is specific to ATL cells in case no. 2, Fas gene transcripts from an EBV-transformed B-cell line were analyzed using an RNase protection assay. It detected no mutations in Fas gene transcript, providing that mutation of the Fas gene was associated with leukemia. Furthermore, despite extensive analysis of normal tissues, we were unable to find aberrantly spliced from Fas transcript (missing exon 4), indicating that this aberrant transcript was pathologically generated.40
DISCUSSION
In this report, we described defects in expression of Fas antigen on ATL cells and the underlying mutations in the Fas genes of these cells. Fas gene mutations were also found in Fas-expressing ATL cells. Although only 1 case of 47 in this study showed a complete defect in expression of Fas antigen, 2 cases with defects in Fas antigen expression were reported in 33 ATL cases examined in another study.41 This fact indicates that loss of expression is not an accidental event, but occurs at a significant (low but consistent) frequency (∼2% or 6%).
Fas and Fas ligand play critical roles in the apoptosis of lymphoid cells. This is important for the negative selection of autoreactive T cells in the periphery and the activation-induced cell death of T lymphocytes. ATL is a malignant proliferation of peripheral T lymphocytes, cells in which apoptosis, Fas, and Fas ligand play critical roles. Mutation of the Fas gene has a dominant negative effect as reported for a congenital defect of Fas gene in humans; this suggests that ATL cells with one intact and one affected Fas allele may have a deregulation of apoptosis. Therefore, the inactivation of single Fas alleles in ATL reported here may be associated with the deregulated apoptosis of ATL cells, leading to disease progression. Family members of patients with Fas gene mutations were reported to have a history of Hodgkin's disease, which suggests that the Fas gene may function as a tumor-suppressor gene.30 Our studies in ATL provide further evidence for the Fas gene acting as a tumor-suppressor gene.
Rearrangement or allelic loss of Fas genes was also reported in 5 cases (rearrangement in 2 cases and allelic loss in 3 cases) of 70 non-Hodgkin's lymphoma cases.42 Recently, mutations of Fas genes were also reported in patients with multiple myeloma.43 Although functional analysis of the apoptosis of these lymphoma cells and myeloma cells has not been performed, these reports, combined with the present study, indicate that Fas gene abnormalities are consistently detected in lymphoid malignancies, suggesting a possible relationship between Fas mutations and disease progression. Our study showed the functional importance of Fas gene mutation in lymphoid malignancy.
We previously reported that ATL cells in some cases recognized autoantigens presented by autologous T- or B-cell lines, which suggested that ATL cells in these cases were derived from autoreactive T cells.33 Apoptosis of autoreactive T cells is mainly controlled by the Fas-Fas ligand system, and its deregulation may lead to uncontrolled growth. In the immune response, autoreactive T lymphocytes are generated, but they are eliminated by clonal deletion. Tax has been shown to inhibit apoptosis.44 If HTLV-I infects such autoreactive T lymphocytes, Tax could inhibit apoptosis, leading to escape from clonal deletion. Because constitutive expression of Tax is a disadvantage for proliferation of cells due to immune surveillance, mutation of genes associated with apoptosis might be an alternative mechanism leading to malignant proliferation. Although only 2 of 36 cases had mutations, there might be more abnormalities in other genes associated with apoptosis such as the DR3, 4, or Fas ligand genes. Indeed, Fas ligand gene transcripts could not be detected in ATL cells and could not be induced by stimulation with phorbol myristate acetate and concanavalin A in all ATL cases examined (manuscript in preparation). Inability to induce the expression of Fas ligand mRNA might be another, more common underlying abnormality of the Fas-Fas ligand system in ATL.
Adriamycin was reported to induce the expression of Fas ligand, resulting in induction of apoptosis; thus, the Fas and Fas ligand system may be associated with drug-induced apoptosis.37Impairment of Fas antigen expression in human cancer cell lines was reported to be associated with drug resistance in vitro.45,46 However, a dissociation between resistance to anticancer drugs and that to Fas-mediated apoptosis was also reported.47 Thus, it is controversial whether the Fas and Fas ligand system is directly involved in drug resistance. However, in our case no. 2, a loss of expression of Fas antigen was associated with unusually strong drug resistance in vivo and in vitro, because anticancer drugs had little effect on the number of ATL cells in vivo and in vitro. This observation is also consistent with reports that drug-resistant cell lines, which were selected in vitro, have reduced expression of Fas antigen.45 46 Further studies are needed to clarify the relationship between drug resistance and the Fas-Fas ligand system.
In case no. 3, the expression of Fas antigen was remarkably decreased. Because viable cells were not available in this case, apoptosis caused by antibody against Fas antigen could not be studied. However, an adriamycin-resistant myeloma cell line showed a similar decrease in expression of Fas antigen, and the reduced expression occurred at the level of transcription.46 Decreased expression of Fas antigen was also shown to be caused by a low level of transcription in case no. 3. It is possible that decreased surface expression of Fas antigen in case no. 3 is also associated with resistance to apoptosis and anticancer drugs.
It is interesting that 2 cases (cases no. 2 and 4) with Fas gene mutations were chronic ATL at first. Mutation of Fas genes may have inhibited apoptosis without promoting the growth of leukemic cells. Mutations of tumor-suppressor genes such as p16 or p53 were reported in acute and lymphoma-type ATL but not chronic or smoldering ATL, which indicated that those mutations were associated with the progression of ATL. p16 and p53 suppress the cell cycle, and their inactivation leads to uncontrolled progression of the cell cycle. On the other hand, inactivation of the Fas gene is associated with a defect of apoptosis. The different clinical subtypes associated with the inactivation of these tumor-suppressor genes may reflect the roles and functions of these genes: inhibition of apoptosis leads to long survival of affected cells, and inactivation of a cell cycle inhibitor contributes to uncontrolled proliferation.
Aberrant transcripts without exon 2 and 3 and little or no intact IRF-1 mRNA were reported in bone marrow and PBMCs from patients with myelodysplastic syndrome.48 As in our case, no mutations could be found within exons and splicing junctions of IRF-1 genes. This aberrant IRF-1 transcript generated an abnormal protein without a transcriptional activation domain. Although the exact mechanism causing this aberrant splicing remains to be identified, it is thought to be one mechanism to inactivate tumor-suppressor genes. The fact that aberrant transcripts without exon 4 was found in 2 cases in this study suggests that this is not a rare phenomenon, but occurs like in the IRF-1 gene. The loss of exon 4 caused premature termination, resulting in loss of Fas antigen expression, whereas the splicing out of exon 6, which was observed in normal tissues, can produce a soluble form of Fas antigen.38 40
The mutation of Fas genes described here indicates that abnormalities of the Fas gene are associated with progression of the disease and drug resistance. Further studies of other genes associated with apoptosis should clarify the significance of apoptosis in the leukemogenesis of ATL and other lymphoid neoplasms.
ACKNOWLEDGMENT
The authors are grateful to Dr Linda Kingsbury for critical reading of the manuscript.
Supported by a grant-in-aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan. M.M. received support from the Okukubo Memorial Fund for Medical Research at Kumamoto University School of Medicine and the Sagawa Foundation for Cancer Research.
Address reprint requests to Masao Matsuoka, MD, The Second Department of Internal Medicine, Kumamoto University School of Medicine, Honjo 1-1-1, Kumamoto 860, Japan.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal