To the Editor:
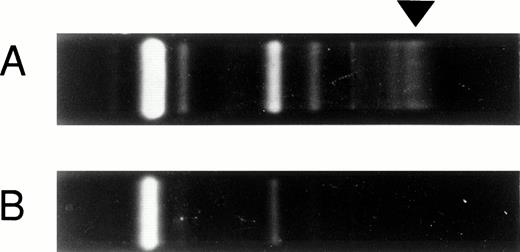
There have been few reports on immune-mediated neurological disturbances and none on solitary occurrence of optic neuritis after bone marrow transplantation (BMT). We experienced a very rare case of immune-mediated optic neuritis as one symptom of graft-versus-host disease (GVHD). A 34-year-old man with chronic myelogenous leukemia in accelerated phase received BMT from a human leukocyte antigen (HLA)-matched unrelated donor. Their histocompatibility antigens included DR2, which is often associated with multiple sclerosis. GVHD prophylaxis was performed with cyclosporine and short-term methotrexate. Grade I acute GVHD developed on day 10 and resolved with daily administration of cyclosporine. On day 71, he suddenly developed bilateral visual disturbance accompanied by severe bilateral ocular pain, which progressed rapidly to total blindness in a day. Significant bilateral papilledema was noted by ophthalmoscopic examination. Computed tomographic scan and magnetic resonance imaging of the brain revealed no abnormal organic findings. Other neurological deficits were not detected, except for decreased light reflexes in both eyes. Cerebrospinal fluid analysis revealed 24 cells/μL (predominantly matured lymphocytes) with 77 mg/dL of protein, 69 mg/dL of glucose, 3 mg/mL of IgG with positive oligoclonal bands (Fig1A), and 9.1 ng/mL (normal, 0 to 4 ng/mL) of myelin basic protein. Bacteriological and virological culture studies of the cerebrospinal fluid were both negative. Polymerase chain reaction study of human herpesvirus 6 (HHV-6) DNA in serum and cerebrospinal fluid was also negative. These findings suggested that his visual disturbance was induced by demyelinating optic neuritis and the abnormality only affected the optic nerve. No other laboratory data suggested viral infection, autoimmune disease, or other organ dysfunction. He was treated with intravenous methylprednisolone (1 g per day) for 3 days,1 followed by intravenous prednisolone (60 mg per day) with discontinuation of cyclosporine. After two courses of the corticosteroid therapy, cyclosporine was resumed while tapering the prednisone with gradual improvement of his vision. Six months after the attack his vision returned almost to the pretransplant level. There has been neither recurrence of optic neuritis nor any other abnormal neurological findings, including the character of cerebrospinal fluid (Fig 1B). Although a few cases of immune-mediated central nervous system disease after BMT have been reported in animals2 and humans,3 it is still controversial whether GVHD really affects the central nervous system.4 Recently, association of HHV-6 with multiple sclerosis has been reported,5 so we studied HHV-6 DNA in serum and cerebrospinal fluid. In our case, however, HHV-6 DNA was negative. Our case, showing resolution of the visual symptoms by immunosuppressive therapy, strongly suggested that an immunological disturbance appearing after unrelated BMT was involved in the pathogenesis of the neurological deficits. Prompt use of corticosteroid would be advisable for the resolution of the neurological deficits.
Positive oligoclonal bands (arrow) on day 72 (A) and the disappearance of the bands after the two courses of corticosteroid therapy on day 91 (B).
Positive oligoclonal bands (arrow) on day 72 (A) and the disappearance of the bands after the two courses of corticosteroid therapy on day 91 (B).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal