Interferon-α (IFN-α) is considered the standard therapy for chronic myeloid leukemia (CML) patients not suitable for allogeneic stem cell transplantation. From 1987 through 1992, 195 patients in the Benelux with recent untreated CML were randomized between low-dose IFN-α2b (3 MIU, 5 days/wk) or hydroxyurea alone (control group). The white blood cell count had to be kept less than 10 × 109/L in both arms; to this end, the IFN group received additional hydroxyurea, if necessary. The complete hematologic responses at 6 months in the IFN group were 62%, versus 38% in the control group. In the IFN group, a complete hematologic response at 6 months predicted a better survival (P = .001), but such a tendency was also seen in the control group (P = .07). Cytogenetic responses in the IFN group yielded 9% complete responders, 7% partial responders (<35% Ph+), and 24% minor responders (36% to 95% Ph+). The quality of cytogenetic response within the first 24 months was highly predictive for survival (P = .002). Twenty-four patients discontinued IFN-α because of side effects, but they did this at a long median interval of 17.6 months; the remaining patients did not require dose adaptations. Although the hematologic and cytogenetic responses in the IFN group were higher than in the control group, the duration of chronic phase from randomization was not statistically different with 53 and 44 months in the IFN and control group, respectively. Also, no advantage for survival calculated from diagnosis was seen for the IFN group (median, 64 months) compared with the control group (median, 68 months).
FOR MANY DECADES, the median survival of patients with chronic myeloid leukemia (CML) treated with chemotherapy ranged from 30 to 72 months, and prognostic factors as measured by the Sokal score were the most important parameters delineating the prognosis.1 Recently, it was convincingly demonstrated that hydroxyurea therapy results in a longer survival than busulfan.2 Therapy with IFN-α not only results in control of the disease, but in a considerable number of patients with early stage CML also in a decrease of the percentage of Philadelphia-positive (Ph+) metaphases, leading to complete cytogenetic conversion in a minority of these patients.3-6 Randomized studies from Italy,7 Japan,8 and the United Kingdom9 showed a survival advantage in favor of interferon-α (IFN-α). However, because the Japanese used busulfan as a control, a comparison with IFN-α is inequitable. Further analysis of the British MRC III showed that the survival advantage of IFN-α compared with chemotherapy decreased when the busulfan-treated patients were removed from the control group. Although a trend for better survival of the IFN-group versus the hydroxyurea-treated patients persisted, this was not significant anymore.10Also, the German CML I study trialists reported a lack of survival advantage for IFN-α compared with hydroxyurea.11
In 1987, the CML Benelux Study Group initiated a multicenter randomized trial comparing recombinant IFN-α2b + hydroxyurea versus hydroxyurea alone. Because the optimal dose of IFN-α was not known, IFN-α2b was used at a total dose of 15 MIU/wk. It was assumed that such a low dose would give less toxicity and, if combined with hydroxyurea, equally good results. After an accrual of 200 patients, the study was closed in January 1993. All results were updated until March 1996.
PATIENTS AND METHODS
Inclusion criteria.
Previously untreated patients with newly diagnosed Ph+ CML in chronic phase (age ≥18 years) were included. Patients with cytogenetic abnormalities other than loss of chromosome y, or <10% of either +8, i(22q−), or a second 22q− were excluded. Patients who did not show the presence of the Ph chromosome could be included if by Southern blot analysis or by reverse transcription-polymerase chain reaction (RT-PCR) the rearrangement of BCR/ABL was demonstrated. A good World Health Organization performance status (0, 1, or 2), adequate hepatic and renal function as defined by bilirubin and creatinine levels below twice the upper limit of normal, and informed consent were required.
Study design.
Upon entry, patients received hydroxyurea to reduce the white blood cell count (WBC) to 10 to 20 × 109/L and to obtain a stabilization phase of 3 weeks during which the WBC had to be kept between 5 and 15 × 109/L. None of the patients left the study during this phase. Next, patients were randomized between 2 arms: arm A (IFN group): IFN-α2b (Intron A; Schering Plough, Kenilworth, NJ) at a total dose of 3 MIU (not corrected for body surface), 5 days a week with, if necessary, additional hydroxyurea; arm B (control group): hydroxyurea alone. In both groups, the WBC had to be kept below 10 × 109/L for as long as possible. During follow-up, the doses of IFN-α and hydroxyurea were recorded. When acceleration or blast crisis occurred, other cytostatic drugs were added, the dose of IFN-α was increased or a bone marrow transplantation (BMT) was performed, the patients went off protocol treatment, but remained under follow-up for events. Case report forms were filled in during the first 3 months at a monthly base and then at 3-month intervals until death or until a patient went off protocol. For all patients, the date of BMT and the date of acceleration, blast crisis, and death (including cause of death) were recorded. At 3-month intervals, hematologic responses were registered and verified. In the absence of data on spleen size and/or a differential, no complete hematologic response could be scored. At 6-month intervals, a bone marrow aspirate and cytogenetic analysis had to be performed.
Hematologic responses.12
A complete hematological remission was defined as WBC less than 10 × 109/L, with a normal differential with no more than 1% circulating immature cells (only if consisting of metamyelocytes), and the disappearance of all clinical symptoms related to CML activity including palpable splenomegaly. A partial hematological remission was defined as WBC of 10 to 20 × 109/L, or normal WBC but with greater than 1% circulating immature cells (blasts, promyelocytes, myelocytes, or metamyelocytes), or palpable splenomegaly, or the presence of other signs of disease. A failure was defined as WBC greater than 20 × 109/L.
Cytogenetic analysis.
At least 30 metaphases had to be analyzed obtained from bone marrow aspirates. Analysis of peripheral blood was only acceptable for the assessment of the initial diagnosis. If 10 or less metaphases had been analyzed, the data were not used unless they fitted in a pattern obtained from the previous and subsequent tests. If 5 or less metaphases had been analyzed, the data were skipped for final analysis. If only 1 normal metaphase among the remaining Ph+metaphases was observed, this was not interpreted as a cytogenetic response. In 2 Ph−/BCR+ patients, the cytogenetic response was assessed with help of the fluorescence in situ hybridization (FISH) technique on metaphases and by Southern blot analysis (not quantitative). For the Dutch patients, cytogenetic analysis was centrally performed by Prof Dr A.M. Hagemeijer (Rotterdam, The Netherlands), who also reviewed the final results. The large majority of the Belgian patients were analyzed in Leuven (Prof Dr H. Van den Berghe, Leuven, Belgium). A complete cytogenetic response was defined as Ph present in none of the metaphases. A partial cytogenetic response was defined as Ph present in 1% to 35% of the metaphases. A minimal cytogenetic response was defined as Ph present in 36% to 94% of the metaphases. No cytogenetic response was defined as Ph present in greater than 95% of the metaphases or greater than 90% if 10 or less metaphases could be analyzed.
Statistics.
The sample size was based on the requirement to detect a 20% improvement from 50% to 70% for a 3-year median freedom from progression period (acceleration or blastic crisis1), measured from randomization. At least 83 patients were needed in each arm to detect this 20% improvement (level of significance, .05, one-sided; power, 0.80). All analyses were performed following the intention to treat principle and included all patients regardless of the type or time of any protocol violation. Patient data at entry were compared using the χ2 test and the nonparametric Mann-Whitney test. Kaplan Meier curves and the log-rank test with a trend analysis if appropriate were used to compare the survival and duration of chronic phase (freedom from progression) in different subgroups. Because of the delay between CML diagnosis at entry and date of randomization, time to event analyses were performed for both the date of diagnosis and the date of randomization to enable comparison with other published randomized studies in which both start dates were overlapping. Time to event analyses were performed both with and without censoring for the date of BMT (but only if performed in chronic phase). Landmark analyses13 were performed to study the prognostic effect of hematologic response, cytogenetic response, and WBC values after randomization on survival. To evaluate the possible benefit of a complete hematologic response, the hematologic response at 6 months after randomization was related to the survival starting at 6 months after randomization. The best cytogenetic response in the first 24 months after randomization was calculated and related to survival starting at 24 months after randomization. The prognostic role of stable WBC control was studied by calculating the mean WBC count (beginning at day +30) for all patients with 6 or more WBC analyses in this first year. These mean WBC counts were divided into three categories (mean WBC <6, 6 to 10, and >10 × 109/L) and related to the survival starting at 1 year after randomization.
RESULTS
Patient characteristics.
Seventy-two different hospitals from Belgium, The Netherlands and Luxembourg contributed patients to this study between December 1, 1987 and December 31, 1992 (see Addendum). From 200 patients entered in the study, 5 patients were considered ineligible: 1 patient was at start in blastic phase; from 4 patients insufficient data were available. The remaining 195 were well balanced in both study arms, except for a marginally significant (P = .05) difference in the WBC counts at start (Table 1). Both arms showed a high median age (56 years) and a low percentage (30%) of patients in the favorable subgroup according to the Sokal score (<0.8)14(Table 1). During revision, it appeared that 7 patients (4 in arm A and 3 in arm B) had initial high (10% to 20%) percentages of circulating blasts, with at the same time less than 6% blasts in the bone marrow. All were kept in the study. The time interval between CML diagnosis at entry in the study followed by the stabilization phase with hydroxyurea and randomization ranged from 0 to 10 months, with a median of 86 days for patients in the IFN arm (in parallel with initial higher WBC counts) and 70 days in the control arm. All results were updated until March 31, 1996. The median observation time of all patients from randomization on was 51 months, and for the living patients was 66 months.
Entry Characteristics of Both Patient Groups
| . | IFN Arm (n = 100)-150 . | Control Arm (n = 95)-150 . | P Value . |
|---|---|---|---|
| Age (yr) | 55.7 (20-83) | 56.4 (27-84) | NS |
| Female/male | 42/58 | 42/53 | NS |
| Spleen palpable (n) | 61 | 62 | NS |
| If yes, median in cm below lcm | 5 (1-19) | 7 (1-20) | NS |
| Hb (g/dL) | 11.8 (6.1-15.9) | 12.2 (5.5-22.5) | NS |
| WBC (×109/L) | 149 (11-451) | 105 (16-430) | P = .045 |
| Absolute no. of basophils (×109/L) | 4.14 (0-44.7) | 3.06 (0-25.9) | NS |
| Absolute no. of eosinophils (×109/L) | 2.41 (0-45.8) | 1.72 (0-29.7) | NS |
| Absolute no. of blasts (×109/L) | 2.60 (0-64.9) | 1.31 (0-37.7) | NS |
| Platelets (×109/L) | 371 (120-1,719) | 388 (76-2,816) | NS |
| Sokal score <0.8 | 29% | 30% | NS |
| Sokal score 0.8-1.2 | 43% | 33% | NS |
| Sokal score >1.2 | 28% | 37% | NS |
| . | IFN Arm (n = 100)-150 . | Control Arm (n = 95)-150 . | P Value . |
|---|---|---|---|
| Age (yr) | 55.7 (20-83) | 56.4 (27-84) | NS |
| Female/male | 42/58 | 42/53 | NS |
| Spleen palpable (n) | 61 | 62 | NS |
| If yes, median in cm below lcm | 5 (1-19) | 7 (1-20) | NS |
| Hb (g/dL) | 11.8 (6.1-15.9) | 12.2 (5.5-22.5) | NS |
| WBC (×109/L) | 149 (11-451) | 105 (16-430) | P = .045 |
| Absolute no. of basophils (×109/L) | 4.14 (0-44.7) | 3.06 (0-25.9) | NS |
| Absolute no. of eosinophils (×109/L) | 2.41 (0-45.8) | 1.72 (0-29.7) | NS |
| Absolute no. of blasts (×109/L) | 2.60 (0-64.9) | 1.31 (0-37.7) | NS |
| Platelets (×109/L) | 371 (120-1,719) | 388 (76-2,816) | NS |
| Sokal score <0.8 | 29% | 30% | NS |
| Sokal score 0.8-1.2 | 43% | 33% | NS |
| Sokal score >1.2 | 28% | 37% | NS |
Abbreviation: NS, not significant.
Median values, with ranges in parentheses.
Adherence to the protocol and drug doses.
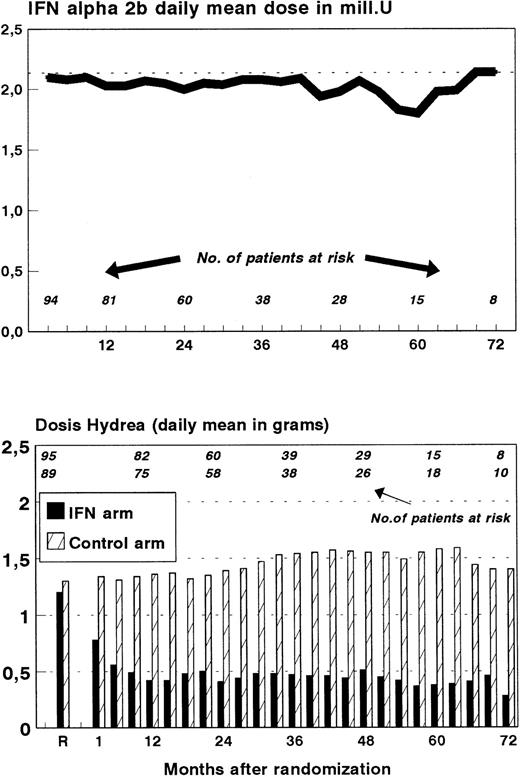
After 93 months, 168 patients had discontinued the protocol treatment. The median time of going off protocol was 25 months (range, 0 to 93 months). Reasons for going off protocol were progressive disease, adverse reactions (see below), intercurrent other diseases, BMT in chronic phase, refusal (which usually meant that the patient preferred and received the therapy from the other treatment arm), and protocol violations (Table 2). Twenty-four patients (25%) left the study because of IFN-related side effects at a median of 17.6 months after randomization (mean, 27 months; range, 1 to 93 months). The patients who remained in the study could tolerate almost the full prescribed dose, recalculated as 2.14 MIU/d. Figure 1 shows the mean doses of IFN-α2b and hydroxyurea used in both groups. The reasons for going off protocol because of adverse reactions in the IFN group were severe fatigue and flu-like symptoms (n = 7), neuropsychiatric (n = 6), renal including vasculitis (n = 4), cutaneous related to injection sites (n = 3), and other (n = 4). Adverse reactions in the control group consisted of hydroxyurea-related fever in 2 cases and drug eruption and vasculitis in 1 each. Of the 10 control patients who received IFN-α after they went off protocol, 6 began within 1 year of randomization.
Reasons for Ending Protocol Treatment
| . | IFN Arm (n = 85) . | Control Arm (n = 83) . |
|---|---|---|
| Acceleration or blast crisis | 37 | 52 |
| Adverse reactions | 24 | 4 |
| Intercurrent other diseases | 6 | 6 |
| BMT in chronic phase | 16 | 7 |
| Refusal | 1 | 10 |
| Protocol violations | 1 | 4 |
| . | IFN Arm (n = 85) . | Control Arm (n = 83) . |
|---|---|---|
| Acceleration or blast crisis | 37 | 52 |
| Adverse reactions | 24 | 4 |
| Intercurrent other diseases | 6 | 6 |
| BMT in chronic phase | 16 | 7 |
| Refusal | 1 | 10 |
| Protocol violations | 1 | 4 |
(Lower part) Dosages of hydroxyurea in both treatment arms during follow-up. Patients at risk are indicated. (Upper part) Dosage of IFN-α2b during follow-up. Patients at risk are indicated.
(Lower part) Dosages of hydroxyurea in both treatment arms during follow-up. Patients at risk are indicated. (Upper part) Dosage of IFN-α2b during follow-up. Patients at risk are indicated.
Duration of chronic phase, type of blast crisis, and survival.
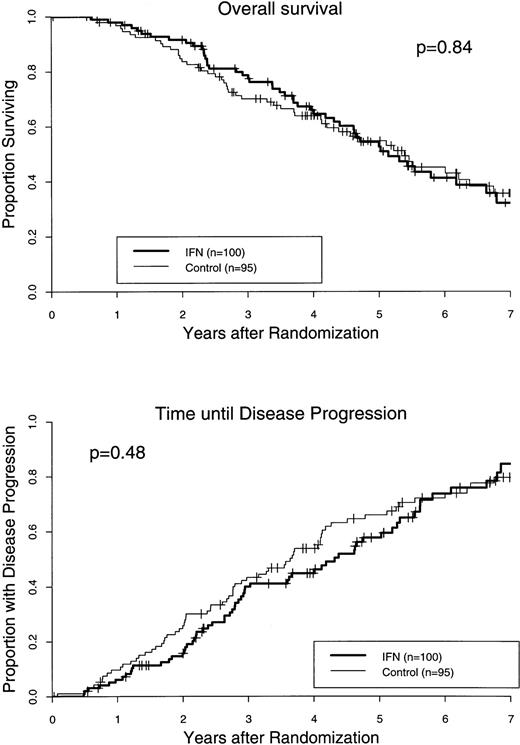
Analysis of duration of chronic phase for all patients, including those who went off protocol for reasons not related to disease progression, disclosed a median progression-free survival after randomization of 53 months for the IFN group and 44 months for the control group, being not statistically different (P = .48; Fig 2). Because more patients in the hydroxyurea arm went off protocol because of progressive disease, duration of survival after going off protocol was calculated in both groups. No significant difference in median survival was found for those patients going off protocol because of disease progression (IFN arm, 13.1 months; control arm, 9.1 months). No difference in type of blast crisis was observed. Analysis of all patients, including those who obtained a blast crisis after going off protocol, yielded a myeloid blast crisis in 77% (IFN arm) and 64% (control arm). At March 31, 1996, 111 patients have died due to either disease progression (IFN arm, n = 38; control arm, n = 41) or intercurrent diseases (in half of the cases BMT related, IFN arm, n = 19; control arm, n = 12). In 1 case (IFN arm), the cause of death was unknown. No difference in overall survival calculated from date of diagnosis or from randomization was seen for both treatment arms regardless of whether the results were censored for the date of BMT (Fig 2). The median overall survival from diagnosis without censoring for date of BMT was 63 months in the IFN arm and 68 months in the control arm. The results censored for date of BMT disclosed a median survival of 64 months (95% confidence interval, 52 to 75 months) for the IFN arm and 68 months (95% confidence interval, 54 to 82 months) for the hydroxyurea control arm. The same figures without censoring for date of BMT calculated from randomization onwards (note the large interval between diagnosis at entry and randomization in this particular study compared with other groups) showed a median survival of 61 months in the IFN group and 66 months in the control group. The 5-year survival from diagnosis was similar for both arms, ie, 55% (95% confidence interval, 44% to 66%).
Overall survival (upper part) and time to disease progression (lower part) of patients with CML treated with IFN-α2b or hydroxyurea only, calculated from date of randomization. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Overall survival (upper part) and time to disease progression (lower part) of patients with CML treated with IFN-α2b or hydroxyurea only, calculated from date of randomization. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Hematologic responses.
During follow-up, the WBC were kept below 10 × 109/L in both groups, although the WBC counts were persistently lower in the IFN arm (Fig 3). The percentages of complete hematologic responses assessed from 6 months of therapy on ranged from 50% to greater than 60% in the IFN arm, versus 20% to 50% in the control arm (Fig 3).
(Upper part) WBC counts during treatment. Patients at risk are indicated. (Lower part) Percentages of complete hematologic responses in both treatment arms during follow-up. Patients at risk are indicated.
(Upper part) WBC counts during treatment. Patients at risk are indicated. (Lower part) Percentages of complete hematologic responses in both treatment arms during follow-up. Patients at risk are indicated.
Cytogenetic responses.
The cytogenetic responses were calculated per individual patient (Table 3). For the majority, sufficient data were obtained to assess responses. The mean and median numbers of cytogenetic analyses were 4.4 and 4 per patient (including the initial analysis), with a mean and median number of metaphases analyzed of 22.5 and 20. No follow-up data were available from only 3 patients in the IFN arm and 9 in the control arm. In most of these missing cases, the patients went off protocol before the first cytogenetic analysis at 6 months had been performed. Overall, 40% of the IFN-treated patients, versus 11% in the control group, showed any response. In the IFN group, there were 9% complete and 7% partial responses; 24% of the patients obtained a minimal response. In the control group, 2 patients (2%) obtained a partial response and 8 patients (9%) a minimal response. Twenty patients of the evaluable patients group (16% in the IFN arm and 4% in the control arm) went off protocol within the first year because of early blast crisis or side effects and did not have an opportunity to develop any cytogenetic response. Of the responding patients in the IFN arm, 24 (57%) still used some hydroxyurea at the time of their first cytogenetic response. A fixed dose of IFN-α was used for all patients, resulting in a varying dose per square meter body surface, the latter ranging between 1.4 m2 and 2.3 m2. No relationship between cytogenetic response and IFN-α dose per square meter body surface was observed (data not shown).
Cytogenetic Responses
| . | IFN Arm (n = 100) . | Control Arm (n = 95) . |
|---|---|---|
| Evaluable patients | 97 | 86 |
| Early blast crisis | 5 (5%) | 2 (2%) |
| Early side effects | 11 (11%) | 2 (2%) |
| No response | 41 (42%) | 72 (84%) |
| Minimal response (35-95% Ph+) | 24 (25%) | 8 (9%) |
| Partial response (1-35% Ph+) | 7 (7%) | 2 (2%) |
| Complete response | 9 (9%) | 0 (0%) |
| Nonevaluable patients | 3 | 9 |
| Dry tap, Ph− | 1 | |
| No follow-up data | 3 | 8 |
| . | IFN Arm (n = 100) . | Control Arm (n = 95) . |
|---|---|---|
| Evaluable patients | 97 | 86 |
| Early blast crisis | 5 (5%) | 2 (2%) |
| Early side effects | 11 (11%) | 2 (2%) |
| No response | 41 (42%) | 72 (84%) |
| Minimal response (35-95% Ph+) | 24 (25%) | 8 (9%) |
| Partial response (1-35% Ph+) | 7 (7%) | 2 (2%) |
| Complete response | 9 (9%) | 0 (0%) |
| Nonevaluable patients | 3 | 9 |
| Dry tap, Ph− | 1 | |
| No follow-up data | 3 | 8 |
Prognostic factors.
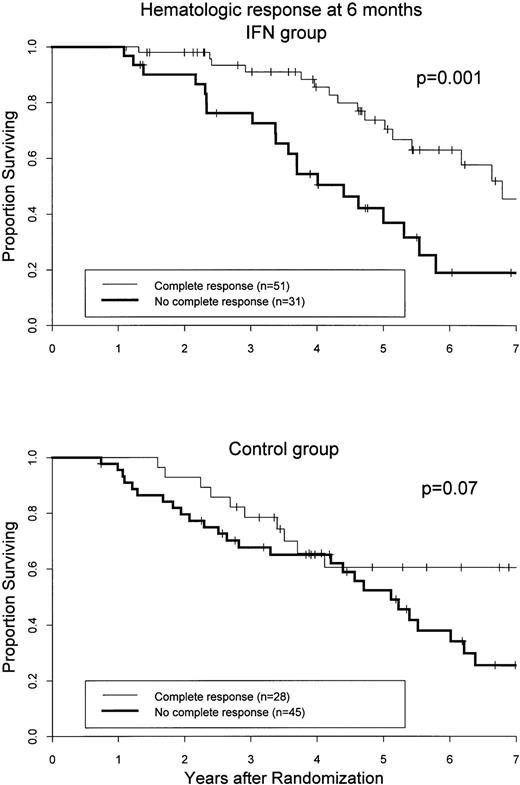
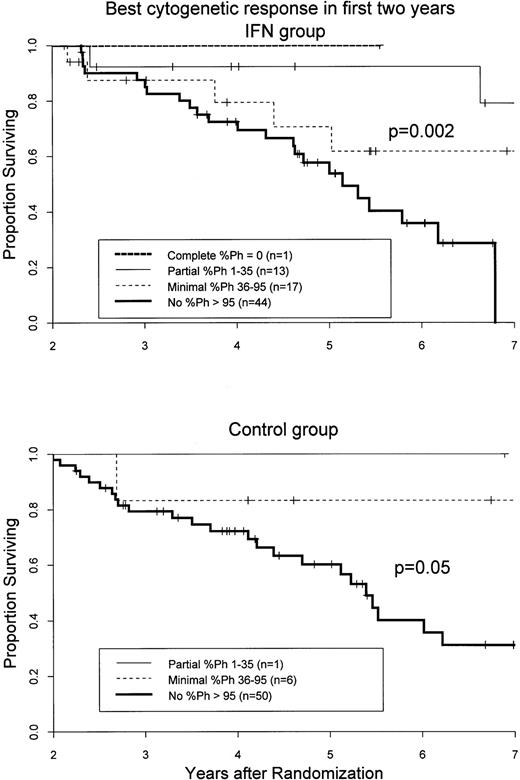
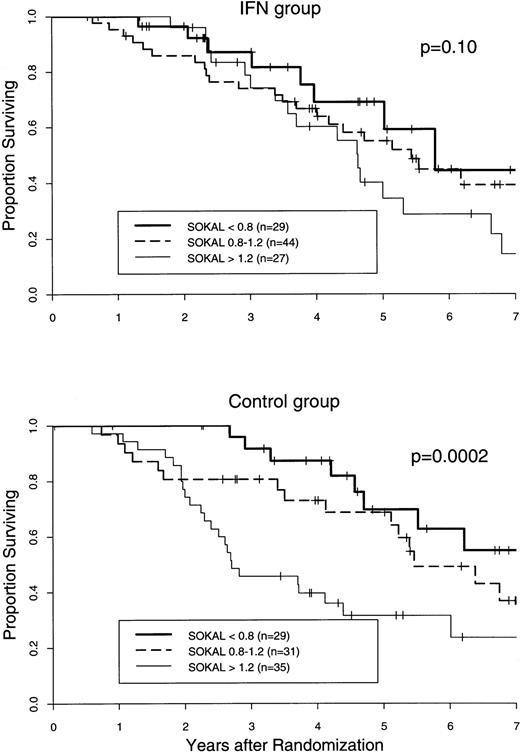
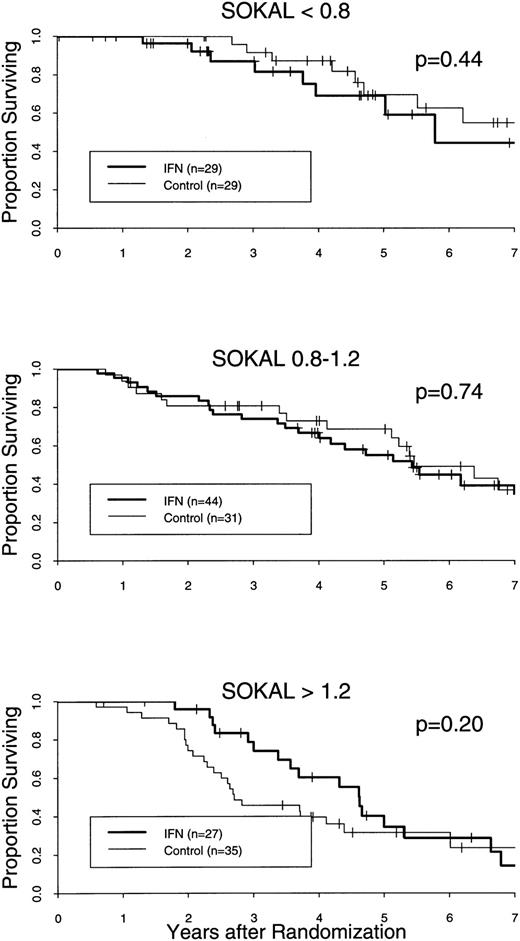
Survival in patients reaching a complete hematologic response at 6 months was significantly better for the IFN group (P = .001; Fig 4), with a trend for improvement in the control group (P = .07). In the landmark analysis, the quality of cytogenetic response within the first 24 months appeared highly predictive for survival (P = .002, test for trend; Fig 5). This was also the case for the few patients in the control group who obtained a minor or partial cytogenetic response (P = .05). Thus far, none of the patients with a complete cytogenetic response and only 2 from the partial cytogenetic responders have died. The median survival of the nonresponders in the landmark analysis, calculated from randomization, was 62 months for the IFN group (43 patients who had a follow-up of at least 24 months could be analyzed), versus 65 months for the control group (49 patients analyzed), which is not different. The Sokal score14 at entry was highly discriminative for survival for the hydroxyurea group (P = .0002, test for trend), but not for the IFN group (P = .10; Fig 6). When we analyzed the three prognostic groups (<0.8; 0.8-1.2; and >1.2) separately, IFN-α therapy showed a trend for better survival only for unfavorable patients (Sokal >1.2; log-rank P = .20; Breslow P = .03; Fig 7). This trend was significant when restricting the analysis to the first few years of follow-up (first 2 years: P = .05; 3 years: P = .009; 4 years: P = .05).
Prognostic value of obtaining a complete hematologic response at 6 months for both treatment groups. The numbers of patients from whom data were available to calculate the hematologic response at 6 months ±4 weeks after randomization are given. Survival is calculated after a landmark analysis at 6 months. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Prognostic value of obtaining a complete hematologic response at 6 months for both treatment groups. The numbers of patients from whom data were available to calculate the hematologic response at 6 months ±4 weeks after randomization are given. Survival is calculated after a landmark analysis at 6 months. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Prognostic value related to the quality of any cytogenetic response obtained within the first 24 months after randomization for both treatment groups. The numbers of patients from whom data were available are given. Survival is calculated after a landmark analysis of 24 months. Note that the axis starts at 2 years after randomization. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation. The numbers of cytogenetic responders in this figure relate to the response obtained only during the first 2 years, and they therefore differ from the numbers given in Table 3, in which all responders obtained at any time on protocol have been shown.
Prognostic value related to the quality of any cytogenetic response obtained within the first 24 months after randomization for both treatment groups. The numbers of patients from whom data were available are given. Survival is calculated after a landmark analysis of 24 months. Note that the axis starts at 2 years after randomization. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation. The numbers of cytogenetic responders in this figure relate to the response obtained only during the first 2 years, and they therefore differ from the numbers given in Table 3, in which all responders obtained at any time on protocol have been shown.
Survival curves of CML patients treated with IFN-α2b or hydroxyurea only, related to the Sokal prognostic score. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Survival curves of CML patients treated with IFN-α2b or hydroxyurea only, related to the Sokal prognostic score. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Survival curves of CML patients treated with IFN-α2b or hydroxyurea only, related to the Sokal prognostic score, and shown for the different prognostic groups separately. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation. Only for the group with an unfavorable risk profile (Sokal score >1.2) is a trend (log-rank, P = .20; Breslow, P = .03) for better survival seen in favor of IFN therapy.
Survival curves of CML patients treated with IFN-α2b or hydroxyurea only, related to the Sokal prognostic score, and shown for the different prognostic groups separately. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation. Only for the group with an unfavorable risk profile (Sokal score >1.2) is a trend (log-rank, P = .20; Breslow, P = .03) for better survival seen in favor of IFN therapy.
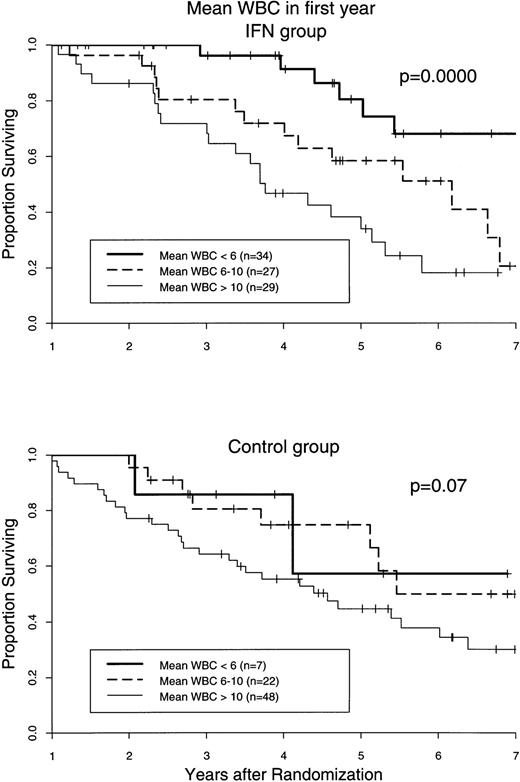
Finally, the possible impact on WBC control during the first year on survival was analyzed for both groups. To this end, we calculated the mean WBC score for all 173 patients from whom at least 6 analyses were available during the first year. To avoid the factor instability during the first weeks of IFN-α therapy, we started from day +30 after randomization. As shown in Fig 8, it appeared that, in the IFN arm, patients with a mean WBC below 6 × 109/L experienced the best survival, whereas mean WBC counts between 6 and 10 × 109/L gave an intermediate outcome and greater than 10 × 109/L gave an unfavorable outcome (P = .0000; test for trend). For the control arm, the results were less discriminative, but still showed a trend (P = .07) for better survival if the WBC counts had been below 10 × 109/L during the first year.
Survival curves from the first year on of CML patients treated with IFN-α2b or hydroxyurea only, related to WBC control during the first year of therapy. Only data from patients with 6 or more analyses during this period were used. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
Survival curves from the first year on of CML patients treated with IFN-α2b or hydroxyurea only, related to WBC control during the first year of therapy. Only data from patients with 6 or more analyses during this period were used. Curves are based on the intention to treat, regardless of any protocol violation or cause of death. Data on those patients that underwent BMT during chronic phase were censored as of the date of transplantation.
DISCUSSION
The data of this multicenter randomized study for newly diagnosed untreated CML patients treated with either low-dose IFN-α2b + hydroxyurea or hydroxyurea alone showed a progression-free period of 53 months for the IFN group and 44 months for the control group. However, this was not statistically different and neither was there a statistically significant difference in total survival time. Although the survival curves are overlapping, it is important to realize that the size of the Benelux study was relatively small. The Benelux results differ from those of the Italian Cooperative CML Group, who observed a statistically significant survival in favor of the IFN-treated patients, but are in agreement with those recently published by the German and updated British groups. Differences in the inclusion and exclusion criteria might explain some of the differences found. The Benelux study excluded patients with unfavorable cytogenetic characteristics or signs of accelerated disease at start, but had no upper age limit. The Italian study did not accept patients older than 70 years and patients with extramedullary manifestations or more than 10% circulating blasts at presentation. The German study, on the other hand, included all of these patients with unfavorable signs. For comparison, the survival results related to age, Sokal risk score, IFN dose, and cytogenetic responses of the three European CML studies randomizing between IFN and hydroxyurea,7,9,11 one multicenter study from the CALBG,15 and the IFN arm from the French study randomizing between IFN and IFN+ cytarabine (see below) are given in Table 4. The median age of the Benelux cohort is higher (56 years) than that of the other studies, which could have been disadvantageous given the fact that IFN is more effective in younger patients.16-18 Table4 further shows that the survival of the Benelux IFN-α arm, despite the low dose applied, was in line with the survival of the other IFN arms. The similar survival in the IFN arm is not unexpected given the fact that, despite the high median age group, the percentages of cytogenetic responses did not differ from those of the other randomized studies7-9,11 (Table 4). The fact that only 2 of the 16 responding patients have died also underlines the fact that partial and complete cytogenetic responses obtained on low doses of IFN-α have a similar impact on prognosis as those obtained on much higher doses. If the rule of thumb is applied that half of the sum of complete and partial cytogenetic responses will be found in the Sokal low group,16 we observed in the Benelux cohort the percentage of responses (16%) as expected (half of 29%). Whereas the other randomized studies used higher doses of IFN (Table 4), in the Benelux study a fixed low dose was used. Presumably, the combination of hydroxyurea and IFN-α will have contributed to the equally good cytogenetic responses found in our study. In more than half of the patients, both drugs were still used at the time of the first cytogenetic response. The recently published detailed comparative analysis of the Italian and German CML trials17 also suggests that the combination of IFN with hydroxyurea as needed is more effective than either agent alone. In the Italian trial, in which the addition of chemotherapy was allowed if believed to be necessary, 41% of the patients received hydroxyurea simultaneously in addition to IFN.17
Comparison of Survival Between Patients Treated in Five Randomized and One Nonrandomized Multicenter Studies Containing One Arm With IFN-α
| Group . | Median Age (yr) . | % Sokal High Risk . | % Partial + Complete Cytogenetic Responses in IFN Arm . | Aim of Daily IFN Dose at Start of Protocol . | IFN Arm Median Survival (mo) . | Hydroxyurea Arm Median Survival (mo) . |
|---|---|---|---|---|---|---|
| Italian Cooperative Study Group | 48 | 24% | 19% | 5 MIU/m2 | 72 (n = 218) | 52 (n = 104)3-150 |
| German CML Study Group | 47 | 37% | 6%3-151 | 5 MIU/m2 | 66 (n = 133) | 56 (n = 194) |
| MRC CML III, United Kingdom | 52 | 42% | 11% | 3-12 MIU | 64 (n = 152) | 52 (n = 152) |
| Benelux CML Study Group | 56 | 33% | 16% | 2.14 MIU | 64 (n = 100) | 68 (n = 95) |
| CALBG, United States | 44 | Not given | 16%3-152 | 5 MIU/m2 | 66 (n = 107) | |
| French CML Study Group | 51 | 18% | 24% | 5 MIU/m2 | Too early (n = 361) |
| Group . | Median Age (yr) . | % Sokal High Risk . | % Partial + Complete Cytogenetic Responses in IFN Arm . | Aim of Daily IFN Dose at Start of Protocol . | IFN Arm Median Survival (mo) . | Hydroxyurea Arm Median Survival (mo) . |
|---|---|---|---|---|---|---|
| Italian Cooperative Study Group | 48 | 24% | 19% | 5 MIU/m2 | 72 (n = 218) | 52 (n = 104)3-150 |
| German CML Study Group | 47 | 37% | 6%3-151 | 5 MIU/m2 | 66 (n = 133) | 56 (n = 194) |
| MRC CML III, United Kingdom | 52 | 42% | 11% | 3-12 MIU | 64 (n = 152) | 52 (n = 152) |
| Benelux CML Study Group | 56 | 33% | 16% | 2.14 MIU | 64 (n = 100) | 68 (n = 95) |
| CALBG, United States | 44 | Not given | 16%3-152 | 5 MIU/m2 | 66 (n = 107) | |
| French CML Study Group | 51 | 18% | 24% | 5 MIU/m2 | Too early (n = 361) |
All data from the Italian and Benelux group are censored for date of BMT.
Ten percent of the patients used busulfan.
Eight patients, consisting of 6 complete and 2 partial + minor responses.
Partial response was defined by the CALBG group as less than 50% Ph+ metaphases, whereas the other groups took less than 35% as cut-off level.
The Benelux study required the selection of early CML patients (diagnosed within less than 6 months) and then an induction period with strict WBC control during the 3 weeks before IFN treatment was to be started. In the early years of the study, not every physician was aware of the benefit of starting as soon as possible with IFN, which induced some delay in entry. Moreover, because some physicians meticulously adhered to this required 3-week stabilization phase and in cases with fluctuating WBC counts needed much more time, the interval between the time of CML diagnosis and initiation of IFN was sometimes rather long. This delay could have had influence on the outcome of this study, because it is widely accepted that the efficacy of IFN therapy decreases with the duration of the disease,16 17 whereas hydroxyurea remains helpful even at advanced stages.
The optimal dose of IFN-α to be used for CML is presently unknown. It is evident that dose is an important issue regarding the side effects and costs of IFN.15,19,20 Even if the side effects are considered minor, these can seriously interfere with the quality of life21 given the long duration of treatment required for a disease that of its own usually has only minor symptoms. The MD Anderson Cancer Center Group who pioneered the anti-CML efficacy underlines the importance of high-dosed schemes of at least 5 MIU/m2 or the maximally tolerated lower dose schedule.16 This group obviously obtained the best results with IFN-α up till now. However, given among others the fact that many patients had to be referred and commonly showed a favorable Sokal risk profile (>50% Sokal score of <0.8), some selection is inevitable. All multicenter studies observed a reduction of the initial aimed IFN dose during follow-up. The CALBG trial (a single-arm study with daily 5 MIU/m2) had to reduce the dose with greater than 10% in 64% of the patients and with greater than 50% reductions in 38% of the patients.15 The Italian study aiming at 5 MIU/m2 observed that actually a median dose of 4,28 MIU/m2 was used during the first 14 months. However, after 5 years, 50% of the IFN-assigned patients had discontinued their treatment. Moreover, the protocol allowed a marked dose reduction to daily a total of 1.3 MIU IFN for those patients who did not respond after 14 months.7 The British MRC study showed that the mean dose of IFN-α during the first year was 3.2 MIU (total, not per square meter); at 4 years, only 52% of the patients still used this drug.9 The German CML I study started with 5 MIU/m2 and succeeded to maintain this dose during the first 4 weeks. However, during the following 60 months, a decline to 2 MIU/m2 was seen.11 In the Benelux cohort, 25% of the patients had to stop IFN, although they did this after a rather long median time interval of 17.6 months; moreover, the remaining patients succeeded in continuation of the drug at the assigned dose of 2.14 MIU/d. Most certainly, patient compliance will improve if the toxicity can be reduced. Two new studies, one in The Netherlands (HOVON 20 study) and one in the United Kingdom (MRC-V), randomizing between the low Benelux dose of 15 MIU/wk and the dose considered by others to be the standard starting dose of daily 5 MIU/m2 are presently addressing this question of whether a dose-response relationship exists. It needs to be elaborated whether in patients treated with IFN-α it is not the dose of IFN-α per se but rather the control of the disease reflected by complete hematologic and major cytogenetic responses that are the key factors predicting a better survival.
The survival data of the hydroxyurea-treated group in the Benelux appeared better than those observed in other trials (Table 4). The survival at 5 years for the Benelux control group was 55% (95% confidence interval, 44% to 66%), compared with 45% (35% to 55%) for the Italian study (Prof M. Baccarani, personal communication, April 1997), 44% (36% to 53%) for the German Hydroxyurea group,11 and 34% (27% to 42%) for the British MRC Study,9 which, however, contains the data of both busulfan and hydroxyurea-chemotherapy regimens. The Benelux patients differed from the Italian patients, who had 47% in the Sokal low group versus 30% in the Benelux (29% in Germany and 23% in UK). Because the Sokal score is an important prognostic factor for chemotherapy-treated patients, the survival results (median, 68 months) from the Benelux patients are even more impressive if compared with the Italian cohort (median, 52 months). It is attractive to assume that early and stringent disease control has been responsible for the observed good results for the hydroxyurea-treated patients, the suggestion for which also came from the results of the German CML study.18 However, other confounding factors have to be excluded. Ten patients of this group went off protocol because of preference to IFN, and 6 of them received this drug within 1 year from diagnosis. An analysis of the hydroxyurea group without these 6 patients did not show a different survival time (remaining 68.3 months). In the Italian hydroxyurea group, 8 patients refused continuation, but no data on the number of patients switching to IFN were given. Missing data of follow-up in the control arm could also have biased the results, but the median time interval between the study closure time (March 31, 1996) and last follow-up of all individual patients on and already off protocol was very short, ranging between 11 and 16 days for both arms.
The design of the Benelux study aimed at a more strict control of WBC counts than in the other studies: in Italy, a WBC of greater than 30 × 109/L was permitted before restarting of hydroxyurea (although hydroxyurea was usually restarted at lower WBC counts; Prof M. Baccarani, personal communication, EICML meeting, Athens, April 1997); in Germany, a range between 5 and 15 × 109/L was allowed; and in the United Kingdom, a WBC count of 5 to 20 × 109/L was permitted. In the Benelux, the large majority had median WBC counts of 10 × 109/L from early after randomization on. On the other hand, the MRC patients did obtain this level of control not before 10 months after randomization, but then continued at better levels of control (about 60% to 65% had WBC <10 × 109/L).10 An analysis using a cut-off point of 10 × 109/L by the German group showed a significantly better survival in the group, with lower WBC counts at month 6.11 We analyzed duration of good WBC control during the first year and found highly significant results for survival prediction for the IFN-treated group and a trend for better survival in the hydroxyurea group, which supports the assumption that durable tumor control gives a survival advantage, but that other factors may be important as well.18
In conclusion, in this randomized study between a low dose of IFN-α and hydroxyurea, we could not detect a statistically significant difference in duration of chronic phase or survival for patients with early CML. These results are in line with two other randomized studies from northern parts of Europe10,11 using much higher doses of IFN-α. The Benelux results contrast with the first published study from Italy.7 In our hands, the benefits of a better hematologic and cytogenetic response after IFN-α did not translate into a longer survival for the IFN-α–treated group as a whole. However, in a metaanalysis to which the Benelux study and the other above-mentioned studies participated, a survival advantage for IFN could still be found.22 As a second interesting observation, it appeared that for both groups strict WBC control during the first year resulted in a better survival. This finding suggests that the combined scheme of a low dose of IFN-α with additional hydroxyurea as used in the Benelux leaves room for further improvement. The ongoing studies randomizing between low and high doses of IFN can hopefully answer the question of whether strict WBC control obtained by high doses of IFN gives better results than the same low WBC count obtained by lower doses of IFN plus hydroxyurea. New treatment designs aiming at more complete hematologic responses and cytogenetic responses such as recently have been reported for the combination of IFN-α and cytarabine23 are required to obtain meaningful survival improvements in patients with CML who are not candidates for allogeneic BMT.
APPENDIX
Study Coordinator for The Netherlands: Dr J.C. Kluin-Nelemans, Department of Hematology, Leiden University Medical Center (Leiden, The Netherlands). Study Coordinators for Belgium: Dr A. Delannoy, Department of Hematology, Jolimont Hospital, Haine-Saint-Paul, and University Hospital St. Luc, Brussels (Brussels, Belgium); Dr A. Louwagie, Department of Hematology, University Hospital St Jan, Brugge (Brugge, Belgium). Statistics: Dr S. Le Cessie and Dr J. Hermans, Department of Medical Statistics, Leiden University Medical Center. Data management: Drs J.F. van der Burgh, Department of Hematology, Leiden University Medical Center. Cytogenetics:Prof Dr A.M. Hagemeijer (Rotterdam, The Netherlands) and Prof Dr H. Van den Berghe (Leuven, Belgium) performed the majority of the cytogenetic studies. The Benelux CML Study Group thanks P. Lubbers for data entry and Schering Plough Belgium/The Netherlands for help with data accrual and financial support.
The following physicians contributed patients to this study: Belgium: Dr Boogaerts, Leuven (22); Dr Bosly, Mont-Godine Yvoir (19); Dr Louwagie, Bruges (16); Dr Michaux and Dr Ferrant, Brussels (10); Dr Zachee, Antwerp (7); Dr Delannoy, Haine-St Paul (6); Dr Peetermans, Edegem (6); Dr van Hove, Gent (5); Dr Berneman, Antwerp (5); Dr Delwiche, Charleroi (3); Dr Humblet, Brussels (3); Dr Teuwen, Kapellen (3); Dr van Camp, Brussels (2); Dr van Stralen, Hasselt (2); Dr Stryckmans, Brussels (2); Dr Bastin, Charleroi (1); Dr Vandenbulcke, Tournai (1); Dr Bury, Huy (1); Dr Brohée, Mont-le-Tilleuil (1); Dr Cauchie, Brussels (1); Dr Duprez, Ottignies (1); Dr Dutrieux-Fauchet, Tournai (1); Dr Focan, Liège (1); Dr Feremans, Brussels (1); Dr Gangi, Brussels (1); Dr Honhon, Loverval (1); Dr Marcelis, Brussels (1); Dr Matthijs, Antwerp (1); Dr Mineur, Gilly (1); Dr Montfort, Bouge (1); Dr Neve, Brussels (1); Dr Reginster, Huy (1); Dr Richard, Baudour (1). Luxembourg: Dr Dicato, Luxembourg (1); Dr Sand, Luxembourg (1). The Netherlands: Dr Kluin-Nelemans, Leiden (13); Dr Joosten, Leeuwarden (4); Dr van Oers/Thomas/Von dem Borne, Amsterdam (4); Dr Daenen, Groningen (3); Dr Fickers, Heerlen (3); Dr Hensen, Haarlem (3); Dr Marx, Utrecht (3); Dr Muller, Blaricum (3); Dr Ananta/Jansen, Zoetermeer (2); Dr Baggen, Rotterdam (2); Dr Gerrits, The Hague (2); Dr ‘t Hart, Amersfoort (2); Dr Heering, Gouda (2); Dr Meuwissen, Nieuwegein (2); Dr Nortier, Utrecht (2); Dr Roozendaal, Amsterdam (2); Dr van de Stadt, Heemstede (2); Dr de Swart, Haarlem (2); Dr Sybesma, Dordrecht (2); Dr van Turnhout, Nijmegen (2); Dr Brouwers, Deventer (1); Dr Geelhoed-Duijvestijn, The Hague (1); Dr van Gent, Breda (1); Dr van Harskamp, Lelystad (1); Dr Herben, Leidschendam (1); Dr Michiels, Rotterdam (1); Dr Siegenbeek van Heukelom, Alkmaar (1); Dr Holdrinet, Breda (1); Dr Keuning, Veldhoven (1); Dr Kurstjens, ‘s-Hertogenbosch (1); Dr Lobatto, Hilversum (1); Dr van Marion-Kievit, Eindhoven (1); Dr Njo, Hoogeveen (1); Dr Peters, Leiderdorp (1); Dr Ploem, Amsterdam (1); Dr Rodenhuis, Amsterdam (1); Dr Slagboom, Voorburg (1); Dr Vermeer, Heerenveen (1).
For contributors and study coordinators, see the Appendix.
Address reprint requests to J.C. Kluin-Nelemans, MD, PhD, Department of Hematology, Bldg 1, E1-Q, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, The Netherlands.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal