To the Editor:
In a recent issue of Blood, Pestalozzi et al1reported interesting data on computerized tomographic (CT)-scan examinations in chronic systemic candidiasis in leukemia patients that become invisible during neutropenia. CT-scan is known to be sensitive, as has been demonstrated for magnetic resonance imaging (MRI)-scan.2,3 However, only ultrasound can be repeated as often as needed. Data correlation to ultrasound findings in these patients are lacking. Ultrasound examinations are easy to perform, comfortable for the patient, and cost-effective. We have analyzed prospectively the value of serial ultrasound examination in the diagnosis and follow-up of chronic systemic candidiasis in leukemia patients.4 From November 1996 until October 1997, a total of 220 ultrasound examinations (Kranzbühler Logiq 500, 3.5 MHz-convex array; Solingen, Germany) were performed in 58 leukemia patients undergoing intensive chemotherapy. Initial ultrasound pictures were stored on a personal computer and compared with the live ultrasound at the time of re-evaluation in cases of persistent fever. Abdominal ultrasound detected microabscesses in 8 patients. Diagnosis was confirmed by autopsy/biopsy (n = 6), blood culture (n = 1), and a significant candida-antibody titer at the time of neutrophil recovery (n = 1). According to Pestalozzi et al,1 focal lesions representing microabscesses in liver or spleen were detected by ultrasound only after neutrophil recovery. None of our serially monitored patients (ranging from 1 to a maximum of 16 follow-up examinations) showed a disappearance of hepatic lesions within subsequent phases of aplasia with a reappearance after recovery of the neutrophil count. We point out that our experiences with ultrasound are different from the observed CT-scans in the study of Pestalozzi et al.1 Based on our data, we believe that ultrasound examinations should be performed in addition to CTscan, because this might provide helpful complementary information.
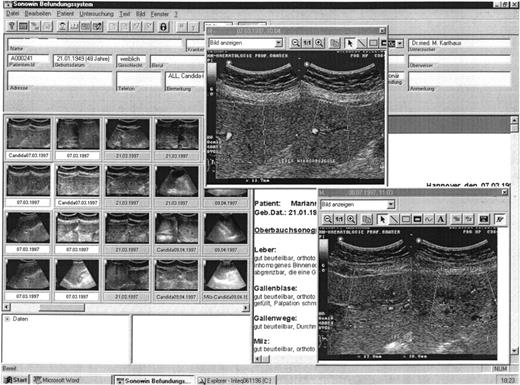
In addition to the reported CT-scan findings, a nonhomogenous micronodular parenchyma reflex pattern of liver and/or spleen was observed by ultrasound as a first sign in two of three patients who subsequently developed focal lesions, which persisted during febrile neutropenia (Table 1). A third patient developed a nonhomogenous parenchyma reflex pattern in the liver without evolving focal lesions subsequently. This patient had a proven septicemia with candida tropcalis and died in aplasia. A changing reflex pattern of the liver parenchyma has been also reported by Grois et al5 as a first sign in the course of chronic systemic candidiasis; however, this is not proven to be specific. New evolving focal lesions (wheel-in-wheel sign) in liver or spleen of small diameter are known to be ultrasound characteristics in chronic systemic candidiasis.6,7 Ultrasound proved to be as sensitive as CT-scan to detect these lesions in our study. Focal lesions detected in the liver and spleen ranged from 5 to 19 mm in diameter. The incidence of chronic systemic candidiasis was 13.8% in our study group, comparable to data in the literature.5 8 Because ultrasound was sensitive, follow-up of these patients with chronic systemic candidiasis was performed using ultrasound alone. One possible disadvantage of ultrasound examinations is a lack of sufficient documentation in serial ultrasound. However, we improved the reliability of ultrasound by computer-assisted documentation. Follow-up was easy to perform, because ultrasound pictures could be compared directly with live examinations on the screen (Fig1).
Ultrasound Features and Clinical Characteristics in Leukemia Patients With Chronic Systemic Candidiasis
| Patient No. . | Diagnosis . | Treatment . | Focal Lesions in the Liver . | Focal Spleen Lesion . | Irregular Pattern During Aplasia . | Autopsy or Biopsy Results (+ = microabscesses) . | CT-liver/ Spleen (+ = focal lesions) . | AP (J/L) GGT (J/L) (max) . | Blood Culture . | CandidaAntibody Titer (max) . | CandidaAntigen Titer (max) . | Outcome (+ = inf. related death) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | AML | IVA | + | + | No | ND | + | AP 214 GGT107 | Neg | 1:40,960 | Neg | Alive |
| 2 | AML | DAV | + | No | No | Neg | + | AP 304 GGT170 | Neg | 1:640 | Neg | Alive |
| 3 | CML blast crisis | ViDAP | + | + | No | + | + | AP 416 GGT 69 | Neg | 1:640 | Neg | + |
| 4 | AML | m-amsa/ida | No | No | ++L/−S | + | ND | AP 358 GGT 80 | C tropicalis | 1:640 | Neg | + |
| 5 | AML | DA | + | No | +L and +S (first) | + | ND | AP 738 GGT402 | Neg | 1:40,960 | Neg | + |
| 6 | CML blast crisis | IVA | + | + | No | + | ND | AP 112 GGT 16 | Neg | 1:1,280 | Pos 1:8 | + |
| 7 | ALL | ViDAP | + | + | +L and +S | + | + | AP 960 GGT550 | Neg | 1:20,480 | Neg | Alive |
| 8 | AML | IVA | + | + | No | + | + | AP 311 GGT122 | Neg | 1:2,560 | Neg | Dead, due to AML |
| Patient No. . | Diagnosis . | Treatment . | Focal Lesions in the Liver . | Focal Spleen Lesion . | Irregular Pattern During Aplasia . | Autopsy or Biopsy Results (+ = microabscesses) . | CT-liver/ Spleen (+ = focal lesions) . | AP (J/L) GGT (J/L) (max) . | Blood Culture . | CandidaAntibody Titer (max) . | CandidaAntigen Titer (max) . | Outcome (+ = inf. related death) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | AML | IVA | + | + | No | ND | + | AP 214 GGT107 | Neg | 1:40,960 | Neg | Alive |
| 2 | AML | DAV | + | No | No | Neg | + | AP 304 GGT170 | Neg | 1:640 | Neg | Alive |
| 3 | CML blast crisis | ViDAP | + | + | No | + | + | AP 416 GGT 69 | Neg | 1:640 | Neg | + |
| 4 | AML | m-amsa/ida | No | No | ++L/−S | + | ND | AP 358 GGT 80 | C tropicalis | 1:640 | Neg | + |
| 5 | AML | DA | + | No | +L and +S (first) | + | ND | AP 738 GGT402 | Neg | 1:40,960 | Neg | + |
| 6 | CML blast crisis | IVA | + | + | No | + | ND | AP 112 GGT 16 | Neg | 1:1,280 | Pos 1:8 | + |
| 7 | ALL | ViDAP | + | + | +L and +S | + | + | AP 960 GGT550 | Neg | 1:20,480 | Neg | Alive |
| 8 | AML | IVA | + | + | No | + | + | AP 311 GGT122 | Neg | 1:2,560 | Neg | Dead, due to AML |
Abbreviations: DA, daunorubicin/cytosine arabinoside; DAV, daunorubicin, cytosine arabinoside, vepesid; IVA, idarubicin/vepesid/cytosine arabinoside; m-amsa/ida, m-amsacrine/idarubicin; ViDAP, vincristin/daunorubicin/l-asparaginase/prednisone; ND, not done; candida-antibody, indirect haemagglutinin-test (Roche Co, Basel, Switzerland); candida-antigen, CanTec (Ramco-Lab 4507; MT, Mount Vernon, VA); L, liver; S, spleen.
The ultrasound pictures of this patient show a nonresponse to antifungal therapy in the course of chronic systemic candidiasis. The micro-abscesses in the left lobe of the liver are documented to be nonresponding. All stored ultrasound pictures, in part demonstrated on the left side of the computer screen, can be enlarged for comparison.
The ultrasound pictures of this patient show a nonresponse to antifungal therapy in the course of chronic systemic candidiasis. The micro-abscesses in the left lobe of the liver are documented to be nonresponding. All stored ultrasound pictures, in part demonstrated on the left side of the computer screen, can be enlarged for comparison.
In conclusion, we would recommend ultrasound examination in all patients with suspected or proven chronic systemic candidiasis, especially in those cases in which the lesions become invisible by CT-scans. In addition, a change in the parenchyma reflex pattern of liver and/or spleen during febrile neutropenia might be the first manifestation of an evolving chronic systemic candidiasis. Ultrasound proved to be sensitive and effective for the detection and follow-up of patients with chronic systemic candidiasis. Finally, ultrasound is comfortable for the patient and cost-effective.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal