Abstract
Posttransplantation lymphoproliferative disorders (PT-LPDs) represent a heterogeneous group of Epstein-Barr virus–associated lymphoid proliferations that arise in immunosuppressed transplant recipients. Some of these lesions regress after a reduction in immunosuppressive therapy, whereas some progress despite aggressive therapy. Morphological, immunophenotypic, and immunogenotypic criteria have not been useful in predicting clinical outcome. Although structural alterations in oncogenes and/or tumor suppressor genes identified in some PT-LPDs correlate with a poor clinical outcome, the presence of these alterations has not been a consistently useful predictor of lesion regression after reduction of immunosuppression. We examined 57 PT-LPD lesions obtained from 36 solid organ transplant recipients for the presence of mutations in the BCL-6 proto-oncogene using single-strand conformation polymorphism and sequence analysis, followed by correlation with histopathologic classification and clinical outcome, which was known in 33 patients. BCL-6 gene mutations were identified in 44% of the specimens and in 44% of the patients; none were identified in the cases classified as plasmacytic hyperplasia. However, mutations were present in 43% of the polymorphic lesions and 90% of the PT-LPDs diagnosed as non-Hodgkin's lymphoma or multiple myeloma. BCL-6 gene mutations predicted shorter survival and refractoriness to reduced immunosuppression and/or surgical excision. Our results suggest that the BCL-6 gene structure is a reliable indicator for the division of PT-LPDs into the biological categories of hyperplasia and malignant lymphoma, of which only the former can regress on immune reconstitution. The presence of BCL-6 gene mutations may be a useful clinical marker to determine whether reduction in immunosuppression should be attempted or more aggressive therapy should be instituted.
IMMUNOSUPPRESSED SOLID organ transplant recipients are prone to the development of a clinically heterogeneous group of lymphoid proliferations referred to as posttransplantation lymphoproliferative disorders (PT-LPDs). PT-LPDs were originally believed to be non-Hodgkin's lymphomas (NHLs), but their malignant status has been questioned because they frequently regress after a reduction of immunosuppressive therapy.1 However, disease behavior has been difficult to predict. It is now known that PT-LPDs are most frequently Epstein-Barr virus (EBV)-driven B-cell proliferations, which can be poly-, oligo-, mono-, or multiclonal based on phenotype2,3 or genotype.4-8 Furthermore, PT-LPDs are also morphologically heterogeneous; they do not resemble any of the recognized entities which fall under the broad category of lymphoid hyperplasia, and they have been difficult to classify using the standard lymphoma classification schemes, mainly due to the frequent polymorphic appearance of the lymphoid cells in these lesions. In an attempt to distinguish benign and malignant lesions, Frizzera et al3 divided PT-LPDs into the morphological categories of polymorphic B-cell hyperplasia (PBCH) and polymorphic B-cell lymphoma (PBCL). Subsequently, Nalesnik et al2 recognized two principal categories of PT-LPDs, which they designated polymorphic and monomorphic. However, neither morphology nor clonality has proven capable of reliably predicting disease behavior.
Molecular genetic characterization of PT-LPDs, including an assessment of the presence of structural alterations in some oncogenes and tumor suppressor genes, has proven to be more informative in predicting clinical outcome. It was first noted by Locker and Nalesnik6 that those monomorphic PT-LPDs displaying a strong clonal immunoglobulin gene rearrangement band on Southern blotting and a c-myc gene rearrangement exhibit disease progression. We subsequently showed that PT-LPDs are divisible into three distinct categories exhibiting unique morphological and molecular characteristics as follows: (1) plasmacytic hyperplasia (PH): usually polyclonal by immunoglobulin gene rearrangement analysis, and polyclonal or faint monoclonal by EBV terminal repeat analysis; (2) polymorphic PT-LPD, including PBCH and PBCL: monoclonal or oligoclonal by immunoglobulin gene rearrangement or EBV terminal repeat analysis, without other identifiable genetic alterations; and (3) NHL/multiple myeloma (MM): monoclonal with structural alterations of the N-ras, p53, and/or the c-myc genes.8 According to this scheme, the PT-LPDs classified as PH and polymorphic PT-LPD were more likely to regress with a reduction in immunosuppression or to undergo resolution with more aggressive therapy than those classified as NHL or MM.9 10 Although molecular analysis in conjunction with careful morphological evaluation permitted the classification of PT-LPDs into categories with clinical relevance, these criteria were not helpful in predicting response by the polymorphic PT-LPDs to a reduction in immunosuppression. We have now extended these studies to include analysis of the BCL-6 oncogene.
The BCL-6 gene codes for a nuclear protein that is normally expressed at high levels only in lymphoid cells, and predominantly in mature B cells and CD4+ T cells within germinal centers.11-14 The BCL-6 protein has six C-terminal zinc finger motifs and one N-terminal POZ motif, and functions as a sequence-specific transcriptional repressor.15-17 BCL-6 can bind Stat6 DNA binding sites and block Stat6-mediated interleukin-4 signaling.18 Experiments using BCL-6 knock-out mice have shown that this protein controls germinal center formation as well as T-helper cell type 2–mediated inflammatory responses.18,19The BCL-6 gene was identified because of its involvement in chromosomal translocations affecting band 3q27, which is a frequent breakpoint site in diffuse large-cell lymphomas.20-24 Rearrangements of this gene can be identified by Southern blot analysis in 30% to 45% of diffuse large-cell lymphomas, in 6% to 10% of follicular lymphomas, and in 20% of acquired immunodeficiency syndrome (AIDS)-related diffuse large B-cell lymphomas.25-28 The majority of rearrangement breakpoints cluster within a 4-kb region spanning the BCL-6 promoter and first noncoding exon, resulting in the fusion of BCL-6 coding sequences (exons 2 to 10) to heterologous promoters from other chromosomes, leading to deregulated expression by the mechanism of promoter substitution.29 Subsequent analysis of BCL-6 has shown the presence of point mutations and/or small deletions in 70% of diffuse large-cell lymphomas and 45% of follicular lymphomas, as well as in 58% of AIDS-associated NHLs.30,31 These mutations occur within a 4-kb region spanning the first exon, but tend to cluster in the 5′ region of the first intron, and overlap with the major cluster of chromosomal breakpoints. Analyses of both BCL-6 gene rearrangements and mutations have shown that structural alterations in the 5′ noncoding region of BCL-6 are present in virtually all cases of diffuse large-cell lymphoma and the majority of cases of follicular and AIDS-related NHLs,30 31 but are absent from all nonhematopoietic tumors examined thus far. The frequency, clustering, and disease-association of these alterations suggest that they may contribute to B-cell lymphomagenesis, presumably by altering BCL-6 gene expression. Therefore, we analyzed a panel of 57 PT-LPD lesions obtained from 36 patients for the presence of rearrangements and/or mutations in the BCL-6 proto-oncogene, and correlated the results with the outcome of the 33 patients for whom complete clinical information was available.
MATERIALS AND METHODS
Pathological specimens.
Fifty-seven PT-LPD specimens were collected from 36 solid organ transplant recipients (1 lung, 11 kidney, and 24 heart) during the course of clinical evaluation using standard diagnostic procedures. Cases were processed at or submitted in consultation to the Columbia-Presbyterian Medical Center and/or The New York Hospital-Cornell Medical Center. The cases were selected based on the morphological diagnosis of a lymphoproliferative disorder in a solid organ transplant recipient and the availability of cryopreserved cells or tissue blocks. The morphological and molecular analysis of 21 of the 57 lesions, as well as the clinical outcome of 32 patients, have been previously reported.8,10 32 Involved tissues included biopsies from lymph nodes, tonsils, adenoids, lungs, colon, liver, brain, breast, bone marrow, and soft tissues. Representative portions of the solid specimens were snap-frozen and stored at −70°C. A sample of aspirated bone marrow was collected in a heparinized syringe. A viable mononuclear cell suspension was prepared from this sample by Ficoll-Hypaque (Pharmacia Biotech, Uppsala, Sweden) density gradient centrifugation. The cells were cryopreserved in dimethylsulfoxide and fetal calf serum at −170°C. Portions of each of the specimens were routinely fixed for histopathologic examination.
DNA extraction.
Genomic DNA was extracted from cryopreserved mononuclear cell suspensions and tissue blocks using a salting-out procedure.33
Histopathologic classification.
The 57 PT-LPD lesions were classified as described8 by two of the authors (A.C. and D.M.K.), without knowledge of the molecular features or the patient's clinical outcome, into one of four morphological categories as follows: (1) PH, lesions exhibited retention of the underlying architecture and expansion of the interfollicular area or diffuse infiltration of other tissue by a predominant population of plasmacytoid lymphocytes, associated with plasma cells and sparse immunoblasts; (2) PBCH, lesions produced extensive disturbance of organ architecture and were composed of a mixture of lymphoid cells with prominent plasmacytoid differentiation and abundant immunoblasts without cytological atypia; in these lesions necrosis was limited to single cells or small foci; (3) PBCL, lesions were composed of a mixture of lymphoid cells lacking prominent plasmacytoid differentiation and displaying significant cytologic atypia, atypical immunoblasts, and contained large confluent areas of coagulative necrosis; (4) NHL/MM, lesions were composed of a monomorphic collection of cytologically malignant large lymphoid cells or plasma cells, respectively.
Southern blot hybridization analysis.
Five microgram–aliquots of genomic DNA were digested withBamHI and XbaI, respectively (Boehringer-Manheim, Indianapolis, IN), electrophoresed in 0.8% agarose gels, denatured with alkali, neutralized, and transferred to nitrocellulose filters according to Southern analysis. The filters were hybridized to a32P-labeled BCL-6 probe (Sac4.0) as previously described.20
Oligonucleotide primers.
Five sets of primers were used, spanning a 741-bp region which is altered in almost 70% of diffuse large-cell lymphomas. These sets have been designated E1.9 through E1.13 as follows: E1.9: 5′-GGGTTCTTAGAAGTGGTG-3′ and 5′-CAAAGCATTTGGCAAGAG-3′; E1.10: 5′-ctcttgccaaatgctttg-3′ and 5′-TAATTCCCCTCCTTCCTC-3′; E1.11: 5′-AGGAAGGAGGGGAATTAG-3′ and 5′-AAGCAGTTTGCAAGCGAG-3′; E1.12: 5′-TTCTCGCTTGCAAACTGC-3′ and 5′-CACGATACTTCATCTCATC-3′; E1.13: 5′-GATGAGATGAAGTATCGTG-3′ and 5′-ACACTGAAAGGCATCGCA-3′.
Single-strand conformation polymorphism (SSCP) analysis.
Polymerase chain reactions (PCRs) were performed with 100 ng of genomic DNA, in the presence of 10 pmol of each primer, 25 μmol/L dNTPs, 1 μCi of [α-32P]dCTP (NEN Life Science Products, Boston, MA; specific activity, 3,000 Ci/mmol), and 1.5 mmol/L MgCl2. Thirty cycles of denaturation (94°C), annealing (56°C for E1.10, 58°C for E1.11, and 54°C for E1.10), and extension (72°C) were performed. The reaction mixture (2 μL) was diluted 1:25 in 0.1% sodium dodecyl sulfate, 10 mmol/L EDTA, and further mixed 1:1 with a sequencing stop solution (95% formamide, 20 mmol/L EDTA, 0.05% bromophenol blue, and 0.05% xylene cyanol). Samples were heat denatured and electrophoresed in a 6% acrylamide gel containing 10% glycerol.
Sequencing of PCR products.
Eight representative PCR products were cloned in the pCR2.1 vector using the TA Cloning Kit (Invitrogen Corp, Carlsbad, CA) following the manufacturer's instructions. Sequence of the inserts was performed with a Taq DyeDeoxy Terminator Cycle Sequencing method with an ABI 373A automated DNA sequencer (Applied Biosystems, Foster City, CA). The two strands and at least four independent clones were sequenced in each case to exclude mismatches due to polymerase mistakes, and to analyze the status of both alleles.
Classification of clinical outcome.
Clinical follow-up was available in 33 patients. The clinical outcomes with respect to their PT-LPDs were categorized using a modification of the guidelines suggested by Nalesnik et al.2 A more extensive review of the clinical features of 32 of these patients has been reported separately.10 “Regression” was defined as disappearance of PT-LPD lesions after reduction in immunosuppression, with or without acyclovir, as evaluated by physical examination (28 patients), endoscopy (3 patients), and/or radiographic studies (21 patients). In these instances, surgical intervention was limited to biopsy or partial excision of the PT-LPD only. “Surgical resolution” refers to cases in which the entire tumor was surgically excised. Two cases in which adjuvant radiation was administered were included in this category. “Medical resolution” refers to cases in which the tumor disappeared after chemotherapy. Progression of PT-LPD in spite of therapeutic intervention was considered a “no response.” Four cases in which there was no clinical documentation of either regression or progression of the PT-LPD were classified as “not evaluable.” With one exception (Case 19), all patients who received chemotherapy initially had a reduction of immunosuppression, and thus a “medical resolution” implies a lack of response to reduction in immunosuppression in the majority of cases. In three patients there was a recurrence in a different site, of different clonal origin and of different histological category. In these instances, only the outcome after the most recent lesion was considered for statistical analysis.
Statistical methods.
The Fisher's exact test was used to determine if a particular morphological category and clinical outcome of patients with PT-LPD was associated with the presence of mutations in the BCL-6 gene. If a significant association was found, then pairwise comparisons with a Bonferroni correction were performed to determine where the difference actually existed.34 Formal analysis of survival (Kaplan-Meier estimate) was performed with regard to the presence or absence of BCL-6 gene mutations using the LIFETEST Procedure.
RESULTS
Histopathology.
Histological sections from the 57 PT-LPD specimens included in this study were classified as follows: (1) PH, 11 specimens from 10 patients; (2) PBCH, 8 specimens from 7 patients; (3) PBCL, 29 specimens from 13 patients; (4) NHL/MM, 9 specimens from 8 patients. Nine patients had multiple (2 to 12) PT-LPD lesions that were evaluated in this study. In 6 of these patients (Cases 6, 23 through 26, and 31) all lesions corresponded to the same histopathologic category, and in 3 patients (Cases 34 through 36) the PT-LPD lesions were of different histopathologic subtype (Table 1).
BCL-6 Gene Structural Alterations and Relationship to Other Molecular Features in Posttransplantation Lymphoproliferative Disorders
| Case No. . | DX . | Outcome . | BCL-6 . | Ig . | EBV . | Oncogenes/Tumor Suppressors . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SB . | SSCP . | TR . | Type . | LMP . | c-myc . | p53 . | N-ras . | ||||
| 1 | PH | Regression | G | WT | G | PC | A | WT | G | WT | WT |
| 2 | PH | Regression | G | WT | G | 1FT | A | D | G | WT | WT |
| 3 | PH | Resolution (surg) | G | WT | R (FT) | 1 | A | WT | G | WT | WT |
| 4 | PH | Regression | G | WT | G | PC | A | D | G | WT | WT |
| 5 | PH | Resolution (surg) | WT/P | G | PC | A | D | G | WT | WT | |
| 6A | PH | Resolution (surg) | WT | G | 1FT | A | WT | G | WT | WT | |
| 6B | PH | Resolution (surg) | WT | G | 1FT | A | WT | G | WT | WT | |
| 7 | PH | Resolution (surg) | WT | G | WT | G | |||||
| 8 | PH | Resolution (surg) | WT | NEG | NEG | WT | WT | ||||
| 9 | PBCH | Resolution (surg) | G | WT | R | 1 | A | D | G | WT | WT |
| 10 | PBCH | Regression | G | WT | R (FT) | 1FT | WT | G | WT | WT | |
| 11 | PBCH | Resolution (xrt) | G | WT/P | R | 1 | A | WT | G | WT | WT |
| 12 | PBCH | Resolution (chemo) | G | M | R | NEG | NEG | WT | G | WT | WT |
| 13 | PBCH | Regression | G | WT/P | R | 1 | A | WT | G | WT | WT |
| 14 | PBCH | Unknown | M | D | |||||||
| 15 | PBCL | Resolution (chemo) | G | M* | R | 1 | A | D | G | WT | WT |
| 16 | PBCL | Resolution (chemo) | G | M* | R | 1 | A | WT | G | WT | WT |
| 17 | PBCL | Regression | G | WT/P | R | 1 | A | D | G | WT | WT |
| 18 | PBCL | Regression | G | WT/P | R | 1 | A | D | G | WT | WT |
| 19 | PBCL | Resolution (chemo) | WT | R | 1 + 2FT | A | WT | G | WT | WT | |
| 20 | PBCL | Unknown | WT/P | G | 1 | A | D | G | WT | WT | |
| 21 | PBCL | Regression | WT | WT | |||||||
| 22 | PBCL | Resolution (chemo) | M | R | 1 | A | WT | G | WT | WT | |
| 23A | PBCL | Not evaluable | G | WT | R | 2 + 1FT | A | WT | G | WT | WT |
| 23B | PBCL | Not evaluable | G | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT |
| 24A | PBCL | Resolution (chemo) | G | WT | R | 1 | WT | ||||
| 24B | PBCL | Resolution (chemo) | G | M* | R (SAME) | 1 (SAME) | WT | ||||
| 24C | PBCL | Resolution (chemo) | G | M (DIF) | R (SAME) | 1 (SAME) | WT | ||||
| 25A | PBCL | No response | M | R | 1 | A | WT | G | WT | WT | |
| 25B | PBCL | No response | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25C | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25D | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25E | PBCL | No response | WT | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25F | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25G | PBCL | No response | M (DIF) | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25H | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25I | PBCL | No response | M (DIF) | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25J | PBCL | No response | WT | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25K | PBCL | No response | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25L | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 26A | PBCL | Resolution (surg/xrt) | G | WT | G | NEG | D | ||||
| 26B | PBCL | Resolution (surg/xrt) | G | WT | G | 1FT | D | ||||
| 26C | PBCL | Resolution (surg/xrt) | WT | G | 1FT | D | |||||
| 27 | NHL | Resolution (chemo) | G | M | R | 1 | A | D | G | M | WT |
| 28 | MM | No response | G | M* | R | 1 | A | D | G | WT | M |
| 29 | NHL | Resolution (chemo) | G | M* | R | 1 | B | WT | R/M | WT | |
| 30 | NHL | Unknown | M* | R | 1 | A | D | G | WT | ||
| 31A | NHL | Not evaluable | M | R | 1 | D | G | ||||
| 31B | NHL | Not evaluable | M (SAME) | R (SAME) | 1 | D | |||||
| 32 | NHL | Not evaluable | M | ||||||||
| 33 | NHL | No response | WT | R | NEG | NEG | G | WT | WT | ||
| 34A | PH | Resolution (surg) | G | WT | G | 1FT | A | D | G | WT | WT |
| 34B | PBCL | Resolution (chemo) | G | M | R | 1 + 1FT | D | ||||
| 35A | PBCH | Resolution | M | R | 1 | A | WT | G | WT | WT | |
| 35B | PBCL | Progression | M (SAME) | R (SAME) | 1 | A | WT | G | WT | WT | |
| 36A | PH | Regression | G | WT | G | PC | A | WT | G | WT | WT |
| 36B | MM | No response | G | M* | R | 1 | A | WT | G | WT | M |
| Case No. . | DX . | Outcome . | BCL-6 . | Ig . | EBV . | Oncogenes/Tumor Suppressors . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SB . | SSCP . | TR . | Type . | LMP . | c-myc . | p53 . | N-ras . | ||||
| 1 | PH | Regression | G | WT | G | PC | A | WT | G | WT | WT |
| 2 | PH | Regression | G | WT | G | 1FT | A | D | G | WT | WT |
| 3 | PH | Resolution (surg) | G | WT | R (FT) | 1 | A | WT | G | WT | WT |
| 4 | PH | Regression | G | WT | G | PC | A | D | G | WT | WT |
| 5 | PH | Resolution (surg) | WT/P | G | PC | A | D | G | WT | WT | |
| 6A | PH | Resolution (surg) | WT | G | 1FT | A | WT | G | WT | WT | |
| 6B | PH | Resolution (surg) | WT | G | 1FT | A | WT | G | WT | WT | |
| 7 | PH | Resolution (surg) | WT | G | WT | G | |||||
| 8 | PH | Resolution (surg) | WT | NEG | NEG | WT | WT | ||||
| 9 | PBCH | Resolution (surg) | G | WT | R | 1 | A | D | G | WT | WT |
| 10 | PBCH | Regression | G | WT | R (FT) | 1FT | WT | G | WT | WT | |
| 11 | PBCH | Resolution (xrt) | G | WT/P | R | 1 | A | WT | G | WT | WT |
| 12 | PBCH | Resolution (chemo) | G | M | R | NEG | NEG | WT | G | WT | WT |
| 13 | PBCH | Regression | G | WT/P | R | 1 | A | WT | G | WT | WT |
| 14 | PBCH | Unknown | M | D | |||||||
| 15 | PBCL | Resolution (chemo) | G | M* | R | 1 | A | D | G | WT | WT |
| 16 | PBCL | Resolution (chemo) | G | M* | R | 1 | A | WT | G | WT | WT |
| 17 | PBCL | Regression | G | WT/P | R | 1 | A | D | G | WT | WT |
| 18 | PBCL | Regression | G | WT/P | R | 1 | A | D | G | WT | WT |
| 19 | PBCL | Resolution (chemo) | WT | R | 1 + 2FT | A | WT | G | WT | WT | |
| 20 | PBCL | Unknown | WT/P | G | 1 | A | D | G | WT | WT | |
| 21 | PBCL | Regression | WT | WT | |||||||
| 22 | PBCL | Resolution (chemo) | M | R | 1 | A | WT | G | WT | WT | |
| 23A | PBCL | Not evaluable | G | WT | R | 2 + 1FT | A | WT | G | WT | WT |
| 23B | PBCL | Not evaluable | G | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT |
| 24A | PBCL | Resolution (chemo) | G | WT | R | 1 | WT | ||||
| 24B | PBCL | Resolution (chemo) | G | M* | R (SAME) | 1 (SAME) | WT | ||||
| 24C | PBCL | Resolution (chemo) | G | M (DIF) | R (SAME) | 1 (SAME) | WT | ||||
| 25A | PBCL | No response | M | R | 1 | A | WT | G | WT | WT | |
| 25B | PBCL | No response | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25C | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25D | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25E | PBCL | No response | WT | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25F | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25G | PBCL | No response | M (DIF) | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25H | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25I | PBCL | No response | M (DIF) | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25J | PBCL | No response | WT | R (DIF) | 2 (DIF) | A | WT | G | WT | WT | |
| 25K | PBCL | No response | WT | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 25L | PBCL | No response | M (DIF) | R (DIF) | 1 (DIF) | A | WT | G | WT | WT | |
| 26A | PBCL | Resolution (surg/xrt) | G | WT | G | NEG | D | ||||
| 26B | PBCL | Resolution (surg/xrt) | G | WT | G | 1FT | D | ||||
| 26C | PBCL | Resolution (surg/xrt) | WT | G | 1FT | D | |||||
| 27 | NHL | Resolution (chemo) | G | M | R | 1 | A | D | G | M | WT |
| 28 | MM | No response | G | M* | R | 1 | A | D | G | WT | M |
| 29 | NHL | Resolution (chemo) | G | M* | R | 1 | B | WT | R/M | WT | |
| 30 | NHL | Unknown | M* | R | 1 | A | D | G | WT | ||
| 31A | NHL | Not evaluable | M | R | 1 | D | G | ||||
| 31B | NHL | Not evaluable | M (SAME) | R (SAME) | 1 | D | |||||
| 32 | NHL | Not evaluable | M | ||||||||
| 33 | NHL | No response | WT | R | NEG | NEG | G | WT | WT | ||
| 34A | PH | Resolution (surg) | G | WT | G | 1FT | A | D | G | WT | WT |
| 34B | PBCL | Resolution (chemo) | G | M | R | 1 + 1FT | D | ||||
| 35A | PBCH | Resolution | M | R | 1 | A | WT | G | WT | WT | |
| 35B | PBCL | Progression | M (SAME) | R (SAME) | 1 | A | WT | G | WT | WT | |
| 36A | PH | Regression | G | WT | G | PC | A | WT | G | WT | WT |
| 36B | MM | No response | G | M* | R | 1 | A | WT | G | WT | M |
Abbreviations: DX, histopathologic diagnosis; surg, surgery; xrt, radiotherapy; chemo, chemotherapy; SB, Southern blot; Ig, immunoglubulin heavy chain gene; TR, EBV clonality evaluated by Southern blot using a terminal repeat probe; LMP, latent membrane protein; WT, wild type; P, polymorphic; M, mutant; M, mutations identified in two or more SSCP fragments; *, sequenced; G, germline configuration; R, rearranged; DIF, different mutations or pattern of rearrangement; FT, faint band; NEG, negative; D, deleted.
Analysis of BCL-6 gene rearrangements.
Southern blot analysis was performed to assess the presence of rearrangement in the 5′ region of the BCL-6 gene. Representative examples of each category were evaluated, and included a total of 27 lesions from 21 patients. All of the PT-LPD cases examined showed a distinct band in the germline configuration, and no rearrangements were identified using this method (Table 1).
Analysis of BCL-6 gene mutations.
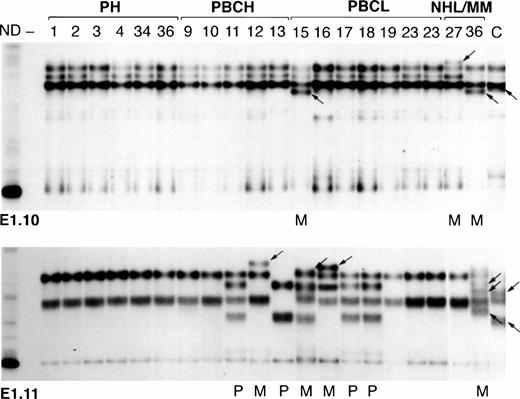
Mutations and/or small deletions in the 5′ noncoding region of BCL-6 were detected by SSCP analysis in a total of 25 PT-LPD specimens (44%) in 16 (44%) patients (Table 1). Representative experiments are shown in Fig1. Cases were scored as positive for mutations only when the migration in the SSCP gel was different from that observed in a negative control as well as from that of known polymorphic controls as described30 (Fig 1). Some specimens showed abnormal migration of one of the five fragments amplified (E1.9 through E1.13) to cover the BCL-6 mutation cluster region, whereas other cases (underlined in Table 1) showed abnormal migration in several of these fragments, reflecting the presence of multiple mutations. There was no evidence for involvement of both alleles, because all cases with abnormal bands also retained the wild-type pattern bands, although these may be derived from infiltrating, reactive cells.
SSCP analysis of representative first intron segments of the BCL-6 gene in PT-LPDs. Samples corresponding to radiolabeled, PCR-amplified fragments from the E1.10 (top) and E1.11 (bottom) regions of BCL-6 are shown. Numbers above the lanes indicate the corresponding cases. Among the patients with more than one PT-LPD lesion are Cases 23 and 36. The histological classification of each case is indicated above the corresponding lanes. Several identical bands were seen in all of the samples in the cases containing the wild-type sequence. Three different wild-type patterns are seen in the E1.11 region (bottom) due to a known polymorphism; polymorphic cases are indicated with a P beneath the corresponding lanes (Cases 11, 15, 17, and 18 are heterozygous and Case 13 is homozygous for this polymorphism). Cases 15, 27, and 36 showed a different pattern (arrows) in region E1.10 (top), and Cases 12, 15, 16, and 36 showed a different pattern (arrows) in region E1.11 (bottom), as a result of the presence of mutations in the corresponding region, indicated with an M beneath the corresponding lanes. ND, amplified DNA that was not denatured before electrophoresis; —, the same PCR reaction in the absence of DNA; C, positive control known to contain BCL-6 mutations in the region examined.
SSCP analysis of representative first intron segments of the BCL-6 gene in PT-LPDs. Samples corresponding to radiolabeled, PCR-amplified fragments from the E1.10 (top) and E1.11 (bottom) regions of BCL-6 are shown. Numbers above the lanes indicate the corresponding cases. Among the patients with more than one PT-LPD lesion are Cases 23 and 36. The histological classification of each case is indicated above the corresponding lanes. Several identical bands were seen in all of the samples in the cases containing the wild-type sequence. Three different wild-type patterns are seen in the E1.11 region (bottom) due to a known polymorphism; polymorphic cases are indicated with a P beneath the corresponding lanes (Cases 11, 15, 17, and 18 are heterozygous and Case 13 is homozygous for this polymorphism). Cases 15, 27, and 36 showed a different pattern (arrows) in region E1.10 (top), and Cases 12, 15, 16, and 36 showed a different pattern (arrows) in region E1.11 (bottom), as a result of the presence of mutations in the corresponding region, indicated with an M beneath the corresponding lanes. ND, amplified DNA that was not denatured before electrophoresis; —, the same PCR reaction in the absence of DNA; C, positive control known to contain BCL-6 mutations in the region examined.
In patients containing multiple PT-LPD lesions, several different patterns were identified. Case 35 had two lesions, 4 months apart and in different anatomic sites, one of which was classified as PBCH, and the second one as PBCL. However, both of the lesions seemed to have the same clonal origin, as evaluated by Ig gene rearrangement and EBV terminal repeat analysis, and the same BCL-6 mutation. Case 24 had three separate lesions at the same time, all classified as PBCL, and all derived from the same original clone. However, two of the lesions contained distinct BCL-6 mutations. Case 25 had multiple lesions in the bowel, all classified as PBCL, but each derived from distinct original clones.35 In this patient, different BCL-6 gene mutations were identified in 8 of 12 separate tumors examined. Cases 34 and 36 presented with a polyclonal PH, and 57 and 13 months later developed lesions classified as PBCL and MM, respectively. In both cases, only the second lesion contained mutations in the BCL-6 gene.
To confirm the results obtained by SSCP analysis, 10 representative PCR products, of which 6 had altered mobility patterns on SSCP analysis and 4 did not, were cloned and subjected to sequence analysis. Lesions from which these PCR fragments were obtained are identified in Table 1 by an asterisk. Mutations identified were as follows, where base numbering corresponds to the first intron of the BCL-6 gene: Case 15, region E1.9: C insertion (117), C→T (134), T→A (141); Case 15, region E1.10: A→T (225), A→G (244), A→C (262), C→G (323), A→C (333); Case 16, region E1.11: G→C (485), C→G (502); Case 28, region E1.11: T→G (526), G→C (552); Case 30, region E1.11: C→T (596); and case 36B, region E1.11: T→G (503), T→G (504), C→G (586). Mutations were frequently multiple, as seen by the abnormal migration patterns in more than one PCR fragment (Table 1), or by the presence of multiple mutations within one sequenced PCR fragment. Wild-type clones were obtained from all six cases with abnormal SSCP migration, which may derive from a normal allele or from normal cells infiltrating the PT-LPD lesion. No cases were detected in which heterozygous mutations were present in both alleles. In the three cases for which PCR fragments with normal SSCP migration patterns were sequenced, either no mutations were identified in any of the four clones examined (one case) or single–base pair mutations in only one clone were observed (two cases), which could not be confirmed by sequencing of additional clones. These changes may represent Taq polymerase mistakes rather than true mutations. However, the possibility of the presence of rare tumor cells carrying mutations that cannot be identified by SSCP analysis cannot be excluded.
Correlation of BCL-6 gene mutations and histopathologic category.
None of 11 PH specimens (0%), 3 of 8 PBCH specimens (37%), 14 of 29 PBCL specimens (48%), and 8 of 9 (87%) NHL/MM specimens contained alterations in this region. These differences were statistically significant (P = .0048; Table 2). Using pairwise comparisons, these differences were not significant between PBCH and PBCL. Grouping these two categories into one of polymorphic PT-LPDs, the correlation of the presence of BCL-6 gene mutations with histopathologic category increased in statistical significance (P = .0022).
BCL-6 Gene Mutations in Different Histopathologic Categories of PT-LPD
| . | Histological Classification . | |||
|---|---|---|---|---|
| PH . | PBCH . | PBCL . | NHL/ MM . | |
| Positive patients | 0/10 | 3/7 | 6/13 | 7/8 |
| 0% | 43% | 46% | 87% | |
| Positive specimens | 0/11 | 4/8 | 14/29 | 8/9 |
| 0% | 50% | 48% | 89% | |
| . | Histological Classification . | |||
|---|---|---|---|---|
| PH . | PBCH . | PBCL . | NHL/ MM . | |
| Positive patients | 0/10 | 3/7 | 6/13 | 7/8 |
| 0% | 43% | 46% | 87% | |
| Positive specimens | 0/11 | 4/8 | 14/29 | 8/9 |
| 0% | 50% | 48% | 89% | |
Correlation of BCL-6 gene mutations and clinical outcome.
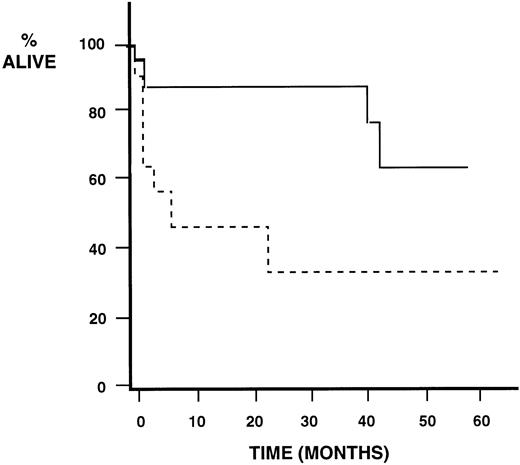
To determine the clinical significance of BCL-6 gene mutations, we compared clinical outcome of 33 patients with the presence of mutations in the BCL-6 gene in their PT-LPD lesions. The presence of these mutations had a significant correlation with time to death (P = .02); patients with lesions lacking BCL-6 gene mutations had a longer survival as seen in the Kaplan-Meier analysis shown in Fig 2. There was also a high correlation between the presence of BCL-6 gene mutations and the different clinical outcome categories. None of the cases with lesions that regressed after reduction of immunosuppression had BCL-6 gene mutations. Moreover, the absence of such mutations had a predictive value for regression when compared with resolution (P = .026) and no response (P= .007), with a significant overall predictive value of BCL-6 mutations when regression versus resolution versus no response were compared (P = .008) (Table 3). Cases that showed surgical resolution also lacked BCL-6 mutations, in contrast to those with medical resolution (P = .0001).
Survival function estimates of BCL-6 gene mutations in PT-LPDs. Formal analysis of survival (Kaplan-Meier estimate) with regard to the presence or absence of BCL-6 gene mutations is shown. There was a statistically significant (P = .02) decrease in time to death in the patients with PT-LPDs containing BCL-6 gene mutations. The continuous line indicates a wild-type BCL-6 as assessed by SSCP, and the discontinuous line indicates a mutant BCL-6.
Survival function estimates of BCL-6 gene mutations in PT-LPDs. Formal analysis of survival (Kaplan-Meier estimate) with regard to the presence or absence of BCL-6 gene mutations is shown. There was a statistically significant (P = .02) decrease in time to death in the patients with PT-LPDs containing BCL-6 gene mutations. The continuous line indicates a wild-type BCL-6 as assessed by SSCP, and the discontinuous line indicates a mutant BCL-6.
Predictive Value of BCL-6 Gene Mutations in PT-LPDs: Regression Versus Resolution Versus No Response
| BCL-6 . | Regression . | Resolution (surg + chemo) . | No Response . | Total . |
|---|---|---|---|---|
| All cases | ||||
| Wild type | 8 | 9 | 1 | 18 |
| 100% | 53% | 20% | 60% | |
| Mutant | 0 | 8 | 4 | 12 |
| 0% | 47% | 80% | 40% | |
| Total (P = .008) | 8 | 17 | 5 | 30 |
| 26% | 57% | 17% | 100% | |
| Polymorphic cases | ||||
| Wild type | 5 | 4 | 0 | 9 |
| 100% | 40% | 0% | 53% | |
| Mutant | 0 | 6 | 2 | 8 |
| 0% | 60% | 100% | 47% | |
| Total (P = .02) | 5 | 10 | 2 | 17 |
| 29% | 59% | 12% | 100% |
| BCL-6 . | Regression . | Resolution (surg + chemo) . | No Response . | Total . |
|---|---|---|---|---|
| All cases | ||||
| Wild type | 8 | 9 | 1 | 18 |
| 100% | 53% | 20% | 60% | |
| Mutant | 0 | 8 | 4 | 12 |
| 0% | 47% | 80% | 40% | |
| Total (P = .008) | 8 | 17 | 5 | 30 |
| 26% | 57% | 17% | 100% | |
| Polymorphic cases | ||||
| Wild type | 5 | 4 | 0 | 9 |
| 100% | 40% | 0% | 53% | |
| Mutant | 0 | 6 | 2 | 8 |
| 0% | 60% | 100% | 47% | |
| Total (P = .02) | 5 | 10 | 2 | 17 |
| 29% | 59% | 12% | 100% |
Abbreviations: surg, surgery; chemo, chemotherapy.
Because the cases belonging to the PH category have been shown to have a benign clinical course with regression after reduction of immunosuppression, and the monomorphic cases classified as NHL/MM to behave as aggressive malignant neoplasms with a poor clinical outcome,10 we performed the same statistical analysis including only the polymorphic categories (PBCH and PBCL) to determine whether the presence of BCL-6 mutations predicted clinical behavior among these cases. Survival analysis could not be performed because of the small sample size of 17 patients. However, a statistically significant predictive value for the presence of BCL-6 gene mutations was observed for regression versus resolution versus no response (P = .02) (Table 3), which was because of the predictive value for regression when compared with resolution (P = .044) and no response (P = .048).
When cases were grouped by either of two clinical outcomes, one including regression and surgical resolution, and the second including medical resolution and no response, the statistical significance of the presence of BCL-6 gene mutations was P = .00001. When the same analysis was performed for only the polymorphic categories, the predictive value for the presence of BCL-6 gene mutations was still statistically significant (P = .0004) (Table 4). None of the lesions in the first outcome category (regression or surgical resolution) contained BCL-6 mutations. In contrast, PT-LPD lesions that showed medical resolution or no response had BCL-6 gene mutations in all but two patients (Cases 19 and 33). Case 19 was the only case in which chemotherapy was administered without previous reduction of immunosuppression, and thus it is unknown whether this lesion would have regressed. The second exception, Case 33, was unusual in that it was an EBV-negative tumor classified morphologically as a diffuse large-cell lymphoma which presented 10 years after renal transplantation. Thus, the lack of mutations in the BCL-6 gene is a very good predictor of regression or resolution with local therapy, whereas the presence of mutations in this gene predicts the need for more aggressive and systemic therapeutic intervention.
Predictive Value of Absence of BCL-6 Gene Mutations in PT-LPDs: Response to Reduction of Immunosuppression or Surgical Excision Versus Medical Resolution or No Response
| BCL-6 . | Regression or Surgical Resolution . | Medical Resolution or No Response . | Total . |
|---|---|---|---|
| All cases | |||
| Wild type | 16 | 2 | 18 |
| 100% | 14% | 60% | |
| Mutant | 0 | 12 | 12 |
| 0% | 86% | 40% | |
| Total (P = .00001) | 16 | 14 | 30 |
| 53% | 47% | 100% | |
| Polymorphic cases | |||
| Wild type | 8 | 1 | 9 |
| 100% | 11% | 53% | |
| Mutant | 0 | 8 | 8 |
| 0% | 89% | 47% | |
| Total (P = .0004) | 8 | 9 | 17 |
| 47% | 53% | 100% |
| BCL-6 . | Regression or Surgical Resolution . | Medical Resolution or No Response . | Total . |
|---|---|---|---|
| All cases | |||
| Wild type | 16 | 2 | 18 |
| 100% | 14% | 60% | |
| Mutant | 0 | 12 | 12 |
| 0% | 86% | 40% | |
| Total (P = .00001) | 16 | 14 | 30 |
| 53% | 47% | 100% | |
| Polymorphic cases | |||
| Wild type | 8 | 1 | 9 |
| 100% | 11% | 53% | |
| Mutant | 0 | 8 | 8 |
| 0% | 89% | 47% | |
| Total (P = .0004) | 8 | 9 | 17 |
| 47% | 53% | 100% |
Relationship of BCL-6 gene mutations with other molecular features.
To determine whether the presence of BCL-6 mutations had any relationship to other molecular features previously reported,8,10,36 37 we compared our results with these previous molecular analyses as shown in Table 1. None of the polyclonal cases contained BCL-6 gene mutations, but only a subset of cases in which clonality was shown by the presence of Ig heavy chain rearrangements and/or EBV terminal repeat analysis contained BCL-6 gene mutations. The type of EBV and the presence of EBV-LMP 1 gene deletions did not show any correlation with the presence of mutations in the BCL-6 gene. A subset of cases with BCL-6 gene mutations, specifically, all but one of those classified as NHL or MM, contained structural alteration in one of the oncogenes/tumor suppressor genes examined (c-myc, p53, and N-ras), and all cases containing structural alterations in one of these genes had mutations in the BCL-6 gene.
DISCUSSION
Lymphoproliferative lesions occurring after solid organ transplantation have been difficult to classify into categories that reflect their pathobiology and behavior. Here we report the frequent presence of somatic mutations in the BCL-6 gene in PT-LPDs. The presence of these mutations is revealing in terms of understanding the biology of these lymphoid proliferations as well as mechanisms of tumor progression. Our findings show that BCL-6 gene mutations are a consistent step in the progression from a PT-LPD lesion that can be controlled by a reconstituted immune system to one that will require more aggressive therapeutic intervention. This is the first report of an objective parameter that apparently can distinguish between “hyperplastic” and “neoplastic” categories of PT-LPDs. This distinction is even true among the polymorphic lesions which, despite considerable histopathologic heterogeneity, possess indistinguishable immunophenotypic and molecular features. Therefore, we show that assessment of the presence of structural alterations in the BCL-6 gene is useful in predicting clinical responses and in guiding informed therapeutic strategies.
Our previous studies suggested that PT-LPDs are divisible into three clinicopathologic categories: (1) PH at the benign end of the spectrum; (2) NHL/MM at the malignant end; and (3) the polymorphic lesions, which include the histopathologic categories of polymorphic hyperplasia and polymorphic lymphoma, in the middle.8 However, we have not been able to identify molecular or clinical differences that consistently correlate with the morphological subdivision of the polymorphic lesions into hyperplasia and lymphoma categories. Age, stage of disease, time from transplantation to development of PT-LPD, and clinical outcome were not statistically significantly different between the two histopathologic subcategories of polymorphic PT-LPD.9 Furthermore, these polymorphic lesions are all clonal as determined by Ig gene rearrangement and EBV terminal repeat analysis, and they lack structural alterations in most of the genes involved in other lymphoid neoplasms, including c-myc, p53, ras, BCL-1, and BCL-2.8 We now show that BCL-6 gene mutations are common in the polymorphic PT-LPDs, but the presence of these mutations is not preferentially associated with the morphological subcategories of hyperplasia or lymphoma. However, the results of BCL-6 gene mutation analysis correlated well with clinical outcome, suggesting that these molecular studies may be more accurate than morphology in dividing PT-LPDs into the biological categories of hyperplasia and malignant lymphoma.
In this study, rearrangements of the BCL-6 gene were not identified by Southern blot analysis, distinguishing PT-LPDs from diffuse large B-cell lymphomas. However, because only a small number of PT-LPD lesions classified as NHL were examined, we cannot exclude the possibility that BCL-6 gene rearrangements occur more frequently among PT-LPDs than is reflected in this report. Our results confirm previous studies demonstrating that mutations can occur independently of rearrangements in the BCL-6 locus, and show that mutations are much more common than rearrangements in PT-LPDs.
A subset of PT-LPDs which remain poorly understood are those lacking EBV, which account for only 10% or less of all lesions. It seems that these frequently occur late after organ transplantation, and it has been suggested that these have poor clinical outcomes.38Among the cases included in this study, three cases lacked EBV, classified as PH (Case 8), PBCH (Case 12), and NHL (Case 33), respectively. Although there was no obvious difference between the first two EBV-negative cases and their EBV-positive counterparts, Case 33, classified as NHL, was different from other PT-LPDs in several respects. This case occurred 10 years after a kidney transplant, which is the longest interval we have seen between transplantation and appearance of the first PT-LPD, with all other cases having occurred between 6 weeks and 8 years with a median of 18.5 months. Furthermore, this is the only case of NHL in which we could not detect the presence of BCL-6 gene mutations, and the only case without these mutations which showed no response to therapy. It is possible that this case does not represent a true PT-LPD but rather a sporadic lymphoma presenting coincidentally in a patient with a history of renal transplantation. Although this case was nevertheless included for statistical purposes, this observation suggests that the presence or absence of BCL-6 gene mutations in EBV-negative cases may not be clinically significant. Studies of larger numbers of PT-LPD lesions, especially those negative for EBV, should help to clarify this issue.
Whereas functional characterization of BCL-6 is still in its early stages, BCL-6 is thought to be involved in germinal center formation.18,19 Mutations are always found in a 3.5-kb region spanning the first noncoding exon, and clustering in the 5′ region of the first intron,30 which was the only fragment analyzed in the present study. It is thought that this region contains an important regulatory element. Interestingly, although this is the same region in which chromosomal breakpoints in large-cell lymphomas tend to cluster, we have not identified molecular rearrangements in this region of BCL-6 in PT-LPDs.39Similar to previous studies,30,31 we have found that mutations are often multiple. This finding is consistent with the hypothesis that these mutations are caused by a mechanism similar to that responsible for Ig variable region gene hypermutation, although they can occur independently of translocation to Ig loci and in the absence of any recognizable rearrangement of BCL-6.30 BCL-6 protein is normally expressed in germinal centers. In neoplastic situations it is expressed in B-cell lymphomas thought to originate in germinal center or post–germinal center B cells, specifically, follicular lymphomas, diffuse large B-cell lymphomas, Burkitt's lymphoma, and lymphocyte-predominance Hodgkin's disease.40Furthermore, the BCL-6 gene has only been found to be altered in follicular, diffuse large-cell lymphomas, and AIDS-related NHLs.20,25,30,31,41 PT-LPDs are most likely derived from germinal center B cells. The germinal center is where the Ig variable region gene undergoes somatic hypermutation,42 and hypermutation in this region suggesting antigen selection has been reported in a small number of PT-LPDs.43 It remains to be determined whether mutations in the noncoding region of the BCL-6 gene are directly responsible for transformation of PT-LPDs, or are simply a reflection of an altered genetic stability or abnormal hypermutation mechanism, which in turn may result in alterations of other genes that are responsible for tumor progression. Regardless of the direct mechanism of transformation, alterations in the BCL-6 gene are the earliest genetic lesions identified thus far in the progression of PT-LPDs, occurring after clonal expansion and before mutations and rearrangements in other oncogenes (c-myc and N-ras) and tumor suppressor genes (p53). Thus, the presence of BCL-6 gene mutations seems to be a good early marker of progression from a reactive lesion that can still be controlled by the immune system to a malignant lymphoma.
In conclusion, this study suggests that the presence of BCL-6 gene mutations distinguish posttransplantation-associated lymphomas from hyperplasias. Furthermore, assessment of the presence of mutations in the BCL-6 gene provides an evaluable and objective parameter for tumor progression that does not depend on subjective histomorphological evaluation. Although our results should be confirmed in larger prospective studies, they indicate that the presence of mutations in the BCL-6 gene may be a useful clinical marker to determine whether a reduction in immunosuppression should be attempted or more aggressive therapy should be instituted.
ACKNOWLEDGMENT
We are grateful to Dr Cristina Sison for statistical analysis; to Drs Jonathan M. Chen, Daphne T. Hsu, Thomas J. Garrett, J. Gregory Mears, Steven Zangwill, Linda J. Addonizio, Robert E. Michler, and Gabriela Cesarman for submitting the PT-LPD tissues to our immunopathology laboratory and providing the relevant clinical information; to Dr Glauco Frizzera for assistance in the morphological classification of many of the cases presented in this study; and to Dr Elaine Schattner for critical review of this manuscript.
Supported in part by National Institutes of Health Grants No. CA73531 and CA68939 to E.C.
Address reprint requests to Ethel Cesarman, MD, PhD, The New York Hospital-Cornell Medical Center, Department of Pathology, 525 E 68th St, New York, NY 10021; e-mail: ecesarm@mail.med.cornell.edu.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal