The effect of recombinant human erythropoietin (rHuEpo) on megakaryopoiesis remains controversial. Treatment with rHuEpo in renal failure patients has been associated with a slight elevation of platelet counts. In animal studies, high doses of rHuEpo produced an increase of platelet counts followed by a gradual return to normal after 7 to 15 days or even a substantial degree of thrombocytopenia. However, because iron deficiency is also known to be associated with thrombocytosis, (functional) iron deficiency during rHuEpo could be contributing to these observations. We investigated the impact of iron supply on changes in platelet counts induced by rHuEpo. Rats were either fed normal food (normal rats) or received 1% carbonyl iron for 2 weeks or 3 months, as well as during the experiment, to achieve iron supplementation or overload, respectively. Rats of all three categories then received daily intravenous injections of rHuEpo (10, 50, or 150 U) or normal saline (0 U) for 20 days. With 0 to 10 U rHuEpo, platelets remained stable. In normal rats receiving 50 to 150 U rHuEpo, platelets increased to 120% to 140% of baseline at 4 to 12 days to level off at 120% at 16 to 20 days. This response was less sustained in splenectomized animals. Iron-supplemented rats receiving 50 to 150 U rHuEpo also increased platelets initially, but the peak was at day 4, followed by a gradual return to baseline and even a moderate thrombocytopenia later on. Iron-overloaded rats receiving 50 to 150 U rHuEpo also had increased platelets at day 4, but the duration of platelet increase was shorter, and they experienced a more pronounced degree of thrombocytopenia in proportion to the dose of rHuEpo. Because the early elevation of platelets was of larger magnitude than hematocrit changes, it is unlikely that it could be accounted for by shrinkage of plasma volume. Because it was observed in all three iron conditions, there appears to be some direct positive effect of rHuEpo on platelet production. However, after this transient effect, expanded erythropoiesis appears to exert a negative impact upon platelet production. Secondary thrombocytopenia was not related to splenic pooling, and its very slow correction after cessation of rHuEpo therapy is not compatible with changes in platelet survival. Rather, it is consistent with stem cell competition between erythroid and megakaryocytic development. However, this secondary thrombocytopenia is masked by (functional) iron deficiency in rats not receiving an adequate iron supply from food or stores.
ERYTHROPOIETIN (Epo) is the primary erythropoietic growth factor, but it has also been shown to affect platelet production. In large clinical trials of recombinant human Epo (rHuEpo) in renal failure patients, platelet counts increased significantly within 2 weeks and then gradually returned to pretreatment levels after months of maintenance therapy.1,2Mean platelet volumes decreased, but platelet counts remained unchanged in patients receiving rHuEpo and oral iron before scheduled surgery.3 In adult but not in infant monkeys, rHuEpo therapy resulted in elevated platelet counts throughout the 6-week treatment, followed by rapid normalization thereafter.4 In dogs, mice, or rats, short-term treatment with high doses of rHuEpo has been shown to stimulate platelet production, but platelet counts tended to normalize after 7 to 15 days.5-9 However, transgenic mice expressing the human Epo gene develop both polycythemia and a moderate degree of thrombocytopenia.10 Actually, large, chronic doses of rHuEpo also caused thrombocytopenia in mice, and stem cell competition between erythroid and platelet precursors has been suggested as the cause of this phenomenon.11
In a previous study of patients with end-stage renal disease, we demonstrated that platelet changes in response to rHuEpo therapy correlated with modifications of erythropoietic activity.2However, enhanced erythropoiesis is also associated with modifications of iron metabolism. In particular, functional iron deficiency, ie, an imbalance between iron needs in the bone marrow and iron supply from stores, may develop even in the presence of adequate storage iron when these stores cannot be mobilized rapidly enough.12 Iron deficiency has been shown to be associated with reactive thrombocytosis.13-17 Iron supplementation in iron-deficient infants18 or rats19 20 was rapidly followed by a return of platelet counts to normal levels.
Therefore, we undertook the present study to investigate the impact of iron supply on changes in platelet counts induced by rHuEpo. We studied the effect of various doses of rHuEpo and various durations of treatment on both erythropoiesis and megakaryopoiesis. We also examined the potential role of the spleen in this setting, because some studies had suggested that splenic pooling could interfere with these observations.7,21 22 We observed a diphasic pattern of response of platelet counts to rHuEpo, with the initial increment of platelet counts being followed by substantial thrombocytopenia. The study demonstrated that the iron status of the animals played an important role in the second phase of the diphasic response, with iron deficiency protecting them from thrombocytopenia.
MATERIALS AND METHODS
Animals.
Male Wistar rats were obtained from Janssen (Beerse, Belgium) and raised at the University of Liège (Liège, Belgium) from the age of 3 weeks through the end of the experiment. One group of animals (normal rats) was fed standard granular food. Other groups of rats were fed standard food in powder form supplemented with 1% (wt/wt) carbonyl iron (Sigma Chemical Co, St Louis, MO) 6 days per week and normal granular food 1 day per week, for a total of 2 weeks (supplemented rats) or 3 months (overloaded rats) before as well as during the experiment, to achieve iron supplementation or iron overload, respectively. Some animals underwent splenectomy under general anesthesia with ether (Gifer Barbezat, Dicenes, France) followed by placement of Autoclip Mikron clips (Becton Dickinson Benelux, Erembodegem-Alst, Belgium) for 10 days. They were then left to stabilize for 30 days before the experiment, and only animals showing no sign of inflammation at that time were used. Other rats underwent the same procedure but without splenectomy (sham-operated).
Epo therapy.
rHuEpo (Recormon) was kindly provided by Boehringer Mannheim (Brussels, Belgium). Rats were injected daily with intravenous rHuEpo at a dose of 10, 50, or 150 U/d for up to 20 days. Control animals (0 U rHuEpo) received the same volume of normal saline.
Laboratory analyses.
Blood samples were drawn from a tail vein under short ether anesthesia 3 times per week just before rHuEpo injections. Part of the blood was drawn on ACD formula A and part on heparin to be centrifuged to obtain plasma, which was frozen at −20°C until processing. Complete blood counts were measured on a Technicon H1 automatic cell counter (Technicon, Tarrytown, NY), with appropriate corrections for dilution by ACD. Preliminary experiments showed that a minor proportion of the smaller rat platelets could not be detected by the counter. However, this fraction was constant from rat to rat as well as over time and platelet volume did not change during rHuEpo therapy. Expressing the results as the percentage of baseline values thus eliminated this problem. The small fraction of larger platelets was appropriately detected. The percentage of reticulocytes was determined by cytofluorometry on a FACSCAN cytofluorometer (Becton Dickinson, San Jose, CA) after coloration with thiazole orange.23Preliminary experiments showed that this automated method gave results similar to manual counting on blood smears colored with brilliant cresyl blue. Plasma soluble transferrin receptor (sTfr) was measured as previously described with minor modifications.24,25 After varying durations of treatment, a subset of the animals were exsanguinated from the abdominal aorta and perfused with 20 to 30 mL saline solution. The spleen was removed and weighted. Nonheme iron was extracted from the liver,26 and iron concentration was determined by proton-induced x-ray emission.27 Serum iron (SeFe) and total iron binding capacity (TIBC) were measured using standard methods,28 and transferrin saturation was derived from these figures.
Statistical methods.
All results were expressed as percentages of a baseline value and expressed as the mean ± standard deviation (M ± SD). Comparisons of baseline values with later measurements in the same group of animals were performed using paired Student’st-tests. Comparisons between groups were performed with Student’s t-tests, with Welsch’s correction in case of unequal variances. Most statistical analyses were performed with the Excel 97 (Microsoft Corp, Redmond, WA) or Prism 2.0 (GraphPad Software Inc, San Diego, CA) software.
RESULTS
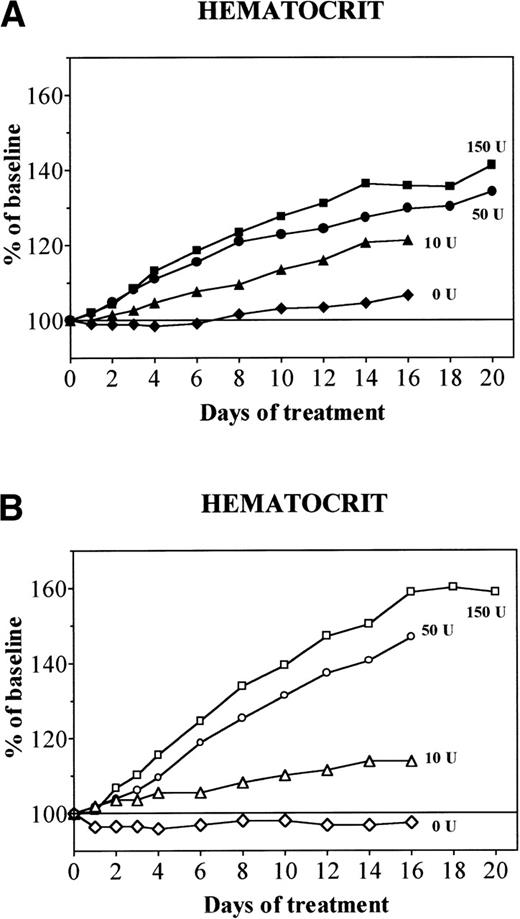
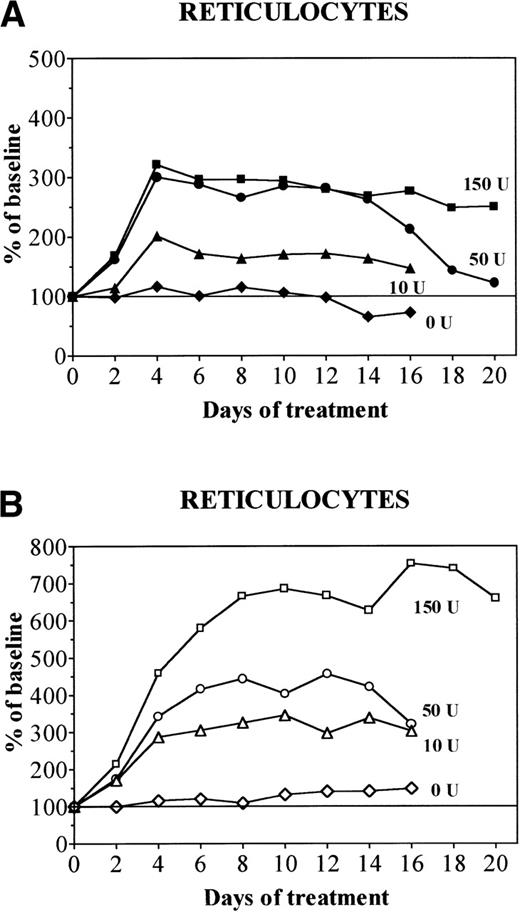
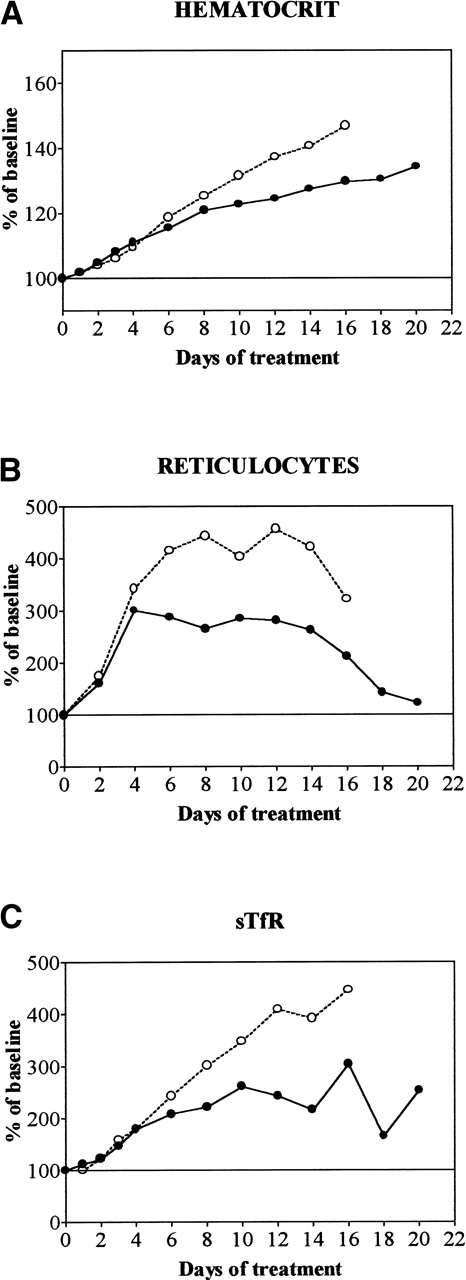
During treatment with rHuEpo, a progressive erythroid response was observed and its amplitude was similar in unmanipulated, sham-operated, or splenectomized animals. This response was proportional to the dose of rHuEpo (Figs 1 and2). Low doses (10 U) of rHuEpo produced some increment of hematocrit (Hct; Fig 1) and reticulocytes (Fig 2) without any change in sTfR levels, suggesting that this was achieved through shift reticulocytosis rather than true stimulation of erythropoiesis. Higher doses caused more substantial increases of sTfR, reticulocytes, and Hct. The iron status of the animals strongly modulated the erythroid response, being significantly more prominent in overloaded rats compared with supplemented and normal rats, even if the initial slope of Hct increase was similar in overloaded compared with normal rats (Fig3). After 20 days of treatment with 150 U rHuEpo, the Hct of overloaded rats attained a plateau at 160% of baseline values, whereas normal rats only achieved a 135% plateau (Fig 1). Reticulocytes attained levels 7 times versus 3 times baseline in overloaded and normal animals, respectively (Fig 2).
Evolution of Hct during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of Hct during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of absolute reticulocyte count during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of absolute reticulocyte count during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of Hct, absolute reticulocyte count, and sTfR during treatment with daily doses of 50 U rHuEpo in normal (•) or overloaded (○) rats. Results are expressed as percentages of baseline value. (A) Hct; (B) absolute reticulocyte count; (C) sTfR.
Evolution of Hct, absolute reticulocyte count, and sTfR during treatment with daily doses of 50 U rHuEpo in normal (•) or overloaded (○) rats. Results are expressed as percentages of baseline value. (A) Hct; (B) absolute reticulocyte count; (C) sTfR.
Spleen weight remained stable with 0 or 10 U rHuEpo, but increased significantly in all categories of animals receiving 50 to 150 U per day (Table 1). The storage (liver) and functional (plasma) iron pools were not modified with 0 or 10 U rHuEpo, but when modified with higher doses of rHuEpo, were significantly depleted compared with baseline (Table 1). With 50 to 150 U rHuEpo, normal rats showed depletion of the functional as well as storage pools consistent with iron deficiency, supplemented rats had functional iron deficiency but iron stores were equivalent to those of untreated normal rats, and overloaded rats retained adequate plasma iron levels in the presence of elevated stores.
Serum Iron, Liver Nonheme Iron, and Spleen Weight in Normal, Supplemented, and Overloaded Rats Treated for 0, 4, or 16 Days With 0, 10, 50, or 150 U rHuEpo Per Day
| Category . | Dose of rHuEpo (U/d) . | Duration of Treatment (d) . | SeFe (μd/dL) . | Liver Nonheme Fe (μg) . | Spleen Weight (mg) . |
|---|---|---|---|---|---|
| Normal | — | Baseline | 64 ± 10 | 326 ± 156 | 491 ± 67 |
| 0 | 4 | 73 ± 16 | 385 ± 89 | 527 ± 75 | |
| 16 | 54 ± 15 | 341 ± 60 | 524 ± 48 | ||
| 10 | 4 | 56 ± 8 | 312 ± 51 | 635 ± 105 | |
| 16 | 59 ± 30 | 318 ± 114 | 567 ± 72 | ||
| 50 | 4 | 25 ± 12* | 292 ± 177 | 845 ± 167† | |
| 16 | 23 ± 11* | 131 ± 33† | 861 ± 148* | ||
| 150 | 4 | 8 ± 4‡ | 267 ± 106 | 1,187 ± 144‡ | |
| 16 | 13 ± 4‡ | 115 ± 9† | 1,105 ± 117‡ | ||
| Supplemented | — | Baseline | — | — | — |
| 0 | 16 | 80 ± 3 | 1,042 ± 92 | 485 ± 26 | |
| 50 | 16 | 64 ± 24 | 383 ± 266† | 1,453 ± 2071-153 | |
| 150 | 16 | 24 ± 111-153 | 276 ± 88‡ | 1,508 ± 2071-153 | |
| Overloaded | — | Baseline | 132 ± 26 | 5,376 ± 1,128 | 687 ± 83 |
| 0 | 16 | 113 ± 19 | 4,203 ± 1,602 | 566 ± 90 | |
| 10 | 16 | 76 ± 11 | 4,601 ± 1,058 | 676 ± 23 | |
| 50 | 16 | 57 ± 10* | 2,333 ± 9421-153 | 1,103 ± 118* | |
| 150 | 16 | 58 ± 7* | 2,282 ± 1,7101-153 | 2,003 ± 571† |
| Category . | Dose of rHuEpo (U/d) . | Duration of Treatment (d) . | SeFe (μd/dL) . | Liver Nonheme Fe (μg) . | Spleen Weight (mg) . |
|---|---|---|---|---|---|
| Normal | — | Baseline | 64 ± 10 | 326 ± 156 | 491 ± 67 |
| 0 | 4 | 73 ± 16 | 385 ± 89 | 527 ± 75 | |
| 16 | 54 ± 15 | 341 ± 60 | 524 ± 48 | ||
| 10 | 4 | 56 ± 8 | 312 ± 51 | 635 ± 105 | |
| 16 | 59 ± 30 | 318 ± 114 | 567 ± 72 | ||
| 50 | 4 | 25 ± 12* | 292 ± 177 | 845 ± 167† | |
| 16 | 23 ± 11* | 131 ± 33† | 861 ± 148* | ||
| 150 | 4 | 8 ± 4‡ | 267 ± 106 | 1,187 ± 144‡ | |
| 16 | 13 ± 4‡ | 115 ± 9† | 1,105 ± 117‡ | ||
| Supplemented | — | Baseline | — | — | — |
| 0 | 16 | 80 ± 3 | 1,042 ± 92 | 485 ± 26 | |
| 50 | 16 | 64 ± 24 | 383 ± 266† | 1,453 ± 2071-153 | |
| 150 | 16 | 24 ± 111-153 | 276 ± 88‡ | 1,508 ± 2071-153 | |
| Overloaded | — | Baseline | 132 ± 26 | 5,376 ± 1,128 | 687 ± 83 |
| 0 | 16 | 113 ± 19 | 4,203 ± 1,602 | 566 ± 90 | |
| 10 | 16 | 76 ± 11 | 4,601 ± 1,058 | 676 ± 23 | |
| 50 | 16 | 57 ± 10* | 2,333 ± 9421-153 | 1,103 ± 118* | |
| 150 | 16 | 58 ± 7* | 2,282 ± 1,7101-153 | 2,003 ± 571† |
P values are given for comparisons with rats of the same category in baseline conditions.
P < .001.
P < .05.
P < .0001.
P < .01.
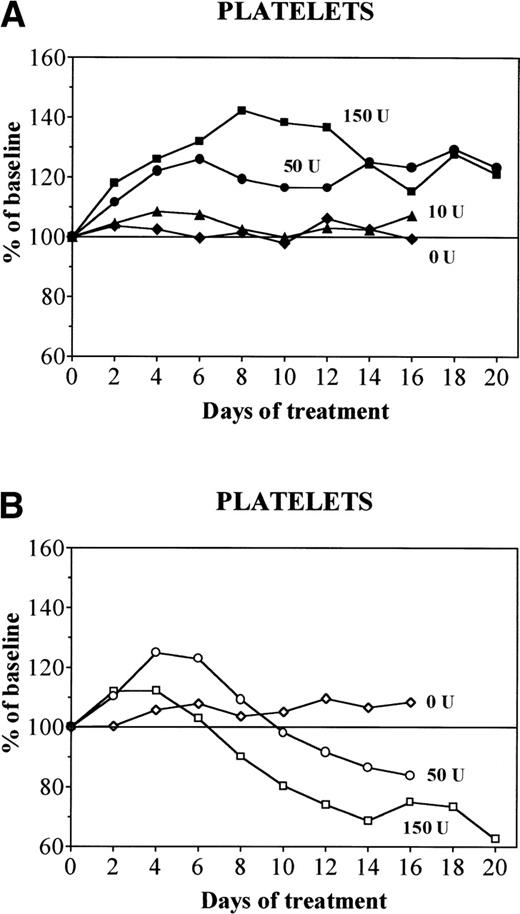
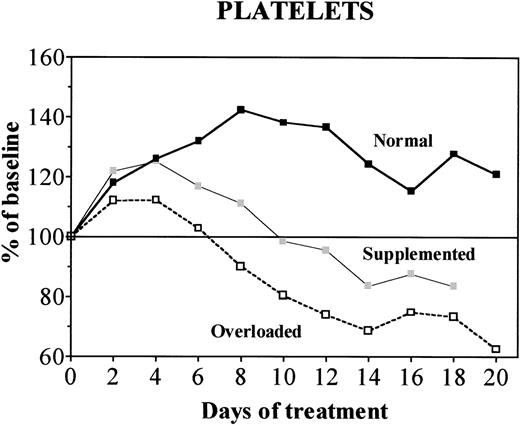
In normal rats, treatment with rHuEpo produced dose-dependent effects on platelet counts (Fig 4A). With 10 U rHuEpo per day, platelets remained stable and comparable to levels observed with 0 U. On the other hand, with 50 U rHuEpo platelet counts increased to 120% of baseline after 4 days and remained stable thereafter. With 150 U rHuEpo daily, they increased to 140% of baseline by day 8 to progressively level off at 120% at 14 to 20 days (Figs 4A and 5). In animals receiving 0 U rHuEpo, supplemented or overloaded (Fig 4B) rats behave similarly to normal rats. Supplemented rats receiving 50 to 150 U rHuEpo also increased platelets initially, but the peak was at day 4, followed by a gradual return to baseline by day 10 and a moderate degree of thrombocytopenia later on (Fig 5). Overloaded rats receiving 50 to 150 U rHuEpo also increased platelets at day 4. However, the duration of platelet increase was shorter and the importance of secondary thrombocytopenia was more pronounced (Figs 4B and 5). This occurred in proportion to the dose of rHuEpo and reached 60% of baseline with 150 U rHuEpo per day for 20 days (Fig 4B).
Evolution of platelet counts during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of platelet counts during treatment with daily doses of 0 (diamonds), 10 (triangles), 50 (circles), or 150 (squares) U rHuEpo. Results are expressed as percentages of baseline value. (A) Normal rats (solid symbols); (B) overloaded rats (open symbols).
Evolution of platelet counts during treatment with daily doses of 150 U rHuEpo in normal (▪), supplemented (▩), or overloaded (□) rats. Results are expressed as percentages of baseline value.
Evolution of platelet counts during treatment with daily doses of 150 U rHuEpo in normal (▪), supplemented (▩), or overloaded (□) rats. Results are expressed as percentages of baseline value.
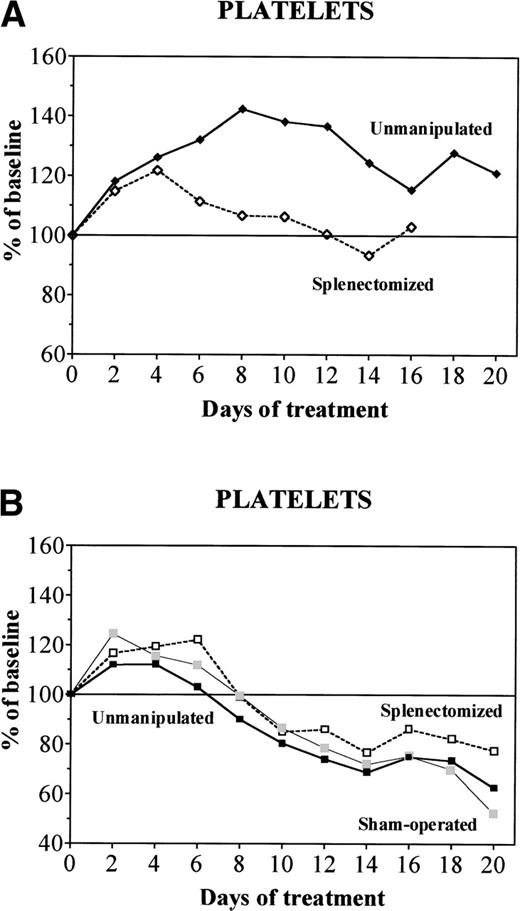
In normal animals previously splenectomized, treatment with high doses of rHuEpo was associated with a transient elevation of platelet counts peaking at day 4 before progressively returning to baseline, whereas unmanipulated animals maintained increased platelet counts throughout the experiment (Fig 6A). This contrasted with supplemented or overloaded rats (Fig 6B), in which unmanipulated, sham-operated, or splenectomized animals behave similarly, ie, first increased platelet counts and then developed secondary thrombocytopenia with high doses of rHuEpo.
Evolution of platelet counts during treatment with daily doses of 150 U rHuEpo in unmanipulated (solid symbols), sham-operated (shaded symbols), or splenectomized (open symbols) rats. Results are expressed as percentages of baseline value. (A) Normal rats (diamonds); (B) overloaded rats (squares).
Evolution of platelet counts during treatment with daily doses of 150 U rHuEpo in unmanipulated (solid symbols), sham-operated (shaded symbols), or splenectomized (open symbols) rats. Results are expressed as percentages of baseline value. (A) Normal rats (diamonds); (B) overloaded rats (squares).
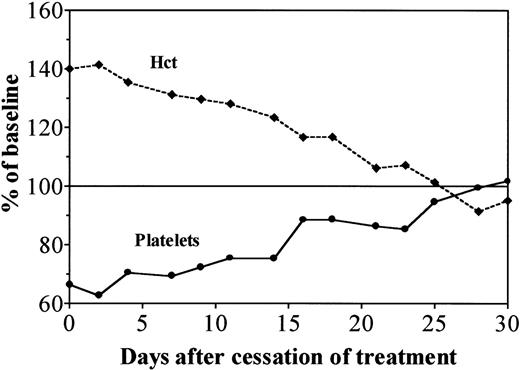
Treatment with 150 U rHuEpo was stopped after 20 days and rats were followed-up for 30 days after cessation of therapy (Fig 7). The Hct, reticulocytes, and sTfR levels decreased progressively, whereas platelet counts recovered in parallel over a period of 4 weeks. The evolution was identical in unmanipulated, sham-operated, or splenectomized animals.
Evolution of Hct (---) and platelet counts (—) after cessation of treatment with daily doses of 150 U rHuEpo in overloaded rats. Results are expressed as percentages of baseline value.
Evolution of Hct (---) and platelet counts (—) after cessation of treatment with daily doses of 150 U rHuEpo in overloaded rats. Results are expressed as percentages of baseline value.
DISCUSSION
In the present study, animals receiving 10 U rHuEpo did not experience changes in platelet counts but had some increase in Hct and reticulocytes. However, as this happened without mobilization of storage iron and without increase in sTfR levels (the best quantitative measure of total erythropoiesis), this was probably achieved through shift reticulocytosis rather than true stimulation of erythropoietic activity. Rats treated with higher doses of rHuEpo underwent a true expansion of erythropoiesis, translating into progressive elevation of all erythroid parameters. Normal animals soon became limited in their capacity to respond because of the occurrence of iron deficiency. The augmentation of erythropoietic activity continued further in overloaded rats and these animals attained much higher sTfR values. Soluble TfR levels, thought in some situations to be a marker of (functional) iron deficiency,24 are therefore much more sensitive to changes in total erythropoietic activity than to changes in iron availability. This is consistent with our previous finding that patients with functional iron deficiency before treatment did not increase sTfR levels in response to rHuEpo.29
Our results confirm that high doses of rHuEpo induce significant changes in platelet counts. The platelet response appeared to undergo two different phases, ie, an initial moderate thrombocytosis and a secondary more pronounced thrombocytopenia. This diphasic pattern of response has already been described in animal models of hypoxia30-33 but not in models of rHuEpo therapy.
The initial increment in platelet counts was initiated within 48 hours of starting rHuEpo therapy and developed in a dose-dependent fashion. This short-term elevation of platelet counts could be accounted for by several mechanisms, including changes in plasma volume or platelet survival and stimulation of megakaryocyte activity or global marrow function. Proportional shrinkage of plasma volume occurs only after rHuEpo treatment has produced changes in the red blood cell (RBC) mass.34 Furthermore, simultaneous elevations of RBCs and platelets should then be observed, but this was not the case in renal failure patients.2 An effect of rHuEpo on platelet survival has never been demonstrated, and there is no reason why this would be limited to patients in whom RBC production is adequately stimulated.2 A number of in vitro data support the concept that Epo directly stimulates megakaryopoiesis. Megakaryocytes have been shown to express constitutive35 or inducible36,37 high-affinity binding sites for Epo, resulting in enhanced growth in the presence of Epo.38 In vitro studies in humans as well as in mice have demonstrated that Epo promotes megakaryocytic colony formation and increases the size, ploidy, and number of megakaryocytes, as well as their DNA and protein synthesis and cytoplasmic process formation.38-42 Instead of directly stimulating megakaryocytes, Epo could also promote platelet production indirectly by enhancing global hematopoietic activity. Treatment of patients with end-stage renal failure rapidly resulted in an increase of not only erythroid progenitors, but also of colony-forming units megakaryocytes (CFU-Meg) and colony-forming unit–granulocyte-macrophage (CFU-GM).43 In such patients, platelet increments correlated with the degree of expansion of erythropoietic activity and platelet counts did not change in nonresponders until the Epo dose was increased and erythropoiesis begun to expand.2 In chronic liver disease, rHuEpo therapy ameliorates platelet counts in patients who also show a response of the erythroid lineage.44 In mice, elevated platelet counts correlated with increased Hct after 5 days of rHuEpo therapy.7 These observations suggest that the Epo effect on platelet formation parallels its effect on RBC production.
In animals with adequate iron supply, the initial elevation of platelet counts rapidly gave way to a substantial degree of thrombocytopenia. This also developed in a dose-dependent manner, with the decrease occurring earlier and being more pronounced in animals receiving higher doses of rHuEpo. In previous studies with rHuEpo, the initial elevation of platelet counts was followed by a return of platelets to control levels after 7 or 15 days.6,7 Actually, large, chronic doses of rHuEpo caused thrombocytopenia, decreased seleno-methionine incorporation into platelets, and reduced number of megakaryocytes in normal mice.11 Transgenic mice expressing the human Epo gene developed both polycythemia and a moderate degree of thrombocytopenia.10 Similarly, chronic hypoxia decreased platelet production,30-33,45 and this was shown to result from decreased differentiation of hematopoietic precursors into the megakaryocytic lineage.31,46 Increased erythropoiesis and not elevated RBCs (as produced by transfusion) was required for the thrombocytopenia to occur.33,47 Conversely, acute thrombocytopenia caused decreased erythropoiesis in some studies.11 Short-term thrombopoietin (Tpo) treatment in normal mice48 as well as chronic exposure to Tpo after gene transfer49 induced erythroid hypoplasia. However, this was at least partially explained by the development of myelofibrosis. Finally, Epo-induced thrombocytopenia is very unlikely to be due to increased platelet destruction, as observed with other growth factors such as macrophage colony-stimulating factor (M-CSF).50 During Epo-induced thrombocytopenia, there is substantial suppression of megakaryopoiesis11,31,46 and no change in platelet survival.30 Furthermore, recovery of a normal platelet count took several weeks after cessation of rHuEpo therapy, a finding difficult to reconcile with recovery after ending activation of the reticulo-endothelial system.
All this is suggestive of a pattern of reciprocal changes in erythropoiesis and megakaryopoiesis. Therefore, stem cell competition between erythroid and platelet precursors has been suggested to occur in these situations of prolonged, intense stimulation.11Recent data support the concept that megakaryocytic and erythrocytic cell lineages share a common precursor.51Multipotential37 or bipotential52-54 cell lines expressing Epo receptors37,53 have been obtained in which erythroid differentiation can be induced through the action of Epo37,52 and megakaryocytic differentiation by Tpo.52,54 Such a bipotent erythro-megakaryocytic progenitor has also been characterized in normal human bone marrow,55coexpressing glycophorin A and glycoprotein IIIa.56
The effect of rHuEpo on platelet counts was strongly modulated by the iron status of the animals. Thrombocytopenia occurred earlier and was more pronounced in overloaded rats (no iron deficiency) than in supplemented animals (functional iron deficiency). Normal animals developed iron deficiency with depletion of iron stores that resulted in apparent protection from Epo-induced thrombocytopenia. Iron deficiency has been shown to be associated with thrombocytosis,13-17 but platelet counts tend to normalize19,20,57 and thrombocytopenia can even occur18,58,59 when iron deficiency becomes very severe. This is consistent with the diphasic pattern of majored stimulation by endogenous Epo. Iron therapy ensures correction of platelet counts in infants18 or in rats19,20 with moderate iron deficiency, but has little effect in rats with severe iron deficiency anemia and normal platelet counts.19,20 In cases with very severe iron deficiency, iron therapy may even be associated with thrombocytopenia.60 Therefore, the effects of iron status and iron therapy on platelet production depend on the severity of iron deficiency.
However, changes in platelet counts during iron deficiency anemia could represent in part an effect of increased endogenous Epo stimulation in response to the anemia rather than an effect of iron deficiency per se. With moderate iron deficiency, a modest increase in serum Epo would stimulate platelet production, whereas with more severe anemia a major Epo response would engender thrombocytopenia. Accordingly, transfusion of RBCs into iron-deficient rats decreases platelet production, whereas transfusion into normal animals has no effect.20 In patients with renal failure receiving moderate doses of rHuEpo, relative platelet increments over baseline correlated inversely with relative changes of serum iron or transferrin saturation (an indication of erythroid marrow activity) rather than with absolute serum iron and transferrin saturation values (an indication of functional iron deficiency) or with ferritin levels (an indication of iron stores), emphasizing the role of marrow response to rHuEpo rather than that of iron deficiency alone.2 Our results in overloaded animals also show that the early stimulatory effect of rHuEpo on platelet production is a direct effect of treatment rather than an indirect effect of iron deficiency. Nevertheless, our data also show that with high doses of rHuEpo thrombocytopenia develops in inverse relationship to the degree of iron deficiency. This indicates that iron deficiency per se plays an important protective role against thrombocytopenia induced by high doses of rHuEpo in the presence of adequate iron supply.
Normal splenectomized animals showed a much less sustained platelet response to rHuEpo therapy compared with unmanipulated rats, but this discrepancy was no longer apparent in supplemented or overloaded rats (Fig 6). Previous studies in mice have shown that the stimulation effect of rHuEpo on megakaryocyte and CFU-Meg numbers may be limited to the spleen in intact mice and become significant in the bone marrow only after splenectomy.7,21,22 Splenectomized animals may thus be unable to maintain the positive response to rHuEpo observed in intact animals. It could also be possible that these rats experienced a higher degree of marrow erythroid expansion compensating for the absence of the spleen, thereby creating more competition with platelet production. However, this was no longer true in supplemented or overloaded rats. Splenic hematopoiesis may be less sensitive to Epo-induced competition, explaining why hypoxia is associated with a normal absolute number of megakaryocytes in the spleen61,62and why splenectomy causes a further degree of hypoxia-induced thrombocytopenia in hypertransfused mice.63
A question remaining to be examined in further studies is whether the effects of rHuEpo on platelet production are a result of the dose itself or of the magnitude of the erythropoietic effect of that dose. For example, could a lower dose administered in a patient with decreased marrow function (because his number of hematopoietic progenitors is decreased by postchemotherapy stem cell damage or in the context of transplantation) bring about the same biological effects as those induced by higher doses of rHuEpo in the presence of a normal marrow function?
Supported in part by Grants No. 3.4555.91, 3.4621.94, and 7.4538.96 from the FNRS. M.L. was supported by a grant from “Télévie” (FNRS, Belgium) and by a grant from the “Fondation Frédéricq” (University of Liège, Belgium). Y.B. is a Senior Research Associate of the National Fund for Scientific Research (FNRS, Belgium).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Yves Beguin, MD, University of Liège, Department of Hematology, CHU Sart-Tilman, 4000 Liège, Belgium; e-mail: yves.beguin@chu.ulg.ac.be.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal