Abstract
The C-C chemokine receptors CCR5 and CCR3 are fusion coreceptors for human immunodeficiency virus (HIV) entry into macrophages. The regulation of their expression influences infectivity by HIV. We report here that interferon-γ (IFN-γ) a cytokine that has bidirectional effects on HIV infection of macrophages, significantly upregulated CCR5 and CCR3 cell surface expression in human mononuclear phagocytes isolated from placental cord blood and adult peripheral blood. Monocytes treated with IFN-γ showed increased chemotaxis to the CCR5 ligands macrophage inflammatory protein-1 (MIP-1) and MIP-1β, confirming the functional relevance of IFN-γ–induced CCR5 expression. However, IFN-γ suppressed HIV entry into macrophages. Interestingly, we demonstrated that IFN-γ inhibited cell surface expression of CD4, the major receptor for HIV. This finding may explain the suppressive effect of IFN-γ on HIV entry into macrophages, despite its enhancing effect on the expression of CCR5 and CCR3 by these cells. In addition, IFN-γ–induced secretion of C-C chemokines (RANTES, MIP-1, and MIP-1β) by mononuclear phagocytes may also suppress HIV entry into macrophages. These data provide further evidence for cytokine-mediated regulation of CCR5 expression and are consistent with a novel paradigm in which cytokines regulate HIV infection and leukocyte migration by reciprocal and opposing effects on the expression of CD4 and chemokine receptors.
INTERFERON-γ (IFN-γ), a cytokine with multiple immunoregulatory effects, mediates host defence against several infections and is a potent activator of mononuclear phagocytes.1 The role of IFN-γ in modulating human immunodeficiency virus (HIV) infection is well established. IFN-γ has been shown to have suppressive as well as enhancing effects on HIV replication.2-4 However, the underlying mechanisms are incompletely understood. IFN-γ secretion is dysregulated in children with perinatally transmitted HIV infection.5 6
Chemokines are chemotactic cytokines of which there are two main classes: C-X-C (α) chemokines, which are primarily active on neutrophils, and C-C (β) chemokines, which act on several leukocyte populations (monocytes, basophils, eosinophils, and natural killer [NK] cells).7 Chemokines bind to and activate seven-transmembrane domain receptors.7 Chemokines and their receptors play a crucial role in immune and inflammatory reactions and in HIV infection. The C-C chemokine receptors CCR5, CCR2b, and CCR3 are fusion coreceptors for HIV entry into macrophages.8-12 Of these, CCR5 is a major determinant of HIV entry into macrophages.8-12 Individuals with homozygous mutant of CCR5 are highly resistant to HIV infection.13 Therefore, the expression pattern of CCR5 and its regulation are thought to influence HIV infection and acquired immunodeficiency syndrome (AIDS) pathogenesis. Three C-C chemokines that are ligands for CCR5—RANTES (regulated upon activation, normal T-cell expressed and secreted), macrophage inflammatory protein-1α (MIP1-α), and MIP1-β—inhibit HIV infection of macrophages and are being investigated as potential therapeutic agents in HIV infection.14 15 Although the roles of CCR5 and C-C chemokines in HIV infection are well established, little is known about the regulation of the C-C chemokine system. Understanding the regulation of HIV coreceptors will help to elucidate the interplay between these receptors and HIV in the pathogenesis of AIDS. Therefore, we investigated the in vitro effect of IFN-γ on CCR5 expression in mononuclear phagocytes isolated from placental cord blood and adult peripheral blood.
MATERIALS AND METHODS
Cells.
Monocytes were obtained according to our previously described technique16 from the cord blood of healthy, term neonates and healthy adult donors. In brief, mononuclear cells were separated by centrifugation for 45 minutes over Lymphocyte Separation Medium (LSM; Organon Teknika Corp, Durham, NC) at 1,500g. The mononuclear cell layer was collected and incubated with Dulbecco’s modified Eagle medium (DMEM) in gelatin-coated flasks for 45 minutes at 37°C, followed by washing off nonadherent cells with DMEM. After detachment with ethylenediamine tetra-acetic acid (EDTA), monocytes were resuspended in DMEM supplemented with 10% fetal bovine serum, 2 mmol/L glutamine, penicillin (100 U/mL), streptomycin (100 μg/mL), and nonessential aminoacids and plated in 48-well culture plates at a density of 106 cells/mL. The monocytes were greater than 97% pure as assessed by fluorescence-activated cell sorting using monoclonal antibody (MoAb) against CD14 (Leu-M3). Freshly isolated monocytes (within 48 hours postisolation) and monocyte-derived macrophages (MDM; 7 to 8 days postisolation) were used for the study.
Reagents.
Human recombinant IFN-α, IFN-β, and IFN-γ and polyclonal blocking rabbit antihuman IFN-γ antibody were obtained from Genzyme (Cambridge, MA). Monoclonal mouse antibodies to CCR5 (2D7) and CCR3 (7B11) from LeukoSite Inc (Cambridge, MA) were obtained through the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH (Rockville, MD). Fluorescein-conjugated (FITC) goat antimouse antibody, CD4-FITC, IgG1-FITC, and IgG2a-FITC were obtained from Immunotech (Westbrook, ME). Recombinant human MIP-1α and MIP-1β and enzyme-linked immunosorbent assay (ELISA) kits for MIP-1α, MIP-1β, and RANTES were purchased from R&D Systems (Minneapolis, MN).
Flow cytometry.
To determine CCR5 and CCR3 expression by indirect immunofluorescence, 2 × 105 monocytes or MDM were suspended in 100 μL of phosphate-buffered saline (PBS; 1×) and incubated first with unlabeled CCR5 antibody (2D7) or CCR3 antibody (7B11) for 30 minutes at 4°C. The cells were then washed twice with PBS and incubated with the second antibody, fluorescein-conjugated goat antimouse antibody, for 30 minutes at 4°C. After washing again with PBS, the cells were fixed with 1% paraformaldehyde in PBS. CD4 expression was determined by direct immunofluorescence. Fluorescein-conjugated control antibodies were isotype-matched for CCR5/CCR3 (IgG2a) and CD4 (IgG1). Fluorescence was analysed on an EPICS-elite flow cytometer (Beckman-Coulter Electronics, Hialeah, FL). In some cases, results are expressed as the relative fluorescence intensity (RFI), calculated according to the formula: RFI = mean fluorescence (sample) − mean fluorescence (control)/mean fluorescence (control).
Polymerase chain reaction (PCR) analysis for CCR5.
Total cellular RNA was extracted by the single-step, acid guanidium thiocyanate-phenol-chloroform extraction. Total RNA (1 μg) was reverse transcribed using Reverse Transcription System (Promega, Madison, WI) with the specific primers for CCR5 (antisense) for 1 hour at 42°C, and the resulting cDNA was used as a template for PCR amplification. PCR amplification was performed with one tenth of the cDNA for 40 cycles with AmpliTaq Gold (Perkin Elmer, Branchburg, NJ) in a GeneAmp PCR system 2400 (Perkin Elmer-Cetus, Norwalk, CT). The PCR reaction mixture contained 0.2 mmol/L of dNTPs, 20 pmol/L of each of two primers, and 1.5 U of AmpliTaq Gold in 1× reaction buffer (Perkin Elmer). Each PCR amplification consisted of heat inactivation of AmpliTaq Gold for 8.5 minutes at 94°C, followed by 5 cycles of 94°C for 1 minute, 55°C for 1 minute, and 72°C for 1.5 minutes; 35 cycles of 94°C for 30 seconds, 60°C for 30 seconds, and 72°C for 45 seconds; and elongation at 72°C for 7 minutes, using the specific primers for CCR5: 5′ CAAAAAGAAGGTCTTCATTACACC 3′ (sense); 5′ CCTGTGCCTCTTCTTCTCATTTCG 3′ (antisense).13 Quantification of CCR5 mRNA was performed by a competitive PCR procedure using a competitor DNA fragment carrying the identical primer recognition sites for CCR5. The competitor DNA fragment was constructed using PCR MIMIC construction kit (Clontech, Palo Alto, CA). Increasing dilutions of the competitive templates were added to the same amount of cDNA from the samples. The cycle conditions were the same as those mentioned above. Amplification products were resolved by 4% agarose gel electrophoresis and quantified by densitometric scanning. According to the principles of competitive PCR, quantification of the target molecules in the samples was obtained by estimation of the ratio between the amplification products (ratio of competitor to CCR5). β-Actin was used as the control to monitor the amount and integrity of RNA in each sample.
Chemotaxis.
Monocytes were incubated with or without IFN-γ (10, 100, 500, and 1,000 U/mL) for 12 hours in Teflon wells. Cell migration was measured in 96-well chemotaxis chambers (Neuro Probe Inc, Cabin John, MD). Thirty microliters of chemoattractant solution (MIP-1α or MIP-1β) at a concentration of 10 ng/mL or control medium (DMEM with 1% fetal calf serum [FCS]) was added to the lower wells of a chemotaxis chamber. A polycarbonate filter (5-μm pore size; Neuro Probe) was layered onto the wells. Twenty-seven microliters of cell suspension (1.5 × 106 monocytes/mL) were seeded in the wells in the upper part of the filter. The chamber was incubated at 37°C in air with 5% CO2 for 2 hours. At the end of the incubation, filters were removed and fixed and the number of cells in five high-power oil-immersion fields were counted. All assays were performed in triplicate.
Luciferase reporter virus entry assay.
Recombinant luciferase-encoding HIV virions pseudotyped with M-tropic ADA Env were used to study HIV infectability of untreated and IFN-γ–treated MDM. The plasmid encoding HIV ADA was provided by John Moore (Aaron Diamond AIDS Research Center, New York, NY), and the NL4-3 luciferase virus backbone was provided by Ned Landau (Aaron Diamond AIDS Research Center). In brief, NL4-3-Luc-R−E− virus stocks pseudotyped by ADA were generated by transfecting 293T cells with NL4-3-Luc-R−E− and pSV7d-based expression vectors encoding HIV ADA. Virus-containing supernatants were collected 48 hours posttransfection and frozen at −70°C. MDM at a concentration of 1 × 106 cells/mL in 48-well plates were infected for 4 hours with 100 μL of the supernatants (50 ng of p24gag virus). At 72 hours postinfection, the cells were lysed in 150 μL of 0.5% Triton-X-100 in 1× PBS. Luciferase activity was determined in 50 μL of each lysate in a Wallac Trilux Microbeta luminometer (Wallac, Turku, Finland).
HIV infection and reverse transcriptase (RT) assay.
MDM at a concentration of 1 × 106 cells/mL in 48-well plates were infected by adding 0.05 mL of HIV BaL virus (5 × 105 cpm/mL of RT activity) to each well. After 3 hours the inoculum was removed and the cells were washed three times with DMEM to remove unabsorbed virus. Supernatants were tested for RT activity every 5 days. To determine the level of RT activity, 10 μL of culture supernatants was added to 50 μL of a cocktail containing poly (A), oligo (dt), MgCl2, Nonidet p-40, and [32P]dTTP and incubated for 20 hours at 37°C. Thirty microliters of the reaction mixture was then spotted on DE 81 paper and air-dried. The filters were then washed in 2× standard saline citrate (SSC; 0.3 mol/L NaCl/0.03 mol/L sodium citrate, pH 7) and 100% ethanol, dried, cut, and placed in a scintillation counter (LS 7000; Beckman Instruments, Inc, Palo Alto, CA) for measurement of radioactivity.
Statistical analysis.
The data were analyzed using the Student’s t-test for paired samples.
RESULTS
Effect of IFN-γ on CCR5 expression in mononuclear phagocytes.
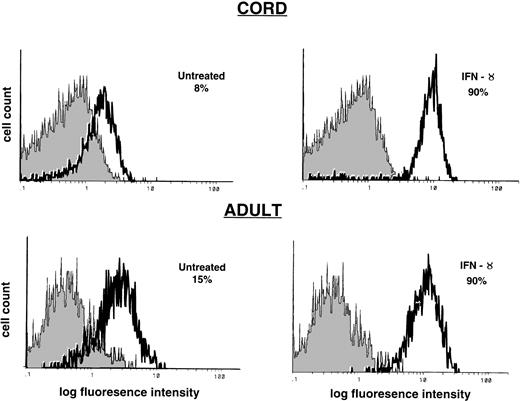
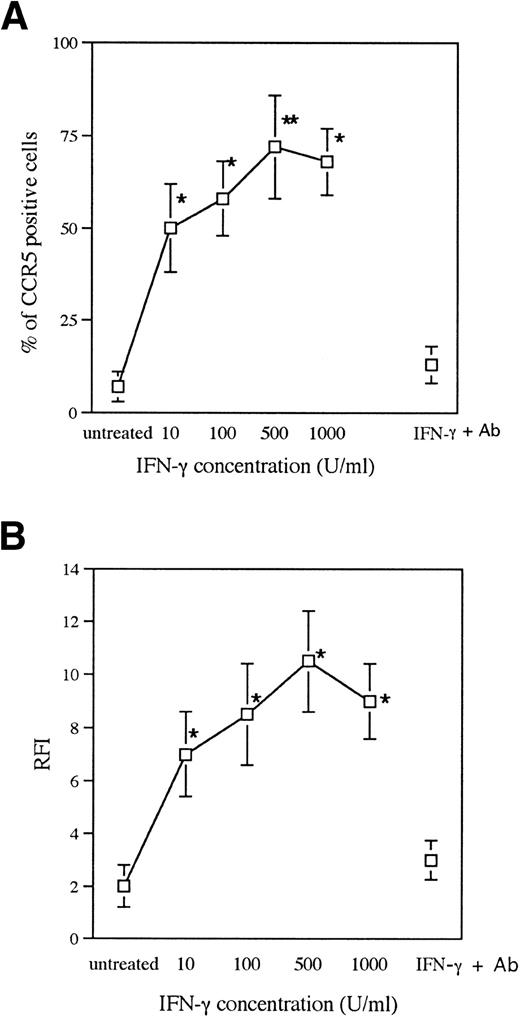
Monocytes obtained from the cord blood of healthy, term neonates and healthy adult donors and MDM (7 to 8 days postisolation) were incubated for 24 hours under one of the following conditions: control (untreated), IFN-γ, or IFN-γ plus anti–IFN-γ antibody. Cells expressing CCR5 were identified by immunofluorescence staining and flow cytometry. Cord and adult blood monocytes treated with IFN-γ showed increased CCR5 cell surface expression in comparison to untreated cells (Fig 1), with respect to the percentage of cells positive for CCR5 (IFN-γ, 50% to 94%; untreated, 1% to 30%;P < .001) and mean fluorescence intensity (IFN-γ, 6 to 29; untreated, 2.6 to 10; P < .05). In contrast, monocytes treated with IFN-α (200 U/mL) and IFN-β (200 U/mL) did not show significant changes in CCR5 expression (data not shown). Monocytes derived from cord blood (n = 10) showed slightly lower levels of CCR5 expression in comparison to monocytes from adult blood (n = 10) (percentage of untreated cells positive for CCR5: cord, 1% to 18%; adult, 2% to 34%; P = .16). Monocytes derived from cord and adult blood showed similar levels of augmentation of CCR5 expression in response to IFN-γ (6- to 10-fold). Significant stimulation of CCR5 expression was observed at a concentration of 10 U/mL of IFN-γ, with only a slight increase in CCR5 expression with higher doses of IFN-γ (100 U/mL to 1,000 U/mL; Fig 2). The augmentation of CCR5 expression by IFN-γ was inhibited by polyclonal anti–IFN-γ antibody (Fig 2). Significant stimulation of CCR5 expression was seen at 12 hours after incubation with IFN-γ, whereas the maximum effect occurred at 18 to 24 hours after treatment with IFN-γ (data not shown).
Effect of IFN-γ on CCR5 expression in monocytes. Cord and adult blood monocytes (1 × 106 cells/mL) were incubated with IFN-γ (500 U/mL) for 24 hours. CCR5 expression was determined by flow cytometry. The shaded histogram represents control staining with isotype-matched antibody (IgG2a). The open histogram represents CCR5 expression using 2D7 MoAb. Results are shown as the percentage of CCR5-positive cells and are representative of 10 cord blood samples and 10 adult donors.
Effect of IFN-γ on CCR5 expression in monocytes. Cord and adult blood monocytes (1 × 106 cells/mL) were incubated with IFN-γ (500 U/mL) for 24 hours. CCR5 expression was determined by flow cytometry. The shaded histogram represents control staining with isotype-matched antibody (IgG2a). The open histogram represents CCR5 expression using 2D7 MoAb. Results are shown as the percentage of CCR5-positive cells and are representative of 10 cord blood samples and 10 adult donors.
Effect of various doses of IFN-γ and anti–IFN-γ antibody. Monocytes were either untreated, pretreated for 24 hours with IFN-γ at the concentrations indicated, or pretreated for 24 hours with IFN-γ (500 U/mL) plus anti–IFN-γ antibody. CCR5 expression was determined by flow cytometry. Results are shown as the percentage of cells positive for CCR5 expression (mean ± SEM) (A) and as the RFI (B) and are representative of 3 cord blood samples and 2 adult donors (*P < .05, **P < .01, IFN-γ vuntreated).
Effect of various doses of IFN-γ and anti–IFN-γ antibody. Monocytes were either untreated, pretreated for 24 hours with IFN-γ at the concentrations indicated, or pretreated for 24 hours with IFN-γ (500 U/mL) plus anti–IFN-γ antibody. CCR5 expression was determined by flow cytometry. Results are shown as the percentage of cells positive for CCR5 expression (mean ± SEM) (A) and as the RFI (B) and are representative of 3 cord blood samples and 2 adult donors (*P < .05, **P < .01, IFN-γ vuntreated).
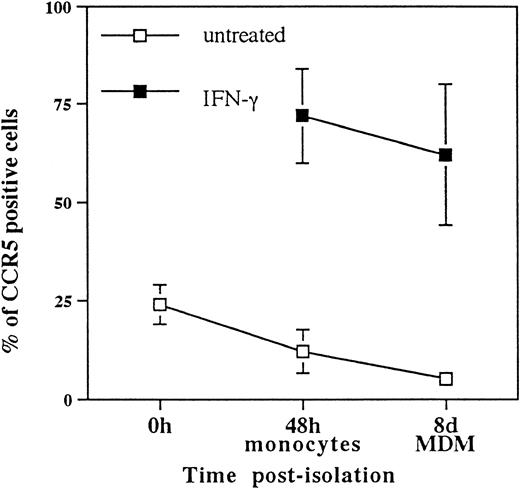
MDM also showed higher levels of CCR5 expression, after incubation with IFN-γ, in comparison to untreated cells (Fig3). Interestingly, we observed downregulation of CCR5 expression after the isolation of monocytes, and during the differentiation of monocytes to macrophages, in vitro (Fig3). However, MDM showed a greater degree of augmentation of CCR5 expression in response to IFN-γ (10- to 15-fold) in comparison to monocytes (6- to 10-fold; Fig 3).
Effect of state of differentiation of mononuclear phagocytes on CCR5 expression. Untreated mononuclear phagocytes from adult blood (n = 2) and cord blood (n = 3) were examined for CCR5 expression immediately after isolation, at 48 hours postisolation, and at 8 days postisolation. Monocytes at 24 hours postisolation and MDM at 7 days postisolation were also incubated with IFN-γ (500 U/mL for 24 hours), and CCR5 expression was studied in IFN-γ–treated cells at 48 hours and 8 days postisolation. Results are shown as the percentage of cells staining positive for CCR5 expression by flow cytometry (mean ± SEM). Similar changes were seen in mean fluorescence intensity (data not shown).
Effect of state of differentiation of mononuclear phagocytes on CCR5 expression. Untreated mononuclear phagocytes from adult blood (n = 2) and cord blood (n = 3) were examined for CCR5 expression immediately after isolation, at 48 hours postisolation, and at 8 days postisolation. Monocytes at 24 hours postisolation and MDM at 7 days postisolation were also incubated with IFN-γ (500 U/mL for 24 hours), and CCR5 expression was studied in IFN-γ–treated cells at 48 hours and 8 days postisolation. Results are shown as the percentage of cells staining positive for CCR5 expression by flow cytometry (mean ± SEM). Similar changes were seen in mean fluorescence intensity (data not shown).
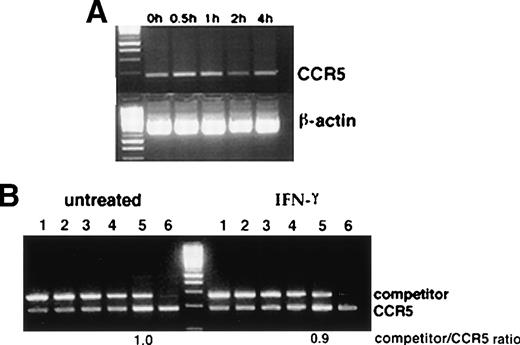
Semiquantitative RT-PCR analysis showed no significant increase in CCR5 mRNA in monocytes at 30 minutes, 1 hour, 2 hours, and 4 hours after treatment with IFN-γ. Competitive PCR confirmed similar levels of CCR5 mRNA in IFN-γ–treated and untreated monocytes (Fig4), indicating that upregulation of CCR5 expression by IFN-γ occurs at the posttranscriptional level.
(A) RT-PCR analysis of the effect of IFN-γ on CCR5 mRNA. Monocytes were incubated with IFN-γ (500 U/mL) and total cellular RNA was extracted at 30 minutes, 1 hour, 2 hours, and 4 hours after incubation with IFN-γ. (B) Competitive PCR analysis for quantification of mRNA. cDNA from the samples (untreated monocytes and monocytes incubated with IFN-γ for 30 minutes) were mixed with varying dilutions of the competitor DNA fragment and amplified with CCR5 primer sets. Lanes 1 through 6 represent increasing dilutions of competitor DNA fragment (3 × 106, 1.5 × 106, 0.7 × 106, 0.35 × 106, 3 × 105, and 3 × 104 molecules/μL). Amplification products were resolved by 4% agarose gel electrophoresis and the ratios of competitor/CCR5 DNA for untreated and IFN-γ–treated cells were determined by densitometric scanning. Lane to lane variation in RNA loading was less than 18% as assessed by densitometric analysis of β-actin expression. Representative results from 4 cord blood samples are shown.
(A) RT-PCR analysis of the effect of IFN-γ on CCR5 mRNA. Monocytes were incubated with IFN-γ (500 U/mL) and total cellular RNA was extracted at 30 minutes, 1 hour, 2 hours, and 4 hours after incubation with IFN-γ. (B) Competitive PCR analysis for quantification of mRNA. cDNA from the samples (untreated monocytes and monocytes incubated with IFN-γ for 30 minutes) were mixed with varying dilutions of the competitor DNA fragment and amplified with CCR5 primer sets. Lanes 1 through 6 represent increasing dilutions of competitor DNA fragment (3 × 106, 1.5 × 106, 0.7 × 106, 0.35 × 106, 3 × 105, and 3 × 104 molecules/μL). Amplification products were resolved by 4% agarose gel electrophoresis and the ratios of competitor/CCR5 DNA for untreated and IFN-γ–treated cells were determined by densitometric scanning. Lane to lane variation in RNA loading was less than 18% as assessed by densitometric analysis of β-actin expression. Representative results from 4 cord blood samples are shown.
Functional relevance of IFN-γ–induced CCR5 expression.
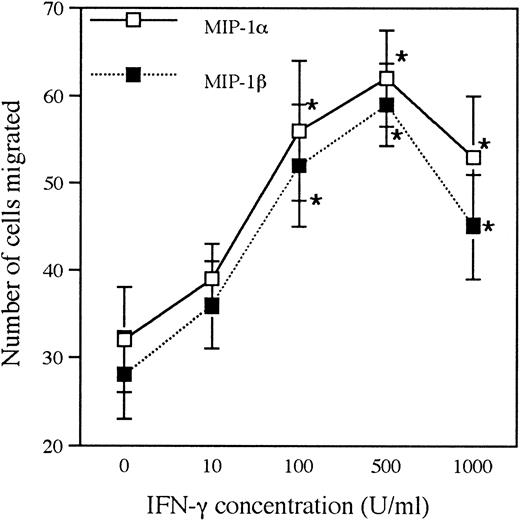
To determine the physiologic significance of IFN-γ–induced CCR5 expression, chemotactic migration of untreated and IFN-γ–treated monocytes to the CCR5 ligands MIP-1α and MIP-1β was studied. Pretreatment of monocytes with various concentrations of IFN-γ (10 to 1,000 U/mL) for 12 hours resulted in a significant increase in the number of cells migrating in response to MIP-1α and MIP-1β in a concentration-dependent fashion (Fig 5). This effect was best evident at a concentration of 10 ng/mL of these chemokine agonists and confirms the functional relevance of IFN-γ–induced CCR5 expression.
Effect of IFN-γ on chemotaxis to MIP-1 and MIP-1β. Monocytes from adult blood (n = 2) and cord blood (n = 1) were incubated for 12 hours with IFN-γ (10, 100, 500, and 1,000 U/mL). Migration of untreated and IFN-γ–treated monocytes to control medium, MIP-1, and MIP-1β (10 ng/mL) was studied as described in Materials and Methods. Results (number of cells migrated per high power field after subtraction of spontaneous migration; mean ± SEM; 3 replicates) from 1 representative donor are shown (*P < .05, IFN-γ v untreated).
Effect of IFN-γ on chemotaxis to MIP-1 and MIP-1β. Monocytes from adult blood (n = 2) and cord blood (n = 1) were incubated for 12 hours with IFN-γ (10, 100, 500, and 1,000 U/mL). Migration of untreated and IFN-γ–treated monocytes to control medium, MIP-1, and MIP-1β (10 ng/mL) was studied as described in Materials and Methods. Results (number of cells migrated per high power field after subtraction of spontaneous migration; mean ± SEM; 3 replicates) from 1 representative donor are shown (*P < .05, IFN-γ v untreated).
Effect of IFN-γ on HIV entry into MDM.
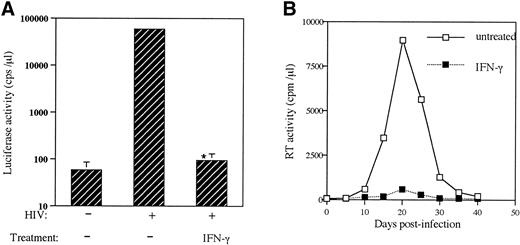
To study the effect of IFN-γ–induced enhancement of CCR5 cell surface expression on HIV entry into MDM, untreated MDM and MDM pretreated with IFN-γ (500 U/mL for 24 hours) were infected in vitro with recombinant luciferase-encoding HIV particles pseudotyped with ADA (M-tropic) Env. Upregulation of CCR5 expression by IFN-γ was confirmed by flow cytometry before infecting the cells from the same donor. Interestingly, we observed that the M-tropic ADA strain that uses CCR5 as the major fusion coreceptor for entry into MDM was unable to infect IFN-γ–treated MDM, as indicated by the very low levels of luciferase activity in these cells in comparison to untreated cells (Fig 6A). Infection of untreated and IFN-γ–pretreated MDM with the M-tropic HIV strain BaL confirmed suppression of HIV infection of macrophages by IFN-γ, as determined by the measurement of reverse transcriptase activity in the culture supernatants (Fig 6B).
Effect of IFN-γ on HIV infection of MDM. (A) Recombinant luciferase-encoding HIV reporter viruses pseudotyped with ADA Env were used to infect untreated MDM and IFN-γ–pretreated MDM (500 U/mL for 24 hours). Luciferase activity was quantitated in cell lysates 72 hours after infection. Results are representative of 4 (3 cord and 1 adult) experiments (*P < .0001, IFN-γv untreated). (B) Untreated or IFN-γ–pretreated (500 U/mL for 24 hours) MDM were infected with BaL strain of HIV and reverse transcriptase activity was measured in the culture supernatants at the times indicated. Each experiment was performed in triplicate and variability between triplicate results was less than 15%. Representative results from 4 donors (3 cord and 1 adult) are shown.
Effect of IFN-γ on HIV infection of MDM. (A) Recombinant luciferase-encoding HIV reporter viruses pseudotyped with ADA Env were used to infect untreated MDM and IFN-γ–pretreated MDM (500 U/mL for 24 hours). Luciferase activity was quantitated in cell lysates 72 hours after infection. Results are representative of 4 (3 cord and 1 adult) experiments (*P < .0001, IFN-γv untreated). (B) Untreated or IFN-γ–pretreated (500 U/mL for 24 hours) MDM were infected with BaL strain of HIV and reverse transcriptase activity was measured in the culture supernatants at the times indicated. Each experiment was performed in triplicate and variability between triplicate results was less than 15%. Representative results from 4 donors (3 cord and 1 adult) are shown.
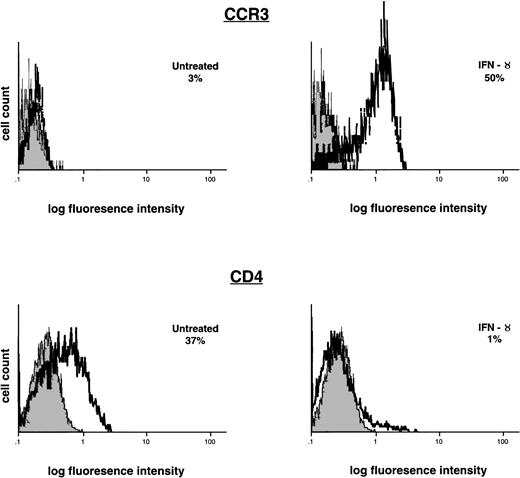
Effect of IFN-γ on CCR3 and CD4 expression in mononuclear phagocytes.
To understand the mechanisms involved in the inhibition of HIV entry into macrophages by IFN-γ (despite upregulation of CCR5 expression), we then studied the effects of IFN-γ on the expression of other receptors that mediate entry of M-tropic HIV strains into macrophages. We observed that IFN-γ also upregulated cell surface expression of CCR3, another chemokine coreceptor for M-tropic HIV. However, IFN-γ inhibited cell surface expression of CD4, the major receptor for HIV (Fig 7). To confirm the suppressive effect of CD4 downregulation on HIV infection of macrophages, we then infected MDM using recombinant luciferase-encoding HIV particles pseudotyped with M-tropic (ADA) Env after blocking CD4 with anti-CD4 (Leu 3a) MoAb. Before infection, the cells were either untreated or incubated with anti-CD4 or control (irrelevent) MoAb at 5 μg/mL for 30 minutes. Blocking CD4 on MDM using anti-CD4 MoAb completely inhibited entry of M-tropic HIV, whereas pretreatment of MDM with control MoAb failed to inhibit HIV infection (data not illustrated).
Effect of IFN-γ on CCR3 and CD4 expression. Monocytes were incubated with IFN-γ (500 U/mL) for 24 hours. CCR3 and CD4 expression were determined in untreated and IFN-γ–treated monocytes by flow cytometry. The shaded histograms represent control staining with isotype-matched antibodies, and the open histograms represent cells staining positive for CCR3 and CD4. Results are shown as the percentage of cells positive for CCR3 or CD4 expression and are representative of 3 cord blood samples.
Effect of IFN-γ on CCR3 and CD4 expression. Monocytes were incubated with IFN-γ (500 U/mL) for 24 hours. CCR3 and CD4 expression were determined in untreated and IFN-γ–treated monocytes by flow cytometry. The shaded histograms represent control staining with isotype-matched antibodies, and the open histograms represent cells staining positive for CCR3 and CD4. Results are shown as the percentage of cells positive for CCR3 or CD4 expression and are representative of 3 cord blood samples.
Effect of IFN-γ on C-C chemokine secretion by mononuclear phagocytes.
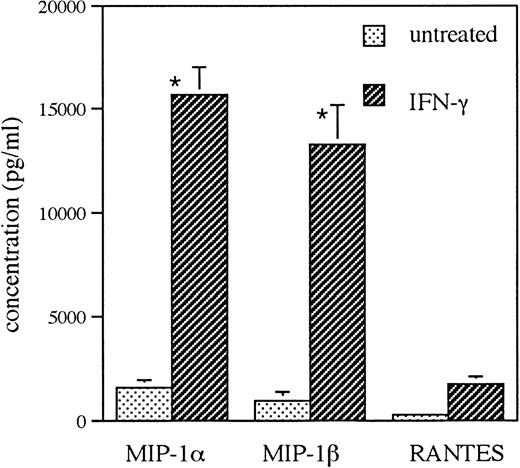
To determine whether IFN-γ modulates C-C chemokine secretion in monocytes, monocytes isolated from cord and adult blood were incubated with or without IFN-γ (500 U/mL) for 72 hours, after which the supernatants were harvested for ELISA. Increased levels of MIP-1α, MIP-1β, and RANTES were demonstrated in the supernatants from IFN-γ–treated monocyte cultures compared with supernatants from untreated cells (Fig 8).
Effect of IFN-γ on C-C chemokine secretion. Monocytes were incubated for 72 hours with IFN-γ (500 U/mL), and the supernatants from untreated and IFN-γ–treated cells were assayed for MIP-1, MIP-1β, and RANTES by ELISA. Results are representative of 3 cord blood samples (*P < .05, IFN-γ vuntreated).
Effect of IFN-γ on C-C chemokine secretion. Monocytes were incubated for 72 hours with IFN-γ (500 U/mL), and the supernatants from untreated and IFN-γ–treated cells were assayed for MIP-1, MIP-1β, and RANTES by ELISA. Results are representative of 3 cord blood samples (*P < .05, IFN-γ vuntreated).
DISCUSSION
IFN-γ has bidirectional effects on HIV infection of macrophages. Some investigators demonstrated suppressive effects of IFN-γ on HIV infection of macrophages.3 Dichotomous effects of IFN-γ on HIV replication have also been observed, with inhibition of virus expression in primary mononuclear phagocytes pretreated with this cytokine and upregulation of p24 Ag production in cells treated with IFN-γ after infection.4 Elevated levels of IFN-γ and/or the IFN-γ–inducible factor neopterin have been found in the plasma and cerebrospinal fluid17 and in the lymph nodes of HIV-infected persons,18 in which the number of infected cells actively expressing HIV is higher compared with peripheral blood,19 suggesting a potential role for IFN-γ in the in vivo regulation of HIV infection. Peripheral blood mononuclear cells from HIV-infected children show decreased stimulus-induced secretion of type 1 cytokines (interleukin-2 [IL-2] and IFN-γ) in association with disease progression.5,6IFN-γ has been used as a therapeutic agent in the treatment of HIV infection, and AIDS-associated Kaposi’s sarcoma20,21 and reduction of p24 antigen levels and improvement of immune function and clinical course have been described.20 The mechanisms responsible for the suppressive or enhancing effects of IFN-γ on HIV infection of macrophages are unclear.
In this study, we demonstrate that IFN-γ upregulates CCR5 and CCR3 expression in cord and adult blood monocytes and MDM at the posttranscriptional level. Upregulation of expression of the coreceptors CCR5 and CCR3 may potentially increase HIV entry into macrophages. However, we observed suppression of HIV infection of macrophages by IFN-γ. Our further experiments showed pronounced inhibition of expression of the major HIV receptor CD4 in monocytes pretreated with IFN-γ. This is in agreement with the findings of Dhawan et al22 and may explain the suppressive effect of IFN-γ on HIV entry into macrophages, despite its enhancing effect on the expression of CCR5 and CCR3 by these cells. The CD4 dependence for infection by M-tropic HIV strains has been established.23,24 Di Marzio et al24 observed that completely blocking CD4 on MDM using anti-CD4 MoAb completely inhibited entry of M-tropic HIV strains, whereas completely blocking CCR5 on MDM inhibited viral entry only by 60%. In addition, IFN-γ–induced secretion of C-C chemokines by monocytes may also contribute to suppression of HIV infection of macrophages.
The in vitro effects of IFN-γ on HIV infection depend on experimental conditions. We observed increased CCR5 and CCR3 expression and decreased infectability by HIV (ADA strain) in human MDM pretreated for 24 hours with this cytokine. However, Zella et al25observed increased CCR5 and CCR3 expression and enhanced susceptibility to HIV infection (HXB strain) in monocytoid U937 cells pretreated with IFN-γ for 5 days. The differences between our findings and these observations may be due to differences in the cell types used, the duration of pretreatment with IFN-γ, and the HIV strains used. The in vivo interpretations of these findings remain to be determined. IFN-γ has diverse effects on the expression of various chemokine receptors. Although it upregulates CCR5 and CCR3 expression, it has been shown to inhibit CCR2 expression in mononuclear phagocytes.26
Mononuclear cells from neonates have diminished ability to secrete IFN-γ in comparison to cells from adults.27 We have reported increased susceptibility of neonatal macrophages to HIV infection compared with adult macrophages.28 We observed similar expression of CD4 on cord and adult blood mononuclear phagocytes. Whether the enhanced susceptibility of neonatal macrophages to HIV is related to the diminished ability of neonates to secrete IFN-γ and/or to differences in CCR5 expression on these cells is under investigation. Fear et al29 recently reported decreased CCR5 expression in neonatal monocytes in comparison to adult monocytes. Our data support this observation, showing that cord blood monocytes have lower levels of CCR5 expression in the resting state in comparison to adult blood monocytes. However, augmentation of CCR5 expression in response to IFN-γ was similar in cord and adult blood mononuclear phagocytes, which is consistent with the similar levels of IFN-γ receptors expressed on cord and adult blood mononuclear phagocytes.30 CXCR4 is the fusion coreceptor for T-cell tropic HIV strains.7 Mark et al31 have demonstrated greater expression of CXCR4 mRNA in cord blood lymphocytes in comparison to adult blood lymphocytes. We speculate that, whereas the lower expression of CCR5 in neonatal macrophages may be protective to the fetus when the mother transmits M-tropic strains of HIV, the greater expression of CXCR4 may contribute to the rapid progression of AIDS in perinatally infected children.
Macrophages are reservoirs of HIV and maturation of monocytes to macrophages results in increased susceptibility to HIV infection.32 Di Marzio et al24recently reported upregulation of CCR5 expression during the in vitro differentiation of monocytes. However, the data presented by this group show that upregulation of CCR5 expression occured in 1-day cultured monocytes (1 day postisolation), whereas there was no significant increase in CCR5 mRNA in MDM (7 days postisolation) in comparison to monocytes (1 day postisolation).24 Fear et al29reported increased cytoplasmic (but not cell surface) CCR5 expression in placental macrophages and suggested that changes in CCR5 expression during the differentiation of monocytes are due to movement of the receptor in and out of the cytoplasm. We observed higher levels of CCR5 expression in freshly isolated cord and adult blood monocytes and progressive decrease in CCR5 cell surface expression during differentiation of monocytes to macrophages. These differences between our observations and others may be due to differences in the methods of isolation of monocytes. It is possible that activation of monocytes in the process of purification using gelatin-coated flasks (our previously described technique16) causes elevated CCR5 expression, with subsequent decrease to unstimulated, baseline levels over time in culture. Macrophages have greater expression of interferon receptors compared with monocytes.33 This may explain the greater levels of augmentation of CCR5 expression in MDM treated with IFN-γ (10- to 15-fold) compared with monocytes treated with IFN-γ (6- to 10-fold).
The regulation of CD4 and chemokine coreceptor expression in mononuclear phagocytes by IFN-γ has potential implications in inflammation as well as in HIV infection and AIDS pathogenesis. The divergent effects of cytokines on chemokine receptor expression and chemokine ligand production have been demonstrated.7Endotoxin inhibits expression of C-C chemokine receptors and augments C-C chemokine secretion by mononuclear phagocytes. Whereas these effects suppress HIV infection of macrophages, inhibition of chemokine receptor expression may possibly limit leukocyte recruitment.34 35 Our data suggest an emerging paradigm in which HIV infection and leukocyte migration are regulated by reciprocal effects on CD4 and chemokine coreceptor expression. The opposing effects of IFN-γ on CCR5/CCR3 and CD4 expression may augment leukocyte recruitment while containing HIV infection in sites of inflammation such as lymph nodes, where the number of infected cells actively expressing HIV is higher compared with peripheral blood. This may have important implications in the use of IFN-γ as a therapeutic agent in HIV infection and AIDS.
ACKNOWLEDGMENT
The authors are grateful to Joann Cutilli, Li Song, and Zangwei Xu for technical assistance.
Supported by 1UO1 AI 32921, NIHMH 49981, NIDA 11887-01, and the W.W. Smith Foundation.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Wen-Zhe Ho, MD, Division of Immunologic and Infectious Diseases, Room 1202B, Abramson Research Building, The Children’s Hospital of Philadelphia, 34th St and Civic Ctr Blvd, Philadelphia, PA 19104; e-mail: HO@EMAILCHOP.EDU.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal