Abstract
Interleukin-12 (IL-12) is a heterodimeric cytokine mediating a dynamic interplay between T cells and antigen-presenting cells (APCs). Preclinical studies have demonstrated that recombinant murine IL-12 (rmIL-12) promotes specific antitumor immunity mediated by T cells in several types of tumors. However, the in vivo antitumor properties of IL-12 in acute myeloid leukemia (AML) have not been previously reported. We show here in a murine AML model that systemic administration of rmIL-12 significantly delays tumor growth but is incapable of rescuing mice from lethal leukemia. In contrast, AML cells genetically modified to express IL-12 (IL12-AML) using murine stem cell virus (MSCV) p40 + p35 elicit very potent antileukemic activity. Vaccines with lethally irradiated IL12-AML cells protect naive mice against challenge with wild-type AML cells and, more importantly, can cure mice bearing a considerable leukemic burden. Immunized mice show no signs of systemic IL-12 toxicity and their spleen histology is comparable with naive mice spleen. In vivo depletion of IL-12, interferon-γ (IFN-γ), or CD8+ T cells after injections with live IL12-AML cells abrogates completely the antileukemia immune responses. Studies on the in vitro effects of IFN-γ on AML cells demonstrate enhanced expression of major histocompatibility complex (MHC) and accessory molecules and induction of the costimulatory molecules B7.1 and B7.2, but no significant direct antiproliferative effect. 51Cr release assays show that rejection of live IL12-AML cells supports the development of long-lasting leukemia-specific cytotoxic T lymphocyte (CTL) activity. In conclusion, our results demonstrate that IL12-AML vaccination is a safe and potent immunotherapeutic approach that has a great potential to eliminate minimal residual disease in patients with AML.
DESPITE THE BROAD USE of the term vaccines in tumor immunology, current cell-based cancer vaccines are always therapeutic, aiming to activate host immune responses against tumor antigens to which the immune system has already been exposed.1-3 Under these conditions, for tumor cell vaccines to confer a favorable clinical outcome, they must circumvent host immune mechanisms conferring the nonresponsiveness (T-cell tolerance) to cancer.4,5 Recent molecular immunology studies focused on pathways of T-cell activation have deciphered several critical steps that can lead to cancer tolerance. It has been clearly demonstrated that effective antigen recognition by T cells can only occur when the surrounding tissues carry danger signals as a result of local inflammation and tissue damage. The most important carriers of these signals, the host antigen-presenting cells (APCs), provide T cells with membrane-bound and soluble molecules, which are absolutely necessary for their costimulation and consequent expansion upon encountering new antigens.6,7 The expression of T-cell costimulatory molecules on APCs and the type of T-cell activation and differentiation largely depends on the cytokine environment at the time of antigen recognition.8-10
The hypothesis that lack of appropriate costimulatory and cytokine-mediated signals are major causes enabling most tumor types to induce T-cell tolerance has been confirmed during recent years in numerous studies on gene therapy tumor models (reviewed in Chen et al,11 Dranoff and Mulligan,12 and Pardoll13). In these studies, tumor cells are genetically engineered to express genes encoding various cytokine and costimulatory molecules or the combination of both. In this context, the members of the B7 family costimulatory molecules CD80 (B7.1) and CD86 (B7.2) have shown efficacy at inducing protective and therapeutic immunity against a number of murine tumors.14-16 Among the different cytokine genes that have been used to enhance tumor immunogenicity, granulocyte-macrophage colony-stimulating factor (GM-CSF) and interleukin-12 (IL-12) appear to be the most potent molecules.17-20 It has been recently reported that the expression of both B7.1 and IL-12 molecules at the tumor site enhances the antitumor efficacy achieved with either molecule alone.21 22 A critical issue that has emerged from these studies is that the sustained local release of low amounts of cytokines leads to the development of dramatic local tissue changes, mostly having the character of local inflammation, without causing any adverse systemic effects.
IL-12, a heterodimeric disulfide-linked glycoprotein consisting of a 35- and a 40-kD subunit, has a relatively short history. It was originally identified in 1989 as natural killer (NK) cell stimulatory factor (NKCS),23 and it was soon demonstrated that it mediates a number of important biological properties, including stimulation of cytotoxicity and proliferation of NK cells and cytotoxic T lymphocytes (CTL), induction of cytokine and chemokine secretion, especially interferon-γ (IFN-γ), and generation of T helper type 1 (Th1) cells.24,25 The primary physiologic sources of IL-12 appear to be APCs, such as macrophages and dendritic cells.26 During the last 4 to 5 years, IL-12 has been demonstrated to be one of the most potent antitumor cytokines. Systemic administration of recombinant murine IL-12 (rmIL-12) in several tumor models mediates profound T-cell–mediated antitumor effects in vivo, leading to regression of established tumor masses, which is frequently associated with the generation of antitumor immunological memory.27-30 However, by the same token, prolonged systemic administration of rIL-12 has been related with systemic toxicity.31,32 To address this problem, several studies on experimental tumors have evaluated the therapeutic potential of IL-12–based tumor cell vaccines and, with few exceptions, the vaccines were found to cure or significantly improve the survival of mice bearing a variety of tumors.19,33 The antitumor activity of systemic or local release of IL-12 is largely mediated by IFN-γ secreted at the tumor site by stimulated NK and T cells,28,34 along with upregulation of major histocompatibility complex (MHC) expression on tumor cells,35 NOS induction,36,37 release of other cytokines,38 and inhibition of angiogenesis through the induction of the chemokine IFN-inducible protein 10 (IP-10) by both tumor cells and infiltrating T cells.39-41
Vitale et al42 and Stine et al43 have recently demonstrated that IL-12 alone or in combination with low-dose IL-2 promotes the lysis of AML blasts in vitro. However, the in vivo activity of IL-12 in AML has not been previously reported. The compelling need to evaluate new therapeutic modalities in AML stems from the fact that AML remains one of the least responsive tumors to therapy. Despite the fact that effective induction chemotherapy regimens induce remission in 60% to 80% of the patients, long-term survival is only achieved in a minority of patients.44 45At present, it appears highly unrealistic that even the most promising immunomodulatory approaches will replace remission-induction chemotherapy protocols in AML. However, it is reasonable to argue that potent preclinical immunotherapy strategies should be tested as adjuvant therapy in AML patients in remission, most of whom are harboring minimal residual disease (MRD).
Recently, we and others have shown in preclinical studies that vaccines with gene-modified AML cells represent a potent immunotherapeutic approach.46-49 We have demonstrated in an SJL primary leukemia model that vaccines with AML cells expressing costimulatory molecules (B7.1) or cytokines (GM-CSF) cure leukemic mice and protect naive mice against subsequent challenge with wild-type (wt) AML cells.47 The efficacy of the AML cell-based vaccines provides convincing evidence that leukemia-specific antigens exist on AML cells and, more importantly, emphasize that the AML antigens recognized by the immune system do not cross-react with epitopes on normal hematopoietic progenitors. In this report, we extend our studies to evaluate the efficacy of the cytokine IL-12 in the SJL AML model. Our results demonstrate that, within the same model, systemic and local release of IL-12 confer distinct clinical effects. Although systemic administration of rmIL-12 leads to significantly delayed leukemia growth and prolonged survival, ultimately it cannot prevent the progression from residual to lethal leukemia. In contrast, vaccines with AML cells expressing IL-12 elicit very potent antileukemia immunity, leading to the curing of leukemic mice
MATERIALS AND METHODS
Mice.
Female SJL/J mice (H-2s), which were 6 to 8 weeks old, were purchased from Jackson Laboratories (Bar Harbor, ME). The animals were kept at the animal facility of Genetics Institute according to the institute's guidelines.
Murine AML model.
The murine AML model used in this study has been previously described.46 Briefly, radiation-induced AML cells are maintained by growth in syngeneic SJL/J female mice. Mice injected intravenously (IV) or intraperitoneally (IP) with ≥104 AML cells develop systemic lethal leukemia in 4 to 5 weeks. In all experiments, freshly isolated or frozen spleen mononuclear cells from leukemic mice (killed just before succumbing to leukemia) were used. Flow cytometry shows that essentially 100% of these cells express the myeloid-specific antigen Gr-1.
rmIL-12 administration.
Mice were injected IV (tail vein) with live 105 AML cells and subsequently received subcutaneous (SC) injections of rmIL-12 (Genetics Institute, Andover, MA) at various doses and schedules. Mice were observed for signs of toxicity and monitored daily for survival.
Retroviral constructs and murine IL-12 transduction of AML cells.
The retroviral vector encoding murine IL-12 and producer clones have been previously described.50 Briefly, the vector uses the LTR of the murine stem cell virus (MSCV) and contains the puromycin N-acetyltransferase (pac) gene under the control of an internal phosphoglycerate kinase (pgk) gene promoter. An encephalomyocarditis virus (EMCV) internal ribosome entry site (IRES) permits the translation of the p35 gene from the same LTR-directed RNA transcript as the p40 gene. The retroviral construct was transfected into helper- free ecotropic packaging GP+E-86 cells and producer clones (GP+E-86/MSCVmIL-12) secreting high titer of virus were used for AML cell infection. Producer cells secreting empty virus (GP+E-86/MSCVpac) were used for infection of control cells. Cells were main- tained at 37°C in Dulbecco's modified Eagle's medium containing 10% fetal calf serum, 2% glutamine, 1% penicillin-streptomycin, and 1 μg/mL puromycin. Infection of AML cells with recombinant viruses has been previously described.46 Briefly, frozen spleen AML cells (5 to 7 × 105/mL) were exposed twice to viral supernatant for 4 to 6 hours in the presence of 8 μg/mL polybrene and 15% WEHI-3B–conditioned media. Designated numbers of infected, unselected cells were used for in vivo injections.
Recombinant murine IL-12 enzyme-linked immunosorbent assay (ELISA).
Levels of rmIL-12 secreted by irradiated and nonirradiated IL12-AML cells, cultured for 24 hours at 106 cells/mL, were determined using the InterTest-12X mouse rmIL-12p70 ELISA kit (Genzyme, Cambridge, MA). The kit is a solid-phase ELISA using the multiple antibody sandwich principle and is used for the quantitation of mouse rmIL-12p70 heterodimer levels. The sensitivity of the assay is 5 pg/mL.
In vivo immunization studies.
For the in vivo immunization studies, groups of leukemic or naive SJL/J mice (8 to 10/group) were injected IV (tail vein) with live or irradiated (7,335 cGy from a 137Cs source discharging 815 cGy/min) IL12-AML or control pac-AML cells. In most of the experiments, 105 cells were used and were diluted in 200 to 300 μL of phosphate-buffered saline (PBS).
In vivo depletion studies.
The following antibodies were used for in vivo depletion studies: C17.15, rat antimouse IL-12 monoclonal antibody (MoAb; Genetics Institute); XGM1.2, rat antimouse IFN-γ MoAb; and GK1.5 and 53-6.7, rat antimouse CD4 and CD8 MoAb, respectively (PharMingen, San Diego, CA). Control mice received the same amount of rat IgG as an isotype control.
Proliferation assays.
AML cells were cultured at 4 × 105 cells/well in U-bottomed 96-well plates in the presence of rmIL-12 (10 ng/mL) or rmIFN-γ (100 U/mL; PharMingen). Proliferation of responder cells was measured after 48 hours by the incorporation of 3H thymidine (1 μCi/well) for the last 20 hours of incubation.
Immunostaining and flow cytometry analysis.
AML cells were cultured at 2 × 106 cells/mL in the presence of rmIL-12 (10 ng/mL) or rmIFN-γ (100 U/mL). After 48 hours in culture, cells were harvested and stained as previously described.46 The following MoAbs (PharMingen) were used for flow cytometry studies: Gr-1 (RB6-8C5), CD18 (C71/16), CD11a (2D7), CD11b (M1/70), CD11c (HL3), CD40 (HM40-3), CD48 (HM48-1), CD54 (3E2), CD95 (Jo2), CD3e (145-2C11), CD4 (L3T4), CD8a (53-6.7), CD45R/B220 (RA3-6B2), CD80 (1G10), CD86 (GL1), and H-2Ds (KH43). For MHC class II antigens, an anti–I-Ab MoAb (KH74) was used (cross-reacts with I-As).
Spleen histology-immunohistochemistry.
Spleens were collected and bisected; one half was cryopreserved in optimum cutting temperature (OCT; Tissue-Tek; Sakura Finetek, Inc, Torrance, CA) by liquid nitrogen-cooled isopentane method, and the other half was fixed in 10% neutral-buffered formalin. For histological evaluation, 5-μm sections from paraffin-embedded tissues were stained with hematoxylin and eosin (H+E). For immunohistochemistry, cryopreserved samples were cryosectioned onto capillary gap microslides and fixed in acetone before storing at −20°C. Immediately before staining, stored cryosections were fixed in cold acetone for 5 minutes, air-dried, blocked with avidin/biotin block (Zymed Laboratories, Inc, South Francisco, CA), and finally washed in PBS. Next, the slides were assembled on an automated immunostainer (Ventana Tech Mate 500; Ventana Medical Systems, Inc, Tucson, AZ) and stained with various MoAbs diluted to final concentrations ranging from 1 to 5 μg/mL. The following MoAbs were used: Gr-1 (RB6-8C5), CD4 (L3T4), CD8a (53-6.7), and CD45R/B220 (RA3-6B2) (PharMingen). Serial sections stained with the appropriate isotype Igs were used as negative controls. An indirect streptavidin-peroxidase method was used with DAB (3, 3′ diaminobenzidine tetrahydrochloride) as color chromogen. For the B220 staining, paraffin-embedded samples were stained using AEC (3-amino-9-ethylcarbazole) as the color chromogen.
51Cr release CTL assays.
Spleens were collected and single-cell suspensions were prepared. Splenocytes (5 × 106) were cocultured with irradiated (7,335 cGy) AML cells (1 × 105) in 2 mL complete RPMI/well of a 24-well tissue culture plate (Costar, Cambridge, MA). Six days later, splenocytes were harvested and used as effector cells in CTL assays. Autologous AML cells or control EL-4 tumor cells (2 × 106) were labeled with 200 μCi of51Cr (New England Nuclear, Boston, MA) for 90 minutes, washed twice, and used as targets (5,000/well) in the CTL assays. The standard 4-hour CTL assays were set up with various effector to target (E:T) ratios in a total volume of 0.2 mL/well in a 96-well microtiter plate. All conditions were set up in quadruplicate. After 4 hours of incubation, 75 μL of supernatant was harvested from each well and mixed with 125 μL of liquid scintillation cocktail (Optiphase Suprmix; Wallac, Turku, Finland), and the quantity of 51Cr was determined using a microbeta counter. Results are expressed as the percentage of specific lysis, which was calculated as follows: 100 × (sample cpm − spontaneous cpm)/(maximum cpm − spontaneous cpm). The cpm of supernatant from wells containing target cells in normal media and from wells containing target cells in 1% sodium dodecyl sulfate (SDS) served as the spontaneous and the maximum release, respectively.
Statistical analysis.
Most individual experiments consisted of 10 mice per treatment group. The data analyzed represent the results of 1 or 2 individual experiments. The statistical survival analysis was performed using the standard Mantel-Cox logrank test. Cytokine values secreted by transduced AML cells and AML cells proliferation results are mean ± SD. The statistical significance between various groups was analyzed using the Student's t-test.
RESULTS
Systemic rmIL-12 administration significantly delays leukemia growth.
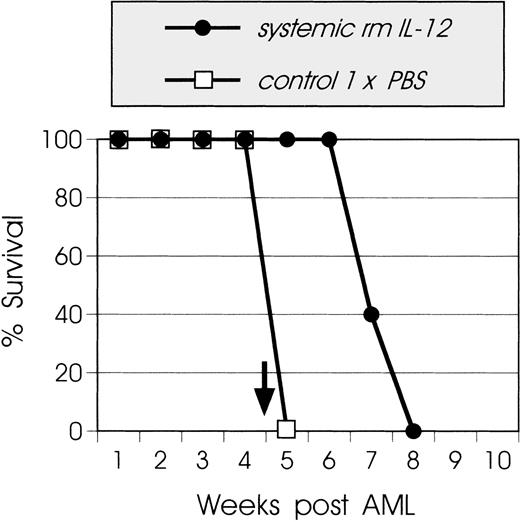
We first investigated the effect of rmIL-12 administration on the tumor growth. In this AML model, untreated mice develop lethal leukemia 4 to 5 weeks after AML inoculation. Various doses and schedules of rmIL-12 administration were tested (including continuous low dose of 0.5 μg/d during the entire period of the experiment), and the best results were achieved when leukemic mice received 2.5 μg/injection of rmIL-12 SC on days 0 through 4, 14 through 18, and 28 through 32. During the course of rmIL-12 administration, mice did not develop any clinical signs of toxicity. Spleen histology and fluorescence-activated cell sorting (FACS) analysis 4 weeks after leukemia inoculation showed that rmIL-12–treated mice had comparable spleen histology and cell subsets with naive mice (data not shown). However, although IL-12–treated mice had a statistically significant prolonged survival compared with control untreated animals (P < .001), this type of treatment could not prevent the development of lethal leukemia (Fig 1).
Effect of systemic administration of rmIL-12 on leukemia growth. SJL mice (8 to 10 mice/group) were injected IV (tail vein) with live 105 AML cells on day 0. rmIL-12 was administered SC (2.5 μg/injection) on days 0 through 4, 14 through 18, and 28 through 32 (•). Control mice (□) received injections with PBS. A solid arrow indicates the time of spleen histology and FACScan analysis. This graph is representative of 4 independent experiments.
Effect of systemic administration of rmIL-12 on leukemia growth. SJL mice (8 to 10 mice/group) were injected IV (tail vein) with live 105 AML cells on day 0. rmIL-12 was administered SC (2.5 μg/injection) on days 0 through 4, 14 through 18, and 28 through 32 (•). Control mice (□) received injections with PBS. A solid arrow indicates the time of spleen histology and FACScan analysis. This graph is representative of 4 independent experiments.
IL-12 gene transduction of AML cells.
The levels of rmIL-12 secreted by IL-12–transduced AML cells (IL12-AML) were 2.2 ± 3.4 ng/106 cells/mL/24 h and were comparable to production levels reported in other IL-12 gene transfer studies. wt AML cells cultured under the same conditions did not secrete detectable amounts of rmIL-12. Irradiation of IL12-AML cells did not abrogate rmIL-12 secretion in vitro for at least 4 days (data not shown). After 3 to 5 days of culture, the in vitro growth characteristics of IL12-AML cells, including cell morphology and growth rate, as well as MHC, costimulatory, and adhesion molecule expression, were similar to those of mock-infected AML cells (data not shown).
IL12-AML cells have reduced tumorigenicity.
Studies on gene therapy tumor models have shown that a dissociation may exist between the tumorigenicity of live cells and the immunogenicity of irradiated transduced tumor cells, suggesting that mechanisms responsible for tumor growth inhibition and immune memory may not be the same.51,52 In this context, Dranoff et al17have demonstrated that irradiated, GM-CSF–transduced murine melanoma cells are potent prophylactic vaccines, whereas live transduced cells are not rejected. In contrast, we have shown in previous studies that leukemogenic numbers of live B7.2-expressing, IL-4–expressing, and tumor necrosis factor-α–expressing AML cells are rejected, whereas irradiated cells do not protect mice against wt AML challenge.53 To assess directly the effect of the cytokine IL-12 upon the tumorigenicity of the AML cells, live transduced cells were inoculated into syngeneic SJL mice. Groups of mice were injected IV with increasing numbers (105 to 2 × 106) of IL12-AML or mock-infected pac-AML cells. All mice inoculated with IL12-AML cells rejected the leukemic cells, did not develop any clinical signs of toxicity, and remained alive and tumor-free for more than 6 months. In contrast, 100% of the mice injected with pac-AML cells developed leukemia and died after 4 to 5 weeks (Fig 2). These results clearly show that local secretion of rmIL-12 by IL12-AML cells supports the generation of effective antileukemic immune responses capable of eliminating high numbers (ie, 2 × 106) of leukemic cells.
IL-12 expression reduces significantly the tumorigenicity of AML cells. SJL mice (8 to 10 mice/group) were injected IV with increasing numbers of live IL12-AML cells or control pac-AML cells. Mice injected with 105 (▴) or 2 × 106 (•) IL12-AML cells do not develop leukemia. Control mice injected with 105 pac-AML cells (□) develop lethal leukemia. This graph is representative of 3 independent experiments.
IL-12 expression reduces significantly the tumorigenicity of AML cells. SJL mice (8 to 10 mice/group) were injected IV with increasing numbers of live IL12-AML cells or control pac-AML cells. Mice injected with 105 (▴) or 2 × 106 (•) IL12-AML cells do not develop leukemia. Control mice injected with 105 pac-AML cells (□) develop lethal leukemia. This graph is representative of 3 independent experiments.
Irradiated IL12-AML cells induce prophylactic and therapeutic immunity.
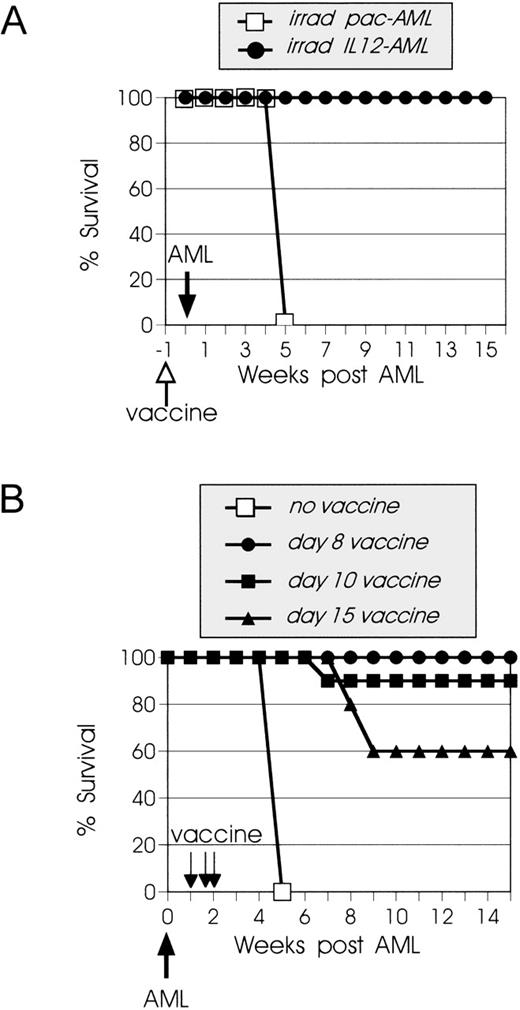
In clinical trials with tumor cell vaccines, cancer patients are vaccinated with irradiated, genetically modified tumor cells. Therefore, we evaluated the capacity of irradiated IL12-AML cells to protect naive mice from live wt AML challenge or to cure mice with already established leukemia. In this model, vaccinations with irradiated wt AML cells confer no detectable antileukemia immunity.46 Mice were injected with 105irradiated (7,335 cGy) IL12-AML or pac-AML cells and 1 week later were challenged with 105 live wt AML cells. All mice immunized with irradiated IL12-AML cells developed antileukemia immunity and survived the AML challenge, whereas the challenge was lethal to all mice immunized with irradiated pac-AML cells (Fig 3A).
Vaccines with irradiated 12-AML cells induce systemic prophylactic and therapeutic immunity. (A) SJL mice (10 mice/ group) were vaccinated IV with irradiated 105 IL12-AML or control pac-AML cells and inoculated 1 week later with live 105 wt AML cells. Mice vaccinated with IL12-AML (•) cells develop antileukemia prophylactic immunity and are resistant to AML challenge, whereas control vaccinated mice (□) develop lethal leukemia. (B) Groups of SJL mice were injected IV with live 105 AML cells. On day 8 (•), 10 (▪), or 15 (▴) after AML inoculation, they were vaccinated IV with irradiated 105 IL12-AML cells. Control leukemic mice (□) did not receive vaccines. The day-8 vaccine experiment was performed twice with identical results.
Vaccines with irradiated 12-AML cells induce systemic prophylactic and therapeutic immunity. (A) SJL mice (10 mice/ group) were vaccinated IV with irradiated 105 IL12-AML or control pac-AML cells and inoculated 1 week later with live 105 wt AML cells. Mice vaccinated with IL12-AML (•) cells develop antileukemia prophylactic immunity and are resistant to AML challenge, whereas control vaccinated mice (□) develop lethal leukemia. (B) Groups of SJL mice were injected IV with live 105 AML cells. On day 8 (•), 10 (▪), or 15 (▴) after AML inoculation, they were vaccinated IV with irradiated 105 IL12-AML cells. Control leukemic mice (□) did not receive vaccines. The day-8 vaccine experiment was performed twice with identical results.
We next determined if vaccination with irradiated IL12-AML cells could cure leukemic mice. In these experiments, mice were first injected with 105 live wt AML cells and then vaccinated with irradiated IL12-AML or control cells. As shown in Fig 3B, the survival of mice vaccinated on day 8, 10, or 15 after leukemia inoculation was 100%, 90%, and 60%, respectively. Although day 8 and 10 vaccines did not have statistically significant difference in clinical outcome (P > .3), day 15 vaccines showed significantly less efficacy than earlier (day 8) vaccines (P < .03). These results are consistent with previous observations that late AML vaccines (2 weeks after tumor inoculation) are always less efficacious than week 1 vaccines, most likely due to a larger tumor burden.47Collectively, these data clearly demonstrate that release of rmIL-12 at the tumor site can promote both the development of protective immunity and the complete regression of an established leukemic burden (up until the follow-up monitoring was terminated after 8 months, the mice remained tumor-free).
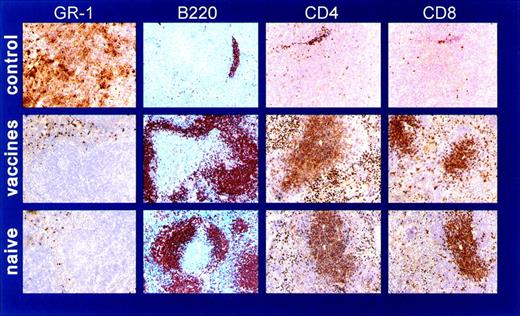
Vaccinated leukemic mice have spleen histopathology comparable with naive mice.
In our studies, mice injected with either live or irradiated IL12-AML cells never developed any clinical signs of toxicity. To obtain information on organ histology of vaccinated mice, we compared spleens from IL12-AML or pac-AML vaccinated mice and naive SJL mice. In this experiment, mice were injected with live wt AML cells and 1 week later were immunized with irradiated IL12-AML or control pac-AML cells. The spleens were removed 31 days after leukemia inoculation, at the time when the control (pac-AML) vaccinated mice had become moribund. Spleen histology showed that the naive spleen and the spleen from IL12-AML vaccinated mouse were comparable, both having appreciable hematopoiesis present and normal complements of what appeared to be relatively active lymphoid tissue or white pulp. In contrast, the spleen from the control vaccinated mouse had virtually complete obliteration of splenic architecture with a diffuse infiltrate of myeloid leukemic cells (data not shown). Spleen immunohistochemistry using the lymphoid antigens CD3, CD4, CD8, and B220 and the myeloid antigen Gr-1 (it is not expressed on lymphoid and erythroid cells) confirmed comparable normal architecture and distribution of lymphoid and myeloid cells in the naive and IL12-AML spleen. In the control vaccinated spleen, very few cells stained positive for lymphoid markers and the spleen was diffusely infiltrated by Gr-1–positive cells (Fig 4). Taken together, spleen histology demonstrates that the local secretion of rmIL-12 by irradiated tumor cells, which presumably leads to transient local recruitment of immune cells and consequent tumor rejection, does not result in any long-term microscopic alterations from the normal splenic architecture.
Vaccinated leukemic mice have spleen features comparable with naive mice. Spleen immunohistochemistry of (A) control pac-AML–vaccinated leukemic mouse; (B) IL12-AML–vaccinated leukemic mouse; and (C) naive SJL mouse. The spleen from pac-AML–vaccinated mouse is almost completely infiltrated by Gr-1–positive cells and has very few residual B220 (B cells) and CD4/CD8 (T cells) positive cells. In contrast, the distribution of myeloid and lymphoid cells in the IL12-AML spleen is comparable with naive spleen.
Vaccinated leukemic mice have spleen features comparable with naive mice. Spleen immunohistochemistry of (A) control pac-AML–vaccinated leukemic mouse; (B) IL12-AML–vaccinated leukemic mouse; and (C) naive SJL mouse. The spleen from pac-AML–vaccinated mouse is almost completely infiltrated by Gr-1–positive cells and has very few residual B220 (B cells) and CD4/CD8 (T cells) positive cells. In contrast, the distribution of myeloid and lymphoid cells in the IL12-AML spleen is comparable with naive spleen.
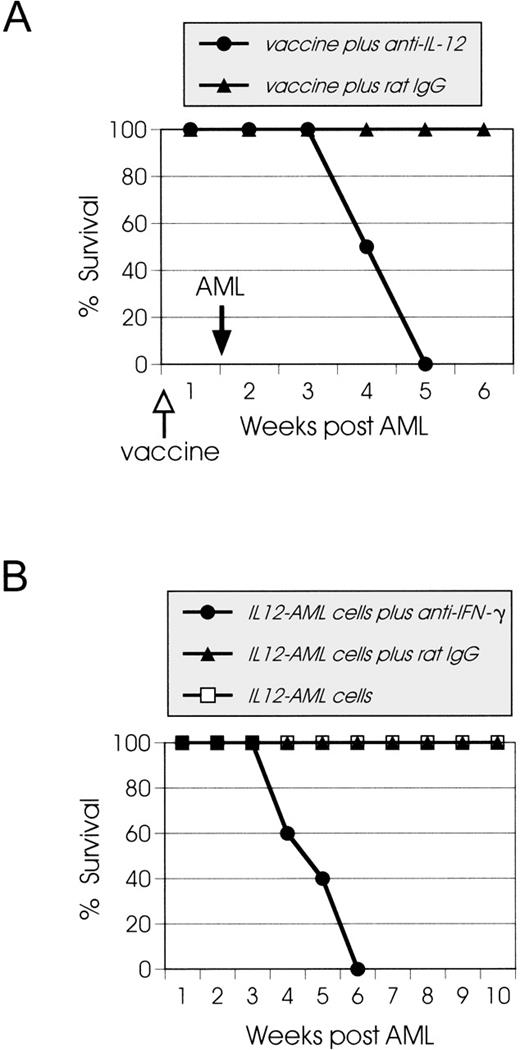
In vivo depletion of IL-12 or IFN-γ abrogates antileukemia immune responses.
To evaluate the role of IL-12 in the generation of antileukemia immunity, mice that were vaccinated with irradiated IL12-AML cells were treated in vivo with antimouse IL-12 MoAb and were challenged 1 week later with live wt AML cells. As shown in Fig 5A, control mice that were treated with control isotype rat IgG were resistant to the AML challenge, whereas all mice treated with anti–IL-12 MoAb developed lethal leukemia. In most tumor models analyzed in the literature, the antitumor effects of rmIL-12 are at least in part mediated by the secondary secretion of IFN-γ.38,54 This is based on the observation that, although IFN-γ production alone is not sufficient to induce significant therapeutic effects,34 the coadministration of IFN-γ neutralizing MoAb abrogates the antitumor efficacy of IL-12.27 28 To determine the importance of endogenous IFN-γ production in IL12-AML rejection, SJL mice were injected with live IL12-AML cells and treated with purified anti–IFN-γ MoAb. Control mice received either saline or control isotype IgG. As shown in Fig 5B, depletion of IFN-γ completely abrogated the rmIL-12–mediated antitumor effect and 100% of treated mice developed leukemia.
Effects of the in vivo depletion of IL-12 or IFN-γ on leukemia growth. (A) SJL mice (10 mice/group) were injected IP on days −1, 0, 2, 4, and 6 with 200 μg of either anti–IL-12 MoAb or rat IgG as an isotype control. On day 0 the mice were immunized IV with irradiated 105 IL12-AML cells, and on day 7, they were challenged with live wt 105 AML cells. In vivo depletion of IL-12 during the immunization with irradiated IL12-AML cells leads to abrogation of protective immunity, and all of the mice developed lethal leukemia. Control mice were resistant to AML challenge. (B) SJL mice were injected IV with live 105IL12-AML cells on day 0 and then injected IP on days 0, 1, 2, and 7 with purified preparations (320 μg/injection) of hybridoma XGM1.2 (•). Control mice were injected with IL12-AML cells and received either no therapy (□) or the same amount of IgG1 as an isotype control (▴). Mice depleted of IFN-γ develop lethal leukemia, and both groups of control mice reject the live IL12-AML cells.
Effects of the in vivo depletion of IL-12 or IFN-γ on leukemia growth. (A) SJL mice (10 mice/group) were injected IP on days −1, 0, 2, 4, and 6 with 200 μg of either anti–IL-12 MoAb or rat IgG as an isotype control. On day 0 the mice were immunized IV with irradiated 105 IL12-AML cells, and on day 7, they were challenged with live wt 105 AML cells. In vivo depletion of IL-12 during the immunization with irradiated IL12-AML cells leads to abrogation of protective immunity, and all of the mice developed lethal leukemia. Control mice were resistant to AML challenge. (B) SJL mice were injected IV with live 105IL12-AML cells on day 0 and then injected IP on days 0, 1, 2, and 7 with purified preparations (320 μg/injection) of hybridoma XGM1.2 (•). Control mice were injected with IL12-AML cells and received either no therapy (□) or the same amount of IgG1 as an isotype control (▴). Mice depleted of IFN-γ develop lethal leukemia, and both groups of control mice reject the live IL12-AML cells.
In vitro effects of rmIL-12 and rmIFN-γ on AML cells.
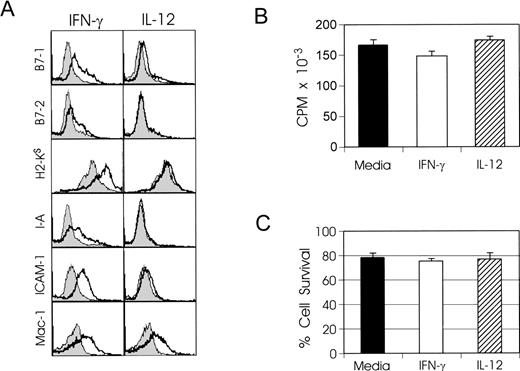
The cytokines IL-12 and IFN-γ may exert their in vivo antitumor effects by activating the host's immune responses and/or by acting directly on tumor cells. We therefore examined the immunophenotype, proliferative response, and survival of AML cells cultured in vitro with either cytokine or the combination of both. After 48 hours, the AML cells were stained with various MoAbs (described in Materials and Methods) that are directed against a wide range of cell surface molecules. We only present here the differences observed when cytokines were included in the culture. As shown in Fig 6A, AML cells had increased expression of costimulatory, MHC class I and II, and adhesion molecules when they were exposed to rmIFN-γ, whereas rmIL-12 had very little or no effect on the phenotype of the AML cells. The AML cell phenotype acquired with both cytokines did not differ from the rmIFN-γ phenotype (data not shown). In addition to the surface markers described above, we also stained the AML cells with Annexin V (detects apoptotic cells), and no positive cells were detected 48 hours after the initiation of the cultures (data not shown). Proliferation assays showed that, although AML cells cultured with IFN-γ exhibited a statistically significant difference in proliferative response compared with media alone (P < .01), it is highly unlikely that this difference is significant with regard to mechanisms of tumor rejection (Fig 6B). Lastly, the viability of AML cells after 48 hours in culture, as assessed by trypan-blue exclusion, showed that there were no statistical differences in survival between the various AML culture groups (Fig 6C). These in vitro data suggest that direct killing of tumor cells by IL-12 or IFN-γ is unlikely to be an immediate primary mechanism leading to tumor rejection. In contrast, FACS analysis data strongly indicate that the heightened expression of molecules known to be very important or necessary for T-cell activation/costimulation may be important in orchestrating the complex immune events leading to antileukemia immunity.
In vitro effects of IFN-γ on AML cells. (A) AML cells were cultured at 2 × 106 cells/mL with either 100 U/mL rmIFN-γ or 10 ng/mL rmIL-12. Control AML cells were cultured in RPMI alone. After 48 hours, cells were harvested and stained as described in Materials and Methods. In all panels, solid histograms represent the expression of the indicated markers by AML cells cultured in RPMI alone. A total of 10,000 cells were analyzed by FACS for each sample. (B) AML cells were cultured at 4 × 105 cells/well in U-bottomed 96-well plates in the presence of 100 U/mL rmIFN-γ or 10 ng/mL rmIL-12. 3H thymidine (1 μCi/well) was added during the last 20 hours of culture. Results are representative of 2 independent experiments and are shown as the mean ± SD of 8 cultures. (C) AML cells were cultured as described in (A). After 48 hours, cells were harvested and their viability was assessed by trypan blue exclusion. Results are representative of 2 independent experiments and are shown as the mean ± SD of triplicate culture.
In vitro effects of IFN-γ on AML cells. (A) AML cells were cultured at 2 × 106 cells/mL with either 100 U/mL rmIFN-γ or 10 ng/mL rmIL-12. Control AML cells were cultured in RPMI alone. After 48 hours, cells were harvested and stained as described in Materials and Methods. In all panels, solid histograms represent the expression of the indicated markers by AML cells cultured in RPMI alone. A total of 10,000 cells were analyzed by FACS for each sample. (B) AML cells were cultured at 4 × 105 cells/well in U-bottomed 96-well plates in the presence of 100 U/mL rmIFN-γ or 10 ng/mL rmIL-12. 3H thymidine (1 μCi/well) was added during the last 20 hours of culture. Results are representative of 2 independent experiments and are shown as the mean ± SD of 8 cultures. (C) AML cells were cultured as described in (A). After 48 hours, cells were harvested and their viability was assessed by trypan blue exclusion. Results are representative of 2 independent experiments and are shown as the mean ± SD of triplicate culture.
IL12-AML cell rejection is CD8+ T-cell dependent and supports the development of long-lasting, leukemia-specific CTL activity.
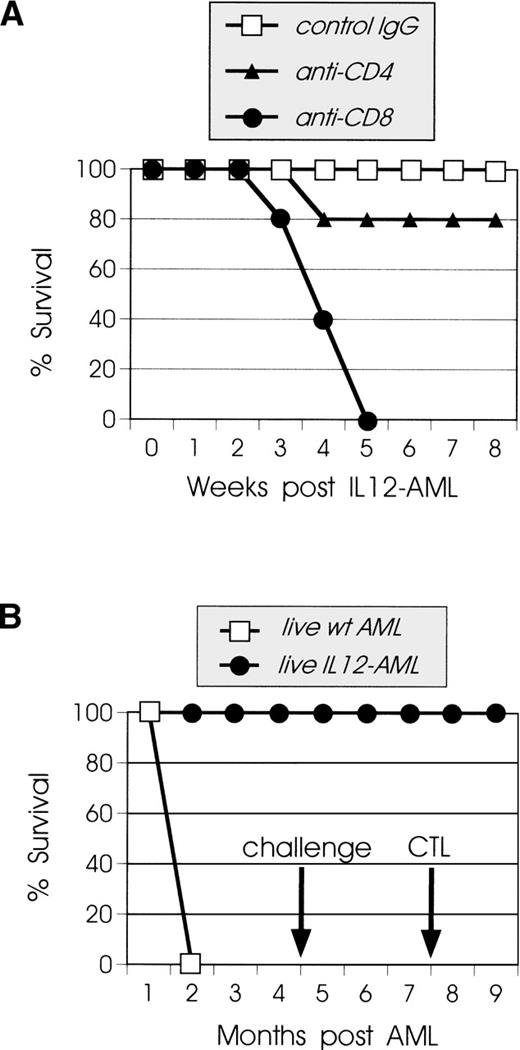
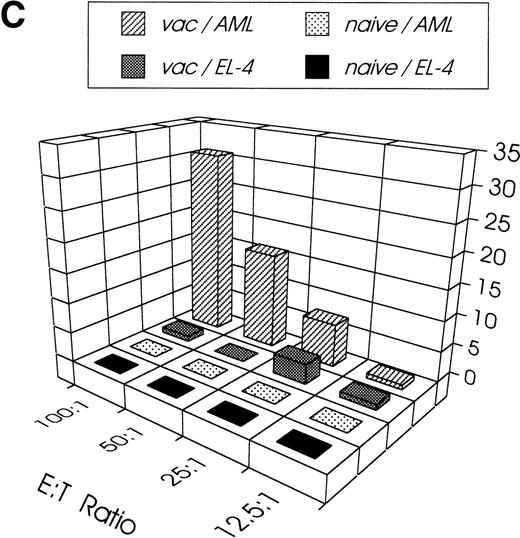
The mechanisms responsible for tumor rejection in cytokine gene immunotherapy may not be the same as those required for immune memory. Several types of immune cells, such as macrophages, eosinophils, and neutrophils, that are recruited locally by the secreted cytokine may participate in tumor killing, but the induction of memory cells is exclusively CD8+ T-cell dependent.12 51 To delineate the role of T-cell subsets in the rejection of live IL12-AML cells, we performed in vivo depletion of CD4+ or CD8+ T cells. As shown in Fig7A, all CD8+-depleted vaccinated mice developed leukemia at the same time as control animals, whereas from the CD4+-depleted group only 20% developed leukemia, with 80% of the mice rejecting live IL12-AML cells. These results demonstrate the absolute requirement for CD8+ T cells in tumor rejection, whereas the participation of CD4+ T cells was not necessary in most of the vaccinated mice. In an attempt to address the issue of CTL memory persistence in the AML model, we challenged mice with wt AML cells 4 months after the rejection of live IL12-AML cells. All the mice in this experiment were resistant to the challenge (Fig 7B). Three months later, spleens from these mice were removed and assayed for in vitro leukemia-specific CTL activity. As shown in Fig7C, splenocytes from immunized mice generated a cytolytic response upon stimulation with wt AML cells. The response was AML-specific, because the same cells did not lyse alloantigen-presenting EL-4 (H-2b) cells. These results indicate that, in this model, the rejection of live IL12-AML cells is mediated almost exclusively by CD8+ T cells, which then develop into long-lived leukemia-specific memory cells.
Rejection of live IL12-AML cells is CD8+T-cell dependent and generates long-lasting leukemia-specific immunity. (A) Groups of SJL mice were injected IP on 3 consecutive days with 150 μg of purified MoAb of either 53.672 hybridoma (▴) or GK1.5 hybridoma (•). One day after the last injection, 1 mouse from each group was killed and the depletion was verified in spleen cells by flow cytometry. The remaining mice were injected IV with 105live IL12-AML cells, and the antibody injections continued twice weekly for 3 weeks. Control mice were treated with isotype control rat IgG (□). All mice depleted of CD8+ T cells developed lethal leukemia, whereas only 20% of CD4+ T-cell–depleted mice developed leukemia and 80% rejected the IL12-AML cells. All of the control mice rejected the IL12-AML cells. (B) Groups of mice were injected IV with 105 live IL12-AML (•) or control (□) cells. All IL12-AML–injected mice rejected the leukemic cells, whereas all control mice developed lethal leukemia. Mice that rejected IL12-AML cells were challenged 4 months later with 105 live wt AML cells. All of the challenged mice were immune against AML cells and did not develop leukemia. Three months after the challenge, 3 mice were killed and their splenocytes were used for CTL assays. (C) Splenocytes from vaccinated mice were stimulated in vitro with irradiated AML cells as described in Materials and Methods. Six days later, cells were harvested and used as effector cells in the indicated E:T ratios. Target cells (autologous H-2s AML or control H-2b EL-4 cells) were incubated with 51Cr for 90 minutes. The standard 4-hour CTL assays were set up in a total volume of 0.2 mL/well in 96-well microtiter plates. All conditions were set up in quadruplicate. As the control in the experiment, normal SJL splenocytes were tested for CTL activity on AML (naive/AML) and EL-4 cells (naive/EL-4). Splenocytes from vaccinated mice lysed autologous AML (vac/AML) but not EL-4 cells (vac/EL-4).
Rejection of live IL12-AML cells is CD8+T-cell dependent and generates long-lasting leukemia-specific immunity. (A) Groups of SJL mice were injected IP on 3 consecutive days with 150 μg of purified MoAb of either 53.672 hybridoma (▴) or GK1.5 hybridoma (•). One day after the last injection, 1 mouse from each group was killed and the depletion was verified in spleen cells by flow cytometry. The remaining mice were injected IV with 105live IL12-AML cells, and the antibody injections continued twice weekly for 3 weeks. Control mice were treated with isotype control rat IgG (□). All mice depleted of CD8+ T cells developed lethal leukemia, whereas only 20% of CD4+ T-cell–depleted mice developed leukemia and 80% rejected the IL12-AML cells. All of the control mice rejected the IL12-AML cells. (B) Groups of mice were injected IV with 105 live IL12-AML (•) or control (□) cells. All IL12-AML–injected mice rejected the leukemic cells, whereas all control mice developed lethal leukemia. Mice that rejected IL12-AML cells were challenged 4 months later with 105 live wt AML cells. All of the challenged mice were immune against AML cells and did not develop leukemia. Three months after the challenge, 3 mice were killed and their splenocytes were used for CTL assays. (C) Splenocytes from vaccinated mice were stimulated in vitro with irradiated AML cells as described in Materials and Methods. Six days later, cells were harvested and used as effector cells in the indicated E:T ratios. Target cells (autologous H-2s AML or control H-2b EL-4 cells) were incubated with 51Cr for 90 minutes. The standard 4-hour CTL assays were set up in a total volume of 0.2 mL/well in 96-well microtiter plates. All conditions were set up in quadruplicate. As the control in the experiment, normal SJL splenocytes were tested for CTL activity on AML (naive/AML) and EL-4 cells (naive/EL-4). Splenocytes from vaccinated mice lysed autologous AML (vac/AML) but not EL-4 cells (vac/EL-4).
DISCUSSION
In this report, we have used a murine primary AML model to assess the in vivo activity of the cytokine IL-12. The results we present show that local release of rmIL-12 by retrovirally transduced AML cells supports the generation of both therapeutic and long-lasting protective immunity. Furthermore, we demonstrate that, in this AML model, the antileukemia immune responses mediated by IL12-AML vaccines are both IL-12 and IFN-γ dependent. Of particular importance and clinical relevance is that this immunization approach has the potential to eradicate an established leukemic burden without any adverse systemic effects.
At present, gene transduction of autologous tumor cells for vaccination remains highly individualized and labor intensive. Therefore, we initiated our AML studies with a simpler therapeutic approach by treating leukemic mice systemically with rmIL-12. Numerous studies have demonstrated that systemic rmIL-12 administration mediates antitumor effects in vivo (reviewed in Brunda et al55). Unfortunately, this type of treatment also leads to dose-dependent toxicity both in mice56 and in humans.57 In the SJL AML model, systemic treatment with rmIL-12 during the course of the disease is clinically well tolerated, with treated leukemic mice having no signs of leukemia in the spleen at the time when control animals develop lethal disease (4 weeks after leukemia inoculation). However, neither continuation nor discontinuation of rmIL-12 treatment is able to prevent leukemia recurrence, and all treated mice die after 2 to 3 weeks. It is conceivable that, although systemic rmIL-12 treatment supports the development of antileukemia effector responses, it does not generate memory cytolytic T cells necessary to control the outgrowth of residual leukemic cells. One possible explanation is that rmIL-12 initiates nonspecific AML killing that is primarily mediated by activated NK cells. However, SJL mice are genetically low-NK strain, and it has been documented that the very low endogenous levels of NK cytotoxic activity can be poorly augmented with conventional NK inducers such as polyinosinic-polycytidylic acid (poly I:C).58 This motivated us to test the in vitro NK activity of naive SJL mice after in vivo treatment with rmIL-12 in comparison to treatment with poly I:C as control. Neither treatment resulted in increased target cell lysis by NK cells (data not shown), suggesting that NK-mediated, MHC-unrestricted cytotoxicity has a very limited, if any, role in the generation of the antileukemia immune responses. A second explanation for the leukemia recurrence in rmIL-12–treated mice is the potential for immunosuppression as a consequence of chronic dosing with rIL-12.32,59 Recently, Koblish et al37 have demonstrated that the high IFN-γ levels induced by IL-12 activate macrophages to produce nitric oxide (NO), which, in turn, leads to suppression of T-cell responses. It has been proposed that the use of lower or fewer doses of rIL-12 may overcome the problems related to its transient immunosuppressive side effects.32 Our attempts to balance a proper, nontoxic dose/schedule of systemic rmIL-12 and a favorable clinical outcome in the AML model were unsuccessful, most probably due to the overwhelming tumor kinetics related to AML.
In contrast to systemic rmIL-12 administration, vaccines with irradiated IL12-AML cells can cure leukemic mice bearing a considerable leukemic burden and can protect naive mice against challenge with wt AML cells. The potency of IL12-AML vaccines to generate effector and memory CTLs most probably relies on a sustained low amount of IL-12 released at the tumor site that is adequate to fuel and control local antileukemia responses without mediating any signals alarming for downregulatory mechanisms. This scenario is supported by a recent report demonstrating that IL-12 is a heparin-binding cytokine.60 This property suggests that IL-12 will be trapped close to its sites of secretion in the tissues by binding to heparin-like glycosaminoglycans, thus favoring a prolonged paracrine role without systemic toxic effects.
The critical requirement of IFN-γ for the IL-12–mediated antitumor effects has been observed in several tumor models.27,36 In the AML model, treatment of anti–IFN-γ MoAb before and concurrent with IL12-AML vaccination abrogates the antileukemia efficacy of the vaccines. IFN-γ has been shown to possess both direct antitumor activity and immunomodulating properties, including activation of macrophages and enhancement of T-cell–mediated immunity.27,28 We have been unable to show in the SJL AML model that IFN-γ has a significant in vitro direct effect on the proliferation and survival of AML cells for at least 48 hours. However, in vitro studies show that IFN-γ increases or induces the expression of MHC, accessory, and B7 costimulatory molecules on AML cells. Because the biological effects of T-cell–mediated immune responses are controlled by the interaction between T-cell receptor (TCR) and the respective peptide ligand(s) presented by MHC molecules, increased MHC expression by AML cells may represent a critical event in the initiation of the cytolytic T-cell responses against the leukemic cells. Equally important, induction of the costimulatory molecules B7.1 and B7.2 and increased expression of accessory molecules such as the integrin Mac-1 and the adhesion molecule ICAM-1 leads to the hypothesis that prolonged AML–T-cell cross-talk mediated by these molecules significantly contributes to the generation and enhancement of leukemia-specific T-cell responses.61
It has recently been demonstrated that IFN-γ induces the paracrine secretion of chemokines such as IP-10 and monokine induced by IFN-γ (MIG).39,41 This family of proteins is involved in the local recruitment of leukocytes that can mediate an inflammatory response and in the inhibition of endothelial cell proliferation, resulting in inhibition of angiogenesis.62,63 This immune mechanism could also be implicated in the IL-12/IFN-γ–mediated leukemia rejection. Indeed, we have data from gene expression analysis using a murine 6,500 gene chip that show that IP-10 is among several molecules induced by IFN-γ in AML cells (B. Clancy, unpublished data). It is well established now that solid tumors promote angiogenesis, and there is increasing evidence that its blockade results in tumor regression.64 65 At present, it is not known if AML cells need new vessel formation for their survival and if AML cells in fact promote angiogenesis, as is the case for solid tumors. In an attempt to address this issue, we used Matrigel implants as an in vivo assay for AML angiogenesis. Surprisingly, repeated experiments showed that Matrigel implants containing SJL AML cells or murine lymphoma EL-4 cells had no evidence of vascularization 5 days after implantation into syngeneic animals (S. Hunter, unpublished data). In the same type of experiments, murine solid tumor cells (ie, MB49 bladder carcinoma cells) promote significant vascularization. These observations raise serious questions as to how, if at all, induction of IP-10 expression participates in the antileukemia response. It also emphasizes that the role of angiogenesis and antiangiogenic compounds in systemic hematologic malignancies is a very important issue that needs to be resolved.
Our challenge experiments have shown that mice are immune against wt AML cells 4 months after the rejection of live IL12-AML cells. Whereas the participation of CD4+ T cells in IL12-AML rejection appears unnecessary, the presence of CD8+ T cells is absolutely necessary for effective antileukemia immune responses. At present, the molecular mechanisms controlling the maintenance of memory T cells in tumors are largely unknown. Although it was suggested several years ago, it has only recently been demonstrated that cross-reactive peptides may play an important role in the expansion and reactivation of CTL clones from the memory CTL pool and may be involved in the long-term maintenance of antigen-specific T-cell memory.66 An extrapolation from the findings in these experimental systems implies that persistence of leukemia-specific antigens is not necessarily required for memory CTL maintenance. We plan to address this issue in the AML system in future studies with adoptive T-cell transfer experiments.
In summary, we have shown that vaccination of mice with IL12-AML cells initiates immune responses leading to cure of leukemic mice and to protection of naive mice against wt AML challenge. We have also shown that, in the SJL AML model, IFN-γ has an indispensable role for the efficacy of the vaccines. We have demonstrated that IFN-γ enhances the expression of several molecules on AML cells that are known to strengthen APC–T-cell interactions, thus facilitating the development of effector T cells and memory CTL.
From a clinical standpoint, the large safety profile of the IL12-AML vaccines presented here, together with previously established safety issues in other cytokine gene therapy studies, is of critical importance in allowing outpatient testing of AML patients in the adjuvant therapy situation. The practical considerations for large-scale testing and application of autologous tumor vaccines are simpler in AML than in any other solid tumor type. This is because the requirement for availability of large numbers of tumor cells can be easily addressed in liquid malignancies such as AML. Our efforts are currently being directed toward optimizing phase I clinical trial designs, and we anticipate that AML cell vaccines will ultimately become part of standard AML treatment in the eradication of MRD.
ACKNOWLEDGMENT
The authors thank Sharon Hunter and Joyce Johnson for technical help, Dr Brian Clancy for the gene chip experiments, Dr Page Bouchard for reviewing the spleen histology slides, and Dr Stan Wolf for critical review of the manuscript.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Kyriaki Dunussi-Joannopoulos, MD, PhD, Genetics Institute, 1 Burtt Rd, Andover, MA 01810.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal