Abstract
Impairment of T-cell renewal has been proposed as contributing to CD4+ T-cell depletion in persons infected with human immunodeficiency virus-1. We analyzed the T-cell development capacity of progenitors using fetal thymus organ culture. Those who progressed to AIDS had a dramatic loss in T-cell development capacity shortly after seroconversion. In contrast, long-term nonprogressors retained progenitor capacity 8 years after seroconversion. Approximately 70% of patients experienced an improvement in T-cell development capacity after receiving 6 months of potent antiretroviral therapy. Improvement in T-cell development in fetal thymus organ culture correlated with an increase in the number of naive CD4+ T cells in peripheral blood. Numbers of progenitors in blood and bone marrow after seroconversion or during therapy did not correlate with the change observed in T-cell development capacity. These data provide evidence that HIV-1 infection can interfere with T-cell renewal at the level of the progenitor cell. Interference with T-cell renewal may contribute to CD4+ T-cell depletion.
The effect of human immunodeficiency virus-1 (HIV-1) infection on T- cell renewal has been studied mainly at the level of peripheral cell proliferation. With the recent evidence that the adult thymus is a functional organ, interest in the impact of HIV-1 infection on immune reconstitution from progenitor sources has grown.
There is a considerable body of evidence to support the contention that HIV-1 infection interferes with hematopoiesis. Defects in stromal architecture1 and a lack of thymocyte subsets2,3 have been reported in infected persons. Moreover, the generation of multiple hematopoietic lineages is blocked by HIV-1 infection in SCID-hu mice.4,5 CD34+cells from HIV-1 infected persons display a reduced capacity to develop cells of erythrocyte, granulocyte, megakaryocyte, and T-lymphocyte lineages in vitro.6-8 In addition, though CD34+cells from HIV− persons can develop on bone marrow stroma from infected persons, CD34+ cells from HIV+ persons do not develop on stroma from uninfected persons.9 These data suggest that at least some of the defect lies within the progenitor cells themselves and is not merely a reflection of the environment in which they reside.
T-cell renewal can be determined by the appearance of new, naive T cells in the blood. By measuring excision circles resulting from T-cell receptor gene rearrangement, Koup et al10 estimated the number of relatively newly developed cells in HIV-1 infected persons. The number of cells in the blood and lymph nodes expressing excision circles was lower in HIV+ persons than in control subjects. They concluded that the output of the thymus is reduced in HIV-1 infected persons. The level of thymic output is likely to be determined by the amount of functional thymic tissue and the functional capacity of progenitor cells. Recent data measuring the size of thymic tissue in HIV+ persons have shown a correlation with numbers of naive cells in the blood.11
Determination of progenitor function is complicated by the requirement for ill-defined thymic signals to induce T-cell development from progenitors. An in vitro T-cell development system, fetal thymus organ culture (FTOC), has been described in which murine fetal thymus is repopulated with human CD34+ cells. Most of the literature describes the development of fetal CD34+ cells in this system. Studies using adult bone marrow show that adult cells do not colonize thymus tissue well in the traditional “hanging drop” method of FTOC.12 In addition, CD34+ cells from adults appear to develop more rapidly than those from fetuses and the adult cells lack the sustained double-positive stage that develops when the cells are grown in fetal thymus.13,14Another concern is that thymus tissue is traditionally treated with deoxyguanosine to deplete the resident thymocytes; however, other thymus cells are also affected by this compound.15 We chose as a method the direct application of cells to untreated fetal thymus of T-cell–deficient mice to provide the most normal thymus environment and to give the adult progenitors the best chance to colonize and develop.
Patients, materials, and methods
Subjects
Persons with known dates of seroconversion, who had histories of consistent sampling and whose pre-seroconversion samples were cryopreserved, were chosen from the Amsterdam Cohort of Homosexual Men. Seven long-term non-progressors (LTNP), defined as seropositive for more than 8 years and with more than 400 CD4+ cells/mL in the 8th year, whose pre-seroconversion samples were cryopreserved as part of the Amsterdam Cohort, were selected. Seven age-matched persons who progressed to AIDS were also selected. Samples from more than 1 year before seroconversion and every 2 years after seroconversion to the end of follow-up were analyzed. For all progressors and some LTNP, a 6-month post-seroconversion sample was also analyzed. Two of the LTNPs and 4 of the progressors were on AZT therapy containing regimens for the last time point only; for all other samples, the patients were untreated.
For the analysis of anti-retroviral therapy, persons who had undetectable viral RNA load after 6 months of therapy were assessed. For the Era study (zidovudine or stavudine, lamivudine, nevirapine, indinavir, and abacavir) 6 participants were tested before therapy and again after 6 and 12 months. In the NUCB2019 trial (zidovudine, lamivudine, and ritonavir), 6 participants were tested before therapy and again at 6 and 12 months. For the INCAS study (zidovudine, didanosine, and nevirapine), 6 participants were tested before therapy and again at 6 and 12 months, and a subgroup (n = 3) was tested at 18 months. Four participants in the Era study also donated bone marrow before the initiation of therapy and after 12 months of therapy.
Samples
All samples were cryopreserved according to a computerized freezing system that retains the functional capacity of the cells when they are thawed.16 17 Cryopreserved cells were thawed and counted by Coulter (Miami, FL) counter, and viability was assessed by trypan blue dye exclusion. All yields expressed are viable cell yields.
Mice
RAG-1 knockout mice were maintained and bred in microisolator cages in The Netherlands Cancer Institute (Amsterdam, The Netherlands). Fetal thymus lobes from 14- and 15-day gestation mice were placed on Millipore filters (0.45 μm pore size, mixed esters; Bedford, MA) resting on Netwells (74 μm mesh; Costar, Acton, MA) in 6-well plates. Organ cultures were grown in Dulbecco's minimum essential medium, 20% fetal bovine serum (Gibco-BRL, Gaithersburg, MD), 1 μg/mL penicillin, and 1 U/mL streptomycin and were maintained at 37°C with 5% CO2.
Progenitor enrichment
Peripheral blood mononuclear cells (PBMC) were isolated from 10 mL fresh blood or from bone marrow. CD34+ cells were obtained by positive selection with MACS magnetic beads (Miltenyi Biotech, Bergisch Gladbach, Germany) according to manufacturer's instructions. Purity of enriched populations was greater than 90%, as determined by flow cytometry.
Fetal thymus organ culture
Human cells were placed on each thymus lobe by direct application of broken cell pellets in multiple 0.2-μL aliquots to the desired concentration. For unfractionated samples, 5 × 105 to 2 × 106 viable cells per lobe (of 105 samples, 87 were used at a concentration of 7.5 × 105 to 1.3 × 106 cells per lobe) and 1000 to 2200 viable cells per lobe for progenitor purified samples were used. Eight thymus lobes were pooled for each determination. Chimeric constructs were maintained as described above for recipient thymus tissue. After 12 to 14 days in culture, unless otherwise reported, cells were enzymatically digested in 0.4 mg/mL collagenase (type F and N, 1:1; Sigma, St. Louis, MO). Cell yield was assessed by a Coulter counter, and viability was assessed by trypan blue exclusion. All culture supernates were tested for viral replication using p24 enzyme-linked immunosorbent assay (ELISA), and random checks were made by co-culture with phytohemaglutinin blasts, as previously described.18
FACS analysis
Lymphocyte subsets in peripheral blood were analyzed after monoclonal antibody staining using the following panel for the NUCB2019 study: CD62L (fluorescein), CD45RA and CD45RO (phycoerythrin), and CD4 and CD8 (PerCP). Naive T cells were those that expressed both CD45RA and CD62L. For the INCAS and Era studies, the naive determination was made by expression of CD45RA and CD27. CD62L and CD27 have been shown to provide similar results for naive cell determination.19
Cells from FTOC were stained for 3-color flow cytometry with monoclonal antibodies to human CD3 (fluorescein), CD8 (phycoerythrin), and CD4 (Tricolor) or CD45 (Tricolor), major histocompatibility complex (MHC) class II (fluorescein), and MHC class I (phycoerythrin) as described.20 All monoclonal antibodies and isotype controls were obtained from Caltag (San Francisco, CA). Cells were run on a FACScan (Becton Dickinson, Braintree, MA) and analyzed with Cellquest software (Becton Dickinson). Cells were gated based on low forward-scatter and side-scatter characteristics for lymphocytes. Gated cells were analyzed for the expression of CD8/CD4 single-positive and double-positive subsets and for the expression of CD45 and MHC class II. Negative gates were set using isotype controls. Organ cultures that did not display the full spectrum of thymic subsets were excluded from further analyses.
Total human lymphocytes (THL) were calculated using percentage of cells expressing CD45 and/or MHC class II and the cell yield. The CD4 and CD8 expression were then calculated from THL. Each plate of every experiment included 1 organ culture constructed using cells from the same HIV− donor (control). The development of THL of all plates was corrected to the mean of all the control constructs (ie, if the control of plate 1 was half the mean of all controls, the THL of every dish in plate 1 was multiplied by 2). Results are expressed as the number of positive cells/thymus lobe per 10,000 cells in the original inoculum. Statistical analysis was performed using Statview (Abacus, Berkeley, CA), and statistical significance was expressed as aP value with 95% confidence.
Results
FTOC assessment of progenitor function in HIV+ persons
Although unfractionated progenitor sources gave the same result in FTOC as progenitor purified sources using samples from HIV− controls,20 it was possible that mature cells of HIV+ patients would alter the results obtained in FTOC. Mature cells from HIV-1–infected patients could persist or expand in culture and obscure the proper measurement of progenitor function, or the presence of mature cells could inhibit the development of progenitors in FTOC. Because insufficient numbers of purified CD34+ cells could be obtained from cryopreserved samples for use in FTOC, it was important to determine whether the development of progenitor cells from HIV+ patients could be examined, as had been described for HIV−participants.
PBMC samples from HIV+ patients were divided into 2 equal fractions and tested in the chimeric FTOC for their ability to develop along the normal T-cell differentiation pathway. Half was used unfractionated, and the other half was CD34+ cell-enriched before use. Because the number of CD34+ cells in each inoculum should have been approximately the same, the relative impact of mature cells on the development of CD34+ cells could be assessed. The number of CD4+, CD8+, and CD4+/CD8+ (DP) cells that developed in FTOC was slightly higher in the unfractionated group, but this difference was not statistically significant (Figure 1A). The CD34− fraction from the progenitor enrichment yielded few human cells, and these cells did not display thymocyte phenotypes (not shown).
FTOC assessment of progenitor function in HIV+ patients.
(A) CD4+, CD8+, and CD4+/CD8+ (DP) cell development in FTOC from peripheral blood of HIV+ patients. Samples were split; half were CD34+ cell enriched (▪), and the other half were used unfractionated (□). (B) Kinetics of development in FTOC from unfractionated PBMC of HIV− and HIV+participants. Immature cells were CD4+/CD3− (▪), mature cells (•) were CD3+/CD4+ or CD8+ cells (▴) represents double positive cells. Graphs show mean ± SEM of cells from 3 different donors.
FTOC assessment of progenitor function in HIV+ patients.
(A) CD4+, CD8+, and CD4+/CD8+ (DP) cell development in FTOC from peripheral blood of HIV+ patients. Samples were split; half were CD34+ cell enriched (▪), and the other half were used unfractionated (□). (B) Kinetics of development in FTOC from unfractionated PBMC of HIV− and HIV+participants. Immature cells were CD4+/CD3− (▪), mature cells (•) were CD3+/CD4+ or CD8+ cells (▴) represents double positive cells. Graphs show mean ± SEM of cells from 3 different donors.
The kinetics of development was then tested using equal numbers of unfractionated cells from HIV+ patients and HIV− controls. In both cases, few human CD3+ cells were present in the thymic construct after 3 days of culture, indicating that mature cells were not retained in the construct. Immature CD3−/CD4+ and CD8+ (not shown) T cells appeared at approximately 6 days of culture, and CD4+/CD8+ double-positive cells could be measured by day 9. Mature CD3+/CD4+ or CD8+ (not shown) T cells were found by day 12 (Figure 1B). Although the kinetics of development was the same in both groups, the number of cells that developed was lower in the HIV+donor group, particularly in the mature CD3+ subset.
All culture supernates were tested for virus production by p24 ELISA, and no culture yielded any measurable virus production. The addition of AZT, saquinavir, or a combination of the 2 drugs did not alter the reduced development in FTOC from cells of HIV+ patients (not shown).
HIV-1 infection reduces T-cell development capacity
To assess the effect of HIV-1 infection on T-cell development capacity during the course of infection, we used peripheral blood samples, from persons with known seroconversion dates, that had been cryopreserved as part of the Amsterdam Cohort Studies on AIDS. We examined the ability of CD34+ cells in these PBMC samples to develop T cells in FTOC during the course of infection. To determine whether a lack of T-cell development played a role in CD4+T-cell depletion, we compared pre-seroconversion and sequential post-seroconversion samples for patients who progressed to AIDS (progressors) and age-matched LTNPs. Progressors and LTNPs had substantially different slopes in CD4+ and CD8+T cells during the course of infection (Figure2). Characteristics of those tested are shown in Table 1.
Profile of peripheral cells during the course of infection.
Mean ± SEM number of CD4 and CD8 expressing peripheral blood cells from LTNPs (circles) and progressors (squares) during the course of infection. For the LTNP group, all patients are represented at all time points (n = 7). For the progressor group, patients were eliminated from the study with the AIDS diagnosis; therefore, for time points 0, 0.5, and 2 (n = 7), for time point 4 (n = 6), for time point 6 (n = 5), and for time point 8 (n = 2).
Profile of peripheral cells during the course of infection.
Mean ± SEM number of CD4 and CD8 expressing peripheral blood cells from LTNPs (circles) and progressors (squares) during the course of infection. For the LTNP group, all patients are represented at all time points (n = 7). For the progressor group, patients were eliminated from the study with the AIDS diagnosis; therefore, for time points 0, 0.5, and 2 (n = 7), for time point 4 (n = 6), for time point 6 (n = 5), and for time point 8 (n = 2).
Characteristics of seroconverter groups
| Subject . | Group . | Age (y) . | Follow-up (mo) . | Baseline CD4+ (per mm3) . | ΔCD4+ (per mm3 per mo) . | Baseline CD4+ development (per lobe/ 104 input) . | ΔCD4+ development (per lobe/ 104 input per mo) . |
|---|---|---|---|---|---|---|---|
| 424 | Prog | 47 | 37.9 | 860 | 34 | 16.6 | 1.4 |
| 656 | Prog | 40 | 73 | 620 | 7 | 52.1 | 0.7 |
| 1029 | Prog | 51 | 100.3 | 590 | 5.4 | 38.3 | 0.4 |
| 1031 | Prog | 57 | 105.6 | 790 | 6.9 | 34.5 | 0.3 |
| 1091 | Prog | 46 | 64.2 | 770 | 11.1 | 149 | 2.3 |
| 1094 | Prog | 52 | 61.7 | 720 | 10.7 | 78.5 | 1.2 |
| 1112 | Prog | 48 | 68.3 | 570 | 8.1 | 80.1 | 1 |
| Mean | 48.7 | 73 | 754 | 9.4 | 62.4 | 1 | |
| 545 | LTNP | 58 | 101.7 | 880 | 4.8 | 25.4 | 0.2 |
| 658 | LTNP | 49 | 97.2 | 620 | 0 | 34.4 | 0.3 |
| 1024 | LTNP | 53 | 104 | 520 | 0.9 | 70 | 0.5 |
| 1140 | LTNP | 48 | 93.6 | 630 | 2.4 | 17.6 | 0.1 |
| 1160 | LTNP | 46 | 68.6 | 720 | 0 | 24.8 | 0.3 |
| 1171 | LTNP | 40 | 94.5 | 830 | 2.3 | 112.8 | +0.2 |
| 1194 | LTNP | 51 | 96 | 790 | 3.3 | 24.1 | +0.2 |
| Mean | 49.3 | 93.7 | 711 | 2.0 | 44.2 | 0.1 |
| Subject . | Group . | Age (y) . | Follow-up (mo) . | Baseline CD4+ (per mm3) . | ΔCD4+ (per mm3 per mo) . | Baseline CD4+ development (per lobe/ 104 input) . | ΔCD4+ development (per lobe/ 104 input per mo) . |
|---|---|---|---|---|---|---|---|
| 424 | Prog | 47 | 37.9 | 860 | 34 | 16.6 | 1.4 |
| 656 | Prog | 40 | 73 | 620 | 7 | 52.1 | 0.7 |
| 1029 | Prog | 51 | 100.3 | 590 | 5.4 | 38.3 | 0.4 |
| 1031 | Prog | 57 | 105.6 | 790 | 6.9 | 34.5 | 0.3 |
| 1091 | Prog | 46 | 64.2 | 770 | 11.1 | 149 | 2.3 |
| 1094 | Prog | 52 | 61.7 | 720 | 10.7 | 78.5 | 1.2 |
| 1112 | Prog | 48 | 68.3 | 570 | 8.1 | 80.1 | 1 |
| Mean | 48.7 | 73 | 754 | 9.4 | 62.4 | 1 | |
| 545 | LTNP | 58 | 101.7 | 880 | 4.8 | 25.4 | 0.2 |
| 658 | LTNP | 49 | 97.2 | 620 | 0 | 34.4 | 0.3 |
| 1024 | LTNP | 53 | 104 | 520 | 0.9 | 70 | 0.5 |
| 1140 | LTNP | 48 | 93.6 | 630 | 2.4 | 17.6 | 0.1 |
| 1160 | LTNP | 46 | 68.6 | 720 | 0 | 24.8 | 0.3 |
| 1171 | LTNP | 40 | 94.5 | 830 | 2.3 | 112.8 | +0.2 |
| 1194 | LTNP | 51 | 96 | 790 | 3.3 | 24.1 | +0.2 |
| Mean | 49.3 | 93.7 | 711 | 2.0 | 44.2 | 0.1 |
Prog, progressor; LTNP, long-term nonprogressor.
Follow-up was the time from the known seroconversion date to AIDS diagnosis in the progressors and to approximately 8 years after seroconversion in the LTNPs. Baseline CD4+ counts and CD4+ T-cell development were from a sample at least 1 year before seroconversion. CD4+ T-cell development is expressed as the number of CD4+ cells that developed in FTOC per 104 cells in the original inoculum. ΔCD4+ is the loss of CD4+ T cells per month during follow-up. ΔCD4+ development was the change in development in FTOC during the entire course of follow-up.
After seroconversion, progressors showed a substantial reduction in the pre-seroconversion T-cell development capacity as measured by CD4+ and CD8+ T-cell development in FTOC (Figure 3A). Longitudinal analysis showed that a dramatic loss in T-cell development capacity occurred within 6 months of seroconversion for progressors (Figure 3C). The remaining T-cell development capacity was depleted during the subsequent years of infection preceding AIDS diagnosis. In contrast, LTNPs experienced a slower loss of progenitor development capacity after seroconversion (Figure 3C); at no time was the difference from pre-seroconversion statistically significant. After 8 years of infection, LTNPs retained 43.4% of their progenitor capacity compared with their pre-seroconversion level (Figure 3B). Development in FTOC did not correlate with the CD4+ T-cell count, the CD8+T-cell count, plasma HIV RNA load, or T-cell reactivity to anti-CD3 antibody (data not shown). These data strongly support a role for the loss of progenitor function in CD4+ T-cell depletion and progression to AIDS.
T-cell development in FTOC from progressors and LTNPs.
(A) CD4 and CD8 expression of cells from FTOC of samples taken during the course of infection for a representative LTNP (top panels) and progressor (bottom panels). (B) Shown is the mean (± SEM) number of CD4+, CD8+, and double-positive cells per lobe per 10 000 cells in the original inoculum that developed in FTOC. Pre-seroconversion (▪) and the last post-seroconversion sample tested (□), at AIDS diagnosis for progressors and 8 years post-seroconversion for LTNPs, are depicted. P values were calculated with Mann–Whitney U test between the groups and by Wilcoxon signed rank test within the groups. (C) Longitudinal data for CD4+ and CD8+ development in FTOC for all progressors (open squares) and LTNPs (closed circles) combined. Time 0 is the pre-seroconversion sample taken at least 1 year before seroconversion. P values were calculated with repeated-measures ANOVA. *P < .001. For the LTNP group, all patients are represented at all time points (n = 7). For the progressor group, patients were eliminated from the study with AIDS diagnosis; therefore, for time points 0, 0.5, and 2 (n = 7), for time point 4 (n = 6), for time point 6 (n = 5), and for time point 8 (n = 2).
T-cell development in FTOC from progressors and LTNPs.
(A) CD4 and CD8 expression of cells from FTOC of samples taken during the course of infection for a representative LTNP (top panels) and progressor (bottom panels). (B) Shown is the mean (± SEM) number of CD4+, CD8+, and double-positive cells per lobe per 10 000 cells in the original inoculum that developed in FTOC. Pre-seroconversion (▪) and the last post-seroconversion sample tested (□), at AIDS diagnosis for progressors and 8 years post-seroconversion for LTNPs, are depicted. P values were calculated with Mann–Whitney U test between the groups and by Wilcoxon signed rank test within the groups. (C) Longitudinal data for CD4+ and CD8+ development in FTOC for all progressors (open squares) and LTNPs (closed circles) combined. Time 0 is the pre-seroconversion sample taken at least 1 year before seroconversion. P values were calculated with repeated-measures ANOVA. *P < .001. For the LTNP group, all patients are represented at all time points (n = 7). For the progressor group, patients were eliminated from the study with AIDS diagnosis; therefore, for time points 0, 0.5, and 2 (n = 7), for time point 4 (n = 6), for time point 6 (n = 5), and for time point 8 (n = 2).
T-cell development capacity rebounds with anti-retroviral therapy
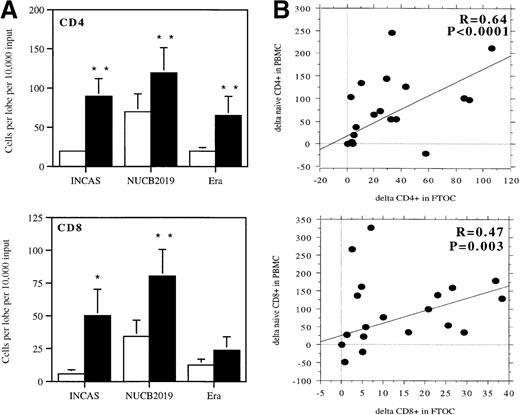
CD4+ T-cell counts, including naive CD4+ T cells, increase after the initiation of potent anti-retroviral therapy.21-23 If CD4+ T-cell depletion is partially caused by the inhibition of development, then the increase in naive CD4+ T-cell numbers after initiation of therapy should also be related to an improved developmental capacity. To determine the effect of therapy on T-cell development capacity, we studied samples from participants in 3 therapy trials: a 3 reverse transcriptase inhibitor regimen (INCAS),24 a regimen of 2 reverse transcriptase inhibitors and 1 protease inhibitor (NUCB2019),25 and a 5-drug regimen including a protease inhibitor (Era).26 After 6 months of therapy, approximately 60% of the participants experienced at least a 2-fold increase in T-cell development capacity (4 of 6 for Era, 4 of 6 for NUCB2019, 4 of 6 for INCAS) (not shown). T-cell development was substantially increased after the initiation of therapy in all 3 groups (Figure 4A). The greatest change in T-cell development capacity occurred within the first 6 months of therapy, but many participants continued to experience improvement beyond 6 months. After 18 months of therapy, 10 of the 18 patients tested (3 from Era, 4 from NUCB2019, and 3 from INCAS) had reached levels of T-cell development capacity comparable to those of uninfected persons within 18 months of the start of therapy. Most of the participants (3 from Era, 3 from NUCB2019, and 1 from INCAS) achieved this level after 6 months of therapy. Of the 11 remaining participants, 1 INCAS patient and 1 NUCB2019 patient reached normal levels after 12 months, and another INCAS patient reached them after 18 months (not shown).
Development of T cells in FTOC for participants in therapy trials.
(A) CD4+ and CD8+ T-cell development before the start of therapy (□) and after 6 months of therapy (▪) for all 18 participants. P values were calculated using Wilcoxon signed-rank test. *P < .001; **P < .005. (B) Correlation analysis for change in number of naive cells in peripheral blood and the change in the development of cells in FTOC. Graphs show the changes in naive CD4+ and CD8+ T cells in peripheral blood in the first 6 months of therapy compared with the changes in the development of CD4+ and CD8+cells in FTOC during the same period for all participants in the therapy trials. Correlations and P values were determined using the Spearman rank correlation test.
Development of T cells in FTOC for participants in therapy trials.
(A) CD4+ and CD8+ T-cell development before the start of therapy (□) and after 6 months of therapy (▪) for all 18 participants. P values were calculated using Wilcoxon signed-rank test. *P < .001; **P < .005. (B) Correlation analysis for change in number of naive cells in peripheral blood and the change in the development of cells in FTOC. Graphs show the changes in naive CD4+ and CD8+ T cells in peripheral blood in the first 6 months of therapy compared with the changes in the development of CD4+ and CD8+cells in FTOC during the same period for all participants in the therapy trials. Correlations and P values were determined using the Spearman rank correlation test.
We then determined the relationship between an increase in T-cell development capacity and the number of naive cells circulating in peripheral blood.23 There was no correlation between absolute values of these parameters (data not shown). However, the change in T-cell development capacity between day 0 and 6 months of therapy showed a positive correlation with the change in the number of circulating naive CD4+ or CD8+ T cells measured in patients during the same time period (Figure 4B). The strength of the correlation was lower for CD8 cells, but this might have been because the development of CD8+ cells in FTOC was less consistent than of CD4+ cells.
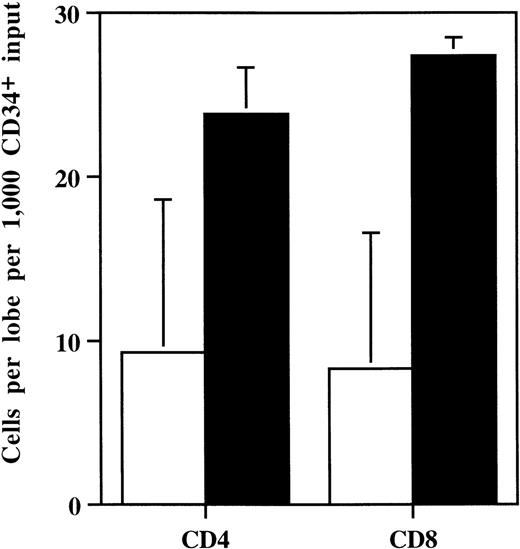
Assessment of bone marrow progenitors
Bone marrow samples were tested from 4 participants in the Era study. Bone marrow was first enriched for CD34+ cells before use in FTOC. The number of cells that developed from bone marrow obtained before therapy was lower than that found for uninfected persons.13 20 The number of cells that developed in FTOC was significantly higher after anti-retroviral therapy (Figure5). Variation of samples was much lower after treatment, possibly indicating that the effect of HIV on the bone marrow is mitigated by treatment.
Development in FTOC from bone marrow CD34+cells.
Mean (± SEM) CD4 and CD8 cell development in FTOC from CD34+ cells of bone marrow from participants in the Era trial (n = 4). P values were calculated using the Wilcoxon signed-rank test. Open bars indicate cell development before therapy; closed bars, after 6 months' therapy.
Development in FTOC from bone marrow CD34+cells.
Mean (± SEM) CD4 and CD8 cell development in FTOC from CD34+ cells of bone marrow from participants in the Era trial (n = 4). P values were calculated using the Wilcoxon signed-rank test. Open bars indicate cell development before therapy; closed bars, after 6 months' therapy.
Progenitor cell numbers
It was possible that the observed results could be explained by a difference in the number of progenitors in the inoculum. Cells from participants in the seroconverter group and the therapy trial group were stained for CD34. The number of progenitor cells in the blood expressing CD34 was lower in LTNPs after seroconversion (Figure6A). There was no difference in this parameter before and after seroconversion for the progressor group (Figure 6A). Participants in the therapy trials had slight decreases in the number of CD34+ and CD34+/CD7+cells in peripheral blood after therapy (Figure 6B). In those participants for whom bone marrow was tested, the number of total CD34+ cells increased after therapy, but the number of CD34+ cells co-expressing CD7 increased only slightly (Figure 6B).
Number of CD34+ cells.
(A) Number of CD34+ cells in peripheral blood of progressors and LTNPs (n = 7 for each group) more than 1 year before (black bars) and 2 years after (white bars) seroconversion. (B) Number of CD34+ or CD34+/CD7+ cells in bone marrow (BM) or peripheral blood mononuclear cells (PBMC) of 4 participants in the Era trial before therapy (black bars) and after 6 months of therapy (white bars). P values were determined using the Wilcoxon signed-rank test.
Number of CD34+ cells.
(A) Number of CD34+ cells in peripheral blood of progressors and LTNPs (n = 7 for each group) more than 1 year before (black bars) and 2 years after (white bars) seroconversion. (B) Number of CD34+ or CD34+/CD7+ cells in bone marrow (BM) or peripheral blood mononuclear cells (PBMC) of 4 participants in the Era trial before therapy (black bars) and after 6 months of therapy (white bars). P values were determined using the Wilcoxon signed-rank test.
Discussion
The use of the FTOC system for the assessment of T-cell progenitor capacity from uninfected persons has been previously established. We have shown that the system can be used to assess the development of cells from HIV-1 infected persons with a good degree of confidence. The data obtained from unfractionated and CD34+ cell-enriched populations were similar to those published for HIV−donors20 in which mature cells contributed little to, or detracted little from, the development of CD34+ cells in FTOC. The kinetics of development was the same in the 2 groups, with cells from HIV+ patients developing far fewer cells overall. The appearance of double-positive cells, a subset seen only during T-cell development, in cultures from unfractionated cells demonstrates that CD34+ cells in the inoculum could enter the thymus tissue and develop into T cells. Virus production in these cultures did not appear to play a role in the reduced development observed with samples from HIV+ persons because the addition of anti-retroviral drugs to the cultures did not alter the outcome.
Our data provide strong evidence for HIV-1–related decreases in the T-cell development capacity of progenitors. The difference in the developmental profiles between progressors and LTNPs suggests that the HIV-1–related inhibition of T-cell development capacity plays a role in CD4+ T-cell depletion and progression to AIDS. A reduction in the developmental capacity of progenitor cells can result in a decrease in the number of newly produced cells. If cells lost by natural death or HIV-1–induced killing are not replaced, eventual depletion of the pool of cells could be expected. This could help explain the observed impact of HIV-1 on naive cells during infection, though these cells are not considered primary targets for infection.27 In time, naive cells will be primed to an activated phenotype, and, if the naive pool is not replenished, the pool will effectively be depleted.28 These data also explain the observed loss of naive CD8+ T cells during infection.28 Impaired progenitor function would be expected to affect the development of CD4+ and CD8+cells and to result in a decrease in the number of naive cells of both phenotypes produced.
Potent anti-retroviral therapy has been reported to result in increases in the number of CD4+ T cells in the periphery. In the first few weeks, this increase in CD4+ cells is most likely the result of a redistribution from the lymphoid tissue because it concerns mainly cells with a memory phenotype.21-23,29 A slow increase in the number of naive cells can be observed. Our results suggest that this increase in naive cells can be related to a restoration of T-cell development capacity. There was a very strong correlation between the change in the number of naive CD4+and CD8+ T cells in the periphery during therapy with the change in the developmental capacity measured in FTOC for the same period. Thus, reconstitution of the number of naive circulating CD4+ T cells is related to an increase in T-cell development capacity during therapy. Results from FTOC for participants in therapy trials showed that approximately 70% had a 2-fold or better increase in T-cell development capacity after 6 months of therapy, regardless of the regimen. However, only 10 of the 18 persons had reached normal levels of T-cell development capacity after more than a year of therapy. These data show that the decrease in T-cell development capacity is, in some cases, reversible but that immune reconstitution will be slow, as expected from other studies.30
In this study approximately 30% of participants did not respond with increases in T-cell development capacity, and changes in the numbers of naive cells in vivo were extremely small. This may indicate an irreversible effect of HIV-1 infection on progenitors in some persons. These persons might also have had previous impairment of progenitor function, but, without a pre-seroconversion assessment, the actual cause could not be determined. Additionally, some increases in T-cell development capacity were not accompanied by increases in naive CD4+ T cells during therapy. These observations may indicate potential problems with the other parameter important for naive T-cell development, the thymus. If the progenitor cell function increases but the function of the thymus is insufficient, new T cells will not develop. Indeed, it has recently been reported that only approximately 30% of infected persons older than 40 had thymi of substantial size, which correlated with the number of circulating naive CD4+ T cells.11 This is also consistent with the report that a fraction of treated patients do not experience immune reconstitution despite long-term HIV-1 suppression.19 It remains to be determined which parameters are involved in a patient experiencing increases in T-cell development during therapy.
The mechanism for HIV-1–related inhibition of T-cell development capacity has not been determined. One possibility is that the number of CD34+ cells is reduced in infected persons. There are conflicting reports on this subject. In our own study, we did not find a decrease in the number of circulating CD34+ cells after seroconversion in progressors, but, paradoxically, a slight decrease was found in LTNPs. We also did not detect an increase in the number of circulating CD34+ cells in patients on therapy concomitant with their improved T-cell development in FTOC or increase in naive cell numbers. In bone marrow, there was an increase in the total number of CD34+ cells after therapy but only a slight increase in the mean number of lymphocyte-committed CD7+cells, with some participants experiencing no increases at all. It does not appear that the number of progenitors was responsible for the observations we report.
In this system, a linear relationship between input numbers and output numbers could be observed between 105 and 106input cells per lobe, with a log increase in input translating to an approximately 2-fold increase in output.8 There was approximately 1 progenitor per 105 cells, and 105 cells can fully reconstitute a fetal thymus lobe. Therefore, small differences in the number of cells used in this study would not be responsible for the observed differences in T-cell development. These data, therefore, indicate that decreased T-cell development capacity is the result of decreased T-cell development per T-cell progenitor.
A second possibility is that there is some alteration in the migration of progenitors such that the CD34+ cells in peripheral blood of infected persons are not the same as those in uninfected persons. This is an unlikely explanation because there was no difference in the numbers of lymphocyte-committed progenitors after seroconversion. Additionally, development from bone marrow showed the same response to infection and therapy as peripheral blood.
Numerous other possibilities have yet to be investigated. One is that the cytokine imbalance seen in HIV-1 infection prevents the proper development of bone marrow progenitors. Several pro-inflammatory cytokines, such as TGF-β and TNF-α, are produced at inflated levels during HIV-1 infection29,31-35and are potent inhibitors of hematopoiesis.36-39 During therapy, the level of inhibitory cytokines has been shown to decrease,40,41 which may allow progenitors to develop normally. There are also possible direct effects of virus or viral products on progenitors38 42-44 that could be reversed with the decrease in viral replication associated with therapy.
In conclusion, several lines of evidence now point to interference with T-cell renewal in HIV-1 infection. Our data suggest that part of the interference is a diminished capacity of progenitors to develop into T cells. Furthermore, lack of development of new cells would be expected to contribute to the T-cell depletion that is the hallmark of HIV-1 infection. With the use of potent antiretroviral therapy, the function of T-cell progenitors is restored in most patients.
Acknowledgments
We thank all who donated blood and bone marrow for this study and all the clinicians who were involved, particularly R. Kauffmann, N. Foudraine, P. Meenhorst, H. Sprenger, M. van der Ende, and C. ten Napel. We thank R. van Rij and M. Brower for performing p24 ELISA, the laboratory of M. T. L. Roos for immunological assays, and E. Tanger for maintaining the murine breeding colony. Mice were provided by H. Spits at The Netherlands Cancer Institute.
Supported by grants from The Netherlands Foundation for Preventive Medicine, The Netherlands Organization for Scientific Research, and the Dutch AIDS Foundation. Glaxo-Wellcome sponsored NUCB2019 and the Era study, Boehringer Ingelheim sponsored INCAS and the Era study, and Abbott Laboratories sponsored NUCB2019.
Performed as part of the Amsterdam Cohort Studies on AIDS.
Reprints:Frank Miedema, Research and Development Division, CLB, Sanquin Blood Supply Foundation, Plesmanlaan 125, 1066CX, Amsterdam, The Netherlands; e-mail: f_miedema@clb.nl.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal