Abstract
Acute promyelocytic leukemia (APL) is characterized by a specific translocation, t(15;17), that fuses the promyelocytic leukemia (PML) gene with the RA receptor RARα. Pharmacologic doses of retinoic acid (RA) induce differentiation in human APL cells and complete clinical remissions. Unfortunately, APL cells develop resistance to RA in vitro and in vivo. Recently, mutations in PML/RARα have been described in APL cells from patients clinically resistant to RA therapy. The mutations cluster in 2 regions that are involved in forming the binding pocket for RA. These mutant PML/RARα proteins have been expressed in vitro, which shows that they cause a diversity of alterations in binding to ligand and to nuclear coregulators of transcription, leading to varying degrees of inhibition of retinoid-induced transcription. This contrasts with the nearly complete dominant negative activity of mutations in PML/RARα previously characterized in cell lines developing RA resistance in vitro. Current data from this study provide additional insight into the molecular mechanisms of resistance to RA and suggest that alterations in the ability of mutants to interact with coregulators can be determinant in the molecular mechanism of resistance to RA. In particular, ligand-induced binding to the coactivator ACTR correlated better with transcriptional activation of RA response elements than the ligand-induced release of the corepressor SMRT. The diversity of effects that are seen in patient-derived mutations may help explain the partial success to date of attempts to overcome this mechanism of resistance in patients by the clinical use of histone deacetylase inhibitors.
Introduction
Acute promyelocytic leukemia (APL) accounts for approximately 10% of all cases of acute myeloid leukemia. APL is a unique subtype of leukemia characterized by a distinct chromosomal translocation, t(15;17), with breakpoints within the retinoic acid receptor alpha (RARα) gene on chromosome 17q21 and a gene termed PML (promyelocytic leukemia), on chromosome 15q22. This translocation generates a chimericPML/RARα gene and a PML/RARα fusion protein.1-4 The resulting fusion protein is found in all APL patients and contributes to the pathogenesis of the disease. The oncogenic potential of PML/RARα derives from its ability to inhibit, in a dominant negative fashion, both PML- and RARα-signaling pathways. This inhibition of PML and RARα functions leads to a block of myeloid differentiation and ultimately to the APL phenotype.5 6
The fusion protein consistently retains both the DNA-binding C-domain of the RARα and the E-domain, which is required for ligand binding and receptor dimerization.7,8 When dimerized with a retinoid X receptor (RXR), RARs bind to the retinoic acid response elements (RAREs) on target genes and activate transcription in the presence of all-trans retinoic acid (RA). In the absence of ligand, RXR/RAR heterodimers interact with nuclear receptor corepressors (termed SMRT and N-CoR) that recruit histone deacetylases to induce chromatin modifications and transcriptional repression.9,10 In APL, the PML/RARα fusion protein can heterodimerize with RXR, bind RA, and activate transcription through the RAREs.11,12 All-transRA can dissociate SMRT from both RARα and PML/RARα, but higher concentrations are required for the fusion protein, suggesting a more tightly associated PML/RARα–SMRT complex. The differentiation block by PML/RARα may be due to the association of the corepressor complex and the inability to dissociate this complex with physiological concentrations of RA.13 The release of corepressor induced by pharmacological concentrations of RA may underlie the cytodifferentiation of APL cells.14
RA therapy induces complete remission in a high percentage of patients with APL.15 Unfortunately, the duration of response is short, and further therapy with this agent is less effective, suggesting the development of drug resistance.16-19 Explanations for this resistance include progressive reduction of RA plasma concentration, which may be explained by an increased level of cellular RA-binding protein (CRABP),20 an increased oxidative catabolism of RA by cytochrome P450 enzyme activity, or multidrug-resistance (MDR) gene product.21,22 But additional genetic mechanisms of retinoid resistance, such as mutations in nuclear retinoid receptors, have previously been found in HL-60 myeloid leukemic cells.23-25
In vitro studies on APL cells are provided by a cell line, NB4, derived from an APL patient.26 Our laboratory, and others, have developed RA-resistant NB4 subclones to study cellular or molecular mechanisms that mediate retinoid response or resistance.27-29 We have reported RA-resistant subclones that are highly resistant to natural and synthetic retinoids that do not bind CRABP and are not metabolized by P450 enzymes.29,30 We identified a point mutation in the ligand-binding domain (LBD) of the RARα portion of the PML/RARα fusion protein in the RA-resistant NB4 subclone, NB4-R4.31Relative to the RARα sequence,32 the mutation is located at the amino acid 398, where the leucine (L) is replaced by a proline (P) (L398P) in helix 11 (H11) of the LBD. The mutant PML/RARα does not bind ligand but retains the ability to bind RXRα and RAREs and to block the transcription of RA-responsive genes in a dominant negative fashion. We found that pharmacologic concentrations of RA could not release the corepressor SMRT from this PML/RARα mutant, suggesting that the phenotypic RA resistance may be directly coupled to the inability to dissociate the corepressor complex and activate retinoid target genes.13 There have been 4 additional mutations reported in independently developed RA-resistant subclones.33-36 On the basis of these findings, mutations in the E-domain of the RARα portion of the fusion protein PML/RARα appear to be an important mechanism of developing RA resistance in vitro.
Recently, mutations in the RARα/E-domain of thePML/RARα chimeric gene were reported in APL cells from patients who developed RA resistance, confirming the clinical relevance of molecular aberrations in the retinoid receptors. In 2 patients who exhibited RA resistance at relapse, Imaizumi et al37 identified mutations in thePML/RARα chimeric gene. Both mutations were absent at the onset of the disease, suggesting that the alterations were acquired during clinical therapy. The 2 mutations result respectively, in amino acid changes from arginine (R) to glutamine (Q) at codon 272, and from methionine (M) to leucine at 297, according to the sequence of the RARα.32 The mutation R272Q is located in the H5, and the other one, M297L, in the H6 of the LBD of the fusion protein.
At the same time, Ding et al38 foundPML/RARα mutations in 3 patients of 12 who received RA in combination with chemotherapy, but none of 8 who received chemotherapy alone. The mutations identified in these patients resulted in the replacement of leucine with valine (V) at codon 290, arginine with tryptophan (W) at codon 394, and methionine with threonine (T) at codon 413, respectively. The L290V mutation lies between H5 and H6 in the central region of the LBD, whereas the R394W and the M413T mutations are located at the carboxy-terminal region of RARα LBD within H11 and H12, respectively. Very recently, additionalPML/RARα mutations have been reported in RA-resistant APL relapsed patients.39 40 None of these studies found mutations in the coexpressed nonrearranged RARα orPML genes.
The goal of this study was to characterize the phenotype of these clinically observed mutations and determine how these mutations, found in RA-resistant APL patients, could impair the ligand-induced and transcriptional functions of the RARα/E-domain of the fusion protein. In vitro expression of these mutant PML/RARα proteins shows that these amino acid changes cause a variety of abnormalities in the ligand-binding, transactivation of RAREs and ligand-dependent binding to the nuclear corepressor SMRT and coactivator ACTR. The results of our analysis provide additional insight into the molecular mechanism of resistance to RA and suggest that the inability of mutants to interact with nuclear coregulators of transcription, in a ligand-dependent manner, can be determinant in the development of resistance to RA.
Materials and methods
Cell culture
The Cos-1 cells were grown in RPMI-1640 medium (Life Technologies, Inc [GIBCO BRL], Burlington, Ontario, Canada), supplemented with 10% fetal calf serum (FCS) (Wisent Inc; St-Bruno, Quebec, Canada) and incubated in a humidified chamber at 37°C with a 5% CO2 environment.
Plasmid constructs
The PML/RARα with either R272Q or M297L mutations were cloned into the pCMX mammalian expression vector harboring the short form (S-form) of the wild-type PML/RARαcomplementary DNA (cDNA) by means of a QuikChange Site-Directed Mutagenesis kit (Stratagene; La Jolla, CA). The PML/RARα with either L290V or R394W mutations was derived from pSG5 mammalian expression vector harboring the wild-type PML/RARα S-form cDNA by means of the Gene Editor kit (Promega, Madison, WI) for the site-directed mutagenesis, whereas the PML/RARα with M413T mutation was also cloned into the pSG5 expression vector but harboring the long form (L-form) of the wild-type PML/RARα cDNA. All the constructs were verified by sequencing analysis, by means of the dsDNA Cycle Sequencing System (Life Technologies). The construction of the mammalian expression vector for PML/RARα L-form harboring the L398P mutation (PML/RARα–m4), from the NB4-R4 resistant cells, was previously described.31
Assay for ligand-binding activity
The Cos-1 cells were transiently transfected by electroporation with the expression vectors containing either wild-type or mutant PML/RARα. Nuclear extracts were prepared from 1 to 5 × 108 cells and incubated for 18 hours at 4°C with 10 nmol/L [3H]-RA (50.7 Ci/mmol; DuPont-NEN, Boston) or with [3H]-RA in the presence of 200-fold excess of unlabeled RA, as previously described.11 The extracts were subsequently fractionated at 4°C by HPLC by means of a superose 6 HR 10/30 size exclusion column (Pharmacia, Uppsala, Sweden). The flow rate was 0.4 mL/min; fractions of 0.4 mL were collected; and radioactivity was determined by means of a liquid scintillation counter. The HPLC system was calibrated by means of a series of molecular weight (MW) markers, consisting of the following: blue dextran, MW 2 000 000; thyroglobulin, MW 669 000; β-amylase, MW 200 000; bovine serum albumin, MW 66 000; and ovalbumin, MW 45 000.
Limited proteolytic digestion of translated fusion proteins
Wild-type and mutant PML/RARα fusion proteins were synthesized in vitro by means of a coupled transcription and translation reticulocyte lysate system for 90 minutes at 30°C as suggested by the manufacturer (Promega). The reaction was performed in the presence of [35S]-methionine (NEN; Streetsville, Ontario, Canada) to produce radioactive fusion proteins. We incubated 5 μL of in vitro synthesized wild-type or mutated PML/RARα proteins with 1 μmol/L of all-trans RA (Sigma, St Louis, MO) for up to 30 minutes at room temperature in the dark. After treatment with 0.5 μL of different concentrations of trypsin (Sigma-Aldrich Canada Ltd; Oakville, Ontario, Canada) for 10 minutes at room temperature, 20 μL of denaturing loading dye was added. An equal volume of water was added for the undigested controls or untreated samples. The samples were denatured and directly analyzed by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (10% wt/vol). The gels were then dried and exposed for autoradiographic analysis.
Transient transfection experiments for transcriptional activity
Cos-1 cells were grown in RPMI-1640 with 10% FCS and were seeded at 120 000 cells per well in 6-well plates 1 day before transfection. Cells were rinsed with serum-free OPTI-MEM (Life Technologies) and transfected by the lipofectamine method (Life Technologies) with 0.7 μg of wild-type or mutant fusion protein plasmids, 1 μg of the reporter plasmids DR5-tk-CAT41 or TREpal-tk-CAT,41 and 0.3 μg of pCMV-βGalactosidase (βGal) as an internal control for transfection efficiency. Cells were transfected for 5 hours, replenished with 2 mL of RPMI-1640 with 10% FCS, and grown for 24 hours in the absence or presence of different concentrations of RA. The chloramphenicol acetyltransferase (CAT) activity was measured by means of a modified protocol of the organic diffusion method.42 Briefly, 50 μL of cell extract was incubated at 37°C for 1 to 5 hours with 200 μL of 1.25 mmol/L cold chloramphenicol (ICN; Costa Mesa, CA) dissolved in 100 mmol/L Tris-Cl, pH 7.8, and 0.25 μCi [3H]-labeled acetyl coenzyme A (NEN). The reaction was extracted with Ready Organic Scintillation Cocktail (Beckman; Mississauga, Ontario, Canada), and 750 μL of the organic phase was counted on a scintillation counter. The CAT counts were normalized with βGal activity43 to obtain the relative CAT activity.
Electrophoretic mobility shift assays
Electrophoretic mobility shift assays were performed with the use of a direct-repeat 5 (DR5) RARE. The nucleotide sequence of the [32P]-labeled oligonucleotide duplex used was as follows: 5′-agcttcAGGTCAccaggAGGTCAgagagct-3′. [35S]-labeled wild-type and mutant PML/RARα fusion proteins were synthesized by means of a coupled transcription and translation reticulocyte lysate system, according to the manufacturer's recommended protocol (Promega). Equal counts of in vitro translated wild-type and mutant fusion proteins, purified glutathione S-transferase (GST) fusion proteins (1 μg), and [32P]-labeled DR5 (100 000 cpm) were incubated with or without RA, as indicated with the following: 0.3 μg poly (dI:dC) for 30 minutes at room temperature in a 24-μL reaction containing 100 mmol/L KCl; 6% glycerol; 10 mmol/L Tris, pH 8.0; 0.05% NP-40; and 1 mmol/L dithiothreitol. Where specified, bacterially expressed and purified GST fusions containing the receptor interacting domains of SMRT (GST-SMRT-IDII; amino acid 1073-1168; 1 μg/lane) or ACTR (GST-ACTR–RID; amino acid 621-821; 1 μg/lane) were added.13 44 The protein-DNA complexes were resolved on a 4.5% native polyacrylamide gel electrophoresis in 0.5X TBE and visualized by autoradiography.
Results
PML/RARα mutations analyzed in this study
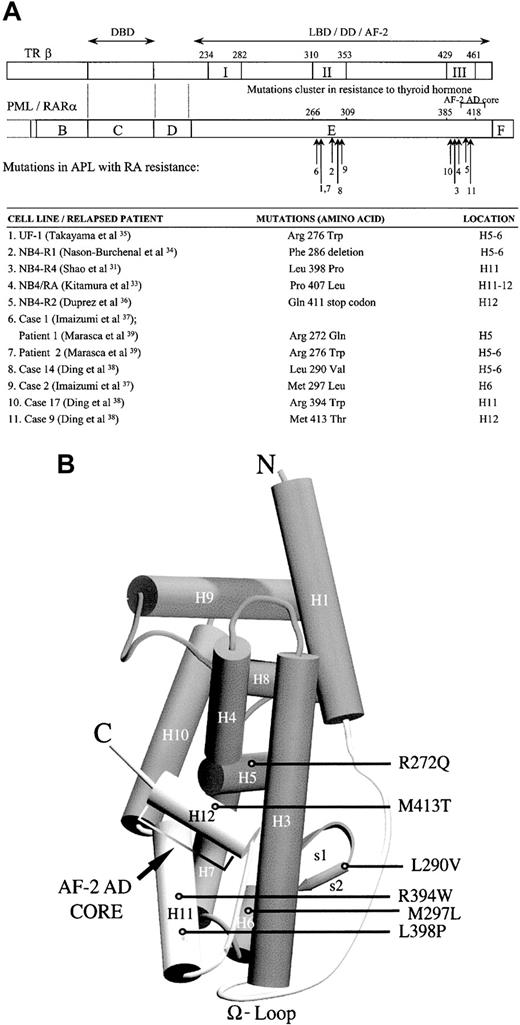
Figure 1 presents the summary of the LBD PML/RARα mutations associated with RA resistance in cell lines (numbers 1-5) and in APL patients (numbers 6-11). In this study, the phenotypes of the first PML/RARα natural mutations identified in RA-resistant APL patients were characterized. Transcriptional properties of the mutations, indicated by number 6, 8, 9, 10, and 11 in Figure 1A, were examined to discover the extent of functional impairment. The locations of the mutations were described with reference to normal protein of RARα1,32 because their position in the fusion molecule depends on the isoforms of PML/RARα messenger RNA. Approximate locations of the evaluated mutations in the 3-dimensional structure of the RAR LBD are shown in Figure 1B.
Schematic representations of the PML/RARα mutations.
(A) Schematic of the LBD PML/RARα mutations identified in RA-resistant APL cell lines (numbers 1-5) and relapsed patients (numbers 6-11). The alignment of TRβ LBD and the PML/RARα E-domain by sequence homology indicates that the mutations in RA-resistant APL patients and cell lines cluster in accordance with the regions in resistance to thyroid hormone (RTH) syndrome denoted as I, II, and III. Numbers 6, 8, 9, 10, and 11 indicate the mutations in the LBD PML/RARα of RA-resistant APL patients evaluated in this study. The position of the mutations is described with reference to normal amino acid sequence of RARα1.32 DBD indicates DNA-binding domain; LBD, ligand-binding domain; DD, dimerization domain; AD, activation domain. (B) A 3-dimensional model of the LBD of the holo-RAR, showing the locations of the evaluated mutants. The structure of the LBD is based on x-ray crystal structure analysis of the liganded RARγ.45,46
Schematic representations of the PML/RARα mutations.
(A) Schematic of the LBD PML/RARα mutations identified in RA-resistant APL cell lines (numbers 1-5) and relapsed patients (numbers 6-11). The alignment of TRβ LBD and the PML/RARα E-domain by sequence homology indicates that the mutations in RA-resistant APL patients and cell lines cluster in accordance with the regions in resistance to thyroid hormone (RTH) syndrome denoted as I, II, and III. Numbers 6, 8, 9, 10, and 11 indicate the mutations in the LBD PML/RARα of RA-resistant APL patients evaluated in this study. The position of the mutations is described with reference to normal amino acid sequence of RARα1.32 DBD indicates DNA-binding domain; LBD, ligand-binding domain; DD, dimerization domain; AD, activation domain. (B) A 3-dimensional model of the LBD of the holo-RAR, showing the locations of the evaluated mutants. The structure of the LBD is based on x-ray crystal structure analysis of the liganded RARγ.45,46
RA-binding activity of the wild-type and mutant PML/RARα fusion proteins
To evaluate how these point mutations of PML/RARα alter the function of the LBD, we examined their RA-binding activity. Binding of [3H]-RA to nuclear extracts from Cos-1 cells transiently transfected with the wild-type or the mutant PML/RARα expression vectors was analyzed. The size exclusion HPLC profile of extracts from cells expressing the wild-type form of PML/RARα is characterized by 3 main peaks as previously described.11 The 50-kd peak represents the endogenous RARs in Cos-1 cells. The 110-kd peak characterizes the binding of PML/RARα monomers, and the approximately 670-kd peak represents macromolecular complexes formed by the interaction of PML/RARα with itself and/or other nuclear proteins. The HPLC profiles of extracts from cells expressing the PML/RARα mutations R394W and M413T are similar to the pattern observed with the wild-type form, indicating that these mutations in the LBD of PML/RARα do not substantially impair the binding of ligand (Figure2). Nuclear extract from cells expressing the PML/RARα mutations M297L and R272Q showed HPLC profiles consistent with the elution of PML/RARα macromolecular nuclear complexes in fractions corresponding to MWs of about 400 to 200 kd. In addition, the mutation R272Q of PML/RARα decreased RA binding to the fusion protein. Specific RA-binding activity was not detectable in nuclear extracts prepared from cells transiently transfected with the PML/RARα containing the mutation L290V (Figure 2A).
Specific nuclear RA-binding activity in Cos-1 cells transfected with wild-type in comparison with those transfected with mutant PML/RARα fusion proteins.
HPLC RA-binding profiles of wild-type (top panels) and mutant (bottom panels) PML/RARα S-form (A) and L-form (B). Nuclear extracts were incubated with 10 nmol/L [3H]-RA or with [3H]-RA in the presence of 200-fold excess of unlabeled RA. Extracts were subjected to HPLC analysis using a 6 HR 10/30 size exclusion column.
Specific nuclear RA-binding activity in Cos-1 cells transfected with wild-type in comparison with those transfected with mutant PML/RARα fusion proteins.
HPLC RA-binding profiles of wild-type (top panels) and mutant (bottom panels) PML/RARα S-form (A) and L-form (B). Nuclear extracts were incubated with 10 nmol/L [3H]-RA or with [3H]-RA in the presence of 200-fold excess of unlabeled RA. Extracts were subjected to HPLC analysis using a 6 HR 10/30 size exclusion column.
Proteolytic analysis of the wild-type and mutant PML/RARα
We predicted that changes in the ligand binding of mutated receptors would correlate with altered conformations of the receptors. Because proteolytic analysis is a powerful method for analyzing conformational changes within proteins, we performed a limited trypsin digestion of the wild-type and mutated fusion proteins in the absence and presence of RA (Figure 3). Distinct fragment patterns were observed for the wild-type and for certain mutant fusion proteins, mainly after RA treatment. The distinction centered around a fragment at 32 kd and 2 closely migrating fragments at 36 to 37 kd. The S- and L-forms of wild-type PML/RARα did not differ in digestion pattern (Figure 3). In the absence of RA, a 32-kd fragment was more resistant to trypsin digestion. After 1 μmol/L RA treatment, the 32-kd fragment disappeared, whereas 2 fragments of 36 to 37 kd were more resistant to protease treatment. As with human RARα,47 human progesterone receptor,47 and human estrogen receptor,48 ligand binding causes a conformational change of PML/RARα, resulting in the modification of accessibility of trypsin cleavage sites. Analysis of the mutations M297L and M413T showed that their trypsin digestion patterns are identical to that of the wild-type. The digestion patterns for the mutated R272Q and R394W PML/RARα differ from that of the wild-type by the presence of an intense 32-kd resistant fragment after RA treatment. These results indicate that RA can still bind to the mutated fusion protein LBD, but induces a different conformational change than in the wild-type LBD. In the case of the mutation L290V, the trypsin digestion pattern after RA treatment is completely different from that of the wild-type: the 32-kd fragment is still present and the 36- to 37-kd fragments are absent. The identical digestion patterns in the absence and presence of RA indicate that the mutated fusion protein does not bind the ligand, which is consistent with our ligand-binding analysis (Figure 2A). The same results were obtained with the mutation found in NB4-R4 cells, PML/RARα (m4), which we have previously shown is not able to bind RA.31
RA-induced conformational changes in wild-type and mutant PML/RARα fusion proteins.
Limited trypsin digestion analysis of wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro [35S]-methionine synthesized PML/RARα proteins were incubated without (−) or with (+) 1 μmol/L RA, and subsequently treated with increasing trypsin concentrations (0 to 25 μg/mL). Digestion products were analyzed by denaturing electrophoresis. The arrows indicate the intact PML/RARα proteins. Asterisks indicate resistant fragments.
RA-induced conformational changes in wild-type and mutant PML/RARα fusion proteins.
Limited trypsin digestion analysis of wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro [35S]-methionine synthesized PML/RARα proteins were incubated without (−) or with (+) 1 μmol/L RA, and subsequently treated with increasing trypsin concentrations (0 to 25 μg/mL). Digestion products were analyzed by denaturing electrophoresis. The arrows indicate the intact PML/RARα proteins. Asterisks indicate resistant fragments.
Ligand-dependent transcriptional activity
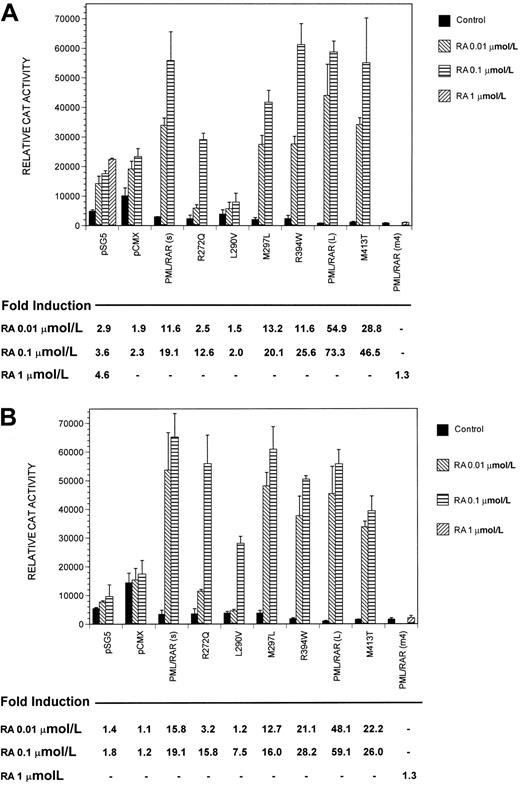
The conformational changes induced by certain mutations might also be expected to alter protein-protein interactions that are required for RARE binding and activation. Thus, we compared the transcriptional activity of PML/RARα mutants with that of the wild-type fusion protein on 2 retinoid-responsive elements. Fusion protein plasmids were cotransfected into Cos-1 cells with tk-CAT reporters driven by either a DR5 RARE (Figure 4A) or a palindromic thyroid response element TREpal (Figure 4B). Figure 4 showed that RA slightly induced transcription of both DR5-tk-CAT and TREpal-tk-CAT reporters cotransfected with the empty vectors (pSG5 and pCMX), consistent with the known endogenous RAR present in Cos-1 cells. The wild-type PML/RARα S-form and L-form acted as dominant negative inhibitors of the control transcriptional activity for both DR5-tk-CAT and TREpal-tk-CAT reporters (Figure 4), reducing the baseline CAT activity as compared with the empty vectors. This dominant negative activity of the fusion protein is maintained in all PML/RARα mutants, as exhibited by a smaller baseline CAT activity than was seen with the empty vectors. As shown in Figure 4, ligand-dependent transcriptional activity of both S-form and L-form of the wild-type PML/RARα chimeric proteins was increased in a manner dependent on RA concentrations. The PML/RARα L-form stimulated the RA-induced transcription more efficiently than the S-form (Figure 4). The PML/RARα chimeric proteins harboring either M297L or R394W mutations showed a ligand-dependent transcriptional activity on both tk-CAT reporters that was similar to the wild-type S-form fusion protein (Figure 4). In contrast, the mutant R272Q and L290V fusion proteins had an altered transcriptional activity on DR5 and TREpal reporters in the presence of RA. The mutant R272Q showed no increase in CAT activity in the presence of 0.01 μmol/L RA on the DR5 (Figure 4A) and on the TREpal (Figure 4B). In the presence of 0.1 μmol/L RA, both reporters produced increased transcriptional activity that remained less than that of the wild-type PML/RARα. The mutated form, PML/RARα L290V, has significantly lost ligand-dependent transcriptional activity on both reporters (Figure 4). As previously reported, PML/RARα (m4) does not activate transcription in response to even 1 μmol/L RA, on all reporters tested (Figure 4 and data not shown). The PML/RARα fusion protein harboring M413T mutation showed a loss of approximately half of the CAT activities on RARE reporters, as compared with the wild-type L-form PML/RARα, in the presence of RA (Figure 4). Similar results were obtained with the use of a DR5-tk-LUC reporter (data not shown).
Transcriptional activity of wild-type and mutant PML/RARα fusion proteins.
DR5-tk-CAT (A) or TREpal-tk-CAT (B) reporters were cotransfected with the indicated PML/RARα. The pCMX and the pSG5 represent the vectors alone. Relative CAT activity without (control) or with indicated concentrations of RA is shown, with the calculated corresponding fold induction below. Each data point represents results from at least 3 independent transfections. Control, ▪; RA 0.01 μmol/L, ▧; RA 0.1 μmol/L, ▤; RA 1 μmol/L, ▨.
Transcriptional activity of wild-type and mutant PML/RARα fusion proteins.
DR5-tk-CAT (A) or TREpal-tk-CAT (B) reporters were cotransfected with the indicated PML/RARα. The pCMX and the pSG5 represent the vectors alone. Relative CAT activity without (control) or with indicated concentrations of RA is shown, with the calculated corresponding fold induction below. Each data point represents results from at least 3 independent transfections. Control, ▪; RA 0.01 μmol/L, ▧; RA 0.1 μmol/L, ▤; RA 1 μmol/L, ▨.
Ligand-dependent corepressor SMRT release by wild-type and mutant PML/RARα fusion proteins
Ligand-dependent activation of nuclear receptors is associated with displacement of corepressors and recruitment of coactivating proteins. To determine the molecular mechanism of RA resistance caused by these mutants, the interactions of wild-type and mutants with the corepressor, SMRT, and the coactivator, ACTR, were tested in gel shift assays. We first evaluated the binding of mutants to the receptor interacting domain (IDII) of the corepressor SMRT, using an electromobility shift assay. In vitro translated wild-type and mutant PML/RARα bound a radio-labeled DR5 element in the absence of SMRT-IDII. Addition of purified GST-SMRT-IDII shifted the bound complex, as indicated by an arrow in Figure5. Binding of GST-SMRT-IDII to each of the mutants was similar to the wild-type PML/RARα in the absence of RA. In contrast, ligand-induced dissociation of SMRT-IDII from certain mutants was very different from the wild-type. As previously reported, the wild-type PML/RARα fusion proteins completely dissociated SMRT-IDII at RA concentrations between 10−6 and 10−5 mol/L (Figure 5). PML/RARα harboring the mutations M297L or R394W required about 10-fold higher concentrations of RA to dissociate the corepressor SMRT than did the wild-type (Figure 5A). The fusion proteins harboring the mutations R272Q, L290V, M413T, or PML/RARα (m4) could not be dissociated from the corepressor SMRT-IDII even at 10 μmol/L RA concentration (Figure 5), indicating that these mutants required more than 100-fold higher concentrations of RA to dissociate SMRT than did the wild-type.
Ligand-dependent dissociation of the corepressor SMRT from wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay.
Interaction of SMRT with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-SMRT-IDII in the presence of increasing concentrations of RA. The position of the complex shifted by SMRT is indicated.
Ligand-dependent dissociation of the corepressor SMRT from wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay.
Interaction of SMRT with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-SMRT-IDII in the presence of increasing concentrations of RA. The position of the complex shifted by SMRT is indicated.
Recruitment of the coactivator ACTR by mutants PML/RARα
In the presence of ligand, proteins termed coactivators are recruited to mediate the ligand-dependent response. To test whether mutants of PML/RARα could normally recruit the coactivator ACTR, the central receptor-interacting domain of ACTR (ACTR-RID) fused to the GST protein was expressed in bacteria. Purified GST–ACTR-RID and in vitro translated fusion proteins were then employed in a gel-shift study of wild-type and mutated PML/RARα to a DR5 probe (Figure6). In the absence of RA, ACTR-RID did not form a complex with the wild-type or mutated fusion proteins. The wild-type PML/RARα–ACTR-RID complex was first noted at 0.01 μmol/L and was maximal at 0.05 μmol/L RA. The M297L mutant appeared to be similar to the wild-type in its ability to recruit ACTR-RID over the RA concentrations tested (Figure 6A). The mutant M413T required about 10-fold greater RA concentrations, relative to the wild-type, to begin the recruitment of ACTR-RID (Figure 6B). The protein harboring the mutation R394W started recruiting the coactivator at 0.01 μmol/L as did the wild-type, but its association is maximal only at 1 μmol/L RA, as compared with 0.05 μmol/L for the wild-type. The mutant R272Q and L290V fusion proteins were least able to associate with the coactivator. The mutation R272Q is fully associated with ACTR-RID only at 1 μmol/L RA, which is 20-fold greater than for the wild-type association. PML/RARα harboring the mutation L290V showed only minimal recruitment of ACTR at 1 μmol/L RA, which indicates that the coactivator needs more than 100-fold RA concentrations for its association with this mutated fusion protein. The mutation PML/RARα (m4) showed that even with 1 μmol/L RA, ACTR-RID was not able to bind the fusion protein (Figure 6B).
Differential recruitment of the coactivator ACTR by wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay.
Interaction of ACTR with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-ACTR-RID in the presence of increasing concentrations of RA. The position of the complex shifted by ACTR indicated.
Differential recruitment of the coactivator ACTR by wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay.
Interaction of ACTR with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-ACTR-RID in the presence of increasing concentrations of RA. The position of the complex shifted by ACTR indicated.
Discussion
APL has the unique characteristic of responding in vitro and in vivo to differentiation therapy with RA. The chimeric protein PML/RARα retains the majority of the functional domains of theRARα gene, in particular the DNA- and the ligand-binding domains, maintaining the capacity to bind the ligand and activate transcription. RA used alone in APL treatment induces clinical remission in a range of 72% to 100%.15 Unfortunately, acquired clinical RA resistance appears within a few months of treatment, and relapse occurs in almost all patients who do not receive additional cytotoxic therapy. Therefore, the development of resistance to RA in patients with acute promyelocytic leukemia is one of the major problems that limit the effectiveness of therapy with this agent. Different mechanisms have been proposed to explain this clinical resistance. The decrease in RA plasma concentrations, as a result of enhanced activity of P450,21,22 as well as up-regulation of the CRABP20 and MDR22 gene products, could be responsible for the decrease in RA sensitivity observed in some resistant APL patients.
However, several groups have identified specific genetic lesions associated with RA resistance, both in cell lines and in patients. Several missense mutations in the LBD of the RARα moiety of the fusion protein PML/RARα have now been reported, as shown in Figure 1. The mutation that we found in the NB4-R4 resistant cell line, L398P, abrogates the binding of the fusion protein PML/RARα to its ligand and blocks the transcription of RA-responsive genes in a dominant negative manner.31 In these cells, we found that RA could not release the corepressor SMRT from the mutant PML/RAR (m4), even with suprapharmacological concentrations,13 suggesting that the phenotypic RA resistance may couple directly to the inability to dissociate the corepressor complex and activate retinoid target genes. Here, we report that the fusion protein is able to interact with the coactivator ACTR only in the presence of the ligand, whereas the mutant PML/RAR (m4) is unable to recruit the coactivator, even at the highest tested concentrations of RA (Figure 6). This is consistent with the total inhibition of transcriptional activity by PML/RARα (m4) on different RARE reporters (Figure 4).
Recently, 2 independent groups identified the presence of the first missense mutations in the LBD of the RARα moiety of thePML/RARα chimeric gene in 5 RA-resistant APL patients who had received prolonged or intermittent administration of RA before relapse.37 38 In this study, we found that thesePML/RARα mutations caused a variety of alterations in the known functions of the RARα LBD.
The L290V mutation is located in the β-turn between H5 and H6, and nearby residues (F286, S287) in this β-turn are also involved in the binding pocket for RA.45 Although this amino acid change from leucine to valine is the most conservative substitution that we analyzed, the mutated PML/RARα fusion protein dramatically lost its RA-binding capacity (Figure 2) and exhibited no change in the pattern of resistant fragments in limited proteolytic digestion in the presence of RA (Figure 3). Consistent with these results, the L290V mutation in PML/RARα protein completely impaired the release of the corepressor SMRT and abolished the ability of the mutant protein to recruit the coactivator ACTR, even at high doses of RA (Figures 5 and 6). These ligand-binding and protein-interaction studies are consistent with the transient transfection analyses, which show that of the tested patient mutations, this is the least responsive to transcriptional activation by RA (Figure 4). We propose that amino acid L290, in the β-turn between H5 and H6, is probably directly implicated in the formation of the RA binding pocket, and so even a conservative mutation of this amino acid could disrupt the binding of the ligand. This L290V mutation of PML/RARα identified in a RA-resistant patient is the most similar, phenotypically, to the L398P mutation observed in NB4-R4 APL resistant cells.
In contrast, other mutations observed in cells from resistant patients had quite varying effects on RARα LBD functions. The mutation of the amino acid 272, located in H5, changed a positively charged arginine to a polar uncharged glutamine. This arginine is one of the 24 amino acids directly implicated in the formation of the ligand binding pocket, specifically by making van der Waals contact with the carbon molecule of the acyl chain of RA.45 The replacement of this arginine at position 272 by a glutamine considerably decreased the capacity of the fusion protein PML/RARα to bind RA (Figure 2). In accord with our results, the site-directed mutagenesis of R272 of the nonrearranged RARα has been shown to impair the binding of RA.49 The R272Q mutant also exhibited an impaired responsiveness to low concentrations of ligand in transient transfection assays (Figure 4). Nevertheless, the R272Q mutant PML/RARα was able to activate transcription at a higher RA concentration (10−7 mol/L), although still not as efficiently as did the wild-type fusion protein. These aberrant transcription properties of the R272Q mutant were associated with an impaired ability to release the corepressor SMRT and to recruit the coactivator ACTR: 10 μmol/L RA is not sufficient to release SMRT from the fusion protein, while its association with ACTR does occur at high levels of ligand.
Our results with the mutation R272Q of PML/RARα provide a link between RA resistance in APL and mutations in thyroid receptor beta (TRβ) associated with the syndrome of resistance to thyroid hormone (RTH). RTH is a dominant negative syndrome characterized by reduced tissue responsiveness to thyroid hormones caused by mutations in TRβ that abolish the hormone binding. In a recent study, Privalsky and Yoh50 showed that the V264D mutation of TRβ, located in the omega loop between H1 and H3, exhibits a phenotype very similar to the mutation R272Q in PML/RARα. The V264D TRβ mutant shows impaired hormone binding and corepressor release, but retains the ability to recruit coactivator and activate transcription at high hormone concentrations. Privalsky and Yoh suggested that this substitution may be able to recruit both corepressor and coactivator simultaneously and that the regulatory properties of this receptor may therefore be a combined manifestation of both corepressor and coactivator functions. They further proposed that the V264D mutated protein serves as a bridge to simultaneously tether the corepressor and the coactivator. These data suggest the possibility that the R272Q mutant of PML/RARα might be able to bind simultaneously to both SMRT and ACTR. Multiple sites for coactivator and corepressor interaction have been mapped within the RARα protein, particularly in H5 where the R272Q mutation is located, so it may be possible, under certain circumstances, for SMRT and ACTR to occupy the same receptor molecule. In this case, the predicted result would be a composite transcriptional activity reflecting the counteracting contributions of the corepressor and the coactivator, as in the results we obtained. Additional analyses of these mutations will be necessary to confirm these hypotheses.
An additional case, the substitution of the methionine at position 413 by threonine (M413T), suggests that loss of ligand-inducible coactivator binding does not always accompany loss of corepressor release. This methionine, located in H12 of the LBD is believed to contribute directly to stabilization of the RA binding pocket through the formation of hydrogen bonds or van der Waals contacts with the bound RA molecule.45 Although this substitution is not conservative, our analysis of ligand binding, as well as our limited proteolytic-digestion assay, indicated that this mutation has only a minor effect on the binding of RA for PML/RARα (Figures 2 and 3). This effect on binding may be limited because contact of the H12 of the receptor with RA occurs only after the ligand-induced conformational flip of the H12 over the binding pocket. This is consistent with studies showing that ligand is still able to bind the RARα receptor in presence of mutations in this particular region of the molecule, even though the mutations cause constitutive repression of gene expression.45,51 Rather, the major dysfunction of this mutation may be due to its central location in the AF-2 activation domain, which mediates essential interactions with coregulators of transcription.45,46,52,53 With this M413T mutation, ligand binding does not induce dissociation of the corepressor, whereas the ligand dependence of coactivator recruitment is minimally altered. As with the R272Q mutation, even in the continued presence of significant corepressor binding, the association with the coactivator correlated with the considerable transcriptional activity (Figure 4). These data suggest that an intact AF-2 domain is required for corepressor release, but transactivation in vitro may better correlate with coactivator recruitment than with corepressor release.
We also characterized 2 patient mutations in PML/RARα that exhibit additional alterations associated with RA resistance. R394W substitutes arginine for tryptophan in a region of H11 contributing to stabilization of the RA binding pocket.45 Surprisingly, our analysis of ligand binding showed that this nonconservative substitution did not impair the RA binding to the fusion molecule (Figure 2). However, our analysis of limited trypsin digestion of R394W suggested that the conformation of the mutated PML/RARα after RA treatment is different from that of the wild-type fusion protein (Figure 3). This may explain the impairment of the ligand-dependent release of SMRT and the recruitment of ACTR by the mutated protein (Figures 5 and 6), since the final configuration of the H12 of the holo-receptor determines the association of the coregulators.45,46,52,53
Finally, we analyzed the substitution of the methionine at position 297 for a leucine (M297L), within H6, which presented almost the same phenotype as that of the wild-type chimeric protein. These results suggest that the methionine at 297 does not play a major role in the ligand binding and in the interaction with transcriptional coregulators. The nature of the conservative substitution may explain the very minor effect of this mutation on the tested functional properties of the fusion protein PML/RARα. Alternatively, the RA resistance of this patient may be due to other mechanisms that our in vitro assays of LBD function did not detect.
The relationship of different mutations to the severity of the clinical phenotype of RA resistance in APL patients is difficult to establish, in part because it was not possible to define differences in the degree of clinical resistance among patients. A given mutation of the PML/RARα may also have different phenotypic consequences in different leukemic clones. The complexity of characterizing the role of mutations in RA resistance is also due to the location of these genetic lesions in regions of the receptor that play multiple roles, including ligand binding, receptor dimerization, and interaction with the transcriptional machinery. Indeed, the clustering of mutations within these “hot spot” regions in the RA resistance disorder highlights their functional importance.
The comparison of RA-resistant APL with the RTH syndrome may help us understand the functional roles of these mutations. More than 70 different natural TRβ mutations have been identified in the RTH syndrome. Rather than being randomly distributed, the mutations cluster mainly in 3 areas, denoted by I, II, and III in Figure 1; these correspond to the amino-terminus, the central region, and the carboxy-terminus of the LBD, respectively.54-56 These mutations in TRβ LBD inactivate the ligand binding of the receptor, but retain the receptor-dimerization and DNA-binding functions and act as dominant negative inhibitors on the wild-type receptor. More importantly, a comparison of all PML/RARα mutations identified in APL RA-resistant patients and cell lines highlights the clusters of mutations identified as hot spots in the RTH syndrome, as shown in Figure 1.
Since the discovery of these mutations, new mutations have been found in the above hot spots of the LBD of the fusion protein PML/RARα in additional RA-resistant APL relapsed patients.39 40 These mutations are located between H1 and H3, within or between H5 and H6, and within H11 and H12. The growing list of new mutations identified in the LBD of the fusion protein is an indication of the importance of this mechanism for the development of RA resistance in patients with APL. The findings of naturally occurring point mutations in PML/RARα of RA-resistant relapsed APL patients confirmed the results obtained in the cellular models, indicating that stable genetic alterations in APL cells could mediate RA resistance.
It is now clear that the acquisition of mutations in PML/RARα plays a critical role for the development of RA resistance in patients with APL. In this report, we demonstrated how mutations of PML/RARα could impair the functions of the RARα/E-domain at a molecular level. We showed that specific mutations of the LBD of PML/RARα led to altered interactions with transcriptional coregulators that may be directly involved in the molecular mechanism of RA resistance. We previously reported that retinoid resistance of the NB4-R4 subclone was associated with transcriptional repression by increased association of the mutated PML/RARα with histone deacetylase (HDAC). In these cells, pharmacologic inhibition of HDAC function could partially induce RA-mediated transcription and phenotypic differentiation.13 One patient with RA-refractory APL received combined treatment with RA and HDAC inhibitor, leading to a durable, complete remission.57 However, no other such patients have been reported to date, nor have other acute leukemias whose fusion oncoproteins may repress transcription by recruitment of HDACs yet responded to this therapy. The diversity of alterations observed here in patient-derived mutations suggests the hypothesis that specific mutations of PML/RARα may vary in response to manipulation of HDAC activity. Further studies of additional mutations of PML/RARα from RA-resistant patients will provide a clearer picture of how structural features of the PML/RARα protein determine interactions with transcriptional coregulators and modulators of histone acetylation. This molecular understanding may allow novel treatment strategies for retinoid-resistant patients with APL, and possibly other leukemias.
Acknowledgments
We thank Wei Ding for the generation of the pSG5-PML/RARα mutants (L290V, R394W, and M413T); Dr Sylvie Mader for kindly providing the DR5-tk-CAT and TREpal-tk-CAT response elements; Drs Anne Reutens and Richard Pestell for providing the DR5-tk-LUC reporter; Dr Ronald M. Evans for his generous gift of the GST fusions of the receptor interaction domain of SMRT and ACTR (GST-SMRT-IDII and GST-ACTR-ID); and Michael Sparks for his assistance with Figure 1B.
Supported by grants from the Medical Research Council of Canada, Public Health Service Grant No. CA56771, and the Associazione Italiana per la Ricerca sul Cancro. S.C. is supported by fellowships from Fonds de la Recherche en Santé du Québec, Cancer Research Society, and Israel Cancer Research Fund. A.B. is supported by the Fondazione Italiana per la Ricerca sul Cancro. W.H.M. is a scientist of the Medical Research Council of Canada.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Wilson H. Miller Jr, Lady Davis Institute for Medical Research, Sir Mortimer B. Davis Jewish General Hospital, 3755, Chemin de la Côte Ste-Catherine, Montreal, Quebec, Canada H3T 1E2; e-mail:wmiller@ldi.jgh.mcgill.ca.

![Fig. 2. Specific nuclear RA-binding activity in Cos-1 cells transfected with wild-type in comparison with those transfected with mutant PML/RARα fusion proteins. / HPLC RA-binding profiles of wild-type (top panels) and mutant (bottom panels) PML/RARα S-form (A) and L-form (B). Nuclear extracts were incubated with 10 nmol/L [3H]-RA or with [3H]-RA in the presence of 200-fold excess of unlabeled RA. Extracts were subjected to HPLC analysis using a 6 HR 10/30 size exclusion column.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/96/9/10.1182_blood.v96.9.3200/5/m_h82100300002.jpeg?Expires=1767723290&Signature=uA0~SxCEDugvrXZQqkLK8SU37C96XMvulP9nlYYCyMj2vOTj7zMv7J8w8RDMWbZ2BsyJzSDUKH4PDeRdYc8deijabNEk4wT9K4qwtVNrc0-mkzIKy4kmBQzihFR8nNkQsxfIduNnwkLD2HoGA2urCurZIlWsfqERehIVxPoEm14ZgklmysNK2Cpecd1NQkMNiPDWpcpkfMJe2rCYSaNpzY3zT6XkTjMUxZHwtAJ1IdweiS9jbL4JdsLVof6nUQSn2daVKeqsnXHrEoDcXRVP46Um-gImj~i3SBsnKm4P-iC2jzZubymYY9fVcKONDVoHnr6oGTfpQz1RSIyHEft62w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 3. RA-induced conformational changes in wild-type and mutant PML/RARα fusion proteins. / Limited trypsin digestion analysis of wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro [35S]-methionine synthesized PML/RARα proteins were incubated without (−) or with (+) 1 μmol/L RA, and subsequently treated with increasing trypsin concentrations (0 to 25 μg/mL). Digestion products were analyzed by denaturing electrophoresis. The arrows indicate the intact PML/RARα proteins. Asterisks indicate resistant fragments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/96/9/10.1182_blood.v96.9.3200/5/m_h82100300003.jpeg?Expires=1767723290&Signature=GBE-ETKMN~N10rigbR7U-s3vStETyRLr3-rQ8HdQ2GlIidw3GxDuUuAr0OMCKHAiHPOtsuWEGyuRGCHZ4fws9jVhzyOi-zeMUvljA8SLw-OdErZ0JFeu0T2lLJBgUF534MOVBmD3-g9jOzrAwzM600dDJVT23na0C74CFnFS1AtUXuUH5ABsp2dkVfH9uGdAKxiLXlZ2S644HbQcQvfRyf5liRFoDTbeeyYmb1ANPVMXi2w1vyWMIbn8yn~5Lvr3JrjAPFTOgzRHumUiQD3QqOsVPeB0EQnmFwNKOu~Bc-KPXkGCoKfPqch562qSSMCLv1o5j1gQ-jburqzarQhx7Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Ligand-dependent dissociation of the corepressor SMRT from wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay. / Interaction of SMRT with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-SMRT-IDII in the presence of increasing concentrations of RA. The position of the complex shifted by SMRT is indicated.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/96/9/10.1182_blood.v96.9.3200/5/m_h82100300005.jpeg?Expires=1767723290&Signature=Is7GrDZIA3jUtKK0nJ3TwfkVCkOiV0lVDVoVzyVAq1JnOGsQqzX08jILOMAVIpajpwhs9SMpmOoNqoaEPWXZiFlJA21t1crkSEXhvLjA4s15QuABWdBk9rfSfqPGB9iULhBKr2YIAaP7VC-saT76AnY771TDdThTHsNIvT2TyGBzIKGDTsWEd0kTvuv7O8fYyWM8QKlwCuFQ2Qjm99FRPUZguPJfplSmUyN04WlkdhGl27AXKuhrjuzNXTvOI8MbDbZFuXx0vBhAh6r29c6oAXTd3pKfeY8xGNb6H-J3WGxwHm7LUVsIYSnp8jNwo2dEsIjdG17O-56vT9MvwIpJ2w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 6. Differential recruitment of the coactivator ACTR by wild-type and mutant PML/RARα fusion proteins on a DR5 RARE in gel mobility shift assay. / Interaction of ACTR with wild-type and mutant PML/RARα S-form (A) and L-form (B). In vitro translated PML/RARα fusion proteins were coincubated with the [32P]-labeled DR5 RARE, along with bacterially expressed GST-ACTR-RID in the presence of increasing concentrations of RA. The position of the complex shifted by ACTR indicated.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/96/9/10.1182_blood.v96.9.3200/5/m_h82100300006.jpeg?Expires=1767723290&Signature=XKQ9zEJpdtMY4aR-jLPP53ww5qs9Fs29io6h0~1emhws6AOz7fCqls7trcajx01TyG48AnxRY9oUsPYRSEeP~I4W0U~2kYCNVwFXkqeaeF7sUKRJC2F-Wz19t47IG8Wtb3L4neNxphujGlOl4GTrxClFqFB6x5JZr2fbe6f257LnyukWe-YxwagJ2Cg1fOjmeogzoxwJwSWl1bjocVO436ZQZ~PUmkPjLbb1hy4mC2aBzmhvNELs7Lop~7I24URl~iHOXfJsuqezT-snyl-eyf4HZuudvbPVyL3PNhwfLiYBAdfG2Q0YD7-t~sHibl9qfDHYeFANIWd6gcASjDIiBg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal