Nonmyeloablative host conditioning regimens have been used in clinical allogeneic bone marrow and hematopoietic progenitor transplantation to effectively treat lymphohematopoietic tumors and reduce early toxicity. However, severe graft-versus-host disease (GVHD) remains a major problem. The goal of the current study was to determine whether specific subsets of cells in allogeneic bone marrow transplants can effectively treat the BCL1 B-cell lymphoma in nonmyeloablated BALB/c mouse hosts given a single dose of sublethal (450 cGy) total body irradiation, without inducing severe GVHD. The experimental results show that high doses of whole bone marrow cells from major histocompatiblity complex (MHC)-mismatched donors eliminate both normal and malignant host-type lymphohematopoietic cells without causing injury to nonlymphohematopoietic host tissues. The CD8+T-cell antigen receptor–αβ+(TCRαβ+) T cells within the marrow transplants mediated the killing of the tumor cells via both perforin- and FasL-dependent pathways. Cells present in marrow transplants from either CD8−/− or TCRα−/− donors failed to eliminate malignant and normal host lymphohematopoietic cells. Addition of small numbers of blood mononuclear cells to the marrow inoculum caused lethal GVHD. Thus, the resident allogeneic bone marrow CD8+ TCRαβ+ T cells had the unique capacity to eliminate the host lymphohematopoietic cells without nonlymphohematopoietic tissue injury.
Introduction
Recent advances in clinical allogeneic bone marrow and hematopoietic progenitor transplantation have reduced the toxicity of host-conditioning regimens such that chimerism has been achieved in nonmyeloablated hosts.1-4 Residual tumor cell elimination has been associated with the spontaneous transition from mixed to complete chimerism or with the subsequent infusion of donor blood lymphocytes. A major side effect despite the reduced toxicity regimens is the high incidence of severe graft-versus-host disease (GVHD) even with HLA-matched sibling combinations.1-4 However, mouse models of allogeneic bone marrow transplantation (BMT) in nonmyeloablated hosts conditioned with combinations of sublethal total body irradiation (TBI), thymic irradiation, anti–T-cell monoclonal antibodies (mAbs), and/or chemical cytoreduction show little or no GVHD in major histocompatibility complex (MHC)-mismatched combinations.5-8 The lack of GVHD in the latter models of mixed chimerism is likely explained by the lack of contamination of the BMTs with donor peripheral T cells especially peripheral blood T cells, because only small numbers of the latter cells (∼1 × 104) added to the mouse marrow inoculum induce acute lethal GVHD.9,10 Peripheral blood hematopoietic progenitor transplants mobilized by human bone marrow and granulocyte colony-stimulating factor are highly contaminated with donor blood cells.11-14
Although MHC-mismatched BMT with or without added peripheral T cells can be used to treat lymphomas and leukemias in myeloablated mice,15-18 it is not clear whether this treatment is effective in nonmyeloablated mice with high tumor burdens conditioned with TBI. It is possible that peripheral T cells that induce GVHD are required to eliminate tumor cells in nonmyeloablated hosts. Purified populations of CD8+ T cells from the lymph nodes and spleen effectively kill lymphohematopoietic tumor cells in myeloablated hosts given TBI after addition to T-cell–depleted (TCD) or whole BMTs, but severe GVHD develops as the dose of purified CD8+ T cells increases.16,18 A narrow dose range of purified CD8+ T cells from the bone marrow or spleen has been reported to effectively treat the BCL1 lymphoma/leukemia in myeloablated hosts given purified allogeneic hematopoietic stem cell transplants without subsequent development of the clinical signs of GVHD.19 However, it is not clear whether this dose range of purified CD8+ T cells is effective in treating tumors in nonmyeloablated hosts and whether higher doses may cause GVHD. Recently, a CD8+ non-T cell has been identified in the mouse bone marrow that is able to facilitate the engraftment of hematopoietic stem cells in myeloablated allogeneic hosts without the development of GVHD.20 21 The ability of these CD8+ “facilitator cells” to kill or eliminate tumor cells in vivo has not been determined in either myeloablated or nonmyeloablated hosts.
The object of the current study was to determine whether allogeneic BMT can effectively treat the BCL1 tumor in nonmyeloablated hosts given a single dose of TBI, and to determine the nature of cells in the transplant that can mediate tumor elimination. We used high doses of MHC-mismatched whole bone marrow cells to achieve engraftment in nonmyeloablated hosts because increasing the number of infused hematopoietic stem cells or progenitor cells can overcome engraftment barriers in myeloablated allogeneic hosts.21 Previous studies showed that inclusions of CD8+ T cells and CD8+ non-T cells facilitate the engraftment of these progenitors in these myeloablated hosts.21 The results of the current study show that infusion of the high doses of marrow cells not only engrafted and eliminated residual normal host lymphohematopoietic cells in sublethally irradiated hosts, but also eliminated tumor cells that had been injected 2 weeks earlier. The development of complete chimerism and elimination of tumor cells was mediated by CD8+ T cells in the bone marrow, and the contribution of CD8+ non-T cells was minimal. Although the donor marrow CD8+ T cells eliminated residual normal host normal and malignant lymphohematopoietic cells, microscopic examination of nonlymphohematopoietic tissues including the skin and large intestine showed no evidence of GVHD or obvious tissue injury.
Materials and methods
Animals
Wild-type C57BL/6 (H-2b) male mice, 6 to 8 weeks old, and male BALB/c (H-2d) mice, 8 to 10 weeks old, were purchased from the Department of Comparative Medicine, Stanford University. CD8−/− (C57BL/6J-CD8αtm1Mak), perforin−/− (C57BL/6J-Pfptm1Sdz), T-cell antigen receptor α (TCRα)−/−(C57BL/6J-TCRαtml/Mom), and FasL−/−(B6Smn.C3H-Faslgld) mice were purchased from the Jackson Laboratory (Bar Harbor, ME). CD4−/−(C57BL/6-CD4tm1 N7) mice were purchased from Taconic Farms (Germantown, NY). All gene-deficient mice were male, 8 to 10 weeks old.
BCL1 tumor cell passage and injection
BCL1 is a B-cell leukemia/lymphoma derived from BALB/c mice with an IgMλ surface Ig phenotype.23 This cell line was maintained by serial passage in BALB/c mice as described previously.23 BCL1 cells (1 × 106) from the spleen of BALB/c mice were injected intravenously into normal BALB/c recipients, to allow the lymphoma to grow in the recipients for 13 days before the conditioning treatment.
Sublethal TBI
Recipients injected with BCL1 cells were given a single dose of TBI, 450 cGy. The irradiation was performed with a Philips x-ray unit (200 kV, 10 mA; Philips Electronic Instruments, Rahway, NJ) at a rate of 84 cGy/min with a 0.5-mm Cu filter.
Cell preparation
Femoral and tibial bones taken from donor C57BL/6 mice were rinsed and the residual muscle on the bones were removed. Bone marrow cells were prepared by flushing the bones with phosphate-buffered saline (PBS) (Gibco BRL, Grand Island, NY) with 2% fetal bovine serum, and the cell suspension was filtered through nylon mesh to remove aggregates, washed once before injection. To prepare TCD bone marrow cells, whole C57BL/6 bone marrow cells were incubated with biotinylated anti-Thy1.2 mAb (5a-8; Caltag, Burlingame, CA), and then with streptavidin-conjugated magnetic beads (Miltenyi Biotec, Auburn, CA). Cells were passed through a MACS medi-column (Miltenyi Biotec) twice; the flow through cells contained less than 0.1% TCRαβ+cells as judged by subsequent immunofluorescent staining. The cells retained in the column were harvested and stained with allophyco-cyanin (APC)–anti-TCRαβ, phycoerythrin (PE)–anti-CD4, and fluorescein isothiocyanate (FITC)–anti-CD8 fluorochrome-conjugated mAbs and sorted for CD8+TCRαβ+ and CD4+TCRαβ+ T cells as described in detail previously.10 Peripheral blood mononuclear cells (PBMC) were obtained by applying heparinized blood from the tail to Ficoll-Hypaque gradients as described previously.10
Bone marrow cell infusion
Single bone marrow cell suspensions were injected via the lateral tail vein of recipients 24 hours after irradiation. Cell suspensions for each injection were adjusted to 0.5 mL to minimize variation of infused cell volumes and numbers.
Flow cytometric analysis and sorting
Blood samples for chimerism and BCL1 analysis from transplanted recipients were hemolyzed with ammonium chloride potassium carbonate to remove red cells. The white cell pellets were washed twice with PBS containing 1% fetal bovine serum and 0.05% sodium azide (staining buffer), and incubated on ice for 15 minutes with saturation concentrations of mAbs after incubation with anti-CD16/32 (2.4G2; Pharmingen, San Diego, CA) to block FcR-γII/III receptors as described previously.10 The following conjugated mAbs were used for immunofluorescent staining; biotin–anti-Thy1.2 (5a-8, Caltag), APC–anti-TCRαβ (H57-597, Pharmingen), PE–anti-CD4 (RM4-5, Pharmingen), FITC–anti-CD8 (CT-CD8α, Caltag), APC–anti-B220 (RA3-6B2, Caltag), FITC–anti-BCL1 idiotype (gift from Dr R. Levy, Stanford University), and PE–anti-H-2Kb (CTKb, Caltag). After incubation, cells were washed twice and followed by Texas red-streptavidin (Caltag) staining on ice. After 15 minutes, cells were washed twice, and propidium iodide was added to exclude dead cells. All the samples were analyzed using Vantage and Flojo software (Becton Dickinson, Mountain View, CA). Sorting of stained cells was performed using a Vantage flow cytometer (Becton Dickinson) as described in detail previously.10
Histopathology of skin and intestine
Histopathologic specimens from the skin, liver, kidney, heart, lung, and small and large intestines of hosts were obtained 40 or 100 days after transplantation and fixed in formalin before embedding in paraffin blocks. Tissue sections were stained with hematoxylin and eosin and examined for pathologic changes by light microscopy.
Statistics
Kaplan-Meir survival curves were made using Statview 4.5 software (SAS Institute, Cary, NC), and statistical differences were analyzed using the log-rank (Mantel-Cox) test.
Results
Survival of mice given BCL1 tumor cells and marrow transplants
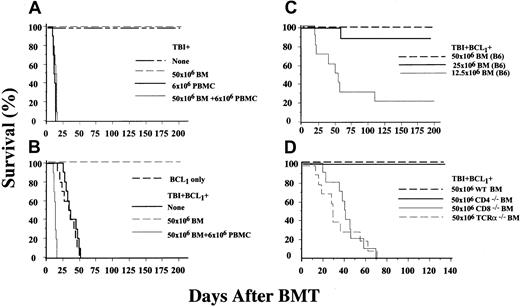
To determine whether the BCL1 B-cell lymphoma of BALB/c origin could be effectively treated by MHC-mismatched (C57BL/6(H-2b) BMT in sublethally irradiated (450 cGy) hosts, control BALB/c (H-2d) mice were given irradiation alone or a single intravenous injection of 50 × 106C57BL/6 marrow cells after irradiation. In both cases, all hosts appeared healthy and survived for at least 200 days (Figure1A). Injection of 6 × 106C57BL/6 PBMC instead of the marrow cells into the irradiated BALB/c hosts resulted in uniform death by 14 days with clinical signs of GVHD including diarrhea, hunched back, and swollen face (Figure 1A). The number of T cells contained within the PBMC was similar to that in the marrow inoculum.10 Addition of the PBMC to the marrow cells resulted in uniform death of the BALB/c hosts by day 16 (Figure1A). Hosts given a single intravenous injection of BCL1tumor cells (1 × 106) and TBI 13 days later all died by day 75 after the tumor cell injection (Figure 1B). Control mice given the tumor cell injection without irradiation all died by day 60, and there was no significant effect of the irradiation on survival as judged by the log-rank test (P > .5).
Survival of sublethally irradiated BALB/c hosts given BCL1tumor cells is markedly improved after wild-type allogeneic BMT.
(A) Survival of control BALB/c mice given irradiation (450 cGy) alone (None) or irradiation and a single intravenous injection of C57BL/6 bone marrow (BM) cells, PBMC, or PBMC and marrow cells. (B) Hosts given an intravenous injection of 0.1 × 106 BCL1tumor cells (BCL1 only) or a single dose of 450 cGy sublethal total body irradiation (TBI) and an injection of tumor cells, 13 days earlier (None). Survival of BALB/c hosts given BCL1tumor cells, sublethal TBI, and bone marrow or PBMC, or PBMC plus marrow cells (BM) cells from C57BL/B6 donors 1 day after TBI is shown in panel B also. (C) Survival of hosts given sublethal TBI, BCL1 cells, and graded numbers of marrow cells from C57BL/6(B6) donors. (D) Survival of BALB/c hosts given BCL1tumor cells, sublethal TBI, and a BMT from wild-type (WT), CD4−/−, CD8−/−, or TCRα−/−C57BL/6 donors. There were 5 or 10 hosts in each group.
Survival of sublethally irradiated BALB/c hosts given BCL1tumor cells is markedly improved after wild-type allogeneic BMT.
(A) Survival of control BALB/c mice given irradiation (450 cGy) alone (None) or irradiation and a single intravenous injection of C57BL/6 bone marrow (BM) cells, PBMC, or PBMC and marrow cells. (B) Hosts given an intravenous injection of 0.1 × 106 BCL1tumor cells (BCL1 only) or a single dose of 450 cGy sublethal total body irradiation (TBI) and an injection of tumor cells, 13 days earlier (None). Survival of BALB/c hosts given BCL1tumor cells, sublethal TBI, and bone marrow or PBMC, or PBMC plus marrow cells (BM) cells from C57BL/B6 donors 1 day after TBI is shown in panel B also. (C) Survival of hosts given sublethal TBI, BCL1 cells, and graded numbers of marrow cells from C57BL/6(B6) donors. (D) Survival of BALB/c hosts given BCL1tumor cells, sublethal TBI, and a BMT from wild-type (WT), CD4−/−, CD8−/−, or TCRα−/−C57BL/6 donors. There were 5 or 10 hosts in each group.
Survival of recipients of the tumor cells was markedly improved by the intravenous injection of 50 × 106 C57BL/6 marrow cells 24 hours after sublethal irradiation, and all survived at least 200 days. When 12.5, 25, or 50 × 106 marrow cells without PBMC were compared, survival was about 25%, 90%, and 100%, respectively, during a 200-day observation period (Figure 1C). Survival of mice given even the lowest dose of marrow cells was significantly increased compared to mice given tumor cells and irradiation without marrow cells (P < .01).
To determine whether the improved survival of irradiated tumor-bearing hosts given MHC-mismatched marrow cells without PBMC was dependent on donor T cells within the marrow transplant, hosts given 50 × 106 marrow cells without PBMC from wild-type C57BL/6 donors were compared to those given the same number of marrow cells from C57BL/6 TCRα−/−donor mice with deficient T-cell development. Whereas all hosts given wild-type cells survived for 140 days, hosts given the cells from TCRα−/− donors all died by day 72 (P < .01) (Figure 1D). Because improved host survival depended on the presence of T cells within the marrow transplants, further studies were performed to determine whether donor CD4+ or CD8+ T cells were responsible for the improved outcome. Accordingly, irradiated tumor-bearing hosts were given 50 × 106 marrow cells from C57BL/6 CD8−/− or CD4−/− donors. Whereas uniform survival was observed for at least 140 days in hosts given the CD4−/− donor cells, all hosts given CD8−/−donor cells died by day 70 (P < .01) (Figure 1D). The results indicate that CD8+αβ+ T cells within the MHC-mismatched BMTs mediate the improved survival of the hosts.
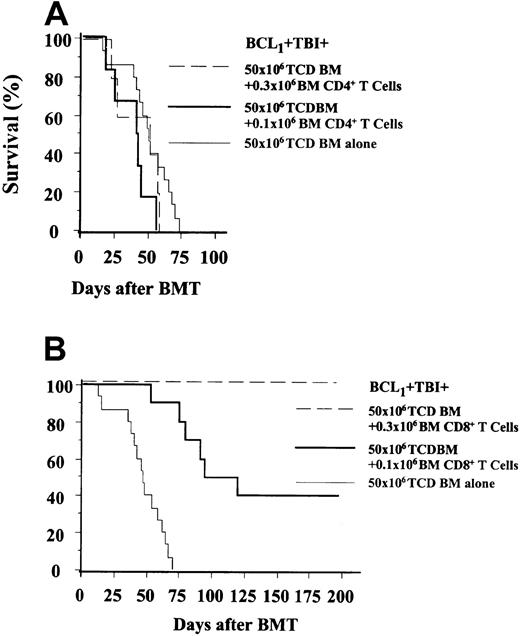
Adoptive transfer of donor marrow CD8+but not CD4+ T cells improves survival of tumor-bearing hosts
In several experiments, BALB/c hosts given BCL1 tumor cells and sublethal irradiation were injected with either 50 × 106 TCD bone marrow cells from C57BL/6 wild-type donors or the latter cells in combination with sorted CD4+or CD8+ T cells from the C57BL/6 bone marrow. Figure2A shows that irradiated tumor-bearing hosts given the TCD marrow cells alone all died by day 74, and survival was not significantly improved compared to hosts given no marrow cells (P > .5; Figure 1B). Addition of either 0.1 or 0.3 × 106 sorted CD4+ T cells from the bone marrow failed to significantly improve survival compared to TCD marrow alone (P > 0.2; (Figure 2A). In contrast, addition of 0.1 × 106 sorted CD8+ T cells from the bone marrow significantly improved survival compared to TCD marrow alone (P < .01; Figure 2B), and addition of 0.3 × 106 sorted CD8+ T cells resulted in uniform survival of hosts for at least 200 days.
Survival of sublethally irradiated BALB/c hosts given BCL1 tumor cells is improved by the inclusion of CD8+TCRαβ+ T cells but not CD4+TCRαβ+ T cells in the BMTs.
(A) Survival of hosts given T (Thy-1+)-cell–depleted (TCD) BMTs alone or combined with sorted BM CD4+TCRαβ+ T cells. (B) Survival of hosts given TCD BMTs alone or combined with sorted BM CD8+TCRαβ+ T cells. There were 5 to 15 hosts in each group.
Survival of sublethally irradiated BALB/c hosts given BCL1 tumor cells is improved by the inclusion of CD8+TCRαβ+ T cells but not CD4+TCRαβ+ T cells in the BMTs.
(A) Survival of hosts given T (Thy-1+)-cell–depleted (TCD) BMTs alone or combined with sorted BM CD4+TCRαβ+ T cells. (B) Survival of hosts given TCD BMTs alone or combined with sorted BM CD8+TCRαβ+ T cells. There were 5 to 15 hosts in each group.
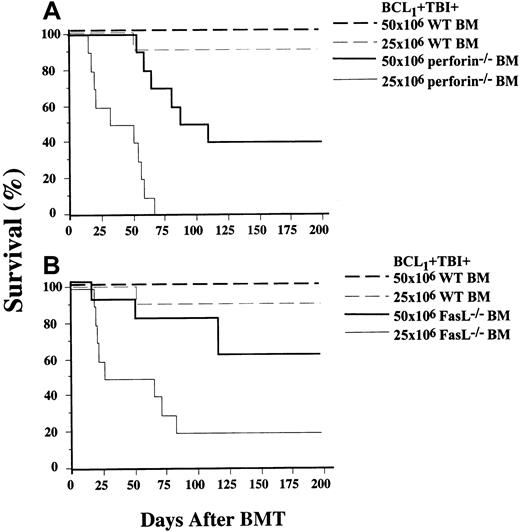
Role of perforin and FasL in improved survival after BMT
Because CD8+ T cells from the marrow of C57BL/6 donors mediated the improved survival of tumor-bearing BALB/c hosts, further experiments were performed to determine the role of perforin and FasL, 2 proteins expressed by CD8+ T cells that have been shown previously to contribute to CD8+ T-cell killing of tumor cells.25 26 Accordingly, irradiated tumor-bearing BALB/c hosts were given BMTs from wild-type, FasL−/−, or perforin−/− C57BL/6 donors. Figure3A shows that at least 90% of hosts given either 25 or 50 × 106 wild-type marrow cells survived for 200 days. In contrast, hosts given 25 × 106marrow cells from perforin−/− donors all died by 65 days, and only 40% given 50 × 106 perforin−/−marrow cells survived 200 days (Figure 3A). Thus, survival with wild-type cells was significantly improved compared to perforin−/− cells at high and low cell doses (P < .01 and .01, respectively). Similar results were observed when wild-type was compared to FasL−/− marrow cells (Figure 3B). Whereas uniform survival for 200 days was found with 50 × 106 wild-type cells, only 60% of hosts survived with 50 × 106 FasL−/− cells (P < .05). When 25 × 106 wild-type and FasL−/− cells were transplanted, 200-day survival was reduced from 90% to 20% (P < .01). Thus, expression of both FasL and perforin contributed to the improved survival mediated by C57BL/6 marrow transplants.
Improved survival of sublethally irradiated BALB/c hosts given BCL1 tumor cells and a BMT is dependent on the expression of
perforin and FasL genes.(A) Survival of hosts given BMTs from wild-type (WT) or perforin−/−C57BL/6 donors. (B) Survival of hosts given BMTs from WT or FasL−/− donors. There were 5 or 10 hosts in each group.
Improved survival of sublethally irradiated BALB/c hosts given BCL1 tumor cells and a BMT is dependent on the expression of
perforin and FasL genes.(A) Survival of hosts given BMTs from wild-type (WT) or perforin−/−C57BL/6 donors. (B) Survival of hosts given BMTs from WT or FasL−/− donors. There were 5 or 10 hosts in each group.
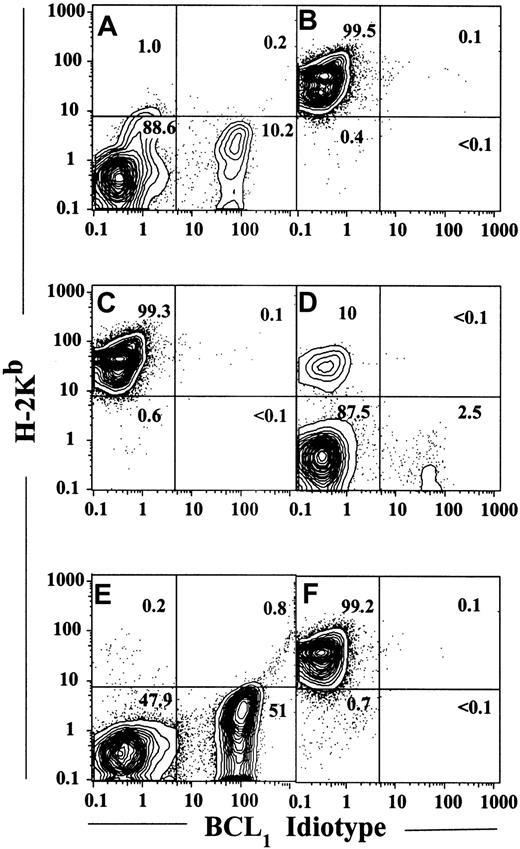
Elimination of BCL1 tumor cells did not occur in mixed chimeras
Irradiated BCL1 tumor-bearing hosts used in the studies described above were examined for the presence of donor-type cells and BCL1 cells in the peripheral blood 20 days after BMT. PBMC from the hosts were stained with fluorochrome-conjugated anti–H-2Kb (donor-type) mAb and anti–BCL1-idiotype mAb (Figure4). Figure 4A shows a representative pattern from a host given BCL1 tumor cells and irradiation without BMT. Approximately 99% of cells did not stain for the donor-type (H-2Kb) marker, and about 10% expressed the BCL1 idiotype (enclosed in lower right box) 20 days after irradiation. In contrast, an irradiated tumor-bearing host given a wild-type C57BL/6 BMT (25 × 106 cells) had more than 99% donor-type and less than 1% host-type cells in the blood, and cells expressing the BCL1 idiotype were not detected on day 20 (Figure 4B). Table 1 shows that all hosts given either 12.5, 25, or 50 × 106 wild-type C57BL/6 marrow cells that were assayed for chimerism had less than 1% host-type (H-2Kb negative) cells at day 20. When the dose of marrow cells was reduced to 6.0 × 106 then irradiated, non-tumor–bearing hosts failed to achieve detectable chimerism, and at least 99% of cells were host type (Table 1). All tested hosts given 50 × 106 marrow cells from CD4−/− donors had less than 1% host-type cells (Table1), and these had no detectable BCL1 tumor cells (Figure4C). Five of 8 hosts given 50 × 106 CD8−/−marrow cells had mixed chimerism with 2% to 98% host-type cells in the blood, and 3 of 8 had complete chimerism with less than 1% (Table1). An example of mixed chimerism in a CD8−/− marrow recipient with 88% host-type, 10% donor-type, and 2.5% BCL1-idiotype–positive cells is shown in Figure4D.
CD8+TCRαβ+ T cells promote complete donor-type chimerism and eliminate BCL1 tumor cells in the peripheral blood 20 days after BMT.
(A) Two-color flow cytometric analysis of H-2Kb versus BCL1-idiotype markers in white blood cells from a control recipient given BCL1 and total body irradiation (TBI, 450 cGy) alone. (B) Analysis of a recipient given BCL1 cells, TBI, and a transplant of 25 × 106 wild-type C57BL/6 whole bone marrow cells. (C) An irradiated tumor-bearing recipient given 50 × 106 CD4−/− bone marrow cells. (D) Recipient given 50 × 106 CD8−/− bone marrow cells. (E) An irradiated tumor-bearing recipient given a transplant of 50 × 106 TCD wild-type bone marrow cells. Add-back of 0.1 × 106 sorted wild-type bone marrow CD8+ T cells to the transplant is shown in panel F. Percentage of cells in each quadrant is shown.
CD8+TCRαβ+ T cells promote complete donor-type chimerism and eliminate BCL1 tumor cells in the peripheral blood 20 days after BMT.
(A) Two-color flow cytometric analysis of H-2Kb versus BCL1-idiotype markers in white blood cells from a control recipient given BCL1 and total body irradiation (TBI, 450 cGy) alone. (B) Analysis of a recipient given BCL1 cells, TBI, and a transplant of 25 × 106 wild-type C57BL/6 whole bone marrow cells. (C) An irradiated tumor-bearing recipient given 50 × 106 CD4−/− bone marrow cells. (D) Recipient given 50 × 106 CD8−/− bone marrow cells. (E) An irradiated tumor-bearing recipient given a transplant of 50 × 106 TCD wild-type bone marrow cells. Add-back of 0.1 × 106 sorted wild-type bone marrow CD8+ T cells to the transplant is shown in panel F. Percentage of cells in each quadrant is shown.
Chimerism 20 d after bone marrow transplantation in peripheral blood of BALB/c hosts given BCL1 tumor
| Cell no. . | C57BL/6 bone marrow donor . | % Host-type cells . | Fraction of hosts with complete chimerism (< 1% host-type cells) . |
|---|---|---|---|
| 6.0 × 106 | Wild-type* | > 99 × 5 | 0/5 |
| 12.5 × 106 | Wild-type | < 1 × 9 | 9/9 |
| 25 × 106 | Wild-type | < 1 × 10 | 10/10 |
| 50 × 106 | Wild-type | < 1 × 5 | 5/5 |
| 50 × 106 | CD4−/− | < 1 × 5 | 5/5 |
| 50 × 106 | CD8−/− | 98, 89, 11, 2, 2, < 1 × 3 | 3/6 |
| 50 × 106 | TCRα−/− | 10, 6, 6, 6, 5, 5, 4, 4, 4, 4 | 0/10 |
| 25 × 106 | Perforin−/− | 98, 94, 4, < 1 × 4 | 4/7 |
| 50 × 106 | Perforin−/− | 6, 4, 4, 2, < 1 × 5 | 5/9 |
| 25 × 106 | FasL−/− | 91, 91, 2, < 1 × 3 | 3/6 |
| 50 × 106 | FasL−/− | 3, 1 × 7 | 7/8 |
| Cell no. . | C57BL/6 bone marrow donor . | % Host-type cells . | Fraction of hosts with complete chimerism (< 1% host-type cells) . |
|---|---|---|---|
| 6.0 × 106 | Wild-type* | > 99 × 5 | 0/5 |
| 12.5 × 106 | Wild-type | < 1 × 9 | 9/9 |
| 25 × 106 | Wild-type | < 1 × 10 | 10/10 |
| 50 × 106 | Wild-type | < 1 × 5 | 5/5 |
| 50 × 106 | CD4−/− | < 1 × 5 | 5/5 |
| 50 × 106 | CD8−/− | 98, 89, 11, 2, 2, < 1 × 3 | 3/6 |
| 50 × 106 | TCRα−/− | 10, 6, 6, 6, 5, 5, 4, 4, 4, 4 | 0/10 |
| 25 × 106 | Perforin−/− | 98, 94, 4, < 1 × 4 | 4/7 |
| 50 × 106 | Perforin−/− | 6, 4, 4, 2, < 1 × 5 | 5/9 |
| 25 × 106 | FasL−/− | 91, 91, 2, < 1 × 3 | 3/6 |
| 50 × 106 | FasL−/− | 3, 1 × 7 | 7/8 |
Recipients without BCL1, tumor cells.
All the hosts given 50 × 106 TCRα−/−marrow cells were mixed chimeras with 4% to 10% host-type cells in the blood at day 20 (Table 1). Thus, the absence of donor T cells in the marrow still allowed for high levels of chimerism, but did not result in eradication of host-type blood cells. This contrasts with the inability to detect host-type cells after transplantation of 50 × 106 wild-type or CD4−/− marrow cells. Whereas the latter recipients all survived at least 200 days, those given TCRα−/− marrow cells all died by 72 days (Figure1D).
Whereas 10 of 10 recipients given 25 × 106 wild-type marrow had no detectable host-type blood cells at day 20, host-type cells (4%-94%) were detected in 3 of 7 recipients given the same number of marrow cells from perforin−/− donors, and in 3 of 6 (2%-91%) given the same number of FasL−/− cells (Table 1). When the dose of perforin−/− cells was increased to 50 × 106, 4 of 9 recipients still had 2% to 6% host-type cells, but only 1 of 8 recipients given FasL−/− cells at that dose had detectable host-type cells.
In conclusion, all hosts given tumor cells shown in Table 1 that were mixed chimeras with at least 2% residual host-type cells in the blood at 20 days died within 75 days after marrow transplantation. All hosts that survived at least 200 days were complete chimeras (≥ 99% donor-type cells) at 20 days. However, in those experimental groups that included mixed chimeras, even some of the complete chimeras without detectable BCL1 cells died by day 75 (CD8−/− group).
Sorted marrow CD8+ T cells facilitate complete chimerism and tumor elimination
Whereas 25 or 50 × 106 wild-type C57BL/6 marrow cells eliminated detectable host-type cells at day 20 in all BALB/c recipients tested, TCD marrow cells at the same doses failed to eliminate residual host-type cells in all recipients (Table2). Some of the latter hosts had few if any donor-type cells in the blood (Figure 4E). Addition of 0.1 or 0.3 × 106 sorted CD8+ T cells from the wild-type marrow to the TCD marrow reduced residual host-type cells to less than 1% in all recipients (Table 2 and Figure 4F). However, it is clear that elimination as judged by flow cytometry at day 20 did not predict long-term survival, because 60% of recipients given TCD marrow and 0.1 × 106 sorted CD8+ T cells died within 125 days after transplantation (Figure 2B). Addition of 0.3 × 106 sorted CD8+ T cells was required to give uniform long-term survival (Figure 2B). In contrast, addition of 0.1 or 0.3 × 106 sorted CD4+ T cells failed to induce complete chimerism in any recipient (Table 2), and failed to improve survival of recipients compared to TCD marrow alone (Figure 2A)
Influence of sorted bone marrow T cells on residual host-type blood cells in BALB/c recipients 20 d after bone marrow transplantation
| Bone marrow cells . | Bone marrow T cells . | % Host-type cells . | Fraction of hosts with complete chimerism (< 1% host-type cells) . |
|---|---|---|---|
| Whole BM (25 × 106) | None | < 1 × 10 | 10/10 |
| Whole BM (50 × 106) | None | < 1 × 5 5/5 | |
| TCD BM (25 × 106) | None | 99, 98, 94, 33, 24, 12, 11, 7, 5 | 0/9 |
| TCD BM (50 × 106) | None | 10, 9, 4, 3, 3, 2, 1 | 0/7 |
| TCD BM (25 × 106) | CD8+ (0.1 × 106) | < 1 × 10 | 10/10 |
| TCD BM (50 × 106) | CD8+ (0.1 × 106) | < 1 × 9 | 9/9 |
| TCD BM (50 × 106) | CD8+ (0.3 × 106) | < 1 × 9 | 9/9 |
| TCD BM (50 × 106) | CD4+ (0.1 × 106) | 33, 31, 30, 6, 2 | 0/5 |
| TCD BM (50 × 106) | CD4+ (0.3 × 106) | 82, 64, 50, 15, 14 | 0/5 |
| Bone marrow cells . | Bone marrow T cells . | % Host-type cells . | Fraction of hosts with complete chimerism (< 1% host-type cells) . |
|---|---|---|---|
| Whole BM (25 × 106) | None | < 1 × 10 | 10/10 |
| Whole BM (50 × 106) | None | < 1 × 5 5/5 | |
| TCD BM (25 × 106) | None | 99, 98, 94, 33, 24, 12, 11, 7, 5 | 0/9 |
| TCD BM (50 × 106) | None | 10, 9, 4, 3, 3, 2, 1 | 0/7 |
| TCD BM (25 × 106) | CD8+ (0.1 × 106) | < 1 × 10 | 10/10 |
| TCD BM (50 × 106) | CD8+ (0.1 × 106) | < 1 × 9 | 9/9 |
| TCD BM (50 × 106) | CD8+ (0.3 × 106) | < 1 × 9 | 9/9 |
| TCD BM (50 × 106) | CD4+ (0.1 × 106) | 33, 31, 30, 6, 2 | 0/5 |
| TCD BM (50 × 106) | CD4+ (0.3 × 106) | 82, 64, 50, 15, 14 | 0/5 |
TCD indicates T-cell depleted; BM, bone marrow.
Lack of injury to nonlymphohematopoietic tissues after BMT
To determine whether irradiated tumor-bearing BALB/c hosts given an injection of 25 × 106 wild-type C57BL/6 bone marrow cells developed microscopic evidence of tissue injury to nonlymphohematopoietic tissues (liver, pancreas, thyroid, small and large intestines, and skin), 6 hosts were euthanized 100 days after BMT, and histologic analysis of the latter tissues was performed. The large intestines and skin are the main targets for GVHD.26 27 Histologic sections were examined for lesions characteristic of the latter disease. At the time of tissue harvest, the blood and spleen were examined also for the presence of residual host-type cells and of cells expressing the BCL1 idiotype. As in the day 20 analysis, all tested hosts given 25 × 106 wild-type marrow cells had no detectable host-type or BCL1 idiotype-expressing cells in the blood or spleen in the day 100 analysis as judged by flow cytometry (data not shown).
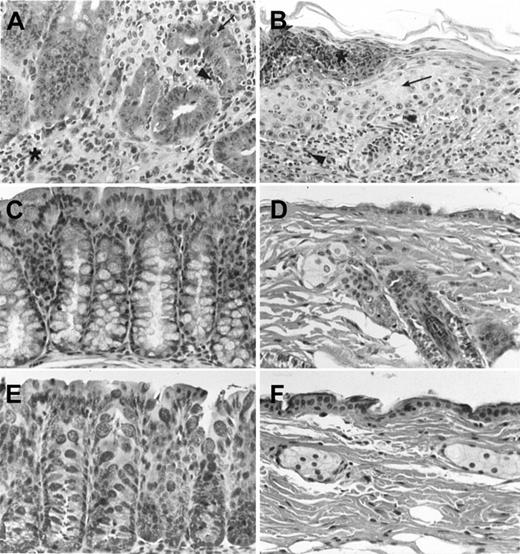
Characteristic lesions of GVHD in the large intestine and skin obtained from positive control BALB/c hosts are shown in Figure 5, panels A and B, respectively. The 6 positive controls were given lethal TBI (800 cGy) and 1.5 × 106 TCD bone marrow and 0.1 × 106 spleen cells from wild-type C57BL/6 donors. Tissues were harvested 40 days after the injection of the C57BL/6 cells because these hosts had severe clinical signs of GVHD and were likely to die shortly thereafter. Figure 5A shows that the intestinal crypts were depleted of plump mucin-containing glandular cells, and a lymphocyte infiltrate was observed surrounding the crypts (asterisk), and extending into the crypt epithelial cells (arrowhead). Apoptotic crypt lining cells where observed also (arrow). Characteristic skin lesions (Figure 5B) included hyperplasia of the epidermis (arrow), lymphocytic dermal infiltrate (arrowhead), and epidermal blistering and necrosis (asterisk). All 6 positive controls showed these characteristic lesions. The same hosts had mild infiltration and fibrosis of the portal triads of the liver, and few if any abnormalities of the small intestines, thyroid, or pancreas (data not shown). Six negative controls were sublethally irradiated tumor-bearing BALB/c hosts given 50 × 106 TCD C57BL/6 marrow cells, and euthanized 40 days after BMT. Figure 5C shows a representative section of the large intestine from the latter group; crypts were lined with mucin-containing glandular cells, and little or no lymphocyte infiltration was observed. The skin showed an epidermal layer 1 to 2 cells thick, and no dermal infiltrate (Figure 5D). The thyroid, pancreas, small intestines, and liver were normal (data not shown).
Tissue sections of the large intestine and skin of BALB/c hosts given BMTs from C57BL/6 donors show no evidence of GVHD.
Sections are stained with hematoxylin and eosin, and magnified × 400. (A) A representative section of the large intestine from a positive control BALB/c host given lethal TBI (800 cGy) and an intravenous injection of 1.5 × 106 TCD bone marrow and 0.1 × 106 spleen cells 40 days earlier. Asterisk shows interstitial lymphocytic infiltrate, and arrowhead shows extension into crypt. Arrow shows apoptotic crypt cell. (B) A representative section of skin from the host in panel A. Arrow shows epidermal hyperplasia, arrowhead shows dermal infiltrate, and asterisk shows epidermal blister. Panels C and D show large intestine and skin, respectively, from a negative control BALB/c host given BCLl tumor cells, sublethal irradiation, and an intravenous injection of 50 × 106 TCD BM cells 40 days earlier. Panels E and F show representative sections of the large intestine and skin, respectively, from BALB/c hosts given BCL1 tumor cells, sublethal irradiation, and 25 × 106 whole BM cells 100 days earlier.
Tissue sections of the large intestine and skin of BALB/c hosts given BMTs from C57BL/6 donors show no evidence of GVHD.
Sections are stained with hematoxylin and eosin, and magnified × 400. (A) A representative section of the large intestine from a positive control BALB/c host given lethal TBI (800 cGy) and an intravenous injection of 1.5 × 106 TCD bone marrow and 0.1 × 106 spleen cells 40 days earlier. Asterisk shows interstitial lymphocytic infiltrate, and arrowhead shows extension into crypt. Arrow shows apoptotic crypt cell. (B) A representative section of skin from the host in panel A. Arrow shows epidermal hyperplasia, arrowhead shows dermal infiltrate, and asterisk shows epidermal blister. Panels C and D show large intestine and skin, respectively, from a negative control BALB/c host given BCLl tumor cells, sublethal irradiation, and an intravenous injection of 50 × 106 TCD BM cells 40 days earlier. Panels E and F show representative sections of the large intestine and skin, respectively, from BALB/c hosts given BCL1 tumor cells, sublethal irradiation, and 25 × 106 whole BM cells 100 days earlier.
None of the 6 irradiated tumor-bearing BALB/c hosts given 25 × 106 C57BL/6 marrow cells had clinical signs of GVHD disease during a 100-day observation period, and none had microscopic lesions characteristic of GVHD or any other abnormalities of the large intestine or skin when tissues were harvested at 100 days. Figure 5E shows a representative section of the large intestine from the latter hosts. The crypts were lined with plump mucin-containing glandular cells, and there was no crypt atrophy, apoptosis, or infiltration. Figure 5F shows a representative section of the skin from these experimental hosts. The epidermis was 2 to 3 cells thick, dermal appendages were frequent, and there was no dermal infiltrate or epidermal blistering. Histologic sections from the thyroid, liver, pancreas, and small intestines had no evidence of tissue injury or necrosis (data not shown). Thus, the injection of 25 × 106 wild-type C57BL/6 bone marrow cells was not associated with any microscopic injury of the nonlymphohematopoietic tissues examined in the surviving hosts.
Discussion
The object of the current study was to determine whether BMT can effectively treat the BCL1 B-cell lymphoma, in nonmyeloablated (450 cGy TBI) hosts. Tumor cells were transferred to the hosts 13 days before irradiation to allow for substantial growth to provide a model for the treatment of human B-cell lymphoma with a low toxicity BMT regimen. All hosts given 450 cGy TBI without tumor cells survived at least 200 days, and by day 30 the number of nucleated cells in the spleen and blood returned to normal (data not shown). All hosts given irradiation after the transfer of tumor cells died within 72 days unless MHC-mismatched (C57BL/6) bone marrow cells were injected. A marrow dose-dependent increase in survival was observed thereafter, and injections of 25 × 106 (∼1 × 109 cells/kg) or 50 × 106 (∼2 × 109 cells/kg) marrow cells achieved 85% and 100% survival, respectively, of at least 200 days. These doses are considerably higher than that obtained with conventional harvesting of human marrow from the pelvis of living donors (∼2-3 × 108 cells/kg), but can be achieved by harvesting the bone marrow from the vertebral bodies of cadaver organ donors.28
None of the hosts given even the highest doses of MHC-mismatched marrow cells developed clinical signs of GVHD such as diarrhea, hunched back, and hair loss. This was not surprising, because previous studies showed that injection of MHC-mismatched bone marrow cells, with minimal blood contamination, failed to induce severe GVHD in myeloablated hosts unless at least small numbers of donor blood mononuclear cells were coinjected.10 The addition of 5 × 106 donor blood mononuclear cells to 50 × 106 bone marrow cells transplanted to the nonmyeloablated hosts in the current study resulted in acute lethal GVHD whether or not BCL1 cells were injected. Thus, blood, but not marrow T cells, is able to induce lethal disease in myeloablated and nonmyeloablated hosts.10 The low potency of marrow T cells is related to their unusual balance of T-cell subsets including a high proportion of natural killer (NK1.1+) T cells that suppress GVHD.10
Irradiated tumor-bearing BALB/c hosts given 25 × 106wild-type C57BL/6 marrow cells were examined at 100 days after the marrow infusion for microscopic evidence of GVHD and tissue injury in the thyroid, pancreas, liver, small and large intestines, and skin. None of the hosts studied at this time point showed microscopic changes of GVHD or of injury in any of these tissues. In addition, tumor cells bearing the BCL1 idiotype were not detected in the blood or spleen in any of the hosts at the same point. Despite the lack of microscopic evidence of GVHD, residual host lymphohematopoietic cells were eliminated in the blood or spleen as judged by flow cytometry at day 20 and day 100. The mechanisms by which donor marrow cells selectively eliminate one type of host cell but do not injure another is the subject of continued study. This is a unique feature of donor marrow cells, because donor blood or spleen cells clearly cause injury to nonlymphohematopoietic tissues such as the skin and colon.10,26,27 Previous studies using the nonmyeloablative regimen, total lymphoid irradiation, combined with cyclophosphamide, showed that transplantation of large numbers of C57BL/6 marrow cells could effectively treat the BCL1 tumor in BALB/c × C57BL/6 F1 hosts without GVHD.29 A subsequent study using the same model system indicated that marrow CD8 cells were required for tumor eradication, because antitumor activity was lost after ex vivo depletion of CD8 but not CD4 cells.30
Although BALB/c hosts in the current study survived at least 100 days without evidence of BCL1 idiotype-positive tumor cells in the blood or spleen, it is possible that small numbers of “dormant” tumor cells were present in the hosts below the limits of detection of flow cytometry. Previous studies of the BCL1tumor have shown that “dormant” tumor cells can be present in healthy transplant hosts even months after tumor innoculation.31,32 The latter cells can be detected by injecting spleen cells from the hosts into normal BALB/c mice, and observing tumor outgrowth over a period of at least 3 months.31,32 Assays for “dormant” tumor cells were not performed in the current study, but we found a correlation between the detection of at least 2% idiotype-positive tumor cells by flow cytometry in the blood of healthy hosts described in our previous study18 and the outgrowth of tumor in adoptive hosts (data not shown).
The BMT protocol described herein may provide a model for MHC-haplotype–matched or MHC-mismatched nonmyeloablated human transplant recipients such that tumor elimination can be achieved without severe GVHD as long as resident bone marrow T cells but not blood T cells are contained in the transplant. This may require techniques for separating the 2 sources of T cells based on surface markers or other characteristics. Unique phenotypic characteristics of human bone marrow T cells from cadaver vertebral bodies that differ from blood T cells have been reported previously.33
To determine the subsets of donor cells within the BMTs in the current study that were responsible for elimination of normal and malignant host-type lymphohematopoietic cells, marrow cells from wild-type C57BL/6 donors were compared to those from C57BL/6 TCRα−/−, CD4−/−, and CD8−/−donors. The hosts given TCRα−/− marrow cells all died by day 72, and neither normal nor malignant host-type cells were eliminated by day 20. Thus, donor marrow T cells played a necessary role in the elimination of host-type cells. The “facilitator cells” of allogeneic stem cell engraftment that have been reported to be CD8+ non-T cells20,21 appear to be unable to mediate elimination of normal and malignant host-type cells in this nonmyeloablative model despite their capacity to facilitate engraftment. A recent study showed the latter “facilitator cells” express a unique heterodimer containing the TCRβ chain covalently linked to a newly described 33-kd protein, and do not express the TCRα chain.34 Thus, “facilitator cells” expected to be present in the marrow of TCRα−/− donors do not appear to function in the current model. Further evidence that CD8+ T cells in the donor marrow mediate host lymphohematopoietic cell elimination after sublethal irradiation was shown by the long-term survival of tumor-bearing hosts given TCD (Thy-1+) marrow transplants in combination with sorted CD8+ TCRαβ+ T cells from the bone marrow. Hosts given the TCD marrow transplants alone all died by day 75. The depleted transplants are likely to be depleted of T cells as well as “facilitator” CD8+ non-T cells, because the latter cells express the Thy-1 marker also.21
The uniform death of tumor-bearing hosts given CD8−/− BMTs and uniform survival of hosts given CD4−/− BMTs was consistent with the critical role of CD8+ T cells in this model. As expected, genetic deficiencies in the expression of FasL and perforin by C57BL/6 marrow donors resulted in impaired elimination of normal and malignant host-type cells, because these 2 molecules have been shown previously to play a critical role in the cytolytic activity of CD8+ T cells via 2 different pathways of target cell destruction.23 24
The dominant role of marrow CD8+ T cells in the current study using nonmyeloablated hosts is consistent with a recent report showing that marrow CD8+ T cells effectively eliminate BCL1 tumor cells in lethally irradiated hosts using the perforin and FasL pathways without GVHD.19 However, neither the contribution of “facilitator cells,” nor the feasibility of elimination of high levels of residual normal and malignant lymphohematopoietic host-type cells present in sublethally irradiated hosts, nor the presence of microscopic injury of nonlymphohematopoietic tissues was studied.19 In particular, host-type normal B cells were eliminated by the lethal irradiation conditioning regimen.19 Previous murine studies have shown that donor CD8+ T cells from tissue sources outside the marrow (lymph node and spleen) are capable of eliminating lymphohematopoietic tumors and facilitating stem cell engraftment in myeloablated hosts, but lethal GVHD was observed as the dose of purified CD8+ T cells was increased to achieve uniform tumor elimination.16,18 Although donor blood lymphocyte infusions depleted of CD8+ T cells in humans have been shown to induce remissions after tumor relapse in BMT recipients, the nature of the donor cell that effectively kills the host-type tumor is not clear.35 CD4+ T cells in these infusions may be able to help donor CD8+ T cells in the host to eliminate tumor cells. In addition, CD4+ T cells may arrest the growth of some types of leukemia.36
In conclusion, the current study shows that CD8+ T cells in the donor bone marrow have a unique ability to eliminate normal and malignant host lymphohematopoietic cells without causing GVHD or injury to nonlymphohematopoietic tissues in nonmyeloablated hosts.
We thank Aditi Mukhopadhyay for technical assistance and Mary Hansen for preparation of the manuscript.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Samuel Strober, Division of Immunology and Rheumatology Department of Medicine, CCSR Bldg, 2215-C, Stanford Medical Center, 300 Pasteur Dr, Stanford, CA 94305-5166; e-mail:sstrober@stanford.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal