The ATM gene has been found to be mutated or deleted in the majority of cases of T cell prolymphocytic leukemia (T-PLL),1-5 and missense mutations were shown to cluster in the highly conserved gene region encoding the ATM kinase domain.1 Recently, Vanasse et al reported that as many as half of the individuals without ataxia-telangiectasia (A-T) who develop sporadic T-PLL are heterozygous carriers of mutations in theATM gene.6 In a response, Stoppa-Lyonnet et al argued that there was no evidence in the literature for this assertion and provided a valuable set of data supporting a somatic origin ofATM mutations in this sporadic leukemia.5Because nontumor DNA in T-PLL cases was largely unavailable in previous studies, it is unknown to what extent, if any, A-T heterozygosity is associated with a detectable risk of sporadic T-PLL. In addition, the majority of identified ATM mutations in T-PLL were different from those observed in A-T families.1 2
If the ATM mutation in sporadic T-PLL is identical to a previously detected A-T patient allele, haplotype analysis of tumor DNA may be a useful way, in the absence of germline material, to distinguish between a somatic and germline origin of the mutation. Evidence of the same ancestral chromosome shared by a T-PLL and an A-T family would support a germline alteration, whereas an identical mutation in a different haplotype background argues for a recurrent mutation. Our previous analysis of 37 cases with T-PLL, largely from the United Kingdom, identified 3 tumors carrying the same mutations as previously found in the germline of A-T patients.1 Single strand polymorphism (SSCP) analysis and nucleotide sequencing identified only a single mutation in each of the 3 tumors and failed to detect the presence of a normal allele.1 The first tumor (1d5) carried a 9 base pair (bp) deletion (7636del9), the most common A-T allele reported so far, found in 15 apparently unrelated families.7-13 The second tumor (1c10) carried a 7271T>G transversion (V2424G), previously identified only in the British Isles,8 while the third tumor (BJ01) carried a nonsense transition 9139C>T (R3047X) found in different populations.8,9 14-16
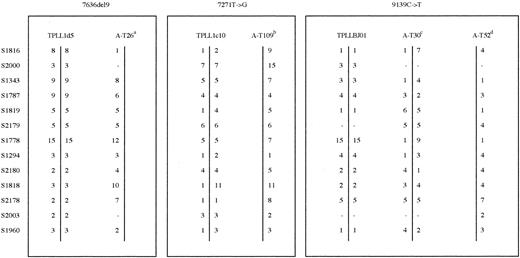
The ATM mutations have been confirmed in all 3 tumors independently. A series of highly polymorphic markers at and flanking the ATM gene and covering a physical distance of about 5.4 megabase (Mb) was used for the haplotype analysis of these T-PLLs together with control DNA from A-T patients carrying the sameATM mutation (Figure 1). Tumor samples 1d5 and BJ01 were shown to be homozygous/hemizygous for markers in the region of ATM. This is consistent with loss of heterozygosity across the ATM region and identification of only a single ATM mutation in each case.1 T-PLL 1c10 also showed homozygosity for most markers although some appeared to be heterozygous. Haplotypes were not the same, however, between the tumor sample and the A-T patient for each of these mutations (Figure 1).
Haplotype analysis of T-PLL tumors and A-T patients carrying the sameATM mutation.
aHaplotype associated with mutation 7636del9 in 8 United Kingdom families. bHaplotype associated with mutation 7271T>G in 3 United Kingdom families. cNot known which haplotype is associated with 9139C>T mutation in this family.dHaplotype associated with mutation 9139C>T in this family.
Haplotype analysis of T-PLL tumors and A-T patients carrying the sameATM mutation.
aHaplotype associated with mutation 7636del9 in 8 United Kingdom families. bHaplotype associated with mutation 7271T>G in 3 United Kingdom families. cNot known which haplotype is associated with 9139C>T mutation in this family.dHaplotype associated with mutation 9139C>T in this family.
In sample 1d5, the allele 5 at D11S2179 (within theATM gene between exons 62 and 63) was identical to that found on the haplotype invariably carrying the 7636del9 mutation in 13 A-T patients in 8 families.8 But this is the most common allele for D11S2179 (36% in normal chromosomes not carrying an ATM mutation in the United Kingdom population), and in the majority of the remaining marker loci, the observed alleles differed. Although tumor 1c10 had allele 6 at D11S2179identical to 6 A-T patients in 3 families with the same 7271T>G mutation, this was the second most common allele for this locus in United Kingdom families (26%). But alleles at and distal toD11S1778 and at and proximal of the D11S1819locus were different in T-PLL DNA compared with the founder haplotype in the A-T patients carrying the 7271T>G mutation. Finally, tumor BJ01, which was found to contain a truncating mutation 9139C>T,1 also showed a haplotype distinct from the 2 different haplotypes observed in 2 A-T families carrying the same 9139C>T mutation (Figure 1).
Although a marker locus mutation can explain occasional variant alleles in short tandem repeats (in particular in those differing by a single repeat unit), this mechanism is unlikely to explain the multiple allelic diversity observed between the A-T haplotypes and haplotypes of T-PLL tumors. In A-T patients founder haplotypes are conserved over the same range of markers as used here to analyze sporadic T-PLL tumors.8 It is unlikely, therefore, that the distance over which the markers are spread will allow changes from germline resulting in such allelic diversity. We conclude that the haplotypes in the region analyzed around the ATM locus are not the same as those carrying the same mutation in the germline. Therefore, our results are not consistent with the germline origin of reported changes in T-PLL tumors, although they ultimately cannot exclude it. In their response to the letter of Stoppa-Lyonnet et al,5 Vanasse and colleagues17 argue that the recurrence ofATM mutations previously found in T-PLL1 2 does not fit well with their strictly somatic origin. Our present data illustrate that recurrent mutations in tumor DNA are compatible with their somatic origin. At present, we believe that there are no data to support a tacit acceptance of the hypothesis of the germline origin ofATM mutations in sporadic T-PLL. This, of course, can now be tested prospectively using matched normal and tumor DNA from a larger number of T-PLL cases with ATM mutations.
We thank the Leukaemia Research Fund, the Cancer Research Campaign, the European Community (QLRT 1999-786), and the Kay Kendall Leukaemia Fund for continued support and Tina Bedenham for technical assistance.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal