Abstract
Treatment of patients with adult T-cell leukemia–lymphoma (ATLL) using conventional chemotherapy has limited benefit because human T-cell leukemia virus type 1 (HTLV-1) cells are resistant to most apoptosis-inducing agents. The recent report that arsenic trioxide induces apoptosis in HTLV-1–transformed cells prompted investigation of the mechanism of action of this drug in HTLV-1 and HTLV-2 interleukin-2–independent T cells and in HTLV-1–immortalized cells or in ex vivo ATLL samples. Fluorescence-activated cell sorter analysis, fluorescence microscopy, and measures of mitochondrial membrane potential (ΔΨm) demonstrated that arsenic trioxide alone was sufficient to induce programmed cell death in all HTLV-1 and -2 cells tested and in ATLL patient samples. IκB-α phosphorylation strongly decreased, and NF-κB translocation to the nucleus was abrogated. Expression of the antiapoptotic protein Bcl-XL, whose promoter is NF-κB dependent, was down-regulated. The collapse of ΔΨm and the release of cytochrome c to the cytosol resulted in the activation of caspase-3, as demonstrated by the cleavage of PARP. A specific caspase-3 inhibitor (Ac-DEVD-CHO) could reverse this phenotype. The antiapoptotic factor Bcl-2 was then cleaved, converting it to a Bax-like death effector. These results demonstrated that arsenic trioxide induces apoptosis in HTLV-1– and -2–infected cells through activation of the caspase pathway.
Introduction
Human T-cell leukemia virus type 1 (HTLV-1) is the etiologic agent of adult T-cell leukemia–lymphoma (ATLL).1 Treatment of patients with ATLL using conventional chemotherapy has limited benefit given that HTLV-1 cells are resistant to most apoptosis-inducing agents.2,3 This may in part be because HTLV-1 leukemic cells overexpress the multidrug resistance protein and the lung-resistance protein, resulting in the pumping of a wide spectrum of agents from the plasma membrane and preventing them from entering the cytoplasm.4,5 In addition, the down-regulation of Fas-ligand expression and rare cases of mutations in the Fas gene sequence have been reported and could also impair the induction of apoptosis through this pathway.6In vivo, but not in vitro, the combination of zidovudine (AZT) with interferon-α is a partially effective treatment that induces cell death in HTLV-1–infected cells.7,8 In vitro, retinoic acid9,10 or arsenic trioxide (As2O3), in combination with IFN-α, can also induce cell death in HTLV-1–transformed cells11,12through mechanisms that remain unclear but that may involve the down-regulation of NF-κB in the latter case.13
Programmed cell death, or apoptosis, consists of a highly regulated series of events allowing the organism to control cell number and tissue size.14 It occurs in 3 phases—initiation, commitment to cell death, and execution. During apoptosis, a complex set of proteins is activated. Among them, caspases play a key role and act as initiators (for review, see 15). These cysteine proteases are normally present as pro-enzymes and are proteolytically cleaved to active heterodimers. They have an active-site cysteine and mediate apoptosis by proteolysis of specific substrates. Substrate specificity is determined by the 4-residue amino-terminal to the cleavage site. Caspase-dependent cleavage can either activate or inactivate the target protein. Close to 100 caspase substrates have been reported.16 Poly (ADP-ribose) polymerase (PARP), a regulator of DNA repair, and Bcl-2 are known substrates of caspase-3. Mitochondria have been recently recognized to play a major role in the control of apoptosis or programmed cell death.14 17 Members of the Bcl-2 family that interact with the permeability transition pore complex regulate permeabilization of mitochondrial membranes, a decisive feature of early cell death.
Bcl-2 is a member of an expanding family of related proteins. Some of them are proapoptotic (Bax, Bak, Bid, Bcl-XS) and some are antiapoptotic (Bcl-2, Bcl-XL) (for review, see14,18). It has been shown that the presence of Bcl-2 blocked the activation of caspase-3. However—and adding another level of complexity—Bcl-2, which inhibits cell death, can also be converted to a Bax-like death effector through its cleavage at Asp-34 by caspase-3.19,20 Interestingly, Bcl-2 and Bcl-XL are overexpressed in HTLV-1 cells.21,22In the latter case, this phenomenon is linked with the constitutive activation of the NF-κB pathway by Tax.23
Tax is a 42-kd protein whose expression is sufficient to induce murine cell transformation or human T cell immortalization.24-26 Tax has pleiotropic effects: not only does Tax transactivate the viral promoter, it is also able to activate or repress the expression or functions of a wide array of genes.27,28 Many of them are regulators of the cell cycle (p21, p53, MAD-1, p16INKA) or of apoptosis (Bcl-2, Bcl-XL, and caspases).2,21,22,28-35 Tax is also competent for inhibiting DNA repair through the suppression of the nucleotide-excision repair and the base excision pathways.36,37 The pro- or antiapoptotic role of Tax is still a matter of debate. Recent data suggest a proapoptotic function for this protein,38 even though it inhibits the caspase cascade.31
Tax-expressing cells have a striking feature—constitutive NF-κB activation.23 This promotes the expression of antiapoptotic factors21 and tumor formation in transgenic mice.39 Interestingly, arsenic treatment inhibits NF-κB activation in different non-HTLV cell lines through interactions with the Iκκβ subunit of the Iκκ complex.40 41Because NF-κB activation has been strongly linked to Tax-induced immortalization, we investigated whether the expression or the function of several apoptosis-regulating proteins, whose expression or function is regulated through the NF-κB pathway, was modified by arsenic trioxide–IFN-α treatment in HTLV-1– and -2–infected cells.
In this report, we demonstrate that arsenic trioxide treatment induced apoptosis in all HTLV-1 and -2 cell lines tested, whether they were interleukin-2 (IL-2) dependent or independent, and in cells obtained from patients with HTLV-1 ATLL. Drug treatment induced the disruption of the mitochondrial ΔΨm and the reversion of NF-κB activation. Apoptosis was correlated with caspase-3 activation and caspase-3–dependent cleavage of PARP and of Bcl-2. Cleavage of Bcl-2 promoted the release of cytochrome c from the mitochondria. Addition of a specific caspase-3 inhibitor prevented arsenic trioxide–induced apoptosis. Finally, Bcl-XL protein, whose promoter is NF-κB dependent, was also down-regulated. These results demonstrated that though multiple apoptosis pathways are inhibited in HTLV-1– and -2–infected cells, these effects were reversible. This may open new avenues for treating patients with HTLV ATLL.
Materials and methods
Drugs
IFN-α (Roche Molecular Biochemicals, Basel, Switzerland) or arsenic trioxide (Sigma, l'Isle d'Abeau, France) was used at 100 units/mL and 1 μM, respectively, as previously described.11 The cell-permeable reversible caspase-3 inhibitor Ac-DEVD-CHO (Bachem, Voisins-le-Bretonneux, France) was dissolved in dimethyl sulfoxide (Sigma) and was used at 50 μM and 100 μM.
Cell lines and ATLL patient cells
HUT-102, MT-2, C8166, and C91/PL are HTLV-1–transformed cell lines, and C19 is an HTLV-2–transformed cell line. CEM, MOLT-4, and Jurkat are leukemic cells not infected by HTLV viruses. All these cells lines were grown in Roswell Park Memorial Institute medium (RPMI-1640; Life Technologies, Gaithersburg, MD) supplemented with 10% fetal calf serum, L-Gln, and penicillin–streptomycin. Boul and Bes (HTLV-1 IL-2–dependent cell lines isolated from a patient with TSP/HAM and a patient with ATLL, respectively)33 and PH878 and PH868 (short-term cultured cells from 2 patients with ATLL) were grown in the same medium supplemented with 20% fetal calf serum and 10% recombinant IL-2 (Roche Molecular Biochemicals). PH868 is a patient with chronic ATLL (WBC showed 2.6 × 109 lymphocytes/L), and PH878 is a patient with acute ATLL (WBC showed 10.7 × 109 lymphocytes/L).
FACS analysis and 4′,6′-diamidino-2-phenylindole dihydrochloride staining
After 48 to 72 hours of treatment, cells were harvested and washed in phosphate-buffered saline (PBS) without Ca++/Mg2+ (Life Technologies). They were then stained using the Vybrant Apoptosis kit (Molecular Probes, Eugene, OR). Briefly, annexin V conjugated to fluorescein allowed the identification of apoptotic cells, whereas propidium iodide (PI) allowed the identification of dead cells. Apoptotic cells were annexin V positive and PI negative. For 4′,6′-diamidino-2-phenylindole dihydrochloride (DAPI) staining experiments, the chambers were coated with poly-L-lysine overnight. Cells were then added to the slide, fixed with 7% paraformaldehyde, washed in PBS without Ca++/Mg2+, and incubated with DAPI (4′-6′-diamine-2 phenylindole dihydrochloride) (Sigma) at 0.1 μg/mL. Cells were then mounted using Vectashield (Vector Laboratories, Burlingame, CA).
Mitochondrial membrane potential (ΔΨm) changes
To investigate the changes in mitochondrial membrane potential that occur during apoptosis, the Apoalert Mitochondrial Membrane Sensor kit (Clontech, Palo Alto, CA) was used. Briefly, after 48 to 72 hours of treatment, cells incubated with Mitosensor reagent for 20 minutes at 37°C. After centrifugation, they were resuspended in incubation buffer and analyzed by fluorescence-activated cell sorter scanner (FACS). Mitochondria containing Mitosensor (normal mitochondria) aggregates were detectable in the PI channel, and Mitosensor monomers (mitochondria with altered membrane permeability) were detectable in the fluorescein isothiocyanate channel.
Cell proliferation and viability assay
To measure cellular proliferation or viability, a cell proliferation–viability kit (XTT; Roche Molecular Biochemicals) was used. In this assay, tetrazolium salt XTT is cleaved to form an orange formazan dye by metabolic active cells. This dye is directly quantified using an enzyme-linked immunosorbent assay reader at 492 nm.
Whole-cell extracts and Western blot analysis
Cells were lysed in TNN buffer (50 mM Tris HCl, pH 7.4, 120 mM NaCl, 5 mM EDTA, 0.5% NP-40, 50 mM NaF, 0.2 mM Na3VO4, 1 mM dithiothreitol) in the presence of protease inhibitors (Complete, Boehringer Mannheim, Germany) for 20 minutes on ice. The lysate was then centrifuged for 10 minutes at 4°C, and the supernatant was frozen at −80°C. Protein concentration was determined by the Bio-Rad protein assay (Bio-Rad, Hercules, CA). Tris-glycine gels (Novex, Groningen, Netherlands)—at 4% to 20%, 10%, or 16%—were used as recommended by the manufacturer. After transfer to an Immobilon polyvinylidene difluoride (PVDF) membrane (Millipore, Bedford, MA), detection was performed with an enhanced chemiluminescence system (Supersignal West Dura; Pierce, Rockford, IL) as previously described.42
Electrophoretic mobility shift assay
Nuclear and cytoplasmic extracts were made as previously described. The 8 mC/EBP oligonucleotide was used as an NF-κB–specific probe, as previously described.43
Mitochondria purification
Cells were washed in PBS without Ca++/Mg2+, the pellet was resuspended in lysis buffer (0.15 mM MgCl2, 10 mM KCl, 10 mM Tris-HCl, pH 7.6, and proteases inhibitors) and kept for 30 minutes on ice. Membranes were then disrupted with a dounce homogenizer, and RLM buffer was added (0.2 mM saccharose, 10 mM Tris-HCl, pH 7.4, ethylene glycol tetraacetic acid (EGTA)–Tris 0.1 mM final). Lysates were centrifuged for 3 minutes, at 900g at 4°C. Supernatants were then centrifuged at 7000g for 10 minutes at 4°C. Pellets were resuspended in RLM buffer and centrifuged again at 7000g for 10 minutes at 4°C. Finally, the pellet was resuspended in protein extraction buffer (50 mM Tris [pH 8.0], 150 mM NaCl, 1% Nonidet P-40, 0.5% deoxycholate, 0.1% sodium dodecyl sulfate) containing proteases inhibitors. Lysates were cleared by centrifugation in a microcentrifuge at 14 000 rpm for 15 minutes and were used for Western blot analysis, as described above.
Antibodies
Anti–Bcl-2 (sc-509), Bcl-2 ΔC21 (sc-783), Bax (sc-526), anti–caspase-3 (sc-7148), phospho-IκB-α (sc-8404), and β-tubulin (sc-9104) were purchased from Santa Cruz (Santa Cruz Biotechnology, Santa Cruz, CA). Anti-cytochrome c (65971A) and anti-PARP (65196E) were purchased from PharMingen (San Diego, CA). Anti Bcl-XL/XS (06-851) was purchased from Upstate Biotechnology (Lake Placid, NY), and anti p53 DO-1 (Ab-6) was purchased from Oncogene Research (Cambridge, MA). Anti-Tax Tab172 was previously described.44 Anti-gag p24 (9281) was purchased from Cambridge Biotech (Rockville, MD). Anti–rabbit and anti–mouse immunoglobulin G horseradish peroxidase–conjugated antibodies were purchased from Amersham (Amersham Pharmacia, Saclay, France) and were used as recommended by the manufacturer.
Confocal microscopy
Cells were centrifuged (Shandon, Pittsburgh, PA) on Superfrost/Plus glass slides (Menzel-Glaser, Braunschweig, Germany) and fixed with 4% paraformaldehyde. They were then permeabilized (PBS/0.1% Triton), blocked (2% PBS–bovine serum albumin [BSA]), and incubated with anti–cytochrome cantibody (65971A) (PharMingen) for 1 hour at room temperature. Cells were washed in PBS/2% BSA and incubated with anti-rabbit–fluorescein isothiocyanate–conjugated antibodies (Uptima, Montluçon, France) for 1 hour at room temperature. The coverglass was finally washed, mounted with Vectashield (Vector Laboratories), and examined using laser confocal microscope argon-krypton (Leica).
Results
Arsenic trioxide alone or in combination with IFN-α induces apoptosis of HTLV-1– and HTLV-2–immortalized or –transformed cells
Arsenic trioxide (As2O3) and IFN-α were recently demonstrated to induce apoptosis in 2 HTLV-1–transformed cells.11 To investigate the mechanism of action of arsenic trioxide, associated or not associated with IFN-α, we treated with these chemicals a series of HTLV-1–immortalized (IL-2–dependent) cells (Bes, Boul), HTLV-1–transformed (IL-2–independent) cells (C8166, HUT-102, MT-2), HTLV-2–transformed (C19) cells, or noninfected control cells (Jurkat and MOLT-4). After 60-hour treatment, the cells were analyzed by FACS using double staining (DAPI/annexin V). Apoptotic cells were scored as annexin V+/PI− versus dead cells, which were PI+. Figure1A shows a typical FACS result obtained with MT-2 cells. An apoptotic population was detected when As2O3 was added to the cell culture. Similar FACS results were obtained with C8166 HTLV-1–infected cells (data not shown). Control Jurkat and MOLT-4 cells were not affected by As2O3 treatment (data not shown and Figure2). DAPI staining of MT-2 cells (Figure1B) demonstrated the expected nuclear condensation after arsenic trioxide or arsenic trioxide–IFN-α treatment, whereas control treatment or IFN-α alone had no or little effect.
As2O3or IFN-α + As2O3 induced apoptosis in HTLV-1 infected cell lines.
(A) FACS, (B) DAPI staining, or (C) ΔΨm collapse analyses of HTLV-1–infected cells after various treatments. (A) MT-2 cells were treated with buffer control, IFN-α, As2O3, or IFN-α + As2O3 for 60 hours. Cells were then harvested and washed in PBS without Ca++/Mg2+. They were stained using the Vybrant Apoptosis kit. Annexin V conjugated to fluorescein allowed the identification of apoptotic cells, whereas PI allowed the identification of dead cells. Apoptotic cells were annexin V+ and PI−. (B) DAPI staining of MT-2 cells after the same treatments. Magnification × 40. (C) ΔΨm Collapse was measured with the Apoalert Mitochondrial Membrane Sensor kit. Results are representative of at least 2 experiments performed with different HTLV-1–transformed cells.
As2O3or IFN-α + As2O3 induced apoptosis in HTLV-1 infected cell lines.
(A) FACS, (B) DAPI staining, or (C) ΔΨm collapse analyses of HTLV-1–infected cells after various treatments. (A) MT-2 cells were treated with buffer control, IFN-α, As2O3, or IFN-α + As2O3 for 60 hours. Cells were then harvested and washed in PBS without Ca++/Mg2+. They were stained using the Vybrant Apoptosis kit. Annexin V conjugated to fluorescein allowed the identification of apoptotic cells, whereas PI allowed the identification of dead cells. Apoptotic cells were annexin V+ and PI−. (B) DAPI staining of MT-2 cells after the same treatments. Magnification × 40. (C) ΔΨm Collapse was measured with the Apoalert Mitochondrial Membrane Sensor kit. Results are representative of at least 2 experiments performed with different HTLV-1–transformed cells.
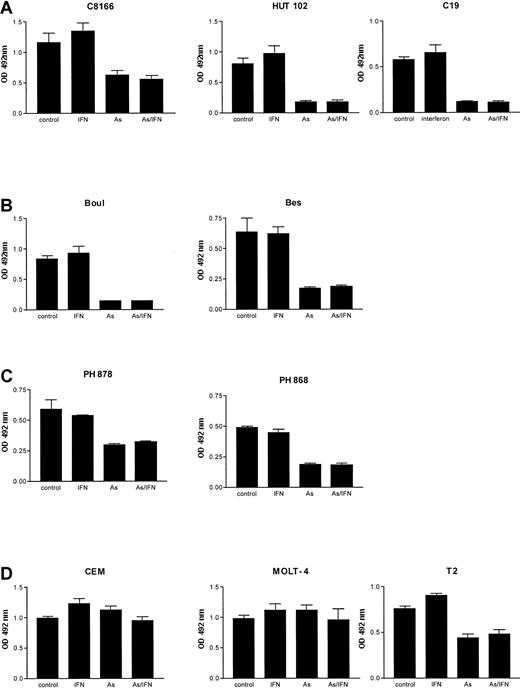
HTLV-1– and HTLV-2–transformed cell lines as well as HTLV-1 cells from patients are sensitive to As2O3.
(A) HTLV-1– or HTLV-2–transformed cells (C8166, HUT-102, C19), (B) HTLV-1 IL-2–dependent cells lines from TSP/HAM or ATL patients (Boul, Bes), (C) ATL cells from patients (PH868 and PH878), and (D) non-HTLV control cell lines (CEM, MOLT-4, T2) were treated with buffer control, IFN-α, As2O3 or IFN-α + As2O3 for 60 hours and then processed using the XTT assay kit. Panels A, B, and D represent the mean of 3 independent experiments performed in duplicate. Panel C represents the mean of 2 independent experiments.
HTLV-1– and HTLV-2–transformed cell lines as well as HTLV-1 cells from patients are sensitive to As2O3.
(A) HTLV-1– or HTLV-2–transformed cells (C8166, HUT-102, C19), (B) HTLV-1 IL-2–dependent cells lines from TSP/HAM or ATL patients (Boul, Bes), (C) ATL cells from patients (PH868 and PH878), and (D) non-HTLV control cell lines (CEM, MOLT-4, T2) were treated with buffer control, IFN-α, As2O3 or IFN-α + As2O3 for 60 hours and then processed using the XTT assay kit. Panels A, B, and D represent the mean of 3 independent experiments performed in duplicate. Panel C represents the mean of 2 independent experiments.
Changes in ΔΨm are a critical step in cells undergoing apoptosis, regardless of the death signal. Therefore, ΔΨm was also measured in MT-2 cells (Figure 1C). Arsenic trioxide or As2O3+ IFN-α–treated cells that entered apoptosis showed an altered mitochondrial membrane permeability that led to ΔΨm collapse. By contrast, MT-2 cells treated with buffer control or with IFN-α did not show any change in ΔΨm (Figure 1C; compare panels 3 and 4 with panels 1 and 2).
To investigate whether all HTLV-1– or HTLV-2–infected cell lines or cells from patients were also sensitive to As2O3 with or without IFN-α, we conducted a series of XTT assays that allowed us to measure cellular proliferation and viability after drug treatment (Figure 2). Confirming the FACS results, HTLV-1–immortalized (IL-2–dependent) cell lines obtained from Boul and Bes patients and HTLV-1–transformed HUT-102, C8166, C91/PL (data not shown), HTLV-2–transformed C19 or short-term cultured cells from 2 patients with ATLL (PH878 and PH868) displayed a significant reduction in cellular proliferation and viability after As2O3 or As2O3 + IFN-α treatment. By contrast, control treatment or IFN-α treatment had no effect (Figure 2A-C). As control cells, CEM, T2, MOLT-4, and Jurkat were tested. CEM, MOLT-4, and Jurkat proliferation was not affected by any treatment. Strikingly, however, As2O3 and As2O3 + IFN-α induced viability and growth alteration in T2 (CEM-derived) cells. This suggested that As2O3 did not specifically induce apoptosis in HTLV-1– or HTLV-2–infected cells but did affect a cellular pathway that might have been altered in HTLV-1 and -2 cells and in the T2 cell line (Figure 2D).
NF-κB activity down-regulated after arsenic trioxide or arsenic trioxide–IFN-α treatment
Because arsenic was reported to inhibit NF-κB activity in various cell lines,40,41 we investigated whether, as suggested by others,13 this was the case in HTLV-1 cell lines. Retardation gels using an NF-κB–specific probe and IκB-α phospho-specific WB confirmed that As2O3, whether used alone (data not shown) or in combination with IFN-α, was able to inhibit the constitutive IκB-α phosphorylation ordinarily present in HTLV-1 cell lines (Figure 3A; compare lanes 2 and 1). This led to a decrease in NF-κB translocation to the nucleus and consequently diminished binding to an NF-κB–specific probe (Figure 3C; compare lanes 2 and 3). In contrast, control treatment (Figure 3A, lane 1) or IFN-α alone (data not shown) did not induce any change. Supershift experiments and competition with a cold probe demonstrated the binding specificity (data not shown).
Inhibition of NF-κB activation by As2O3 in HTLV-1–infected cells.
(A) Sixty micrograms cytoplasmic protein was resolved on 10% to 20% Tris-glycine, transferred to PVDF membranes, and probed with an antibody specific for the phosphorylated form of IκBα. Results are representative of 2 independent experiments. (B) Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin. Results are representative of 2 independent experiments. (C) Electrophoretic mobility shift assay using a previously published NF-κB–specific probe43 mixed with no extract (lane 1), mixed with 5 μg nuclear extract obtained from MT-2 treated with control buffer (lane 2), or treated with As2O3 + IFN-α and run on a 6% DNA retardation gel (lane 3). Specificity of the NF-κB binding was checked by competition with a 50-fold excess of cold probe (data not shown).
Inhibition of NF-κB activation by As2O3 in HTLV-1–infected cells.
(A) Sixty micrograms cytoplasmic protein was resolved on 10% to 20% Tris-glycine, transferred to PVDF membranes, and probed with an antibody specific for the phosphorylated form of IκBα. Results are representative of 2 independent experiments. (B) Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin. Results are representative of 2 independent experiments. (C) Electrophoretic mobility shift assay using a previously published NF-κB–specific probe43 mixed with no extract (lane 1), mixed with 5 μg nuclear extract obtained from MT-2 treated with control buffer (lane 2), or treated with As2O3 + IFN-α and run on a 6% DNA retardation gel (lane 3). Specificity of the NF-κB binding was checked by competition with a 50-fold excess of cold probe (data not shown).
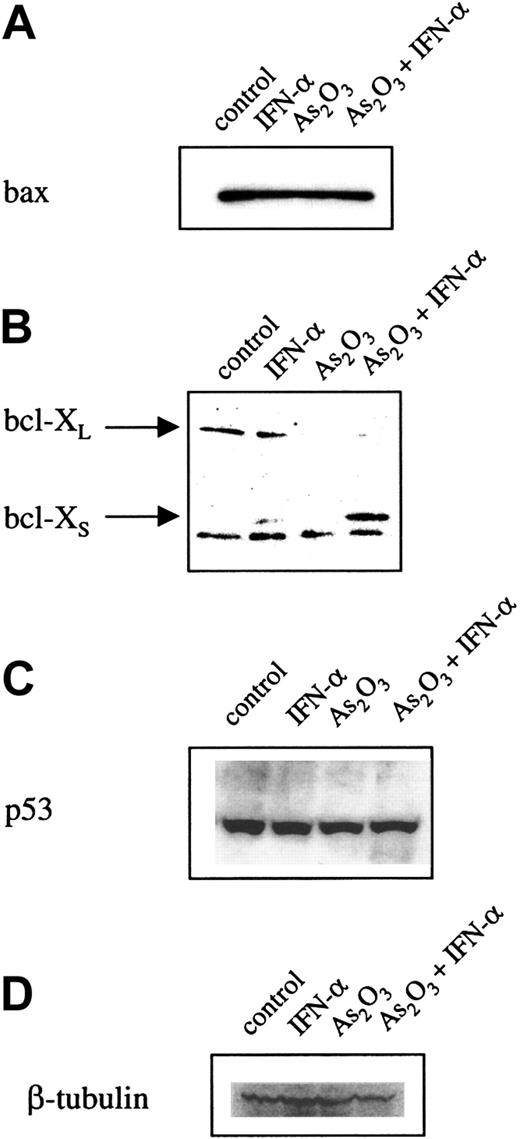
Switch from Bcl-XL to Bcl-XS after As2O3 + IFN-α treatment
NF-κB factors affect the transcription of some Bcl-2 family members such as Bcl-XL.21,22 They also alter p53 transcriptional activity.44,45 Moreover, p53 drives Bax expression. Because we showed that As2O3 affected NF-κB activity, the level of expression of Bax, Bcl-XL, Bcl-XS, and p53 was investigated after drug treatment using whole-cell extracts from C8166 (Figure 4A-C) or from MT-2 and HUT-102 (data not shown). Overall levels of Bax (Figure 4A) and p53 (Figure 4C) remained unchanged, even after the addition of As2O3 + IFN-α. Similar results were obtained for p21 (data not shown). Alternative splicing of theBcl-X gene gives rise to 2 proteins with antagonistic functions: Bcl-XL (antiapoptotic) or Bcl-XS(proapoptotic).46 HTLV-1–infected cells display high levels of Bcl-XL.22 Strikingly, we noted a strong decrease in Bcl-XL expression after As2O3 or As2O3 + IFN-α treatment (Figure 4B). Of note, increased expression of the alternatively spliced, proapoptotic protein Bcl-XS was seen in all the IFN-α–treated C8166 samples. Such an increase in Bcl-XS expression was not observed in the other HTLV-1–cell lines tested, suggesting that this is not a common phenomenon in HTLV-1 cells treated with IFN-α (data not shown). The altered expression levels of Bcl family members might, therefore, have been a factor that influenced the shift toward apoptosis in C8166 cells. β-Tubulin Western blot (Figure 4D) confirmed equal loading of protein extracts.
BclXL/XS expression, but not Bax or p53 expression, is modified by As2O3 in HTLV-1–transformed and –immortalized cell lines.
Sixty micrograms total protein from C8166 cells was resolved on 10% to 20% Tris-glycine, transferred to PVDF membranes, and probed with specific antibodies for (A) Bax, (B) Bcl-XL/XS, (C) and p53. Results are representative of at least 2 independent experiments using different HTLV-1–infected cells. Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin (D). Lane 1, control treatment; lane 2, IFN-α; lane 3, As2O3; lane 4, As2O3 + IFN-α.
BclXL/XS expression, but not Bax or p53 expression, is modified by As2O3 in HTLV-1–transformed and –immortalized cell lines.
Sixty micrograms total protein from C8166 cells was resolved on 10% to 20% Tris-glycine, transferred to PVDF membranes, and probed with specific antibodies for (A) Bax, (B) Bcl-XL/XS, (C) and p53. Results are representative of at least 2 independent experiments using different HTLV-1–infected cells. Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin (D). Lane 1, control treatment; lane 2, IFN-α; lane 3, As2O3; lane 4, As2O3 + IFN-α.
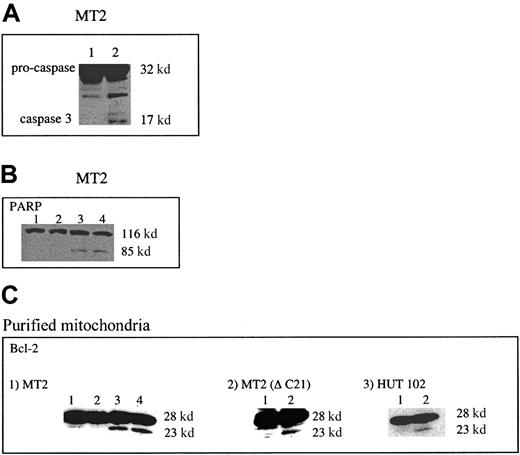
Involvement of caspase-3 in arsenic trioxide–induced apoptosis
ΔΨm Collapse results in the activation of caspases.17 Caspase-3 is a critical downstream protease in the caspase cascade, and PARP is one substrate of the caspase-3 protease activity associated with apoptosis. Interestingly, the activation of caspase-3 was detected after As2O3 (data not shown) or As2O3 + IFN-α treatment, as demonstrated by cleavage of the pro-enzyme (Figure 5A; compare lane 2 [arsenic treated] with lane 1 [control]). This demonstrates that this cysteine protease was activated by the addition of As2O3. We then looked for potential PARP cleavage in As2O3-treated MT-2 cells. Indeed, the 85-kd fragment representing the cleaved form of PARP was detected after treatment of MT-2 HTLV-1 cells by As2O3alone or in combination with IFN-α (Figure 5B; compare lanes 3 and 4 with lanes 1 and 2). This demonstrates the involvement of caspase-3 in this process.
As2O3 induces caspase-3 activation and Bcl-2 cleavage.
Sixty micrograms total proteins from MT-2 cells were resolved on 4% to 20% Tris-glycine gels transferred to PVDF membranes and probed with specific antibodies for (A) caspase-3 and (B) PARP. Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin (data not shown). (C) Sixty micrograms mitochondrial-enriched fraction proteins from MT-2 or HUT-102 cells was resolved on 4% to 20% Tris-glycine transferred to PVDF membranes and probed with specific antibodies for Bcl-2. (A-C) Results are representative of at least 2 independent experiments using different HTLV-1–infected cells (B-C, panel 1). Lane 1, control treatment; lane 2, IFN-α; lane 3, As2O3; lane 4, As2O3 + IFN-α. (A, C, panels 2 and 3) Lane 1, control treatment; lane 2, As2O3+ IFN-α.
As2O3 induces caspase-3 activation and Bcl-2 cleavage.
Sixty micrograms total proteins from MT-2 cells were resolved on 4% to 20% Tris-glycine gels transferred to PVDF membranes and probed with specific antibodies for (A) caspase-3 and (B) PARP. Comparable protein loading was verified using an antibody specific for the housekeeping gene product β-tubulin (data not shown). (C) Sixty micrograms mitochondrial-enriched fraction proteins from MT-2 or HUT-102 cells was resolved on 4% to 20% Tris-glycine transferred to PVDF membranes and probed with specific antibodies for Bcl-2. (A-C) Results are representative of at least 2 independent experiments using different HTLV-1–infected cells (B-C, panel 1). Lane 1, control treatment; lane 2, IFN-α; lane 3, As2O3; lane 4, As2O3 + IFN-α. (A, C, panels 2 and 3) Lane 1, control treatment; lane 2, As2O3+ IFN-α.
Because Bcl-2 is also cleaved by caspase-3 and results in a proapoptotic form,20 we performed MT-2 and HUT-102 subcellular fractionation and mitochondrial enrichment and then Western blot analysis to search for such Bcl-2 posttranslational modification. The proapoptotic, 23-kd Bcl-2 form was detected in As2O3-treated MT-2 cells (Figure 5C; compare lanes 3 and 4 with lanes 1 and 2 in panel 1 and lane 2 with lane 1 in panel 2) and in HUT-102 cells (Figure 5C; compare lane 2 [arsenic trioxide + IFN-α] with lane 1 [control] in panel 3). This confirmed that As2O3-induced apoptosis in HTLV-infected cells was caspase-3 dependent.
Ultimately, HUT-102 cells were also treated with Ac-DEVD-CHO, a specific caspase-3 inhibitor,47 in the presence of As2O3 + IFN-α. As seen on Figure6, incubating HTLV-1–infected cells with DEVD-CHO during As2O3 treatment completely prevented death. Ac-DEVD-CHO treatment of HUT-102 in the absence of As2O3 had no effect on cell growth (data not shown). This result clearly demonstrated the role of the caspase-3 in As2O3-induced apoptosis.
Ac-DEVD-CHO, a caspase-3–specific inhibitor, can prevent As2O3-induced apoptosis.
HUT-102 cells were preincubated with Ac-DEVD-CHO at 100 μM, for 2 hours, then treated with control buffer or with As2O3 + IFN-α for 60 hours in the presence of Ac-DEVD-CHO. XTT assay was then performed, as described in “Materials and methods.” Graph represents the mean of 2 separate experiments performed in triplicate. Lane 1, control treatment; lane 2, As2O3 + IFN-α; lane 3, As2O3 + IFN-α + Ac-DEVD-CHO.
Ac-DEVD-CHO, a caspase-3–specific inhibitor, can prevent As2O3-induced apoptosis.
HUT-102 cells were preincubated with Ac-DEVD-CHO at 100 μM, for 2 hours, then treated with control buffer or with As2O3 + IFN-α for 60 hours in the presence of Ac-DEVD-CHO. XTT assay was then performed, as described in “Materials and methods.” Graph represents the mean of 2 separate experiments performed in triplicate. Lane 1, control treatment; lane 2, As2O3 + IFN-α; lane 3, As2O3 + IFN-α + Ac-DEVD-CHO.
Caspase-3–dependent cleavage of Bcl-2 promotes cytochromec release
Bcl-2 cleavage induced the release of cytochromec from the mitochondria to the cytosol in baby hamster kidney cells.20 We performed a series of confocal microscopy experiments to look for cytochrome c release. Staining of cytochrome c was punctuate and in a mitochondrial distribution around a well-defined nucleus in cells treated with buffer control (Figure 7A) or with IFN-α (data not shown). By contrast, after As2O3 treatment, cytochrome cstaining was no longer clearly defined. (Figure 7B).
Caspase-3–dependent cleavage of Bcl-2 promotes release of cytochrome
c from the mitochondria. HUT-102 cells were treated with (A) control buffer, IFN-α (data not shown), As2O3 (data not shown), or (B) with As2O3 + IFN-α for 60 hours. They were stained with a specific cytochrome c antibody and were analyzed by confocal microscopy. Magnification × 63.
Caspase-3–dependent cleavage of Bcl-2 promotes release of cytochrome
c from the mitochondria. HUT-102 cells were treated with (A) control buffer, IFN-α (data not shown), As2O3 (data not shown), or (B) with As2O3 + IFN-α for 60 hours. They were stained with a specific cytochrome c antibody and were analyzed by confocal microscopy. Magnification × 63.
Discussion
Programmed cell death, or apoptosis, is a genetic program that allows the control of cellular homeostasis. Disruption of apoptosis can contribute to a number of diseases, including cancer.48 It is now well established that anticancer agents induce apoptosis and that disruption of apoptotic programs can reduce treatment sensitivity.49 In vitro and in vivo HTLV-1 cells are resistant to most apoptosis-inducing agents2,3; this might, in part, be because HTLV-1 cells overexpress PgP.4
Inorganic arsenic trioxide (As2O3) was recently reported to induce complete remission in a high proportion of patients with acute promyelocytic leukemia (APL).50,51 In the APL cell line NB4, apoptosis might involve the down-regulation of Bcl-2 expression and the modulation of PML-RARα expression or localization.52-54 However, in other APL cells, the involvement of PML-RARα is a matter of controversy.55Because HTLV-1 causes ATLL, investigators have been prompted to determine whether this chemical is also active in vitro on cell lines infected with HTLV-1.11,12 Indeed, As2O3 in combination with IFN-α kills HTLV-1–transformed cells possibly through Tax down-regulation, leading to NF-κB repression.11,13 23
Caspase cascade is inhibited in HTLV-1–infected cells.31 Here we demonstrate that this inhibition is reversible and participates in arsenic-induced programmed cell death. We show that concomitant with NF-κB inactivation, caspase cascade is reactivated, leading to PARP and to Bcl-2 cleavage and to the release of cytochrome c. Finally, the reversion of As2O3 effects can be achieved by a specific caspase-3 inhibitor, DEVD-CHO. These results are in disagreement with those of El-Sabban et al.13 The DEVD-CHO concentration we used (100 μM vs 50 μM used by El-Sabban et al.13) or the fact that we used DEVD-CHO instead of z-VAD might explain the differences observed.
Bcl-2 cleavage by caspase-3 can also lead to apoptosis.19,20 Indeed, this was the case when HTLV-1 cells were treated with As2O3. Therefore, our results illustrate that though Bcl-2 is postulated to inhibit cell death by acting upstream of caspases, occasionally it might be one of their downstream substrates. Moreover, it has been established that apoptosis can be induced by an elevated number of proapoptotic protein heterodimers.56 Nonetheless, HTLV-1–infected cells have an enhanced ratio of antiapoptotic protein homodimers.22 The possibility that arsenic trioxide treatment modifies such a ratio is an interesting hypothesis that will be examined.
Because p53 is wild type in sequence but functionally inactive in HTLV-infected cells,42,57 one intriguing possibility is that arsenic trioxide treatment causes a reactivation of p53. One might expect that because in our studies the activation of NF-κB by Tax directly correlated with phosphorylation-dependent inhibition of p53 transactivation function44 and that arsenic down-regulated NF-κB translocation, p53 would become functional in HTLV-1 cells by reversing phosphorylation-induced inhibition. Unfortunately, in preliminary studies, we found that arsenic trioxide treatment of control uninfected MOLT-4 cells caused a stress response and subsequent phosphorylation of p53. In fact, in recent reports,58 it is suggested that arsenic induces p53 activity. Although we did not see a change in serine 15 phosphorylation in arsenic trioxide–treated HTLV-1 cells (data not shown), we could not determine whether a shutdown of NF-κB by arsenic relieved p53 transcriptional inhibition by altering p53 phosphorylation status. Detailed analysis is under way to determine the phosphorylation pattern and functionality of p53 in arsenic trioxide–treated HTLV-1 cells. We do note that in examining the level of Bax and p21WAF, 2 well-characterized p53-responsive genes, we did not see an increase in HTLV-infected cells treated with arsenic trioxide. This suggests that perhaps the apoptosis induced by arsenic trioxide, though caspase dependent, was p53 independent.
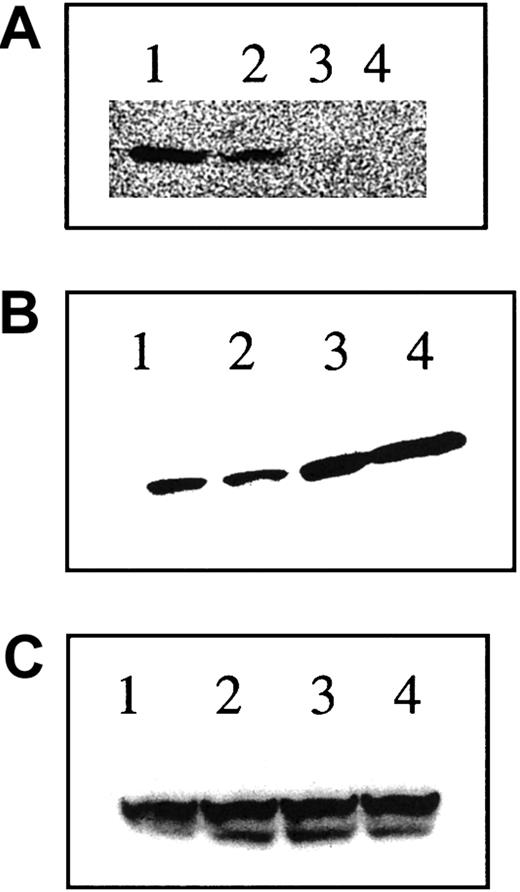
In addition, we think that As2O3-induced NF-κB down-regulation in HTLV-1 cells did not result from Tax down-regulation itself but rather from a direct effect of the chemical component on the Iκκ complex, as reported by other investigators in different cellular systems.40 Therefore, p53 inhibition may still be activated. In fact, conjoined with a Tax decrease, we reproducibly detected by Western blot analysis an increase in p24 gag protein expression after As2O3 treatment (Figure 8A-B). This could indicate that, after stress, there is a shift toward viral production. Indeed, such an effect has been reported in HTLV-1 cells treated with sodium arsenite59 and in HHV-8–infected primary effusion lymphoma cells treated with arsenic trioxide (G. Torelli, written communication, 2000). These results would also explain why the addition of As2O3 is effective on freshly isolated ATLL cells, which show little, if any, Tax expression but do show NF-κB activity.60 This hypothesis is now under study, but it has also been raised by other investigators who treated ATLL cells with all-trans retinoic acid.61 These results also suggest that using As2O3 in vivo to treat HTLV-1– or HTLV-2–infected patients might have pernicious effects. The drug treatment would be anticipated to increase viral production and, therefore, to expand the number of newly infected cells. However, given that in vitro AZT protects cells from infection with HTLV-1, one could suggest that treatment based on the combination of As2O3 and AZT would be expected to induce cell death in HTLV-1–infected cells and prevent new infection.
Tax expression is down-regulated but p24 is up-regulated after arsenic trioxide treatment.
MT-2 cells were treated with control buffer, IFN-α, As2O3, or As2O3 + IFN-α for 48 hours. Sixty micrograms total protein was then resolved on 16% Tris-glycine gels transferred to PVDF membranes and probed with specific antibodies for (A) Tax or (B) Gag p24. Comparable protein loading was verified using an antibody specific for the β-tubulin protein (C).
Tax expression is down-regulated but p24 is up-regulated after arsenic trioxide treatment.
MT-2 cells were treated with control buffer, IFN-α, As2O3, or As2O3 + IFN-α for 48 hours. Sixty micrograms total protein was then resolved on 16% Tris-glycine gels transferred to PVDF membranes and probed with specific antibodies for (A) Tax or (B) Gag p24. Comparable protein loading was verified using an antibody specific for the β-tubulin protein (C).
In conclusion, these results confirm that although multiple apoptotic pathways are inhibited in HTLV-1–infected cells, these effects are reversible. This may open new avenues for treating HTLV-1–infected patients.
We thank Luigi Ravagnan for his technical advice during mitochondria enrichment, Wilfrid Mahieux for preparation of the figures, and Nicole Israël for the generous gift of some reagents.
Supported by a grant from Association de Recherche sur le Cancer and a Bourse Roux from the Pasteur Institute (R.M.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Renaud Mahieux, Unité d'Epidémiologie et Physiopathologie des Virus Oncogènes, Institut Pasteur, 28 rue du Docteur Roux, 75724 Paris cedex 15, France; e-mail:rmahieux@pasteur.fr.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal