Abstract
Heat-shock proteins (HSPs) act as molecular chaperones binding endogenous antigenic peptides and transporting them to major histocompatibility complexes. HSPs chaperone a broad repertoire of endogenous peptides including tumor antigens. For the immunotherapy of tumors, a strategy using HSPs may be more advantageous than other procedures because the identification of each tumor-specific antigen is not necessary. In this study, the efficacy of immunotherapy against minimal residual leukemia cells using HSP preparations was evaluated. HSP70 and GP96 were purified from syngeneic leukemia cell line A20 and immunized into BALB/c mice during the reconstitution period of the immune system after syngeneic bone marrow transplantation. In this procedure, all mice not immunized were dead within 60 days of A20 inoculation, whereas the survival times of HSP-immunized mice were significantly prolonged. In addition, the depletion of either CD4+ or CD8+ T lymphocyte significantly abrogated this efficacy, indicating that both CD4+ and CD8+ T lymphocytes were required for tumor cell rejection. Moreover, the vaccination of HSPs elicited a specific response of potent CD8+ T lymphocytes cytotoxic against A20 in vitro. These observations suggest that immunization of the complex of HSPs and peptides derived from leukemia cells leads to immune responses. These immune responses are sufficient to reject minimal amounts of leukemia cells for relatively immunocompromised mice after syngeneic bone marrow transplantation.
Introduction
Heat-shock proteins (HSPs) are classified according to subcellular localization and molecular weight; for example, HSP70 and HSP90 are located in the cytoplasm and GP96 in the endoplasmic reticulum.1 The major role of these proteins is to act as a molecular chaperone binding immature peptides during their synthesis and assisting their folding. After the peptides are degraded in the cytoplasm, they are transferred to the endoplasmic reticulum by binding to HSP70 or HSP90 but not by natural diffusion.2,3 The peptides are then bound to GP96 and loaded, through a transporter associated with antigen processing (TAP), onto major histocompatibility complex (MHC) class I molecules.4-6 It is known that HSPs bind antigenic peptides of the tumor cells, and tumor-derived HSP-antigenic peptide complexes can be purified for vaccination against cancer.7 The unique features of HSP-based cancer immunotherapy are as follows: (1) the spectrum of HSPs for binding peptides is broad; (2) HSPs are able to bind unknown peptides in vitro and to induce the peptide-specific immune response by vaccination with these peptide complexes; (3) HSP-peptide complexes lack diversity in their HSPs and are able to make use of different haplotype cases.8 Immunotherapy against malignant solid tumor has been extensively studied. It has been reported that specific immunity is induced by immunization with tumor-specific antigens.9,10 Furthermore, several vaccination programs of tumor-specific antigens for cancer patients are undergoing clinical trials.11,12 However, it is difficult to determine the specific antigens of each cancer patient and to identify the peptide motif presented on individual human leukocyte antigen molecules. For this reason, HSP-antigenic peptide complexes derived from tumors would be appropriate materials for the induction of tumor-specific immunity.7 One of the authors previously reported that vaccination with autologous cancer-derived HSP-peptide complex leads to cancer-specific immunity for mice bearing colon cancer without the need to identify tumor-specific antigenic peptides.13 In light of the complexities of determining individually specific antigens, this immunotherapy with an HSP-peptide complex would be a more convenient form of therapy.
Recently, autologous stem cell transplantations for hematologic malignancies have been carried out safely and successfully for elderly patients and for those unable to find donors with the necessary identical human leukocyte antigen.14-16 However, unlike allogeneic transplantation, a major problem is frequent relapse after transplantation because of the presence of minimal residual leukemia cells even after high-dose chemotherapy and the lack of graft-versus-leukemia (GVL) effect. In this study, we purified HSP-peptide complexes from leukemia cells and examined whether immunotherapy with HSPs is useful after syngeneic bone marrow transplantation (BMT) in mice with minimal residual leukemia cells.
Materials and methods
Experimental animals
Female BALB/c mice (H-2b, 5-6 weeks of age) were obtained from Japan Shizuoka Laboratory Center (Shizuoka, Japan) and were used as bone marrow recipients and donors. All animals were kept in conventional cages (6 animals in each cage) and received unsterilized food and water. Experimental animals were inspected daily for survival. All animals received care in compliance with the guidelines of Asahikawa Medical College.
Cell lines
A20 (American Type Culture Collection [ATCC], Manassas, VA), which is a B-cell leukemia/lymphoma cell line derived from 15-month-old BALB/c mice,17 T27A (ATCC), which is a myeloid leukemia cell line derived from BALB/c mice inoculated with N-tropic Friend leukemia virus,18 and colon 26, which is derived from colon adenocarcinoma in BALB/c mice,19 were used in this study. They were grown in RPMI 1640 medium (Gibco BRL, Grand Island, NY) supplemented with 10% fetal calf serum (FCS) and 0.5% 2-mercaptoethanol (ME) at 37°C on 5% CO2.
Purification of HSP70 and GP96
Purification of HSP70 and GP96 was performed as previously reported.20 Briefly, to purify the HSP70, a pellet of each cell line or liver tissue from healthy mice was homogenized in hypotonic buffer (10 mM NaHCO3, 0.5 mM phenylmethylsulfonyl fluoride [PMSF], pH 7.1) in a Dounce homogenizer and centrifuged at 100 000g for 30 minutes at 4°C. The supernatant was applied to a PD10 column (Pharmacia Biotech, Uppsala, Sweden) to remove low-molecular–weight materials and to change buffer to FPLC buffer D (20 mM Tris acetate, 20 mM NaCl, 15 mM 2-ME, 3 mM MgCl2, 0.5 mM PMSF, pH 7.5). The sample was applied to an adenosine 5′-diphosphate (ADP)–agarose column equilibrated with FPLC buffer D. The column was washed with buffer D containing 0.5 M NaCl and then incubated with buffer D containing 3 mM ADP at room temperature for 30 minutes. Then the sample was eluted with the same buffer and finally resolved on Mono Q system (Pharmacia Biotech) equilibrated with FPLC buffer A (20 mM sodium phosphate, 20 mM NaCl, pH 7.0) and eluted by a 20- to 600-mM NaCl gradient. Two micrograms protein from each fraction was resolved on 10% SDS-PAGE followed by the immunoblots using anti-HSP70 (anti-HSP72/73, clone N27F3-4; Stressgen, Sidney, BC, Canada). Fractions containing HSP70 were collected, and the quantity of HSP70 was determined using the Bradford protein assay (Bio-Rad Laboratories, Hercules, CA). The purity of purified protein was confirmed by silver staining.
To purify GP96, a pellet of each cell line and liver tissue from healthy mice was homogenized in buffer (30 mM NaHCO3, 1 mM PMSF, pH 7) and was centrifuged at 2000g for 10 minutes at 4°C. The supernatant was further centrifuged at 100 000g for 30 minutes at 4°C and brought to 50% ammonium sulfate saturation by adding it slowly while stirring for 1 hour at 4°C. The solution was centrifuged at 6000 rpm for 30 minutes, and ammonium sulfate of 70% saturation was added slowly to the supernatant. The solution was stored at 4°C for 1 hour and centrifuged, and the pellet was suspended in phosphate-buffered saline (PBS; 137 mM NaCl, 8.1 mM Na2HPO412H2O, 2.68 mM KCl, 1.47 mM KH2PO4), applied to a Con A column (Pharmacia Biotech), and washed with PBS. The column was incubated with 10% methyl-α-d-mannose pyraminoside at room temperature for 1 hour and subsequently eluted with the same buffer. Fractions were collected and tested by 10% SDS-PAGE followed by the immunoblots using anti-GP96 (anti-GRP94, clone 9G10; StressGen). GP96-containing fractions were pooled and applied onto Mono Q system equilibrated with FPLC buffer B (20 mM sodium phosphate, 20 mM NaCl, 0.1 mM EDTA, 15 mM 2-ME, pH 7) and eluted by a 400- to 600-mM NaCl gradient. Fractions were analyzed as HSP70.
Endotoxins of each of HSP preparation could not be detected (less than 5 pg/mL) by an endotoxin-specific chromogenic test (ES test; Seikagaku Kogyo, Tokyo, Japan).21
In vitro cytotoxic assay
Mixed lymphocyte-tumor cell culture (MLTC) was grown in vitro as previously described.22 Briefly, 8 × 106spleen cells of HSP-vaccinated mice were cultured for 5 days with 1.3 × 105 irradiated A20 cells in a volume of 1 mL RPMI 1640 medium containing 10% FCS and 0.5% 2-ME. Effector cells from MLTC were cultured with chromium Cr 51-labeled target cells (A20) in a volume of 200 μL RPMI 1640 medium containing 10% FCS and 0.5% 2-ME in 96-well round-bottom plates. After 6 hours of incubation at 37°C on 5% CO2, 100 μL supernatant was harvested, and the radioactivity of each sample was counted on a gamma counter. Results were presented as percentage of specific cytotoxicity calculated from the formula:
Spontaneous release and total 51Cr count were obtained from target cells incubated in medium alone and those disrupted with 2% NP-40, respectively.
For the experiment to determine the subset of effector cells, rat anti–mouse CD4 (clone GK1.5, immunoglobulin (Ig) G2b; ATCC) or anti-CD8 (clone 53-6.7, IgG2a; Pharmingen) was incubated with effector cells before cytotoxic assay. In addition, anti–mouse MHC class I antibodies (anti–mouse H-2Kd, clone SF1-1.1, IgG2a; Pharmingen and anti–mouse H-2Dd, clone 34-5-8S, IgG2a; Pharmingen) were incubated with A20 (target cells) before cytotoxic assay to determine the MHC class I restriction.
Conditioning and bone marrow transplantation
Syngeneic BMT in mice was performed according to the protocol reported previously.23 24 Briefly, the recipient mice were received a dose of 7.5 Gy total body irradiation (TBI) in a single dose by a cesium 137 source for conditioning regimen. In BALB/c mice, this dose was found to be lethal for 100% of the animals. Donor mice were killed by cervical dislocation under ether anesthesia. Bone marrow cells were aseptically collected from the femurs and tibias and suspended in RPMI 1640 medium. Two hours after TBI, 5 × 108/kg bone marrow mononuclear cells from healthy donor mice were intravenously injected into recipient mice at a constant volume of 0.2 mL through the retro-orbital sinuses.
Protocol of immunotherapy with HSPs
Ten days after BMT, 2.5 × 104 A20 cells were inoculated to recipient mice through the retro-orbital sinuses to make a model of minimal residual disease. This day was appointed day 0. Inoculated cell number was determined from the clinical results of suspected minimal residual tumor cell numbers of leukemia patients who had undergone chemotherapy and achieved complete response.25 HSP70 (20 μg or 40 μg) or GP96 (2.5 μg or 5 μg) derived from A20 were injected subcutaneously on days 4, 9, 14, and 19. Control groups of mice were treated with PBS (137 mM NaCl, 8.1 mM Na2HPO4 12H2O, 2.68 mM KCl, 1.47 mM KH2PO4), 40 μg HSP70 or 5 μg GP96 from normal liver. Survival times after the A20 cell inoculation were compared using the Kaplan and Meier method. For the experiments to determine the specificity of HSPs derived from A20, 40 μg HSP70 from T27A or colon 26 was injected subcutaneously in the same protocol described above.
In vivo depletion of CD4+ or CD8+ T cells from mice was carried out during this protocol of immunotherapy with HSPs, as described previously.13 26 Briefly, 200 μL 1:8 diluted anti-CD4 (clone GK1.5; ATCC) or anti-CD8 (clone 2.43; ATCC) ascites were intravenously injected into the retro-orbital sinus on days 2, 7, 12, and 17, each time 2 days before immunization of HSP. Depletion efficacy was confirmed by flow cytometry, and specific depletion was 90% to 100%.
Protocol of in vitro analysis of spleen cells immunized with HSPs
After TBI and BMT, 40 μg HSP70 or 5 μg GP96 was injected subcutaneously on days 18 and 25. MLTC was examined on day 32 with spleen cells from mice in these groups, and the specific cytotoxicity was determined by 51Cr release assay on day 37.
Results
Prolongation of survival days in mice injected with HSPs
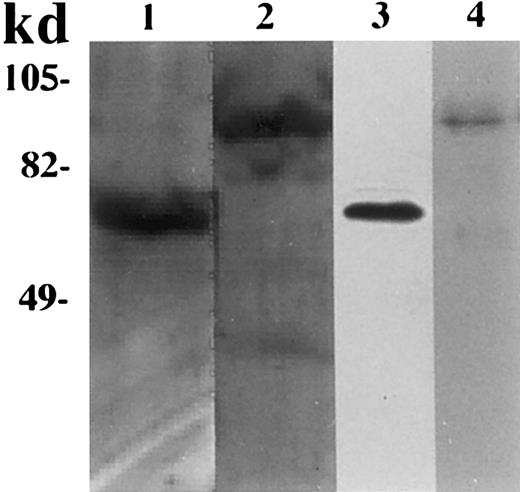
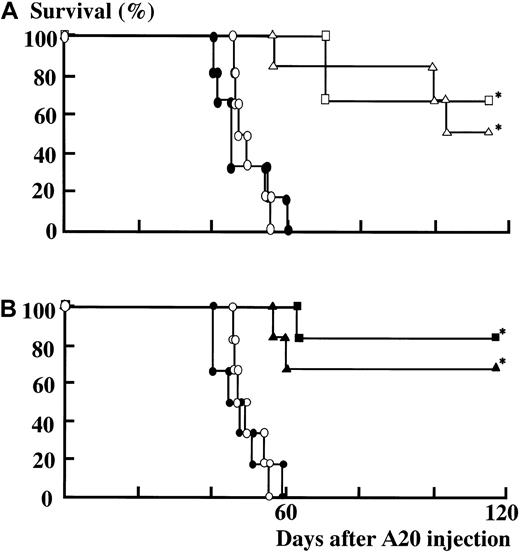
HSP70 or GP96 preparations derived from A20 cells were purified as described in “Materials and methods.” As shown in Figure1, SDS-PAGE of purified HSP70 and GP96 demonstrated a single band by silver staining (lanes 1 and 2), and these bands were reacted with anti-HSP70 and anti-GP96, respectively, by Western blot (lanes 3 and 4). These HSPs were injected into mice, as described in the experimental protocol used for immunotherapy in “Materials and methods.” In the syngeneic BMT procedure, the hematopoietic engraftment shown by the recovery of peripheral blood neutrophils was achieved on the 10th day after BMT. All the mice that received TBI without BMT died within 14 days because of bone marrow failure, whereas those that received both TBI and BMT survived (data not shown). As shown in Figure 2A, in the PBS-treated group, the mice inoculated with A20 cells after TBI and BMT died within 60 days because of systemic dissemination of A20 leukemia cells. Although the survival times in both groups of mice immunized with 20 μg or 40 μg HSP70 derived from A20 (A20-HSP70) were significantly prolonged (P < .01, Wilcoxon study), the mice that survived more than 80 days did not show any residual leukemia cells. Similarly, both groups of mice immunized with 2.5 μg or 5 μg GP96 derived from A20 (A20-GP96) had significantly prolonged survival compared to the PBS-treated group (P < .01, Wilcoxon study) (Figure 2B). In contrast, the survival times in the 40 μg HSP70 or the 5 μg GP96 immunized mice derived from healthy mice liver (liver-HSP70 or liver-GP96) did not show a significant difference from that in PBS-treated mice. These data suggested that repeated injection of HSPs derived from A20 (A20-HSPs) to A20-inoculated mice after BMT resulted in both the rejection of A20 and a survival increase.
SDS-PAGE followed by silver staining and immunoblots of purified HSP70 and GP96.
HSP70 and GP96 were purified from A20 as described in “Materials and methods.” Lane 1, silver staining of purified HSP70. Lane 2, silver staining of purified GP96. Preparations in lanes 1 or 2 were blotted on nitrocellulose membrane and probed with anti-HSP70 (lane 3) and anti-GP96 (lane 4).
SDS-PAGE followed by silver staining and immunoblots of purified HSP70 and GP96.
HSP70 and GP96 were purified from A20 as described in “Materials and methods.” Lane 1, silver staining of purified HSP70. Lane 2, silver staining of purified GP96. Preparations in lanes 1 or 2 were blotted on nitrocellulose membrane and probed with anti-HSP70 (lane 3) and anti-GP96 (lane 4).
Survival days for the groups of mice immunized.
(A) HSP70. (B) GP96. Ten days after BMT, recipient mice were inoculated with 2.5 × 104 A20 cells (day 0). Mice were immunized on days 4, 9, 14, and 19. (A) Immunized with PBS (○), 20 μg HSP70 derived from A20 cells (▵), 40 μg HSP70 derived from A20 cells (■), and 40 μg HSP70 derived from liver (●). (B) Immunized with PBS (○), 2.5 μg GP96 derived from A20 cells (▴), 5 μg GP96 derived from A20 cells (▪), and 5 μg GP96 derived from liver (●). Mice immunized with HSP70 (A) or GP96 (B) derived from A20 had significantly enhanced survival. *P < .01 versus PBS, Wilcoxon test. There were 6 mice in each group. Data are representative of 3 separate experiments.
Survival days for the groups of mice immunized.
(A) HSP70. (B) GP96. Ten days after BMT, recipient mice were inoculated with 2.5 × 104 A20 cells (day 0). Mice were immunized on days 4, 9, 14, and 19. (A) Immunized with PBS (○), 20 μg HSP70 derived from A20 cells (▵), 40 μg HSP70 derived from A20 cells (■), and 40 μg HSP70 derived from liver (●). (B) Immunized with PBS (○), 2.5 μg GP96 derived from A20 cells (▴), 5 μg GP96 derived from A20 cells (▪), and 5 μg GP96 derived from liver (●). Mice immunized with HSP70 (A) or GP96 (B) derived from A20 had significantly enhanced survival. *P < .01 versus PBS, Wilcoxon test. There were 6 mice in each group. Data are representative of 3 separate experiments.
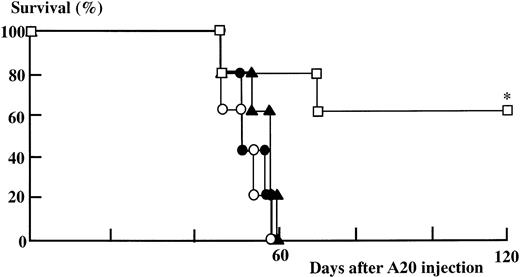
To investigate whether this survival increase was specific to the treatment of A20-HSPs, we injected HSPs derived from other syngeneic tumor cell lines to A20-inoculated mice after BMT. As shown in Figure3, although subcutaneous injection of 40 μg A20-HSP70 significantly increased survival, administration of the same amount of HSP70 derived from syngeneic colon adenocarcinoma cell line (colon 26) or myeloid leukemia cell line (T27A) did not show prolonged survival times in these mice. These results suggested that the survival increase induced by the administration of HSP preparations in A20-inoculated mice after syngeneic BMT was specific to HSPs derived from A20.
Survival days for the groups of mice immunized with HSP70 derived from other syngeneic tumor cell lines.
Ten days after BMT, recipient mice were inoculated with 2.5 × 104 A20 cells (day 0). Mice were immunized with HSPs on day 4, 9, 14, and 19, immunized with PBS (○), 40 μg HSP70 derived from A20 cells (■), 40 μg HSP70 derived from T27A cells (▴), and 40 μg HSP70 derived from colon 26 cells (●). Mice immunized with HSP70 derived from A20, but not HSP70 derived from other syngeneic tumor cells, had significantly enhanced survival. *P < .05 versus PBS, T27A and, colon 26; Wilcoxon test. There were 5 mice in each group. Data are representative of 3 separate experiments.
Survival days for the groups of mice immunized with HSP70 derived from other syngeneic tumor cell lines.
Ten days after BMT, recipient mice were inoculated with 2.5 × 104 A20 cells (day 0). Mice were immunized with HSPs on day 4, 9, 14, and 19, immunized with PBS (○), 40 μg HSP70 derived from A20 cells (■), 40 μg HSP70 derived from T27A cells (▴), and 40 μg HSP70 derived from colon 26 cells (●). Mice immunized with HSP70 derived from A20, but not HSP70 derived from other syngeneic tumor cells, had significantly enhanced survival. *P < .05 versus PBS, T27A and, colon 26; Wilcoxon test. There were 5 mice in each group. Data are representative of 3 separate experiments.
Involvement of CD4+ or CD8+ T cells in survival advantage
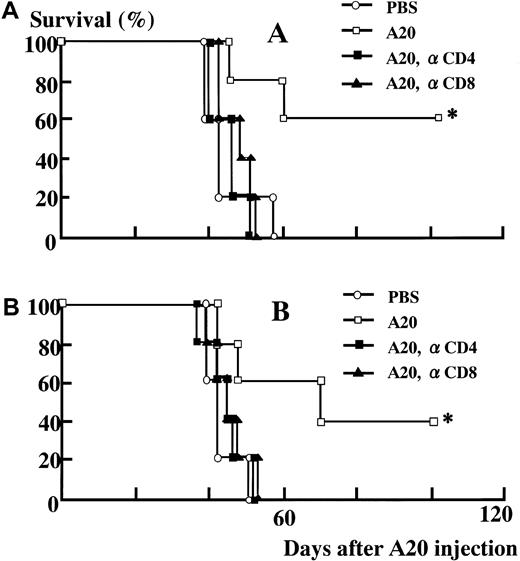
To identify the immune cells mediating the antitumor effects induced by A20-HSPs, we depleted mice CD4+ or CD8+ T lymphocytes in vivo by the intravenous injection of appropriate antibodies, as described in “Materials and methods.” As shown in Figure 4A, all the mice without immunization died within 60 days of A20 inoculation, whereas the mice immunized with A20-HSP70 had significantly prolonged survival times (P < .01, Wilcoxon study). In contrast, the depletion of CD4+ or CD8+ T lymphocytes completely abrogated the efficacy of immunization with A20-HSP70 (P < .01, Wilcoxon study), and the survival of mice with depleted CD4+ or CD8+ T lymphocytes was shortened to almost the same degree as that of mice without immunization. Similar to the results of A20-HSP70 immunization, immunization with A20-GP96 significantly prolonged the survival times, and the depletion of either CD4+ or CD8+ T lymphocytes completely abrogated this efficacy of A20-GP96 immunization (P < .01, Wilcoxon study) (Figure 4B). These results demonstrated that the immunity against A20 induced by A20-HSP70 or A20-GP96 administration required both CD4+ and CD8+ T lymphocytes.
Effect of in vivo depletion of CD4+ or CD8+ lymphocytes on survival in A20-inoculated mice.
(A) HSP70. (B) GP96. CD4+ or CD8+ lymphocytes were depleted by intravenous injection of anti-CD4 or anti-CD8 2 days before HSP immunization, as described in “Materials and methods.” (A) Immunized with PBS (○), 40 μg HSP70 derived from A20 cells (■), 40 μg HSP70 derived from A20 cells in CD4+T-cell–depleted mice (■), and 40μg HSP70 derived from A20 cells in CD8+ T-cell–depleted mice (▴). (B) Immunized with PBS (○), 5 μg GP96 derived from A20 cells (■), 5 μg GP96 derived from A20 cells in CD4+ T-cell–depleted mice (▪), and 5 μg GP96 derived from A20 cells in CD8+ T-cell–depleted mice (▴). Depletion of CD4+ or CD8+lymphocytes in vivo completely abrogated the survival efficacy of both HSP70 (A) and GP96 (B) immunization. *P < .01 versus PBS, CD4+ T-cell–depleted or CD8+ T-cell–depleted mice, Wilcoxon test. There were 5 mice in each group. Data are representative of 3 separate experiments.
Effect of in vivo depletion of CD4+ or CD8+ lymphocytes on survival in A20-inoculated mice.
(A) HSP70. (B) GP96. CD4+ or CD8+ lymphocytes were depleted by intravenous injection of anti-CD4 or anti-CD8 2 days before HSP immunization, as described in “Materials and methods.” (A) Immunized with PBS (○), 40 μg HSP70 derived from A20 cells (■), 40 μg HSP70 derived from A20 cells in CD4+T-cell–depleted mice (■), and 40μg HSP70 derived from A20 cells in CD8+ T-cell–depleted mice (▴). (B) Immunized with PBS (○), 5 μg GP96 derived from A20 cells (■), 5 μg GP96 derived from A20 cells in CD4+ T-cell–depleted mice (▪), and 5 μg GP96 derived from A20 cells in CD8+ T-cell–depleted mice (▴). Depletion of CD4+ or CD8+lymphocytes in vivo completely abrogated the survival efficacy of both HSP70 (A) and GP96 (B) immunization. *P < .01 versus PBS, CD4+ T-cell–depleted or CD8+ T-cell–depleted mice, Wilcoxon test. There were 5 mice in each group. Data are representative of 3 separate experiments.
Induction of cytotoxic T lymphocyte activities against A20 cells in vitro
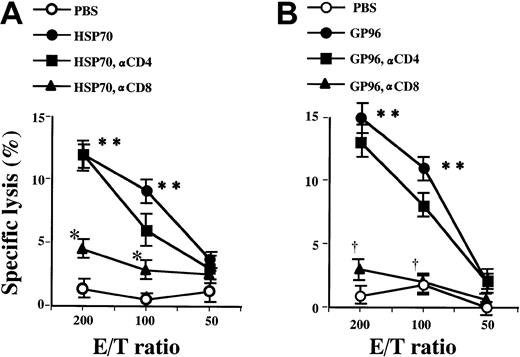
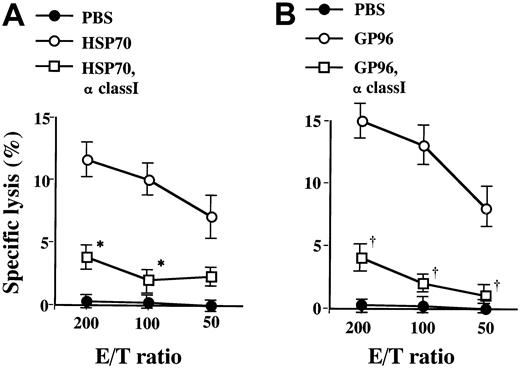
We next examined cytotoxic activities against A20 cells to investigate the immune response in effector phase of anti-A20 immunity. Mouse spleen cells were cultured with irradiated A20 cells, and the specific cytotoxicity against A20 was determined by 51Cr release assay as described in “Materials and methods.” A20 expressed a notable level of MHC class I (Kd and Dd), as detected on the cell surface by flow cytometry (data not shown). As shown in Figure 5, spleen cells derived from both A20-HSP70– and A20-GP96–immunized mice showed significant cytotoxicities against A20 cells at the effector/target cell (E/T) ratio of 200 and 100 (P < .01; t test). However, spleen cells derived from control mice did not show significant cytotoxicities against A20 cells. Therefore, the induction of specific cytotoxicities against A20 cells probably explains the mechanisms of tumor rejection by the administration of A20-HSP70 and A20-GP96. To determine the subset of effector cells in A20, specific killing induced by A20-HSP immunization, effector cells derived from A20-HSP70 or A20-GP96 immunized mice were pretreated with anti–mouse CD4 or anti-CD8 before cytotoxic assay. Cytotoxic activities induced by A20-HSP70 observed at E/T ratios of 200 and 100 were significantly blocked by anti-CD8 pretreatment (P < .01; t test). However, anti-CD4 pretreatment did not block the cytotoxicities against A20 by effector cells in A20-HSP70–immunized mice. Similarly, A20-GP96–induced cytotoxicities against A20 were significantly blocked by anti-CD8 pretreatment but not by anti-CD4 pretreatment (P < .01; t test). Because the CD8+ cells contain not only CTLs but also natural killer (NK) cells, we further analyzed the effector cells to distinguish these 2 cell populations. As shown in Figure 6, pretreatment of A20 cells (target cells) with anti–MHC class I (anti–mouse H-2Kd and anti–mouse H-2Dd) before cytotoxic assay significantly blocked the specific lysis by spleen cells derived from A20-HSP70–immunized mice (P < .01; t test). Similarly, A20-GP96–induced cytotoxicities against A20 were significantly blocked by anti–MHC class I pretreatment (P < .01; ttest). In addition, the level of specific lysis blocked by anti–MHC class I was almost equal to the level blocked by anti-CD8 shown in Figure 5. These results suggested that effector cells against A20, induced by A20-HSP immunization, were mainly contributed by CD8+ CTLs.
Effect of anti-CD4 and anti-CD8 on cytotoxic activities of mice spleen cells immunized with HSPs against A20.
After BMT, 40 μg HSP70 (A) or 5 μg GP96 (B) derived from A20 was injected subcutaneously on days 18 and 25. MLTC was examined on day 32 with spleen cells from mice in these groups, and the specific cytotoxicity against A20 cells was determined by 51Cr release assay on day 37. Mice spleen cells were pretreated with anti-CD4 or -CD8 before cytotoxic assay. Spleen cells derived from HSP70- or GP96-immunized mice showed significant cytotoxicities against A20. These cytotoxicities were significantly blocked by anti-CD8 but not by anti-CD4. Each point represents the mean of triplicate samples. Data are representative of 3 separate experiments. **P < .01 versus PBS. *P < .01 versus HSP70 derived from A20. †P < .01 versus GP96 derived from A20;t test.
Effect of anti-CD4 and anti-CD8 on cytotoxic activities of mice spleen cells immunized with HSPs against A20.
After BMT, 40 μg HSP70 (A) or 5 μg GP96 (B) derived from A20 was injected subcutaneously on days 18 and 25. MLTC was examined on day 32 with spleen cells from mice in these groups, and the specific cytotoxicity against A20 cells was determined by 51Cr release assay on day 37. Mice spleen cells were pretreated with anti-CD4 or -CD8 before cytotoxic assay. Spleen cells derived from HSP70- or GP96-immunized mice showed significant cytotoxicities against A20. These cytotoxicities were significantly blocked by anti-CD8 but not by anti-CD4. Each point represents the mean of triplicate samples. Data are representative of 3 separate experiments. **P < .01 versus PBS. *P < .01 versus HSP70 derived from A20. †P < .01 versus GP96 derived from A20;t test.
Effect of anti–MHC class I on cytotoxic activities of mice spleen cells immunized with HSPs against A20.
After BMT, 40 μg HSP70 (A) or 5 μg GP96 (B) derived from A20 was injected subcutaneously on days 18 and 25, and the specific cytotoxicity against A20 cells was determined by 51Cr release assay on day 37 as described in “Materials and methods.” A20 cells were pretreated with anti–MHC class I before cytotoxic assay. Cytotoxicities of the spleen cells derived from HSP70- or GP96-immunized mice against A20 were significantly blocked by anti–MHC class I. Each point represents the mean of triplicate samples. *P < .01 versus HSP70 derived from A20. †P < .01 versus GP96 derived from A20,t test.
Effect of anti–MHC class I on cytotoxic activities of mice spleen cells immunized with HSPs against A20.
After BMT, 40 μg HSP70 (A) or 5 μg GP96 (B) derived from A20 was injected subcutaneously on days 18 and 25, and the specific cytotoxicity against A20 cells was determined by 51Cr release assay on day 37 as described in “Materials and methods.” A20 cells were pretreated with anti–MHC class I before cytotoxic assay. Cytotoxicities of the spleen cells derived from HSP70- or GP96-immunized mice against A20 were significantly blocked by anti–MHC class I. Each point represents the mean of triplicate samples. *P < .01 versus HSP70 derived from A20. †P < .01 versus GP96 derived from A20,t test.
Discussion
In the present study, we demonstrated that immunization of leukemia cell-derived HSP70 or GP96 during the reconstitution periods of immune system after syngeneic BMT induced an effective survival advantage in mice with minimal residual leukemia cells. In addition, we revealed that this effect required both CD4+ and CD8+ T lymphocytes. Moreover, HSP70 and GP96 immunization induced the cytotoxic T lymphocyte activity in vitro against leukemia cells, from which HSPs were purified.
Our results demonstrating that leukemia cell–derived HSPs induced specific immunity and that CD4+ and CD8+ T lymphocytes are involved for this effect are consistent with the findings of other solid tumors.8,26-28 To confirm the specific cytotoxicity induced by HSPs, we injected HSPs derived from other syngeneic tumor cell lines to A20-inoculated mice after BMT. Because the subcutaneous injection of A20-HSP70 significantly increased survival and the same amount of HSP70, derived from syngeneic colon adenocarcinoma or myeloid leukemia cell lines, did not show the prolongation of survival days in these mice, the administration of both A20-HSP70 and A20-GP96 induced specific immunity against A20 cells. We also demonstrated that—based on the results of in vitro cytotoxicity assay, including blocking with anti-CD8 and anti–MHC class I antibodies—the effector cells against A20, induced by A20-HSP immunization, were CD8+ CTLs. It is becoming clear that the complexes of HSPs and antigenic peptides from tumor cells are taken up by antigen-presenting cells (APCs), such as macrophages and dendritic cells, through a putative receptor and are introduced into the endogenous pathway of antigen presentation.7 Moreover, the HSP-chaperoned peptides are thus presented by MHC class I molecules on the APCs, and these MHC-peptide complexes stimulate the CD8+ T lymphocytes to elicit the protective immunity to tumor cells. Similar mechanisms might have been active in our experimental system. In this regard, the contribution of NK cells to GVL effects has been reported in a similar mouse experimental model after allogeneic BMT using A20 cells.29 However, this study also found that the killing activity of NK cells against A20 cells after syngeneic BMT was low in vitro and that the survival effect of syngeneic BMT for A20-bearing mice was limited in vivo. Therefore, it is possible that NK cells might be involved in the GVL effects for A20-bearing mice after syngeneic BMT but that activity is not strong enough to reject leukemia cells. In contrast to syngeneic BMT, graft-versus-host reaction or host-versus-graft reaction might enhance the antileukemia cell potential of NK cells by cytokine release in allogeneic BMT.
Another concern is the role of CD4+ T lymphocytes on HSP-induced immunity. We demonstrated that CD4+ lymphocytes were required for the prolongation of survival by HSP immunization, whereas effector cells against A20 were CD8+ CTLs in vitro. Until now, it was unclear whether the peptides associated with HSPs were recognized by CD4+ T lymphocytes after they were presented on MHC class II. In the investigation of specific CTLs for lymphocytic choriomeningitis virus, CD62L+ naive T lymphocytes were activated and converted to effector–memory T lymphocytes.30 In addition, a reduced expression of CD62L on T lymphocytes was reported to be induced by immunogenic tumor vaccine, and these CD62 low/− T lymphocytes secreted type 1 cytokines that are known to lead cell-mediated immunity.31 Therefore, it is possible that CD4+ T lymphocytes are activated by an antigenic peptide provided by immunization with the HSP-peptide complex and presented by MHC class II on APCs. Eventually, activated CD4+ T lymphocytes might secrete type 1 cytokines, such as interleukin (IL)-2, interferon-γ, and tumor necrosis factor-β, and lead the cytotoxic CD8+ T lymphocytes.
In the previous studies demonstrating the effective induction of tumor-specific immunity by the HSP-peptide complex, the host immune system was relatively intact.8,26-28 In this study, however, the specific immunity by HSP administration was obtained after syngeneic BMT without any support to strengthen the immune system. From quantitative aspects, the immune system generally returns to normal within 3 to 4 months after syngeneic BMT in mice, though the recovery of qualitative immune function is longer.32 Therefore, the immunocompetence in our experimental mice was thought to be impaired. As shown in Figures 5 and 6, the effector–target cell ratio to obtain significant cytotoxicity was relatively high, and the level of cytotoxicity was low probably because of the partially immunocompromised state early after BMT. However, it is noteworthy that we could successfully induce effective cytotoxicities against A20 cells. Recently, exogenous HSPs have been shown to have a function of binding monocytes and stimulating the production of several cytokines.33 Therefore, it is possible that exogenously injected A20-HSPs not only act as a tumor vaccine but also stimulate the monocytes and help to activate the immune system in mice after BMT. Additional adoptive transfer of ex vivo–expanded APCs or stimulation of APCs in vivo with cytokines, such as flt-3 ligand or granulocyte macrophage–colony-stimulating factor, or T-cell activation by cytokines such as IL-2 or IL-7, may produce stronger killing effects in these immature immune conditions.
Because HSPs chaperone a broad repertoire of peptides, immunization with endogenous HSP-peptide complexes might elicit abnormal autoimmune responses. In addition, it is reported that mice administered dendritic cells pulsed with A20-derived peptides and fibroblasts expressing CD40 ligand and secreting IL-2 showed a systemic disorder resembling graft-versus-host disease.34 In this regard, mice immunized with A20-HSPs did not show fur loss or weight loss. In addition, we preliminarily analyzed the serum levels of alkaline phosphatase, alanine aminotransferase, and lactate dehydrogenase in the mice treated with A20-HSP70; no elevation of these serum enzyme activities was found (data not shown). Similarly, several hundred mice immunized with tumor or normal liver-derived GP96 show no detectable autoimmune phenomena.13 Contrary to our results, it is shown that the depletion of CD4+ lymphocyte in vivo has no immunologic effect on mice immunized with a combination of A20-derived peptide-pulsed dendritic cells and fibroblasts expressing CD40 ligand and secreting IL-2.34 Therefore it is suggested that the CD4+ lymphocytes in our experimental system might play an important role in the regulation of autoimmune disease development. Furthermore, a pilot study of the immunotherapy against human cancers with HSP-peptide complexes has been carried out for advanced malignancies that became refractory to established therapies. Until now, no unacceptable vaccine-related toxicity or autoimmune reactions were observed.1 35 Therefore, the immunization by HSP preparations is thought to be safe and might be clinically useful after autologous stem cell transplantation against minimal residual leukemia.
Recent advances in conventional chemotherapy or high-dose chemotherapy can reduce leukemia cell numbers, even if the initial cell burden is large. Therefore, after appropriate chemotherapeutic treatments supported by autologous hematopoietic stem cell transplantation, it is possible that immunotherapy against a limited number of leukemia cells could extinguish minimal residual disease. We demonstrated in this study that the administration of leukemia cell–derived HSP-peptide complexes led to specific immunity against leukemia cells during the reconstitution period of the immune system after syngeneic BMT in mice. Fortunately, abundant leukemia cells can be obtained from peripheral blood or bone marrow from most patients with leukemia. Therefore, it is possible to prepare sufficient amounts of leukemia cell–derived HSPs from patients, and these purified HSPs might be clinically useful to induce specific immunity. The observations reported in this study will provide the basis for a new generation of vaccines for patients with leukemia.
Supported by a Grant-in Aid for Scientific Research (C) from the Japanese Ministry of Education, Science, Sports and Culture.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Yoshihiro Torimoto, The Third Department of Internal Medicine, Asahikawa Medical College, Midorigaoka Higashi 2-1, Asahikawa, Hokkaido, 078-8510 Japan; e-mail: tori@asahikawa-med.ac.jp.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal