Factor Va is the important cofactor for prothrombinase. Factor Va is inactivated by activated protein C (APC) following 3 cleavages of the heavy chain at Arg306, Arg506, and Arg679.1Cleavage of normal factor Va by APC at these sites results in the production of Mr 45 000, Mr 30 000, Mr 22 000 and 20 000 fragments.1 In plasma, following the addition of APC and a synthetic membrane surface (phosphatidylcholine phosphatidylserine [PCPS]), appearance of the Mr 30 000 fragment demonstrates cleavage of normal factor V at Arg306 and Arg506.2 The Mr 30 000 fragment can be detected in plasma by using an anti–human factor V monoclonal antibody that recognizes an epitope located between residues 307 and 506 of the molecule.2 3
The R2 haplotype in factor V is characterized by an A4070G substitution (His1299Arg) in the factor V molecule and is associated with mild APC resistance,4 but the underlying molecular mechanism remains unclear. We have recently described a thrombotic family with 4 symptomatic members.5 One of them (I3) was doubly heterozygous for the factor V HR2 haplotype and for the factor V Tyr1702Cys mutation, causing CRM–factor V deficiency. Since the factor V allele predicting the Tyr1702Cys substitution is not expressed at the protein level,5 the plasma of this patient contains only R2 factor V, in accordance with her reduced factor V levels (FV:Ag 43%; FV:C 36%; normal range 70%-130%) and mild APC resistance (nAPC-sr 0.72, normal values > 0.84). We have concluded that while the His1299Arg substitution in factor V induces APC resistance, the presence of the Tyr1702Cys mutation was responsible for absence of expression of the corresponding allele (previously reported to result in CRM–factor V deficiency5). This particular condition (pseudohomozygosity for the factor V HR2 haplotype) offers the opportunity to study the APC-mediated inactivation of R2 factor Va in plasma, which is otherwise possible only in the rare (∼0.4% of the general population) homozygous individuals.
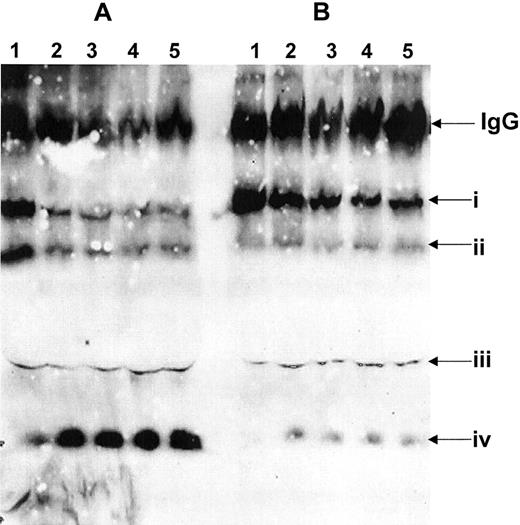
Molecular investigations were undertaken in this thrombotic patient (I3, see Castoldi et al5). The patient was found to be heterozygous, at both the DNA and messenger RNA (mRNA) levels, for the His1299Arg and Asp2194Gly substitutions, characterizing the HR2 haplotype4 as well as for the Tyr1702Cys mutation in factor V. No mutation, in addition to the polymorphic changes previously described4,5 in the factor V gene, were found in this patient at the DNA and/or RNA levels and in particular in exon 7 (Arg306 cleavage site), exon 10 (Arg506 cleavage site), and exon 18 (interaction with APC). Factor Va cleavage in the patient's plasma was investigated by analyzing the presence or absence of the Mr30 000 fragment following incubation of the plasma with APC and PCPS as described.2 Slow cleavage of factor Va at Arg506/Arg306 could be detected in the plasma of the propositus as compared with the rapid cleavage of factor Va in normal plasma and generation of the Mr 30 000 fragment (Figure1A, lanes 2-5). Substantial amounts of uncleaved heavy chain remained in the patient's plasma following extended incubation with APC and PCPS, and low amounts of the Mr 30 000 fragment were generated (Figure 1B, lanes 2-5). These data demonstrate an APC resistance in this individual. Since the allele carrying the Tyr1702Cys substitution is not expressed,5 this individual can be defined as a pseudohomozygous R2 genotype. Thus, because of the absence of normal factor V in the patient's plasma, the factor V molecules resistant to APC inactivation are characterized by the mutations included in the HR2 haplotype.7 These findings suggest the possibility that 1 or more of the amino acid substitutions predicted by the HR2 haplotype might impair factor Va cleavage at Arg506/Arg306, possibly by preventing optimal interaction with APC. Alternatively, impaired factor Va inactivation may result from suboptimal interaction with phospholipid membranes. Overall, our data confirm previous findings that the Tyr1702Cys substitution causes CRM–factor V deficiency and strongly suggest that the amino acid substitutions in R2 factor V confer APC resistance by impairing APC–factor Va interaction, cleavage at Arg506 or Arg306, and subsequent inactivation of factor Va.
Identification of the factor V molecule present in plasma.
Citrated plasma (100 μL) from a pool of normal plasma (A) and from patient I3 (Castoldi et al5, B) was diluted 10-fold in a buffer containing 5 mM CaCl2 and treated with phospholipid vesicles and APC (5 nM) as described.2,3 Immunoreactive fragments were detected using the monoclonal antibody αHFVaHC17 under nonreducing conditions.2 (A) Normal pool plasma; (B) plasma from patient I3 (Catoldi et al5). Lane 1, plasma immediately following clot formation and the addition of APC (5 nM, ∼20 sec); lanes 3-5 plasma at 5, 10, 20, and 30 min following the addition of APC. Roman numerals on the right indicate the following: (i) the heavy chain of factor Va following clot formation; (ii) the Mr 75 000 fragment deriving from cleavage of the heavy chain of factor Va at Arg506 (amino acid residues 1-506); (iii) the Mr 60 000 fragment that derives from factor Va following cleavage at Arg306 (amino acid residues 307-709); (iv) the Mr 30 000 fragment derived from normal factor Va following cleavage at Arg506 and Arg306 (amino acid residues 307-506). The position of the immunoglobulin G (IgG) molecules (nonreduced) is also shown.
Identification of the factor V molecule present in plasma.
Citrated plasma (100 μL) from a pool of normal plasma (A) and from patient I3 (Castoldi et al5, B) was diluted 10-fold in a buffer containing 5 mM CaCl2 and treated with phospholipid vesicles and APC (5 nM) as described.2,3 Immunoreactive fragments were detected using the monoclonal antibody αHFVaHC17 under nonreducing conditions.2 (A) Normal pool plasma; (B) plasma from patient I3 (Catoldi et al5). Lane 1, plasma immediately following clot formation and the addition of APC (5 nM, ∼20 sec); lanes 3-5 plasma at 5, 10, 20, and 30 min following the addition of APC. Roman numerals on the right indicate the following: (i) the heavy chain of factor Va following clot formation; (ii) the Mr 75 000 fragment deriving from cleavage of the heavy chain of factor Va at Arg506 (amino acid residues 1-506); (iii) the Mr 60 000 fragment that derives from factor Va following cleavage at Arg306 (amino acid residues 307-709); (iv) the Mr 30 000 fragment derived from normal factor Va following cleavage at Arg506 and Arg306 (amino acid residues 307-506). The position of the immunoglobulin G (IgG) molecules (nonreduced) is also shown.
Recently, Hoekema et al6 have reported that the rate constants of APC-catalyzed inactivation of normal factor Va and factor Va from individuals with the R2 haplotype were similar. Our present data using a different methodological approach from the one used by Hoekema et al6 clearly demonstrate that in a pseudohomozygous individual the polymorphisms included in the HR2 haplotype confer APC resistance by delaying cleavages at both Arg506 and Arg306. Contribution by other factors present in patient's plasma is unlikely in our experimental system. At present we cannot generalize our findings to all patients with the HR2 phenotype since we have studied by this method only patients related to this family (Castoldi et al5 and present data). It is noteworthy that the patient studied herein is also a carrier of the Asp2194Gly substitution. In fact all the subjects of this family5carrying the R2 allele (His1299Arg mutation) are also carriers of the Asp2194Gly substitution in factor V, and the latter mutation is tightly associated with the R2 phenotype.7 Since the His1299Arg substitution is located in the B region of the cofactor, most likely the APC resistance of factor Va observed in this individual is due to the Asp2194Gly mutation, which is located on the light chain of the active cofactor. Interestingly, Kim et al using alanine-scanning mutagenesis demonstrated that several amino acid residues within the C2 domain of factor V are crucial for the interaction of the cofactor with phosphatidylserine. Among those, the Asp2194Ala factor V mutant had impaired binding to phosphatidylserine.8 Thus, it is possible that factor Va interacts less efficiently with the membrane surface, due to the Asp2194Gly substitution encoded by the HR2 haplotype resulting in delayed cleavage at Arg306 and/or Arg506 of the heavy chain of the cofactor and APC resistance.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal