Abstract
The bcr/abl fusion in chronic myelogenous leukemia (CML) creates a chimeric tyrosine kinase with dramatically different properties than intact c-abl. In P210 bcr/abl, the bcr portion includes a coiled-coil oligomerization domain (amino acids 1-63) and a grb2-binding site at tyrosine 177 (Tyr177) that are critical for fibroblast transformation, but give variable results in other cell lines. To investigate the role of the coiled-coil domain and Tyr177 in promoting CML, 4 P210 bcr/abl-derived mutants containing different bcr domains fused to abl were constructed. All 4 mutants, Δ(1-63) bcr/abl, (1-63) bcr/abl, Tyr177Phe bcr/abl, and (1-210) bcr/abl exhibited elevated tyrosine kinase activity and conferred factor-independent growth in cell lines. In contrast, differences in the transforming potential of the 4 mutants occurred in our mouse model, in which all mice receiving P210 bcr/abl-expressing bone marrow cells exclusively develop a myeloproliferative disease (MPD) resembling human CML. Of the 4 mutants assayed, only 1-210 bcr/abl, containing both the coiled-coil domain and Tyr177, induced MPD. Unlike full-length P210, this mutant also caused a simultaneous B-cell acute lymphocytic leukemia (ALL). The other 3 mutants, (1-63) bcr/abl, Tyr177Phe bcr/abl, and Δ(1-63) bcr/abl, failed to induce an MPD but instead caused T-cell ALL. These results show that both the bcr coiled-coil domain and Tyr177 are required for MPD induction by bcr/abl and provide the basis for investigating downstream signaling pathways that lead to CML.
Introduction
The P210 bcr/abl (P210) fusion oncoprotein results from the t(9;22) chromosomal translocation.1 The c-abl protein is a tightly regulated tyrosine kinase that is predominantly nuclear in hematopoietic cells, whereas bcr is cytoplasmic with serine/threonine kinase activity.2,3 The t(9;22) results in a chimeric protein in which the first exon of c-abl is replaced by truncated bcr that not only creates a novel cytoplasmic fusion protein but also places transcriptional control of abl expression under the bcr promoter. The overwhelming majority of humans with chronic myelogenous leukemia (CML) have the P210 fusion protein; however, a small minority express either a P190 or a P230 bcr/abl fusion protein.4,5 All 3 isoforms are composed of identical c-abl C-terminal coding sequences but differ in their NH2-terminal bcr sequences. P190 contains bcr exon 1, P210 contains bcr exons 1-12/13, and P230 contains exons 1-19.4 Although these 3 different bcr/abl fusion proteins have different propensities to cause CML, acute lymphocytic leukemia (ALL), and neutrophilic CML, each has been identified in patients with CML. The association of each of these 3 different bcr/abl fusion proteins with CML suggests that the minimal bcr sequences required to induce chronic-phase CML are located within exon 1. This possibility is supported by results from retroviral transduction studies in mice in which P190, P210, and P230 cause a similar myeloproliferative disease (MPD) when introduced into murine hematopoietic stem cells6 (J.P.M., W.S.P., unpublished observations, August 1998).
The P210 fusion oncoprotein contains multiple functional domains/motifs. The c-abl protein contains SH3 and SH2 domains, tyrosine kinase activity, motifs for nuclear localization, DNA and actin binding, as well as docking sites for several adapter molecules.3,7,8 The bcr region of P210 includes a coiled-coil (C-C) oligomerization domain (amino acids 1-63), followed by a grb2-binding site at Tyr177, an SH2 binding domain (amino acids 192-214 and 298-413), a serine/threonine kinase domain (amino acids 299-413), Dbl/CDC24 guanine-nucleotide exchange factor homology domain, pleckstrin homology domain, and binding sites for the Abl SH2 domain and several other molecules including 14-3-3.2 9-12 The common bcr region between P190, P210, and P230 contains the C-C domain, Tyr177, SH2-binding domain, and serine/threonine kinase domain.
Numerous studies have been performed to understand the molecular mechanisms of bcr/abl-induced transformation and multiple signaling pathways activated by this chimeric tyrosine kinase have been identified. Most of these studies relied on fibroblast transformation or cytokine-independent growth of transformed hematopoietic cell lines.13 Although all assays suggest that abl tyrosine kinase activity is essential for bcr/abl transformation, the importance of other domains has been equivocal depending on the assay. For example, the Tyr177 motif in bcr is essential for fibroblast transformation, yet dispensable for rescue of factor-dependent hematopoietic cells.10,14 15 It is unclear which of these in vitro assays is more relevant to CML because neither replicates the MPD that is the hallmark of this disease.
To overcome the limitations of assays that may not be relevant to CML, we and others have developed a murine model in which mice receiving P210-transduced bone marrow (BM) cells develop a fatal MPD.6 16-18 The MPD occurs within 21 days of bone marrow transplantation (BMT) in 100% of recipient mice. The development of a 100% efficient reproducible murine model provides the basis for in vivo structure function analysis of bcr/abl. In this report, we focus on several domains within bcr that are necessary for induction of the murine MPD. In particular, we have focused on the C-C domain (amino acids 1-63) and Tyr177 of Bcr. The importance of these domains to the development of the MPD is unclear because results from in vitro studies have been ambiguous. To study the role of the C-C domain and Tyr177 grb2-binding site in the pathogenesis of CML, we assayed 4 different bcr/abl mutant proteins in our in vivo murine model. In vitro studies showed that neither the N-terminal C-C domain nor Tyr177 was required for in vitro kinase activity or rescue of factor-dependent hematopoietic cell lines. In contrast, both regions were required to induce a murine MPD. These findings suggest that the specific signaling pathways activated by both the N-terminal C-C domain and Tyr177 are required for the MPD.
Materials and methods
Plasmid constructs
MigR1 and Mig210 have been described.17 For (1-63) bcr/abl cloning, 5′ primer 77790 TCA CTC CTT CTC TAG GC and 3′ primer 77791 GCC GCT GAA GGG CTT TCA GCA ACG TCT GCA GG were used for polymerase chain reaction (PCR) to produce fragment 1. For fragment 2 PCR, 5′ primer 77792 CCT GCA GAC GTT GCT GAA AGC CCT TCA GCG GC and 3′ primer 77793 AGC AGA TAC TCA GCG GC were used. Two PCR products were purified using the GENECLEAN Spin Kit (Bio101, Vista, CA) and subsequently mixed as the template for PCR using primers 77790 and 77793 to obtain fragment 3, which was then purified and digested withEcoR1 and Asp718. The P210 complementary DNA (cDNA) was released from Mig210 using EcoR1 and subsequently digested with Asp718, and the 3′ cDNA fragment (3.8 kb) was purified. A 3-way ligation was performed using EcoR1 linearized MigR1,EcoR1/Asp718-digested fragment 3, and the 3.8-kb P210 fragment. To clone (1-210) bcr/abl, the 5′ primer 81220 AGG GTT CTC CGG GTA AG and 3′ primer 81221 GCC GCT GAA GGG CTT TCA TCT GCA TGG CCT GG were used to PCR fragment 1. The 5′ primer 81222 CCA GGC CAT GCA GAT GAA AGC CCT TCA GCG GC and the above-mentioned primer 77793 as 3′ primer were used for PCR to produce fragment 2. Two PCR fragments were purified and mixed as template to amplify fragment 3 using primer 81220 and 77793. Fragment 3 was digested with BamHI and Asp718. Mig210 was digested with EcoR1 and BamHI, and a 690-bp fragment was isolated. A 4-way ligation was performed to clone (1-210) bcr/abl into MigR1, using EcoR1-linearized MigR1 as vector, the 690-bp fragment, BamHI/Asp718-digested PCR fragment 3, and the above-mentioned 3.8-kb fragment as inserts. The cloned cDNAs were confirmed by sequencing. Construction of Try177Phe19 and Δ(1-63) bcr/abl (J.A.W. et al, manuscript in preparation) are described elsewhere and were confirmed by sequencing. For in vitro translation, the P210 cDNA was cloned into pSP72 (Promega, Madison, WI). For in vitro translation of His-tagged bcr, Mig210 was digested with MseI to release a 3-kb fragment that encodes the first 925 amino acids of bcr. TheMseI site was filled in with Klenow and the cDNA was cloned into the EcoRV site of the pMT/V5-HisA vector (Invitrogen, Carlsbad, CA). The resulting cDNA, encoding the first 925 amino acids of bcr with a C-terminal V5 epitope and poly-Histine tag, was released with EcoRI and PmeI, and subsequently cloned into the EcoRI and EcoRV sites of pSP72. A similar strategy was used to subclone His-tagged Δ(1-63) bcr into pSP72 via the pMT/V5-HisA intermediate vector, except that the Δ(1-63) bcr cDNA was first released from Mig Δ(1-63) bcr/abl withHapI and MseI.
Immunokinase assay
Each construct was transfected into Bosc23 cells as described previously.17 For the Crk212 control experiments,20 the v-Abl–expressing cell line N54 or FL5.12 cells stably expressing P185, P210, or P210Tyr177Phe were used directly. Two days after transfection, cells were labeled with35S-methionine (NEN, Boston, MA, Catalog no. NEG-072) for 4 hours. Cells were lysed in Triton-X lysis buffer (50 mM Hepes, pH 7.4, 150 mM NaCl, 10% glycerol, 1% Triton-X, 1 mM EGTA, 1.5 mM MgCl2) with protease inhibitors (1 mM sodium orthovanadate, 1 mM phenylmenthylsulfonyl fluoride [PMSF], 10 μg/mL leupeptin, 20 μg/mL aprotinin). The lysate was then immunoprecipitated with α-Abl (24-11, Santa Cruz Biotechnology, Santa Cruz, CA), and subsequently washed with the lysis buffer. After the wash, 80% of the volume of the immunoprecipitate (in 25 μL) was mixed with an equal volume of 2 times sodium dodecyl sulfate (SDS) loading buffer (120 mM Tris, pH 6.8, 10% 2-mercaptoethanol, 4% SDS, 20% glycerol, 0.1% bromophenol blue) for SDS–polyacrylamide gel electrophoresis (SDS-PAGE). One-fifth volume of the immunoprecipitate was washed with 1 times kinase reaction buffer (50 mM Hepes, pH 7.4, 10 mM MgCl2). The kinase reaction was performed in 100 μL containing 1 times kinase reaction buffer, 5 μg substrate, 0.5 μL 2 mM cold adenosine triphosphate (ATP) and 10 μCi (0.37 MBq) γ-[32P] ATP for 5 minutes at room temperature. The kinase reaction was terminated by adding 1 mL cold phosphate-buffered saline (PBS) and washed 5 times with cold PBS. After the final wash, an equal volume of 2 times SDS buffer was added to obtain the final volume of 50 μL for SDS-PAGE. The SDS–polyacrylamide gels were then analyzed by autoradiography.
Coimmunoprecipitation and immunoblotting
Each construct was transfected into Bosc cells as described above.17 Two days after transfection, cells were washed with cold PBS and then lysed in 1 times NP-40 lysis buffer (50 mM Tris, pH 7.6, 150 mM NaCl, 1% NP-40, protease inhibitors mentioned above). A small aliquot of the whole lysis was kept and mixed with SDS loading buffer. The remaining cell lysis supernatant was then immunoprecipitated with anti-Abl antibody 24-11 and the immunoprecipitate was washed 4 times with 1 times NP-40 lysis buffer. After the last wash, an equal volume of SDS loading buffer was added to obtain the final volume of 50 μL. The sample was then subjected to SDS-PAGE and transferred to nitrocellulose membranes, and the protein blots were probed with 24-11 or α-grb2 antibody (Transduction Laboratories, Lexington, KY). The whole cell lysis mentioned above was immunoblotted with the same grb2 antibody. For mouse tissue and FL5.12 immunoblots, the cell suspension (2 × 107cells/mL) was kept in cold PBS with the protease inhibitors described above. An equal volume of 2 times SDS loading buffer was added and the lysate was boiled for 5 minutes. The lysate was sonicated and cleared by centrifugation. The cell lysate was resolved by SDS-PAGE and transferred to nitrocellulose membranes. Protein blots were probed with anti-abl antibody 24-11 or antiphophotyrosine antibody (PY20; Transduction Laboratories) or 4G10 (Upstate Biotechnology, Lake Placid, NY).
The protocol for investigating the interaction between P210 and bcr was kindly provided by Rick Van Etten (K. Smith, R. Van Etten, written personal communication, August 18, 2001). Briefly, proteins were coexpressed using an in vitro transcription/translation (IVT) reticulocyte lysate system (Promega) and the products were labeled with35S-methionine. Then, 40 μL of the IVT products was mixed with 460 μL c-Abl lysis buffer (10 mM Tris-HCL, pH 7.6, 50 mM NaCl, 5 mM EDTA, 30 mM sodium pyrophosphate,1% Triton X-100, 1 mM PMSF, 1% aprotinin, 25 mM NaF, 1 mM NaVO4) and precleared with protein G agarose at 4°C for 1 hour. The precleared supernatant was combined with 1 μg anti-His monoclonal antibody (mAb; Invitrogen) and allowed to immunoprecipitate overnight at 4°C, and subsequently precipitated with protein G agarose for 1 hour, followed by washing (3 times) with 1 mL c-abl lysis buffer. The agarose was resuspended in 20 μL SDS loading buffer, boiled, and subjected to 7% SDS-PAGE. The SDS-PAGE gel was dried and subjected to autoradiography.
Retrovirus preparation and BM infection/BMT
Protocols were performed as previously described.17All retroviral supernatants were titered before use, stored at −80°C, and normalized as previously described.17Briefly, retroviral supernatants were harvested from transiently transfected Bosc23 cells. The retroviral supernatants were stored at −80°C and a 100-μL test aliquot was thawed and used to transduce 2 × 105 NIH3T3 cells that had been plated on a 60-mm dish the previous afternoon. The NIH3T3 cells were trypsinized 48 hours after transduction and analyzed by fluorescence-activated cell sorting (FACS) for green fluorescent protein (GFP) expression. All retroviral supernatants used in the experiments reported in this manuscript gave between 20% and 30% GFP-expressing cells per 100 μL retroviral supernatant (data not shown). We have previously shown that this infectious titer is in the linear range and that infectious titers of 20% allow P210 bcr/abl to induce an MPD in 100% of mice receiving transduced BM cells.17 All BM transductions were performed by spinoculation in the absence of producer cells. All in vivo experiments were repeated at least once using at least 2 different preparations of retroviral supernatant.
Flow cytometry and DNA analysis
These were performed as previously described.17
Results
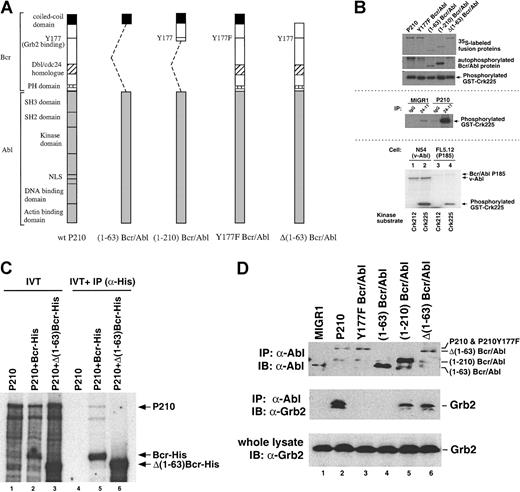
All 4 bcr/abl mutants demonstrate activated tyrosine kinase activity
To determine the requirement for the C-C and Tyr177 bcr domains in the pathogenesis of the murine MPD, 4 P210-derived mutants were constructed. Based on previous studies, we hypothesized that the NH2-terminal C-C domain or the C-C domain plus the grb2-binding site would be sufficient for MPD induction. To test this hypothesis, 4 mutants that contained identical P210-derived c-abl sequences, preceded by different bcr mutant sequences, were assembled (Figure1A). To assay the contribution of the C-C domain directly, 1-63 bcr/abl and Δ(1-63) bcr/abl were constructed. The former appends amino acids 1-63 of bcr to the second exon of c-abl, whereas the latter contains all of P210 except amino acids 1-63 of bcr. The role of Tyr177 was assayed by mutating this residue to phenylalanine (Tyr177Phe bcr/abl). A fourth mutant ([1-210] bcr/abl) fuses the N-terminal 210 amino acids of bcr to the c-abl second exon and contains both the C-C domain and Tyr177. This region lacks 717 amino acid from P210. The mutant cDNAs were cloned into the MigR1 retroviral vector that coexpresses GFP as a surrogate marker.17 Transient expression in Bosc23 cells confirmed that proteins of the correct molecular weight were produced (Figure 1B and data not shown).
Structures and biochemical characterization of bcr/abl proteins.
(A) Schematic of full-length and mutant bcr/abl proteins. The identical COOH-terminal abl portion of the chimeric protein (shaded bar) is present in all fusions. Some of the characterized domains are indicated on the left of wild-type P210. The NH2-terminal of the Abl portion is preceded by different truncated Bcr fragments to produce (1-63) bcr/abl, (1-210) bcr/abl, and Δ(1-63) bcr/abl. P210Tyr177Phe bcr/abl is derived from wild-type P210 with a Tyr177Phe substitution. (B) Kinase activity of wild-type P210 and bcr/abl mutants. Bosc cells were transiently transfected with the indicated constructs and labeled with 35S-methionine. Whole cell lysates were then immunoprecipitated with anti-Abl antibody 24-11. Equal amounts of each immunoprecipitated sample were subjected to SDS-PAGE to reveal the immunoprecipitated bcr/abl protein. Equal aliquots of each immunoprecipitated sample were subjected to an in vitro kinase assay. The figure shows both autophosphorylated bcr/abl and the phosphorylated exogenous substrate GST-Crk. To show specificity, Bosc cells were transfected with MigR1 or P210, immunoprecipitated with control mouse IgG or 24-11 and subjected to identical procedures (middle panel). To show that the immunoprecipitated bcr/abl specifically phosphorylated Crk on phosphotyrosine, the Crk212 mutant,20 which lacks the critical Tyr221 residue, was also used as an exogenous substrate. The α-abl mAb, 24-11, was used to immunoprecipitate the lysates of a v-Abl–expressing cell line N54 or P185-expressing cell line FL5.12 and identical assays were performed using 5 μg of either GST-Crk225 or GST-Crk212. As shown in the bottom section of panel B, Crk225 (lanes 2 and 4), but not Crk212 (lanes 1 and 3), was phosphorylated in this assay. Identical results were obtained in assays using P210 or P210Tyr177-expressing FL5.12 cells (data not shown). (C) P210 bcr/abl was in vitro translated and labeled with 35S-methionine alone or together with either the C-terminal His-tagged bcr polypeptide from P210's bcr portion or the C-terminal His-tagged Δ(1-63) bcr polypeptide from Δ(1-63) bcr/abl's Δ(1-63) bcr portion (lanes 1-3). The in vitro translated products were immunoprecipitated with an α-His mAb. The α-His mAb did not pull down P210 (lane 4), whereas it was able to pull down both the bcr and Δ(1-63) bcr polypeptides (lanes 5 and 6). P210 could only be coimmunoprecipitated with bcr polypeptides but not with the Δ(1-63) bcr polypeptide (lane 5 and 6). The correct P210 band was confirmed by immunoprecipitation with the α-abl mAb 24-11 (data not shown). (D) Grb2 fails to associate with bcr/abl mutants lacking Tyr177. Whole cell lysates of Bosc cells transfected with the indicated construct were coimmunoprecipitated with α-abl 24-11. The coimmunoprecipitated samples were immunoblotted with α-abl (upper panel) or α-grb2 antibody (middle panel). The upper panel shows that each bcr/abl protein was immunoprecipitated and the corresponding proteins are indicated on the right. The middle panel shows that only the wild-type P210 (lane 2), (1-210) bcr/abl (lane 5) and Δ(1-63) bcr/abl (lane 6) bound grb2. In the bottom panel, the whole cell lysates were immunoblotted with α-grb2 antibody as the internal control.
Structures and biochemical characterization of bcr/abl proteins.
(A) Schematic of full-length and mutant bcr/abl proteins. The identical COOH-terminal abl portion of the chimeric protein (shaded bar) is present in all fusions. Some of the characterized domains are indicated on the left of wild-type P210. The NH2-terminal of the Abl portion is preceded by different truncated Bcr fragments to produce (1-63) bcr/abl, (1-210) bcr/abl, and Δ(1-63) bcr/abl. P210Tyr177Phe bcr/abl is derived from wild-type P210 with a Tyr177Phe substitution. (B) Kinase activity of wild-type P210 and bcr/abl mutants. Bosc cells were transiently transfected with the indicated constructs and labeled with 35S-methionine. Whole cell lysates were then immunoprecipitated with anti-Abl antibody 24-11. Equal amounts of each immunoprecipitated sample were subjected to SDS-PAGE to reveal the immunoprecipitated bcr/abl protein. Equal aliquots of each immunoprecipitated sample were subjected to an in vitro kinase assay. The figure shows both autophosphorylated bcr/abl and the phosphorylated exogenous substrate GST-Crk. To show specificity, Bosc cells were transfected with MigR1 or P210, immunoprecipitated with control mouse IgG or 24-11 and subjected to identical procedures (middle panel). To show that the immunoprecipitated bcr/abl specifically phosphorylated Crk on phosphotyrosine, the Crk212 mutant,20 which lacks the critical Tyr221 residue, was also used as an exogenous substrate. The α-abl mAb, 24-11, was used to immunoprecipitate the lysates of a v-Abl–expressing cell line N54 or P185-expressing cell line FL5.12 and identical assays were performed using 5 μg of either GST-Crk225 or GST-Crk212. As shown in the bottom section of panel B, Crk225 (lanes 2 and 4), but not Crk212 (lanes 1 and 3), was phosphorylated in this assay. Identical results were obtained in assays using P210 or P210Tyr177-expressing FL5.12 cells (data not shown). (C) P210 bcr/abl was in vitro translated and labeled with 35S-methionine alone or together with either the C-terminal His-tagged bcr polypeptide from P210's bcr portion or the C-terminal His-tagged Δ(1-63) bcr polypeptide from Δ(1-63) bcr/abl's Δ(1-63) bcr portion (lanes 1-3). The in vitro translated products were immunoprecipitated with an α-His mAb. The α-His mAb did not pull down P210 (lane 4), whereas it was able to pull down both the bcr and Δ(1-63) bcr polypeptides (lanes 5 and 6). P210 could only be coimmunoprecipitated with bcr polypeptides but not with the Δ(1-63) bcr polypeptide (lane 5 and 6). The correct P210 band was confirmed by immunoprecipitation with the α-abl mAb 24-11 (data not shown). (D) Grb2 fails to associate with bcr/abl mutants lacking Tyr177. Whole cell lysates of Bosc cells transfected with the indicated construct were coimmunoprecipitated with α-abl 24-11. The coimmunoprecipitated samples were immunoblotted with α-abl (upper panel) or α-grb2 antibody (middle panel). The upper panel shows that each bcr/abl protein was immunoprecipitated and the corresponding proteins are indicated on the right. The middle panel shows that only the wild-type P210 (lane 2), (1-210) bcr/abl (lane 5) and Δ(1-63) bcr/abl (lane 6) bound grb2. In the bottom panel, the whole cell lysates were immunoblotted with α-grb2 antibody as the internal control.
Oncogenic activity of bcr/abl requires its activated tyrosine kinase.18 To determine the tyrosine kinase activity of each mutant, transiently expressed bcr/abl mutants were directly immunoprecipitated from host Bosc23 cells and an in vitro immunokinase assay was performed using exogenous GST-Crk as a substrate.21,22 Each mutant exhibited elevated and approximately equal tyrosine kinase activity in vitro, as measured by GST-Crk phosphorylation (Figure 1B). The weak phosphorylation of GST-Crk in the MigR1 lysate (immunoprecipitated with 24-11) is likely due to endogenous c-abl activity (Figure 1B). The specificity of the assay was shown by using a Crk deletion mutant, Crk 212, that lacks Tyr221 and is unable to be phosphorylated by the in vitro kinase assay (Figure 1B).20 In contrast to their equivalent phosphorylation of GST-Crk, Tyr177Phe bcr/abl, (1-63) bcr/abl, and Δ(1-63) bcr/abl had a diminished autophosphorylation capacity as compared to wild-type P210 or (1-210) bcr/abl.
The ability of Δ(1-63) bcr/abl to cause elevated tyrosine kinase activity in transfected cells was surprising because a previous report suggested that this mutant was defective in both enhancing tyrosine kinase activity and oligomerization.9 To determine the oligomerization potential of Δ(1-63) bcr/abl, the Δ(1-63) bcr portion from this protein was expressed by in vitro transcription/translation (see “Materials and methods”), and subsequently used in coimmunoprecipitation experiments with wild-type P210. As shown in Figure 1C, P210 bcr/abl retains the ability to coimmunoprecipitate with the bcr portion from wild-type P210, but fails to coimmunoprecipitate with Δ(1-63) bcr. Thus, Δ(1-63) bcr/abl exhibits elevated phosphotyrosine activity in the absence of its oligomerization ability.
Tyr177 is required for grb2 binding
Two of the mutant bcr/abl fusion proteins, (1-210) bcr/abl and Δ(1-63) bcr/abl, and wild-type P210 contain Tyr177. Bcr/abl binds grb2 resulting in ras activation and fibroblast transformation.10,14 15 To assay the ability of our mutants to bind endogenous grb2, each mutant was transfected into Bosc23 cells and coimmunoprecipitations with the α-Abl antibody, 24-11, were performed (Figure 1D). As expected, only P210, (1-210) bcr/abl, and Δ(1-63) bcr/abl associated with grb2 in vivo, and both of these mutants were similar to wild-type P210 in their ability to autophosphorylate Tyr177 and bind grb2. In contrast, the mutants lacking Tyr177 did not associate with grb2 (Figure 1D).
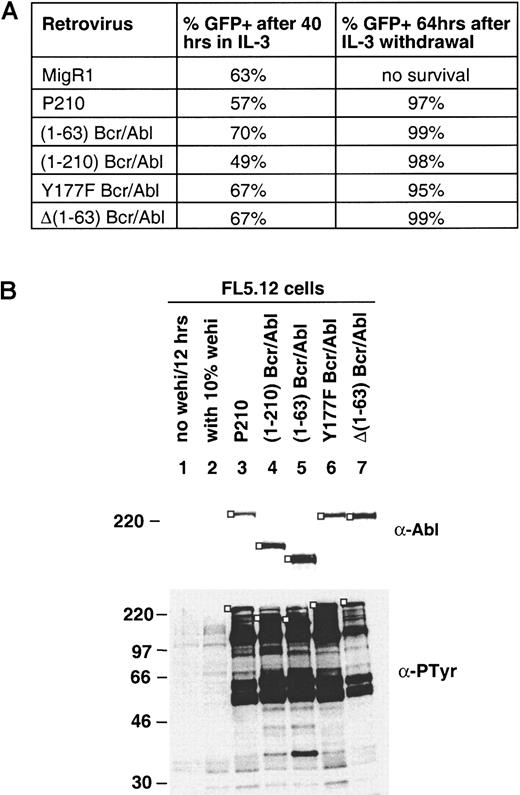
Neither the coiled-coil domain nor Tyr177 is required for factor-independent growth
We assayed the ability of each mutant to confer factor-independent growth to FL5.12 cells, which require interleukin 3 (IL-3) for survival and growth. Because the MigR1 retroviral vector expresses a bicistronic transcript containing the bcr/abl construct and GFP, transduced cells can be identified by GFP expression. FL5.12 cells were transduced by each of the 4 bcr/abl mutants so that roughly equivalent cell percentages were GFP+ by 40 hours after transduction in the presence of IL-3 (Figure 2A). IL-3 was then withdrawn, and by 64 hours later, more than 95% of cells receiving each of the bcr/abl mutants or P210 were GFP+, whereas the MigR1-transduced cells died (Figure 2A). Cell lysates were prepared and examined for bcr/abl expression and tyrosine phosphorylation (Figure 2B). Western blotting confirmed the expression of P210 and mutant proteins and showed that all of the bcr/abl-expressing cells had elevated phosphotyrosine levels compared to parental FL5.12 cells cultured in IL-3–containing media. Although difficult to draw conclusions about specific protein phosphorylation, the phosphotyrosine levels appeared similar between P210 and each mutant, with the exception of Δ(1-63) bcr/abl, which appears to exhibit slightly less phosphotyrosine activity. Nevertheless, the activity of Δ(1-63) bcr/abl is still markedly elevated relative to the negative control, and at this low level of resolution, similar sets of target proteins are phosphorylated by wild-type P210 and all 4 mutants. In parallel experiments, P210 and each of the 4 mutants maintained growth of FL5.12 cells in the absence of IL-3 and the growth rates of the different factor-independent populations were similar (data not shown). Growth factor withdrawal produced similar results after transduction of the IL-3–dependent cell lines 32D and Ba/F3 with each mutant (data not shown).
All bcr/abl mutants confer factor-independent growth to FL5.12 cells.
(A) IL-3–independent growth of FL5.12 cells expressing the indicated bcr/abl proteins. FL5.12 cells were transduced with the indicated viral supernatant. Following transduction, FL5.12 cells were grown for 40 hours and FACS analysis was performed to determine the percentage of GFP+ cells. At 48 hours after transduction, cells were deprived of WEHI-conditioned medium (source of IL-3) and maintained in IL-3–free media for an additional 64 hours at which time aliquots were prepared for FACS and protein analysis. Vector control cells (MigR1) died without IL-3. (B) Immunoblots of whole cell lysates from panel A. For comparison, lysates were prepared from parental FL5.12 cells either growing in 10% WEHI-conditioned medium (lane 2) or deprived of IL-3 for 12 hours (lane 1). For each lane, 106 cells were lysed in a final volume of 100 μL lysis buffer and 12 μL of each lysate was loaded on SDS-PAGE (6% gel for 24-11 blotting and 9% gel for PY20 blotting). The immunoblotting antibodies and size markers (kd) are indicated. In the top 2 panels the bcr/abl proteins are indicated by a ■.
All bcr/abl mutants confer factor-independent growth to FL5.12 cells.
(A) IL-3–independent growth of FL5.12 cells expressing the indicated bcr/abl proteins. FL5.12 cells were transduced with the indicated viral supernatant. Following transduction, FL5.12 cells were grown for 40 hours and FACS analysis was performed to determine the percentage of GFP+ cells. At 48 hours after transduction, cells were deprived of WEHI-conditioned medium (source of IL-3) and maintained in IL-3–free media for an additional 64 hours at which time aliquots were prepared for FACS and protein analysis. Vector control cells (MigR1) died without IL-3. (B) Immunoblots of whole cell lysates from panel A. For comparison, lysates were prepared from parental FL5.12 cells either growing in 10% WEHI-conditioned medium (lane 2) or deprived of IL-3 for 12 hours (lane 1). For each lane, 106 cells were lysed in a final volume of 100 μL lysis buffer and 12 μL of each lysate was loaded on SDS-PAGE (6% gel for 24-11 blotting and 9% gel for PY20 blotting). The immunoblotting antibodies and size markers (kd) are indicated. In the top 2 panels the bcr/abl proteins are indicated by a ■.
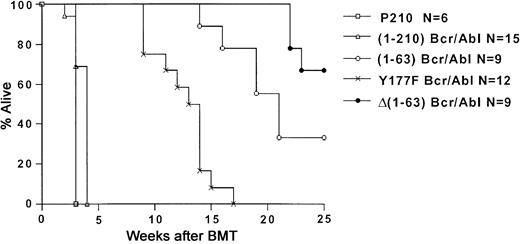
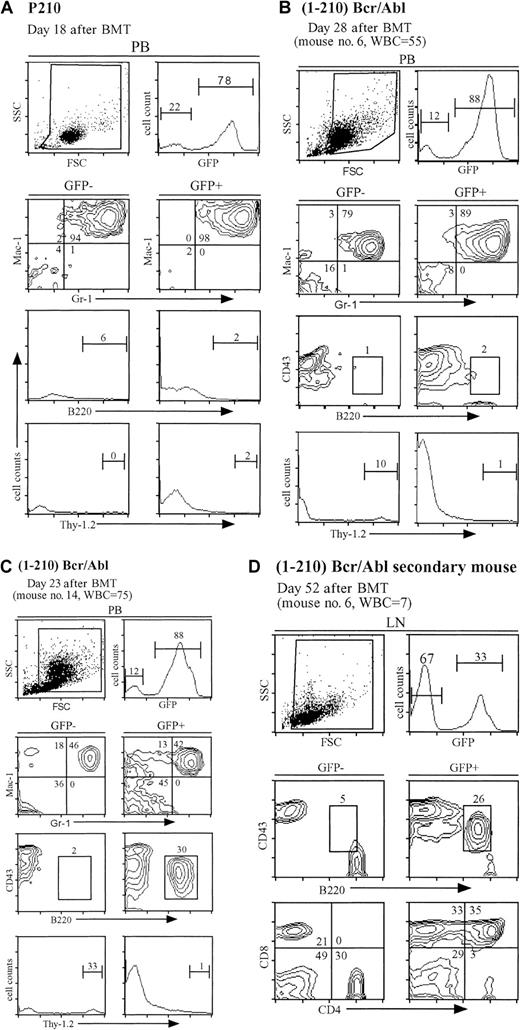
(1-210) bcr/abl induces MPD, in association with B-ALL
To determine the effects of the bcr/abl mutants in vivo, titer-matched retroviral supernatants were used to transduce 5-fluorouracil (FU)–treated BM cells that were subsequently transferred to lethally irradiated recipients. Although MigR1 mice remained healthy for at least 1 year, 100% of P210 mice developed a fatal MPD within 3 weeks after BMT (Figures3 and 4A; Table 1). Using this mouse model, we first assayed (1-210) bcr/abl that contains both the C-C domain and Tyr177. One hundred percent of mice receiving (1-210) bcr/abl developed a rapidly fatal hematopoietic disease by approximately 5 weeks after BMT (Table 1). The disease latency was significantly longer (P = .0125) than that in P210 mice (Figure 3). Similar to wild-type P210 mice, the mice became cachectic, exhibited decreased activity and poor grooming, and developed elevated white blood cell (WBC) counts, suggestive of leukemia (Table 1). The peripheral blood smears of 4 of 15 mice were predominantly comprised of mature granulocytes and very similar to wild-type P210 mice17 (and data not shown). In 11 of 15 mice receiving transplants, however, lymphoblasts were present in conjunction with an excess of granulocytes (not shown).
Kaplan-Meier–style survival curves for lethally irradiated recipients receiving BM cells transduced with the indicated bcr/abl cDNA.
The number of analyzed mice (N) is shown in the figure. Mice receiving MigR1-transduced BM cells were healthy for more than 300 days (not shown). Of the surviving Δ(1-63) bcr/abl mice, 2 mice have been followed for longer than 25 weeks (30 and 40 weeks, respectively).
Kaplan-Meier–style survival curves for lethally irradiated recipients receiving BM cells transduced with the indicated bcr/abl cDNA.
The number of analyzed mice (N) is shown in the figure. Mice receiving MigR1-transduced BM cells were healthy for more than 300 days (not shown). Of the surviving Δ(1-63) bcr/abl mice, 2 mice have been followed for longer than 25 weeks (30 and 40 weeks, respectively).
Mice receiving (1-210) bcr/abl-transduced BM cells develop MPD and B-ALL.
(A) FACS analysis of peripheral blood from a representative symptomatic wild-type P210 mouse at day 18 after BMT. (B) Some (1-210) bcr/abl mice develop MPD without evidence of B-ALL. FACS analysis of peripheral blood from a representative (1-210) bcr/abl mouse (no. 6) with MPD at day 28 after BMT. Note the similarity between this mouse and the wild-type P210 mouse in panel A. (C) The majority of (1-210) bcr/abl mice develop both MPD and B-ALL. FACS analysis of peripheral blood from a representative (1-210) bcr/abl mouse (no. 14) with both MPD and B-ALL at day 23 after BMT. Note the large population of B220+CD43+ cells in the GFP+fraction. (D) FACS analysis of lymph node tissue from the recipient of spleen cells from (1-210) bcr/abl mouse number 6. Note the abnormal populations of GFP+ immature B cells (CD43+B220+) and immature T cells (CD4+CD8+). For panels A through D, the gates used for separating the GFP− and GFP+populations are shown in the upper right panel. The lower panel pairs are divided into GFP− (left) and GFP+ (right) populations. The staining antibodies are adjacent to the axes. The percentage of cells in each population is indicated. The WBC count is measured per 106 cells/mL.
Mice receiving (1-210) bcr/abl-transduced BM cells develop MPD and B-ALL.
(A) FACS analysis of peripheral blood from a representative symptomatic wild-type P210 mouse at day 18 after BMT. (B) Some (1-210) bcr/abl mice develop MPD without evidence of B-ALL. FACS analysis of peripheral blood from a representative (1-210) bcr/abl mouse (no. 6) with MPD at day 28 after BMT. Note the similarity between this mouse and the wild-type P210 mouse in panel A. (C) The majority of (1-210) bcr/abl mice develop both MPD and B-ALL. FACS analysis of peripheral blood from a representative (1-210) bcr/abl mouse (no. 14) with both MPD and B-ALL at day 23 after BMT. Note the large population of B220+CD43+ cells in the GFP+fraction. (D) FACS analysis of lymph node tissue from the recipient of spleen cells from (1-210) bcr/abl mouse number 6. Note the abnormal populations of GFP+ immature B cells (CD43+B220+) and immature T cells (CD4+CD8+). For panels A through D, the gates used for separating the GFP− and GFP+populations are shown in the upper right panel. The lower panel pairs are divided into GFP− (left) and GFP+ (right) populations. The staining antibodies are adjacent to the axes. The percentage of cells in each population is indicated. The WBC count is measured per 106 cells/mL.
Summary of phenotypes of mice receiving transduced BM cells
| Construct . | No. of evaluable mice . | Disease before d 35 after BMT* . | Disease after d 35 after BMT . | Secondary transplantations† . |
|---|---|---|---|---|
| MigR1 (vector) | 7‡ | None | None (up to 300 d) | Not done |
| P210 | 6‡ | MPD (6/6) Latency: 17-18 d, WBC: 50-420, Spleen wt: 0.3-0.6 g | 100% disease before d 35 | Minority: MPD Majority: T-ALL |
| (1-210) bcr/abl | 15 | MPD (4/15) Latency: 18-28 d, WBC: 46-73, Spleen wt: 0.3-0.5 g B-ALL and MPD (11/15) Latency: 21-27 d, WBC: 30-179, Spleen wt: 0.3-0.6 g | 100% disease before d 35 | 1/4 mice with MPD only used for secondary transplantation, recipients developed B-ALL (latency 60-62 d) 3/11 mice with combined B-ALL and MPD used for secondary transplantation: mouse 7: B-ALL, latency 35 and 37 d mouse 10: 1/3 recipients developed combined MPD, B-ALL, and T-ALL; latency 45 d; 2/3 recipients developed combined B-ALL and T-ALL; latency 45 and 47 d mouse 11: 3/3 recipients developed combined B-ALL and T-ALL; latency 52, 60, and 62 d |
| (1-63) bcr/abl | 13 | None | T-ALL (6/9), latency 97-147 d, WBC 7-37, spleen wt: 0.1-0.3 g, all 6 mice had thymic lymphomas. No evidence of disease in 5 healthy mice killed between d 35 and d 194. One mouse had a pleural effusion at d 165 without evidence of neoplasm. | Not done |
| Δ(1-63) bcr/abl | 10 | None | T-ALL (3/10), latency 155-160 d, WBC 5-19, spleen wt 0.1-0.2 g 1 healthy mouse killed at d 97 without evidence of disease 6 mice are alive and well at 167-260 d after BMT | Not done |
| Tyr177Phe bcr/abl | 12 | None | T-ALL (11/12), latency 73-116 d, WBC 5-67, spleen wt 0.1-0.6, 3/11 mice-thymic lymphoma, 8/11 mice-abdominal lymphoma 1/12 uncertain cause of morbidity (latency 80 d, WBC 17, spleen wt 0.5) | Not done |
| Construct . | No. of evaluable mice . | Disease before d 35 after BMT* . | Disease after d 35 after BMT . | Secondary transplantations† . |
|---|---|---|---|---|
| MigR1 (vector) | 7‡ | None | None (up to 300 d) | Not done |
| P210 | 6‡ | MPD (6/6) Latency: 17-18 d, WBC: 50-420, Spleen wt: 0.3-0.6 g | 100% disease before d 35 | Minority: MPD Majority: T-ALL |
| (1-210) bcr/abl | 15 | MPD (4/15) Latency: 18-28 d, WBC: 46-73, Spleen wt: 0.3-0.5 g B-ALL and MPD (11/15) Latency: 21-27 d, WBC: 30-179, Spleen wt: 0.3-0.6 g | 100% disease before d 35 | 1/4 mice with MPD only used for secondary transplantation, recipients developed B-ALL (latency 60-62 d) 3/11 mice with combined B-ALL and MPD used for secondary transplantation: mouse 7: B-ALL, latency 35 and 37 d mouse 10: 1/3 recipients developed combined MPD, B-ALL, and T-ALL; latency 45 d; 2/3 recipients developed combined B-ALL and T-ALL; latency 45 and 47 d mouse 11: 3/3 recipients developed combined B-ALL and T-ALL; latency 52, 60, and 62 d |
| (1-63) bcr/abl | 13 | None | T-ALL (6/9), latency 97-147 d, WBC 7-37, spleen wt: 0.1-0.3 g, all 6 mice had thymic lymphomas. No evidence of disease in 5 healthy mice killed between d 35 and d 194. One mouse had a pleural effusion at d 165 without evidence of neoplasm. | Not done |
| Δ(1-63) bcr/abl | 10 | None | T-ALL (3/10), latency 155-160 d, WBC 5-19, spleen wt 0.1-0.2 g 1 healthy mouse killed at d 97 without evidence of disease 6 mice are alive and well at 167-260 d after BMT | Not done |
| Tyr177Phe bcr/abl | 12 | None | T-ALL (11/12), latency 73-116 d, WBC 5-67, spleen wt 0.1-0.6, 3/11 mice-thymic lymphoma, 8/11 mice-abdominal lymphoma 1/12 uncertain cause of morbidity (latency 80 d, WBC 17, spleen wt 0.5) | Not done |
The characteristics of the MPD are discussed in the text and by Pear et al.17 The MPD is characterized by increased WBC counts, composed primarily of mature granulocytes, hepatosplenomegaly with extensive extramedullary hematopoiesis, and tissue invasion by mature myeloid cells. All mice also developed pulmonary hemorrhage due to infiltrating myeloid cells. The B-ALL and T-ALL are described in the text. WBC count is per 106cells/mL.
1 × 106 spleen cells from primary mice were injected intravenously into each sublethally irradiated (450 R) syngeneic recipient.
We have previously analyzed 10 additional MigR1 and P210 mice with identical findings.17
Immunophenotyping was performed to further characterize the disease process in the (1-210) bcr/abl mice. The majority of circulating cells in all P210 and (1-210) bcr/abl mice were GFP+ (Figure4A,B). In 4 of 15 mice, the majority of cells were Gr-1+/Mac1+ consistent with mature granulocytes (Figure 4B). Eleven of 15 (1-210) bcr/abl mice had high numbers of both circulating Gr-1+/Mac1+ granulocytes and pre-B lymphoblasts (Figure 4C). Consistent with previous findings, the absolute numbers of circulating GFP−Gr-1+/Mac+ cells were also increased, most likely due to excess cytokine production.6,17 18
The (1-210) bcr/abl mice were killed when symptomatic. The pathologic changes in the 4 mice without circulating lymphoblasts were nearly identical to the pathologic changes observed in wild-type P210 mice and included hepatosplenomegaly and pulmonary hemorrhage with extensive infiltration of these organs and BM by mature myeloid cells. There was also extensive extramedullary hematopoiesis in the spleen and liver. Lymphadenopathy was minimal. The gross pathologic changes in the 11 mice with circulating lymphoblasts and MPD were similar, including the lack of lymphadenopathy; however, the spleen, BM, liver, and lungs of these mice showed both infiltrating mature myeloid cells and lymphoblasts (not shown).
The disease in the (1-210) bcr/abl mice suggested this construct was sufficient to induce an MPD; however, in contrast to P210, there were also circulating lymphoblasts in the great majority of mice. To further understand the disease process, cells from the spleen were transplanted into sublethally irradiated secondary recipients (Table 1). Secondary recipients of BMT from P210 mice gave rise to an MPD in the minority of secondary recipients and T-cell lymphomas in the majority (and data not shown).17 None of the secondary recipients of P210 BM or spleen cells developed B-ALL. Transfer of spleen cells from four (1-210) bcr/abl mice into secondary recipients (n = 11) gave rise to pre-B-ALL in all recipients, even though one of the 4 primary mice had no evidence of circulating B lymphoblasts (Table 1). Secondary recipients from 2 mice had both B- and T-ALL; and one secondary recipient developed the triad of B-ALL, T-ALL, and MPD (Figure 4D and Table 1). The high numbers of circulating pre-B lymphoblasts and their transplantability suggest that the circulating B lymphoblasts in the primary mice were leukemic.
Both (1-63) bcr/abl and Δ(1-63) bcr/abl mice develop T-ALL
In contrast to wild-type P210 and (1-210) bcr/abl mice that developed terminal symptoms by 35 days after BMT, all mice receiving either (1-63) bcr/abl or Δ(1-63) bcr/abl showed no evidence of disease at this time. To determine if the mutant constructs were expressed and if there were subtle pathologic changes, 4 healthy-appearing (1-63) bcr/abl mice were killed at various times between 35 and 42 days. Despite evidence that the mutant (1-63) bcr/abl construct was expressed and tyrosine phosphorylated a similar set of proteins (Figure 5A,B), none of the hallmarks of the P210 disease were present, including lack of hepatosplenomegaly, pulmonary hemorrhage, or infiltration of the organs by myeloid cells. Two abnormalities in the (1-63) bcr/abl mice were the presence of circulating GFP+ pre-B cells and an increase in the percentage of circulating granulocytes (Figure6A and not shown). However, unlike wild-type P210 and (1-210) bcr/abl mice, these changes occurred in the presence of normal WBC counts. Furthermore, neither the circulating pre-B cells nor the granulocytes expanded and they did not appear to contribute to morbidity in these mice.
Detection of bcr/abl protein expression and tyrosine phosphorylation in tissues from diseased and healthy mice.
(A) Cells (106) from each indicated mouse tissue were lysed in a final volume of 100 μL and proteins were resolved with 6% SDS-PAGE. An α-Abl Western blot was performed with mAb 24-11 to detect the expressed bcr/abl proteins. (B) Similarly prepared protein lysates were subjected to 9% SDS-PAGE and immunoblotted using the antiphosphotyrosine mAb 4G10. A longer exposure is presented at the bottom to show proteins with weak signals. The bcr/abl proteins are indicated by ■ at the right of each band. The molecular weight standards are shown in kilodaltons on the left. Note that lane 7 (1-63 bcr/abl no. 12 spleen) and lane 11 (Δ[1-63] bcr/abl no. 1 thymus) are derived from “healthy” mice. The other tissues had tumor involvement.
Detection of bcr/abl protein expression and tyrosine phosphorylation in tissues from diseased and healthy mice.
(A) Cells (106) from each indicated mouse tissue were lysed in a final volume of 100 μL and proteins were resolved with 6% SDS-PAGE. An α-Abl Western blot was performed with mAb 24-11 to detect the expressed bcr/abl proteins. (B) Similarly prepared protein lysates were subjected to 9% SDS-PAGE and immunoblotted using the antiphosphotyrosine mAb 4G10. A longer exposure is presented at the bottom to show proteins with weak signals. The bcr/abl proteins are indicated by ■ at the right of each band. The molecular weight standards are shown in kilodaltons on the left. Note that lane 7 (1-63 bcr/abl no. 12 spleen) and lane 11 (Δ[1-63] bcr/abl no. 1 thymus) are derived from “healthy” mice. The other tissues had tumor involvement.
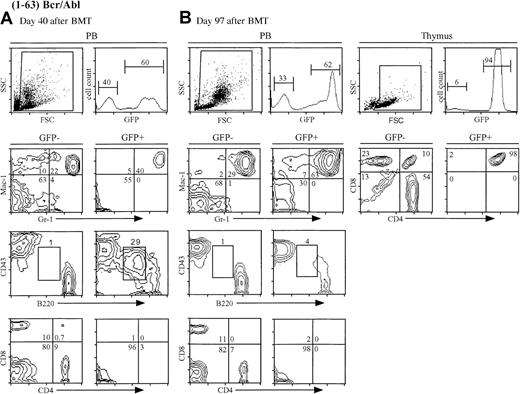
The (1-63) bcr/abl mice develop T-ALL.
(A) FACS analysis of peripheral blood from a representative healthy (1-63) bcr/abl mouse at day 40 after BMT. The WBC count was 15 × 106 cells/mL, which is similar to the MigR1 controls. Note the abnormal population of GFP+B220+CD43+cells. (B) FACS analysis of peripheral blood (center) and thymus (right) from an ill (1-63) bcr/abl mouse (no. 2). The WBC count is normal. Note the disappearance of the abnormal pre-B cells from the peripheral blood. The thymic tumor cells were GFP+CD4+CD8+.
The (1-63) bcr/abl mice develop T-ALL.
(A) FACS analysis of peripheral blood from a representative healthy (1-63) bcr/abl mouse at day 40 after BMT. The WBC count was 15 × 106 cells/mL, which is similar to the MigR1 controls. Note the abnormal population of GFP+B220+CD43+cells. (B) FACS analysis of peripheral blood (center) and thymus (right) from an ill (1-63) bcr/abl mouse (no. 2). The WBC count is normal. Note the disappearance of the abnormal pre-B cells from the peripheral blood. The thymic tumor cells were GFP+CD4+CD8+.
Between 14 and 25 weeks, 7 of 9 of the (1-63) bcr/abl mice developed lethargy and cachexia, and were killed (Table 1). All of the ill mice had normal WBC counts and lacked hepatosplenomegaly. Among them, 6 mice had an atypical immature GFP+ T-cell population within the thymus, consistent with T-ALL (Figure 6B). One of the ill-appearing mice had a pleural effusion without evidence of malignancy. The remaining 2 mice appeared healthy at 25 weeks after BMT. These results show that the C-C domain of bcr fused to abl does not induce MPD but causes a T-cell malignancy in 67% of primary recipients of BMT by 25 weeks after BMT.
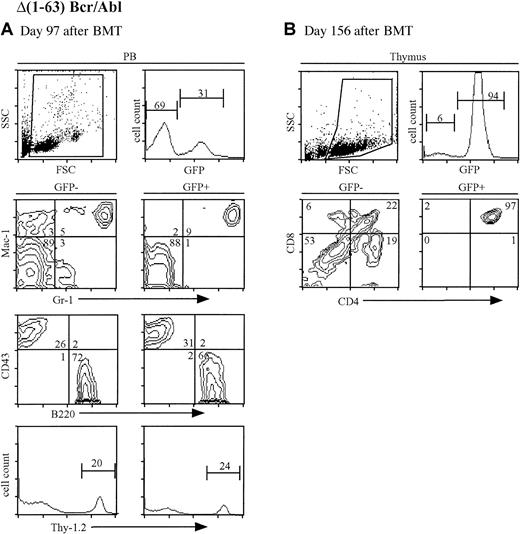
To further assess the role of the C-C domain, the Δ(1-63) bcr/abl mutant, lacking the C-C domain, was assayed in the murine model. Despite evidence of mutant protein expression in the transferred BM cells, there was no evidence of disease prior to 22 weeks after BMT (Figure 7A). At this time, 3 of 9 of the Δ(1-63) bcr/abl mice developed symptoms of lethargy and cachexia, and were killed. Similar to the (1-63) bcr/abl mice, immunophenotyping showed an atypical immature GFP+ T-cell population, consistent with T-ALL (Table 1 and Figure 7B). Six of 9 Δ(1-63) bcr/abl remained healthy at 25 weeks after BMT suggesting that this mutant has a diminished capacity to induce malignancy.
A minority of Δ(1-63) bcr/abl mice develop T-ALL.
(A) FACS analysis of peripheral blood from a representative healthy Δ(1-63) bcr/abl mouse at day 97 after BMT. The WBC count was 20 × 106 cells/mL, which is similar to the MigR1 controls. (B) FACS analysis of thymus from an ill Δ(1-63) bcr/abl mouse (no. 1). The WBC count is normal. The thymic tumor cells were GFP+CD4+CD8+.
A minority of Δ(1-63) bcr/abl mice develop T-ALL.
(A) FACS analysis of peripheral blood from a representative healthy Δ(1-63) bcr/abl mouse at day 97 after BMT. The WBC count was 20 × 106 cells/mL, which is similar to the MigR1 controls. (B) FACS analysis of thymus from an ill Δ(1-63) bcr/abl mouse (no. 1). The WBC count is normal. The thymic tumor cells were GFP+CD4+CD8+.
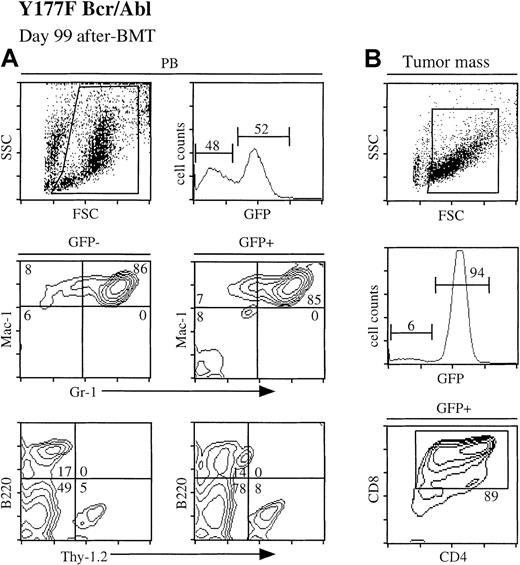
Mutation of Tyr177 inhibits MPD induction
To further analyze the role of bcr in MPD induction, we assayed the Tyr177Phe mutant, which is unable to bind grb2. Similar to the C-C mutants, these mice were healthy at the time that the wild-type P210 or (1-210) bcr/abl mice became ill. Between 9 and 20 weeks after BMT, these mice developed symptoms of cachexia and lethargy. Eleven of 12 analyzed mice developed T-cell lymphoma characterized by an expanding mass of immature CD4+CD8+GFP+ T cells arising in either the thymus or abdomen (Table 1 and Figure8). None of the 12 mice developed a disease similar to that in the wild-type P210 mice. One mouse developed splenomegaly with increased granulocytes in this organ; however, the WBC count of this mouse was normal and there was no infiltration of either the liver or lungs by GFP+ granulocytes (Table1).
Mice receiving Tyr177Phe bcr/abl-transduced BM develop T-ALL.
(A) FACS analysis of peripheral blood from Tyr177Phe bcr/abl mouse (no. 2) at day 99 after BMT. The WBC count was 11 × 106cells/mL. (B) FACS analysis of the tumor mass from the same ill Tyr177Phe bcr/abl mouse. The tumor cells were GFP+CD4+CD8+.
Mice receiving Tyr177Phe bcr/abl-transduced BM develop T-ALL.
(A) FACS analysis of peripheral blood from Tyr177Phe bcr/abl mouse (no. 2) at day 99 after BMT. The WBC count was 11 × 106cells/mL. (B) FACS analysis of the tumor mass from the same ill Tyr177Phe bcr/abl mouse. The tumor cells were GFP+CD4+CD8+.
Analysis of proviral integration and tumor clonality
Hybridization analysis showed that all mice contained intact proviral DNA (data not shown). The number of proviral integrations varied. In the wild-type P210 mice, more than 10 proviral integrations were present in some mice, whereas other mice had fewer proviral integrations (Figure 9A and not shown). Our previous results showed that the number of proviral integrations did not correlate with disease development, because some mice developing MPD had only a single proviral integrant.17 Most of the mutant mice had fewer than 5 proviral integrations. Significantly, some of the mice that were killed when healthy showed many proviral integrations (Figure 9A, lane 11) and tumors from two (1-63) bcr/abl mice showed at least 8 proviral integrations in a single clone. Analysis of the T-cell neoplasms that developed in the (1-63) bcr/abl, Δ(1-63) bcr/abl, and Tyr177Phe bcr/abl mice showed that they contained a predominant clone (Figure9B). This suggests that events in addition to expression of the mutated bcr/abl protein are necessary for tumor development in these mice.
Proviral integration and clonality of tumors.
(A) Proviral integration and (B) T-cell receptor (TCR) rearrangement. Genomic DNA (5 μg) from each indicated mouse tissue was digested with EcoRI and probed with either an IRES probe to detect proviral integration or TCR Jβ1 probe to detect TCR rearrangement status as previously described.17 35 The λHindIII molecular weight marker is shown on the left.
Proviral integration and clonality of tumors.
(A) Proviral integration and (B) T-cell receptor (TCR) rearrangement. Genomic DNA (5 μg) from each indicated mouse tissue was digested with EcoRI and probed with either an IRES probe to detect proviral integration or TCR Jβ1 probe to detect TCR rearrangement status as previously described.17 35 The λHindIII molecular weight marker is shown on the left.
Discussion
Our results demonstrate that both the NH2-terminal C-C domain and Tyr177 from bcr are required for MPD induction by the bcr/abl fusion oncoprotein. In contrast, neither the C-C domain nor Tyr177 alone is essential for bcr/abl tumorigenesis. Three mutants, (1-63) bcr/abl, Δ(1-63) bcr/abl, and Tyr177Phe bcr/abl, were capable of T-ALL induction; however, the prevalence of disease induction varied between the 3 constructs: (1-63) bcr/abl and Tyr177Phe bcr/abl induced T-ALL in the majority of mice, whereas Δ(1-63) bcr/abl induced malignancy in only a few mice during our study. The development of T-cell malignancies in mice receiving 3 of the mutant constructs is unlikely to result from transfer of wild-type Moloney virus because none of our MigR1 control mice developed T-cell malignancies, replication competent retrovirus has not been detected in our retroviral stocks, and all tumors express the appropriate bcr/abl fusion protein.
The (1-210) bcr/abl mutant, which contains both the C-C domain and Tyr177, induced an MPD with short latency in all recipients; however, most mice also had a coexistent B-ALL. There are more than 700 amino acids between Tyr177 and the carboxy-terminus of bcr in P210, which includes sites for binding to Abl SH2 and other proteins, such as 14-3-3.11 12 The emergence of B-ALL in combination with the MPD suggests that sequences within this region either promote a more rapid expansion of the myeloid population or suppress expansion of the pre-B population. The (1-63) bcr/abl mutant also elicited a transient expansion of immature B cells; however, B-ALL did not develop in these mice, suggesting that sequences between amino acids 63 and 210 are also necessary for B-ALL induction.
Both the structure of the bcr/abl fusion protein and the cells in which the fusion protein is expressed have been implicated in determining the phenotype of the murine disease.6,23 All mice receiving P230, P210, or P190 bcr/abl-transduced 5-FU–treated BM cells developed MPD6 (J.P.M., W.S.P., unpublished observations, August 1998), whereas transfer of these fusion proteins into non–5-FU–treated BM results in induction of pre-B ALL by P190 and induction of a macrophage tumor by P210 and P230.6 These results suggest that transduction of hematopoietic stem cells, which are greatly enriched in 5-FU–treated BM,24 are required for MPD induction. Because our current studies used retroviral supernatants with equivalent infectious titers and transduced 5-FU–treated BM cells, the differences in disease phenotypes that we observe are likely to result from structural differences between the fusion proteins themselves, rather than differences in the transduced target cells or differences in infectious titers.
Two different models may explain the phenotypic differences in disease caused by the different bcr/abl mutant proteins. One model proposes that the regions of bcr act in cis on the abl tyrosine kinase resulting in different levels of dysregulated tyrosine kinase activity that ultimately determines the disease phenotype. An alternative model is that proteins interacting in transinitiate signaling cascades that act in synergy with the dysregulated tyrosine kinase. Our data favor the latter hypothesis because the phosphotyrosine pattern of the different mutants is comparable to wild-type P210 both in vitro and in vivo. However, as noted in the results, it is possible that there are subtle differences in kinase activity and tyrosine phosphorylation that we have failed to discern.
The α-helical C-C is a common stabilizing motif in proteins.25 The C-C domains mediate protein-protein interactions and are required for transformation by some fusion oncoproteins, including tel/abl and retinoic acid receptor–promyelocytic leukemia (RAR-PML).26,27The NH2-terminal 63 amino acids of bcr form a C-C domain that mediates oligomerization by bcr/abl leading to a constitutively active tyrosine kinase and actin binding by the abl carboxy-terminal region.9 Previously, McWhirter et al9 showed that a bcr/abl mutant containing bcr amino acids 64-509 had very low tyrosine kinase activity and failed to convert Ba/F3 cells to IL-3–independent growth. The discrepancy between our cell line data and McWhirter et al's9 could be due to different carboxy sequences of bcr because our construct contained an additional 418 bcr amino acid. Regardless, our finding that Δ(1-63) bcr/abl effectively phosphorylates the exogenous substrate Crk and autophosphorylates Tyr177 suggests that in addition to the C-C domain, there are other domains within Bcr that facilitate the activation of the abl tyrosine kinase. Nevertheless, we cannot rule out that the C-C domain is required to reach the threshold of bcr/abl tyrosine kinase activity that is necessary for MPD induction. Alternatively, it is possible that failure of Δ(1-63) bcr/abl to elicit the MPD in vivo may result from ineffective binding of the chimeric kinase to F-actin. This possibility is supported by decreased tumorigenicity occurring in mice expressing a bcr/abl transgene lacking the abl carboxyl-terminus.28 Moreover, adhesion to fibronectin is significantly decreased in factor-independent 32D cells that express Δ(1-63) bcr/abl relative to factor independent wild-type P210-expressing 32D cells (J.A.W., W.P., manuscript in preparation). These results raise the possibility that in addition to regulating tyrosine kinase activity, the bcr amino acids 1-63 also mediate proper interaction with the cytoskeleton, which may play important roles in the induction of MPD.
In contrast to the results reported here, a recent report from Zhang et al19 found that the oligomerization domain fused to abl was sufficient to induce a MPD in mice receiving transduced BM cells. One potential explanation for the different findings is that their oligomerization domain consisted of the first 77 amino acids of bcr, whereas we used the first 63 amino acids. Their rationale for the additional 14 amino acids was that the first 77 amino acids of bcr form a globular structure. An alternative explanation is that technical differences, due to variations in transduction protocols or retroviral titers, may account for the observed phenotypic differences. It is important to note that although the CC-abl mutant of Zhang and coworkers19 induced some aspects of an MPD disease, they pointed out that this MPD differed from that induced by P210 bcr/abl in several important aspects, including (1) failure to induce a fatal disease in the majority of mice, (2) an extended latency (mean = 138 days), (3) a transient MPD phase that occurred in less than 100% of recipients, and (4) the mice did not develop pulmonary hemorrhages. Thus, both our results and those of Zhang et al19 are in agreement in showing that the C-C domain is required to cause the rapid and fatal MPD induced by wild-type P210 bcr/abl.
A direct interaction between bcr/abl and grb2 through Tyr177 is a proximal event in ras activation and is required for fibroblast transformation, but not IL-3–independent growth.10,15Another group recently reported that Tyr177Phe is defective in MPD induction, and instead induces T-cell tumors in most mice.29 In contrast to our results, they also observed B-ALL induction in some mice and some features of the MPD in mice with T-cell lymphomas.29 Differences in retroviral vectors or titers, transduction conditions, or exposure of mice to pathogens may account for the subtle differences between our results and those of Million and Van Etten.29 Moreover, the elevated WBC counts and high neutrophil counts observed in several of Million and Van Etten's29 Tyr177Phe bcr/abl mice were associated with a relatively benign condition and distinctly different from wild-type P210 bcr/abl disease, in which 100% of the mice die within 21 days from a fatal MPD. Both Million and Van Etten's29 and our results, as well as the recent report of Zhang et al,19show that the Tyr177Phe bcr/abl mutant is markedly deficient in MPD induction. Coexpression of another adapter protein, shc, rescues the ability of Tyr177Phe to transform fibroblasts15 and our model provides an opportunity to test whether shc can also rescue MPD induction. In addition, studies of the tel/platelet-derived growth factor receptor (PDGFR) fusion found in some patients with chronic myelomonocytic leukemia show that mutating specific tyrosine residues in the PDGFR portion, including those that mediate grb2 interaction, changes both the latency and phenotype of disease in a murine model.30
Our results show that the role of bcr in CML induction is not simply to activate the abl tyrosine kinase. Consistent with this observation, mice receiving v-abl–transduced BM cells failed to develop an MPD, but instead, developed B-ALL or mast cell tumors.29,31,32 It is important to note that previous descriptions of MPD induction by v-abl33,34 were most likely a reactive process because the expanded polymorphonuclear cells did not contain the bcr/abl provirus.34 Our results show that mutations within bcr itself, some of which have no effect on bcr/abl tyrosine kinase activity, have profound effects on disease phenotype, latency, and penetrance. The signaling pathways affected by the Tyr177Phe mutation are likely to be those that couple grb2 to ras signaling. In contrast, the primary contribution of the oligomerization domain may be to direct proper cytoskeletal interactions. The mechanism by which this occurs is poorly understood. Nevertheless, our results show bcr amino acids 1-63 are required for MPD induction, but dispensable for T-ALL induction. Finally, our results demonstrate the importance of using relevant assays to study bcr/abl leukemogenesis. Neither rescue of factor-dependent hematopoietic cell lines nor in vitro kinase activity revealed significant differences between wild-type P210 and the 4 bcr/abl mutant proteins. In contrast, our BMT model showed significant differences between wild-type bcr/abl and the 4 mutants. The ability to use a murine model that is both relevant to CML and provides a sensitive readout should be extremely useful in further dissecting the pathways that lead from bcr/abl to CML.
We thank Martin Carroll, Alan Gewirtz, and members of the Pear laboratory for critical reading of the manuscript. We thank Mark Lemmon, Xiaomeng Long, Ann Marie Pendergast, Bruce Mayer, and Rick Van Etten for providing reagents and protocols and members of the University of Pennsylvania mouse and flow cytometry facilities. W.S.P. also acknowledges the mentorship of David Baltimore in whose laboratory these studies were initiated.
Supported by RO1 grants from the National Institutes of Health (National Cancer Institute) and Scholar Awards from the Leukemia and Lymphoma Society to R.R. and W.S.P.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Warren S. Pear, University of Pennsylvania, 611 BRB II/III, 421 Curie Blvd, Philadelphia, PA 19104-6160; e-mail:wpear@mail.med.upenn.edu.

![Fig. 5. Detection of bcr/abl protein expression and tyrosine phosphorylation in tissues from diseased and healthy mice. / (A) Cells (106) from each indicated mouse tissue were lysed in a final volume of 100 μL and proteins were resolved with 6% SDS-PAGE. An α-Abl Western blot was performed with mAb 24-11 to detect the expressed bcr/abl proteins. (B) Similarly prepared protein lysates were subjected to 9% SDS-PAGE and immunoblotted using the antiphosphotyrosine mAb 4G10. A longer exposure is presented at the bottom to show proteins with weak signals. The bcr/abl proteins are indicated by ■ at the right of each band. The molecular weight standards are shown in kilodaltons on the left. Note that lane 7 (1-63 bcr/abl no. 12 spleen) and lane 11 (Δ[1-63] bcr/abl no. 1 thymus) are derived from “healthy” mice. The other tissues had tumor involvement.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/99/8/10.1182_blood.v99.8.2957/5/m_h80822382005.jpeg?Expires=1769113474&Signature=sEeFQDWctA8hWicM4efWZSSadadZPIuI6lkdugTmnxgCq3Kdhe-Rih7otXjW~iamyV1rHZFRVfmTydvU8CvNavsDneBoBCWdAh0L73dvdmZ8I0N1O88V~~h1WMt~K0-eEYFnos8pEewkE2PfOBW3zcmqhUrZ2p4coCNevr--vvXfev-lvjVqoOsP8bltkC0Ed70MRl3S2EnjDJTvL2F2dhSep5cFQtPfLKBDbs-34ZhUwuBeoxg~oSAMMzXFfZNAhMyXvuSg25DWNFYBhoD-kYXU09eyQ23oVukUqlXHzJ427t1XZKS~iaaEFaL9cZ1VFTTlPoFyFbusYNJgRsh6bQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal