Abstract
Drug therapy for acute myeloid leukemia (AML) is finally undergoing major changes in 2017. This is due to the US Food and Drug Administration’s approval of several new, targeted agents (midostaurin, enasidenib, and gemtuzumab ozogamicin). Paired with the recent approval of a novel liposomal formulation of daunorubicin/cytarabine (CPX-351/Vyxeos), the standard of care is changing rapidly in AML for subgroups. This review will focus on currently approved agents and promising novel agents in development and will highlight controversial areas in targeted treatment.
Introduction
After decades of stagnation in the antileukemic armamentarium for acute myeloid leukemia (AML), the clinical options are changing quickly with exciting therapeutic developments. In April 2017, the US Food and Drug Administration (FDA) approved midostaurin for FLT3-mutated AML. Midostaurin is the first tyrosine kinase inhibitor (TKI) approved for AML as well as the first drug approved in a mutation-specific, non–acute promyelocytic leukemia (APL) subset. Additionally, the FDA provided accelerated approval of the IDH2 inhibitor enasidenib (AG-221) in August 2017. This approval was based on promising response rates and survival from a recently-completed phase 2 study in an IDH2 mutation–selected population. It is hoped that soon IDH1 inhibitors will also be available because the available clinical data with these drugs is similarly encouraging. Just days after approving enasidenib, the FDA approved the novel liposomal daunorubicin/cytarabine formulation CPX-351 (Vyxeos) for therapy- and myelodysplastic syndrome (MDS)-related AML. Finally, the previously approved but subsequently withdrawn antibody-drug conjugate (ADC) gemtuzumab ozogamicin (GO) was given full approval for CD33-positive AML in September. Taken together, 2017 has seen the approval of 4 novel AML drugs, only one of which is a traditional cytotoxic agent.
Gone are the days where frontline intensive chemotherapy for AML was “one-size-fits-all.” The winds of change are finally filling the sails for novel AML therapy. and it is time to set a course toward new treatment paradigms. This is a dramatic change from the past, where decades of trials left us treatment approaches that were neither targeted nor fundamentally altered for decades. What are these new drugs? Which patients should consider them? And, looking to the future, how might we design new therapeutic approaches to improve outcomes and increase cure rates?
Types of targeted agents
Targeted therapy in AML can be divided into 3 groups. First, mutation-targeted agents act on oncogenic effectors of recurrent AML-associated mutations. Examples of such agents include FLT3 and IDH inhibitors, at least when tested in FLT3- and IDH-mutated patients, respectively. Second, nonmutation-targeted novel agents disrupt key metabolic or cell maintenance pathways without directly damaging DNA or its repair. Examples include epigenetic modifiers and agents that directly target apoptosis. A final group is comprised of the targeted delivery of cytotoxic agents, such as ADCs. Although there has also been significant development of immunotherapeutics, both as cellular therapies and antibody-based immune stimulating strategies, these will not be formally discussed in this review. A selected list of active clinical trials of investigational drugs discussed in this review and related agents is provided in Table 1. Please note that not all listed agents could be discussed in this review out of space concerns.
Mutation targeted agents: FLT3 inhibitors
FLT3 is a cytokine receptor that is expressed almost exclusively in hematopoietic tissues. In addition to playing key roles in early myeloid and lymphoid stem and progenitor cell growth and survival, FLT3 signaling regulates dendritic cell maturation and maintains homeostasis of regulatory T cells. In AML, recurrent mutations occur commonly as FLT3 internal tandem duplications (FLT3-ITDs) in ∼25% of patients. They also occur as point mutations in the tyrosine kinase activation loop (FLT3-TKD; typically at codon D835) in another 5% to 10% of patients. Each mutation can be shown in vitro to constitutively activate the kinase and promote growth, survival, and antiapoptotic signaling through downstream targets, such as MAPK, PI3K/AKT/mTOR, and STAT5. Studies of clonal architecture suggest that FLT3 mutations occur late in leukemogenesis. Accordingly, the allele burden for FLT3 is quite variable, and sometimes FLT3 mutations occur only in a small subclone. In vitro, FLT3 TKIs are cytotoxic to cell lines and AML patient samples bearing FLT3 mutations. Drugs targeting FLT3 first entered clinical trials in 2002.
The first drugs tested as FLT3 TKIs included midostaurin (PKC412), lestaurtinib (CEP-701), and sorafenib. These oral agents all share relatively good in vitro inhibition of FLT3, but rather poor kinase selectivity and complicated pharmacokinetic properties.1 When initially studied in the clinic, it was found that these drugs all bound plasma proteins and/or acute-phase reactant proteins tightly, leading to low and variable steady-state free drug concentrations. Correlative studies from these early trials showed minimal control of leukocytosis when patients achieved either transient or submaximal FLT3 kinase inhibition.2,3 Therefore, a major challenge with the first generation of FLT3 inhibitors was to define clinically active, tolerable doses that could inhibit kinase targets potently throughout the entire dosing interval.
Soon thereafter, a second generation of FLT3 inhibitors emerged with higher potency, markedly more selective kinase inhibition, and improved pharmacokinetic properties. In phase 1 testing, quizartinib (AC220), even at very low doses, abrogated FLT3 signaling in vivo.4 Two concurrently enrolled phase 2 studies of quizartinib in relapsed/refractory AML patients showed enriched responses among patients with FLT3-ITD (who made up two-thirds of enrolled patients in each cohort).5,6 Notably, the elimination of circulating blasts among responders on these trials was paired with marked reductions in marrow blasts to <5%. Such marrow responses occurred in ∼50% of FLT3-ITD–positive patients, and their frequency appeared to be independent of the FLT3-ITD allele burden.5,6
Although quizartinib side effects were generally mild, QT interval prolongation at initially tested doses (90-135 mg/day) occurred commonly and necessitated further dose refinement. Reassuringly, subsequent trials of lower quizartinib doses (ie, 30-60 mg/day) showed comparable response rates, but QT prolongation occurred infrequently.7 With this lower dose range, quizartinib has entered phase 3 testing. Enrollment in a randomized comparison of quizartinib monotherapy vs the investigator’s choice of 3 salvage chemotherapy regimens for first relapse of FLT3-ITD–positive AML was completed in 2017 (clinicaltirals.gov identifier NCT02039726). As well, a phase 3, placebo-controlled trial will examine quizartinib added to infusional cytarabine plus anthracycline (7 + 3) and postremission high-dose cytarabine for newly diagnosed patients with FLT3-ITD–positive AML (identifier NCT02668653).
Of note, nearly all patients with marrow responses to single-agent quizartinib, regardless of dose, had ongoing cytopenias. Indeed, formal International Working Group–defined complete remission (CR) or even complete remission with incomplete platelet recovery (CRp) responses were rare. Instead, nearly all “deep” marrow responses were termed modified complete remission with incomplete blood count recovery (CRi) because transfusion independence was not required, and patients could have both incomplete neutrophil and platelet recovery. Interestingly, a substantial fraction of these patients’ marrows were hypercellular during response and showed persistently high myeloid:erythroid ratios.8 Tracking of FLT3-ITD:wild-type (WT) allelic ratios during therapy confirmed that the marrow’s allele burden for FLT3-ITD frequently did not fall, even when blasts went from >95% of the bone marrow to <5%.8 Unlike preclinical in vitro studies where FLT3 inhibitors generally caused cytotoxicity of blasts in culture, in many patients, the primary clinical effect in the marrow was induction of terminal granulocytic differentiation.9 This was largely analogous to the clinical effects seen with all-trans retinoic acid (ATRA) in treating APL. Indeed, a surge of neutrophils often arose on the second month of quizartinib therapy, and these neutrophils could be shown during treatment response, but not prior to quizartinib therapy, to be FLT3-ITD–positive. Other symptoms associated with granulocytic differentiation of leukemic blasts in response to FLT3 inhibition have included Sweet’s syndrome–like rashes, fevers, fluid retention, and/or pulmonary abnormalities.9-11 Depending on symptom severity, corticosteroids have been used to control what appears to be a differentiation syndrome.
Another observation among relapsed/refractory patients treated with quizartinib as a single agent was the rapid transition from deep marrow response to resistant leukemia, which, on sequencing of the FLT3 kinase domain, often showed treatment emergence of new FLT3-TKD mutations, particularly D835 substitutions or F691L.12 In vitro testing of the same mutations generated in cell lines was indeed associated with impaired inhibition of FLT3 kinase and resistance to cytotoxic effects of quizartinib. Indeed, 8 of 8 patients with deep marrow responses to quizartinib and then loss of response were found to harbor 1 of these 2 mutations; in some patients, polyclonal relapse with multiple independent FLT3-TKD sequences could be identified.12 These finding are highly analogous to the TKI resistance seen in other diseases, notably chronic myeloid leukemia, and some of the affected residues on FLT3 were structurally analogous to the well-characterized resistance mutation in BCR-ABL1. Although the findings validated that the mechanism of response to quizartinib was due to FLT3 inhibition, they also pointed to a need to develop drugs that target both FLT3-ITD and common TKD resistance mutations as a method to circumvent resistance and maximize the efficacy of FLT3 inhibition.13,14
Two such agents quickly followed, each showing in vitro activity against both FLT3-ITD and FLT3-D835, the most common TKD mutation conferring resistance to quizartinib. First to enter trials was crenolanib, which was quickly followed by gilteritinib (ASP2215). The drugs are each highly selective for FLT3, well tolerated clinically, and show minimal potential for QT interval prolongation. They largely differ in terms of their pharmacokinetics, because crenolanib must be taken 3 times a day vs gilteritinib, which is taken once a day. Each of these drugs showed potent in vivo FLT3 inhibition at recommended phase 2 doses and substantial efficacy in patients with relapsed FLT3-ITD–positive AML. Notably, responders included patients who had been resistant to other FLT3 inhibitors, such as sorafenib and quizartinib, and patients with both FLT3-ITD and D835 mutations.15,16 Indeed, the response rate to gilteritinib for patients with FLT3-ITD alone and those with both FLT3-ITD and D835 was identical. Unlike quizartinib and even crenolanib, traditional International Working Group responses of CR or CRp to gilteritinib occurred in 18% of FLT3-ITD–positive patients, with an additional 26% achieving CRi responses. Although differentiation of leukemic blasts also occurred during gilteritinib therapy, serial next-generation sequencing (NGS) quantitation of the FLT3-ITD:WT allele ratio of 80 FLT3-ITD–positive patients treated with gilteritinib identified that approximately one-quarter of patients showed deep reductions in marrow FLT3-ITD–positive allele burden during response to levels well below that capable of polymerase chain reaction (PCR) detection.17 Reduction of the FLT3-ITD–positive clone size to this degree was associated with substantially longer survival than that of patients without reduction in FLT3-ITD–positive allele burden (median of 14 vs 6.5 months, respectively; P = .001).17 With regard to the mechanisms of resistance, data on gilteritinib resistance are forthcoming. Paired exome sequencing of crenolanib-treated patients who ultimately relapsed did not show new mutations in FLT3. This provides indirect proof of principle that the current generation of FLT3 inhibitors can suppress FLT3 mutation–mediated resistance in relapsed/refractory populations.18 Phase 3 testing of gilteritinib and crenolanib has begun (identifiers NCT02421939, NCT02997202, NCT02752035, and NCT02298166).
With all the advances in FLT3 inhibition in the past 15 years, one of the most exciting recent developments comes from its oldest drug. Indeed, after development of midostaurin as a single agent was scrapped, trials began to study it in combination with intensive chemotherapy. This led to a successful dose-optimization study that examined the feasibility of adding midostaurin to frontline therapy of FLT3 mutation–positive patients. The C10603/RATIFY study was a herculean, worldwide effort to screen >3200 newly diagnosed AML patients aged 18 to 60 years to identify ∼700 FLT3 mutation–positive patients for targeted study. The regimen was designed to treat enrolled patients with a uniform induction and consolidation regimen (daunorubicin plus cytarabine induction × 1-2 cycles followed by 4 courses of high-dose cytarabine consolidation) and randomly assign these patients to 14 days of oral midostaurin vs placebo, with each IV chemotherapy cycle followed by a year of midostaurin or placebo maintenance as monotherapy. The C10603/RATIFY trial found that midostaurin therapy was associated with a 22% reduction in the hazard ratio for death, confirming that midostaurin provided a statistically significant improvement in overall survival (OS) when added to standard induction and consolidation therapy.19 Notably, the event-free and OS curves separated relatively early in therapy and remained parallel across many years of follow-up, leading to an absolute improvement in the estimated OS rate at 4 years of 7% (51.4% vs 44.3% for midostaurin and placebo, respectively).19 Importantly, the survival benefit extended to both FLT3-ITD– and TKD–positive populations, was not altered by FLT3-ITD allele burden, and was not affected by censoring for transplant. Similarly, although a substantial number of patients on this trial received allogeneic transplant, the survival rate of patients transplanted in first complete remission (CR1) after midostaurin therapy was better than those transplanted in CR1 after placebo, suggesting that the quality of disease control may have been better among patients transplanted following midostaurin therapy. It is tempting to assume that this transplant outcome reflects a difference in minimal residual disease (MRD) negativity among patients treated with midostaurin, although this was not directly measured. Toxicity was largely overlapping in the study’s 2 arms except for a minor increase in rashes among midostaurin-treated patients. These data led to FDA approval of midostaurin in April 2017 as the first clinically available TKI for FLT3 mutation–positive AML.20
The future looks bright for FLT3 inhibitors. Clearly the next step will be to determine whether more potent/selective agents provide additional benefit beyond that of midostaurin when added to standard frontline approaches. Although head-to-head trials of newer-generation FLT3 inhibitors against midostaurin as the adjunct to cytarabine/daunorubicin have not yet begun, they are the next critical question to answer in the field.
Another key question relates to the role of FLT3 inhibitors in maintenance therapy. Small studies show quite low relapse rates for patients who received FLT3-TKIs after CR1 allogeneic transplant.21 Because FLT3-ITD is an independent risk factor for relapse posttransplant,22 this suggests that adding a FLT3-TKI as maintenance therapy posttransplant could improve survival. This approach is analogous to posttransplant TKI maintenance for BCR-ABL1–positive leukemias. To address this question, a randomized, placebo-controlled study of posttransplant gilteritinib maintenance has been initiated through the Blood and Marrow Transplant Clinical Trials Network (identify NCT02997202).
Whether an FLT3 inhibitor as maintenance therapy post–chemotherapy consolidation improves survival is similarly unknown. Although C10603/RATIFY did include postconsolidation maintenance (but not posttransplant maintenance), only 205 subjects actually proceeded to this treatment, making it challenging to show whether maintenance therapy added additional value. As well, the early separation of survival curves suggests that the benefits of midostaurin largely occurred early in therapy. These limitations presumably explain why maintenance therapy was not included on the midostaurin label. However, this should not be interpreted as proof of no benefit to maintenance therapy without adequately powered, randomized data. Studies to specifically examine FLT3 inhibitors as postconsolidation maintenance agents are important, and such trials have been initiated (identifier NCT02927262).
Mutation-targeted agents: IDH inhibitors
Isocitrate dehydrogenase is a ubiquitously expressed enzyme that catalyzes the oxidative decarboxylation of isocitrate to α-ketoglutarate. Whole-genome sequencing first identified IDH1 mutations in AML in 2009.23 Subsequent work found arginine substitution in specific residues of either IDH1 or IDH2 were indeed recurrent in AML and strongly associated with normal karyotype.23,24 Further studies identified the same IDH mutations in both MDS and myeloproliferative neoplasms and even occasionally among otherwise healthy older individuals with clonal hematopoiesis of indeterminate prognosis.25 These findings, along with studies of allele frequencies and clonal architecture, suggest that IDH mutations occur early in leukemogenesis and act to perturb DNA and histone methylation in hematopoietic stem cells through the production of an abnormal metabolite, 2-hydroxyglutarate (2HG).24,26 In AML, IDH1 and IDH2 mutations are all but mutually exclusive with each other and additionally with mutations in either TET2 or WT1.
Enasidenib (AG-221) is a covalent inhibitor of R140Q- and R172K-mutated IDH2 and has emerged as the first IDH mutation–specific inhibitor.27 Of note, enasidenib induced terminal differentiation of leukemic blasts into neutrophils in vivo during these experiments. Clinical testing of enasidenib has been completed in a first-in-human phase 1/2 trial that enrolled relapsed/refractory AML or MDS patients as well as a small number of untreated AML patients who were not candidates for more intensive therapy.28 Enasidenib was found to be generally well tolerated across a wide dose range. Nausea, diarrhea, fatigue, anorexia, and hyperbilirubinemia without hepatic transaminase elevation were identified as its most common treatment-emergent toxicities. 2HG reduction, a pharmacodynamic readout of IDH inhibition, occurred at dose levels well below the highest tested dose, and no maximum tolerated dose was determined. The CR rate among 159 relapsed/refractory AML patients treated with enasidenib was 19% with another 1% showing CRp.28 Protocol-defined responses occurred in a total of 37% of patients, and the median duration of treatment responses was 6.9 months. A reduction in mutant IDH allele frequency was seen in a subset of responding patients. However, the majority did not show a significant reduction in IDH2 mutation burden because the primary mechanism of response appears to be induction of terminal differentiation.29 As well, ∼12% of enasidenib-treated patients experienced a differentiation syndrome variably characterized by fever, dyspnea/lung infiltrates, pleural effusions, leukocytosis, and kidney injury.30 Similar to the management of APL differentiation syndrome, systemic corticosteroids led to the resolution of these symptoms.
With regard to predictors of response, it is notable that a subset of enasidenib-treated patients had relatively low IDH mutation burden at study entry. This indicates a subclonal IDH mutation arising as a secondary mutation rather than an initiating mutation. The IDH2 mutation allele burden at study entry had no effect on response rate.29 Similarly, reduction in 2HG concentration was profound and nearly uniform across the trial. Accordingly, a reduction in 2HG did not predict response to enasidenib. Certain co-mutations, specifically N- or K-ras, but also a number of mutations that activate hematopoietic cytokine signal transduction (eg, PTPN11, NF1, and FLT3), were associated with relatively low response rates.29 Patients with high numbers of co-mutations, generally a marker for clonal diversity, also had relatively low responses to enasidenib.
Notably, although 45% of enasidenib-treated patients experienced stable disease as their best response, ∼30% of these patients had improvements in blood counts during this time; stable disease responses in some patients were associated with reductions in AML-associated fatigue or constitutional symptoms. Notably, however, some patients responding to enasidenib experienced a robust differentiation syndrome not unlike that seen with ATRA therapy of APL, including leukocytosis, fever, pulmonary infiltrates, and pleuropericardial effusions. Steroids have been used to manage this complication, which is important to recognize when using this class of agents. As noted above, enasidenib therapy was approved for patients with relapsed or refractory AML with IDH2 mutations.
Several IDH1 inhibitors are also under development, including ivosidenib (AG-120), IDH305, BAY-1436032, and FT-2102. Of these, ivosidenib is the furthest along in development and, like enasidenib, has shown favorable toxicity in an ongoing phase 1/2 study exclusively enrolling IDH1-mutated patients. A high rate of protocol-defined responses has been seen in this trial from interim reports.31 As occurs with enasidenib, terminal differentiation of leukemic blasts to ivosidenib has also been observed, including a differentiation syndrome in some patients. In cohort expansion, response rates to ivosidenib looked similar to that of AML patients treated with enasidenib, with a 16% CR rate in relapsed/refractory AML and an additional 13% of patients with CRp or CRi.31 Serial NGS of these responding patients showed that approximately one-third of patients experiencing CR did so by elimination of the IDH1-mutated clone. Although the number of patients experiencing mutation clearance was small (7 of 78 patients treated) 4 of 7 patients with mutational clearance remained on the study drug for over a year.31
Observations from IDH and FLT3 inhibitor trials suggest common features of response to these targeted agents. First, although disease stabilization is widespread, only a small number of patients show traditional chemotherapy response metrics. In fact, clearance of the clones bearing the drug targets occurs in a small minority of treated patients, even with the most potent inhibitors. Second, clinical response to either IDH or FLT3 inhibitors is often characterized by terminal differentiation of the leukemic clone, suggesting that each class of drugs relieves maturational arrest that is attributable to the respective mutations. These effects are similar to targeted therapy of APL. ATRA alone can induce differentiation and CRs, but, as a single agent, ATRA does not cure leukemia, and substantial work has been focused on optimizing agents to be combined with a highly mutation-targeted approach. Now that we have validated IDH and FLT3 inhibitors, it is time to begin optimizing combination strategies. Some of the most promising agents have turned out to be drugs that deliver non–mutation-targeted cytotoxics with lower extramedullary side effects.
Non–mutation-targeted novel agents
The biology of AML is heavily studied, and a large number of strategies have been tried to disrupt its key biologic processes. In 2017, the most promising agents for AML include drugs that target epigenetic regulators and apoptosis machinery.
BCL2 antagonism
Apoptosis regulation at the outer mitochondrial membrane is a complex process regulated by interactions between pro- and antiapoptotic BCL2 family proteins (reviewed in Gilles and Kuwana32 and Cory et al33 ). Following cellular stresses, such as DNA damage, growth factor deprivation, or oncogene activation, a diverse number of BH3-only proteins are released into the cytosol. These proteins localize to the outer mitochondrial membrane and promote apoptosis by interacting with both pro- and antiapoptotic BCL2 family members. BH3-only proteins ultimately activate and promote oligomerization of the proapoptotic BCL2 family proteins BAX and BAK. BAX and BAK oligomers insert into the mitochondrial outer membrane and form porous channels that cause mitochondrial outer membrane permeabilization (MOMP). MOMP results in the release of cytochrome c, which irreversibly commits the cell to apoptosis. A hallmark of cancer is the deregulation of apoptosis. In many hematologic malignancies, including AML, a common mechanism through which antiapoptosis occurs is the overexpression of the BCL2 protein.34
The anti-apoptotic BCL2 family contains 4 proteins: BCL2, BCL-XL, BCL-w, and MCL-1. The BCL2 protein normally interacts with and negatively regulates the function of BAX and BAK. However, BCL2 can also interact with BH3-only proteins, such as BID or BIM. In the context of BCL2 overexpression, proapoptotic BH3-only proteins that are released following cell stress (eg, chemotherapy-induced DNA damage) become sequestered by BCL2 protein. Sequestration of BH3-only proteins makes them unable to activate BAX and BAK to initiate MOMP. Accordingly, BCL2 overexpression disrupts normal regulation of the mitochondrial membrane, antagonizes apoptosis, and contributes to chemotherapy resistance.
Early efforts to target BCL2 therapeutically focused on reducing BCL2 expression via antisense (eg, oblimersen), and studies did suggest clinical activity of the approach in both lymphoid malignancies and AML.35,36 More recently, drugs have been designed to antagonize BCL2 function. These drugs act by mimicking BH3 domains and directly binding to BCL2 protein in a BH3 interacting groove. When these drugs bind BCL2, they displace the proapoptotic BH3 domain proteins, which then activate BAX and BAK and trigger MOMP and apoptosis.37 Overall, BH3 mimetic agents appear most successful at generating antitumor effects in patients with hematologic malignancies.
The earliest developed BH3 mimetics included obatoclax and navitoclax. These each showed clinical activity in lymphoid malignancies like chronic lymphocytic leukemia (CLL), but were limited by significant side effects, such as neurologic toxicity or reduced platelet life span and thrombocytopenia.33 Because these toxicities were thought to be due to the inhibition of multiple BCL2 family members (particularly BCL-XL), more selective and potent BCL2 antagonists were sought. Chief among the highly BCL2-selective BH3 mimetic agents is the oral agent venetoclax.
Venetoclax not only has both greater potency against BCL2 than previous drugs, but it also does not show significant BCL-XL antagonism.38 Although cytopenias (particularly neutropenia) occur commonly during therapy, these typically are transient, and ongoing thrombocytopenia is uncommon. Along with ibrutinib and idelalisib, venetoclax has been transformative in heralding a new era of CLL therapy that largely avoids traditional cytotoxic agents. Close monitoring for tumor lysis syndrome is necessary in CLL therapy because some patients show exquisite sensitivity to venetoclax, and this results in rapid, massive apoptosis.
Venetoclax has also undergone development in AML. Single-agent activity of venetoclax on a 32-patient, single-arm, phase 2 study in relapsed/refractory AML was modest, with only 19% of patients achieving CR/CRi, and the median duration of remission was >2 months.39 Still, it was notable that 6 of the 12 IDH-mutated patients had objective responses, including 4 with CR/CRi. Although the numbers are small, they seem to confirm the results of preclinical studies that demonstrate that 2HG-mediated inhibition of cytochrome C oxidase causes both BCL2 upregulation and dependence in IDH-mutated leukemia cells.40
Recently, exciting data have been presented from studies combining venetoclax with either low-dose cytarabine (LDAC) or hypomethylating agents (HMAs) in previously untreated older AML patients who were not eligible for intensive induction chemotherapy. These multicenter, single-arm studies used a similar design, where venetoclax was dose escalated in cohorts and added to a standard dose of cytarabine in 1 study and either decitabine or 5-azacitidine in the other.41,42 The 2 trials showed largely overlapping and remarkably high response rates among patients treated with the combination regimen, with CR or CRi occurring in 33 of 61 (54%) of the cytarabine patients, and 24 of 34 (71%) of the HMA combination trial patients.41,42 Multiple expansion cohorts testing several doses and schedules of venetoclax and either decitabine or azacitidine were recently presented and confirm a high response rate from a larger sample size (CR/Cri = 68/100 patients, 68%).43 Importantly, the response rates for combination studies of venetoclax and either LDAC or HMAs were appreciably higher than published literature for the standard chemotherapy as single agents. As well, responses occurred even in patients with a high-risk karyotype and were rapid, often within the first cycle of therapy. This is quite distinct because, typically, LDAC or HMAs require multiple cycles to achieve maximal treatment response, and CRs are uncommon.
The toxicity of venetoclax plus HMAs or LDAC has included nausea, diarrhea, constipation, neutropenia. and neutropenic fevers/infections. Tumor lysis prophylaxis was given to all patients, but no cases of clinical tumor lysis syndrome were observed in AML trials. The 30-day mortality rate of 12% from the venetoclax plus HMA study appears somewhat higher than that seen when HMAs were used as single agents, and this will need to be watched closely in randomized trials.43 However, short-term follow-up suggests survival rates with combination therapy that appear at least as good as those of cytarabine or HMAs alone. These early results are quite encouraging, and randomized trials of venetoclax combinations with either LDAC or HMAs have been initiated (identifiers NCT02993523 and NCT03069352). Overall, venetoclax is among the most exciting and promising new agents to be added to low-intensity AML therapy.
If phase 3 testing shows a clinical benefit of venetoclax combined with low-dose chemotherapy or HMAs, then this combination would not only redefine therapeutic approaches to AML in older patients unfit for intensive chemotherapy, but would also likely prompt expanded testing of the venetoclax combinations in younger patients treated with curative intent. Doubtless, venetoclax will also be tested with other targeted agents, such as FLT3 inhibitors, to see if the combination enhances the ability to clear the FLT3-mutated clone rather than merely induce its differentiation.
Drugs targeting epigenetics
Some of the most commonly mutated genes in AML regulate the methylation and/or hydroxymethylation of cytosine bases in DNA. These include DNMT3A, WT1, IDH1/2, and TET2 and together are observed in ∼50% of AML cases.44 Mutations in genes that alter transcription through histone modifications, such as ASXL1, EZH2, or KMT2A (formerly known as MLL) are also frequently seen, particularly in AML that follows antecedent MDS or prior chemotherapy.44 Because epigenetic regulators are so often the targets of recurrent mutations in AML, there has been great interest in drugs that target epigenetic modifications. That few of the recurrently mutated genes themselves are enzymes that are activated by mutations makes this a challenging prospect. Still, many novel epigenetic-modifying drugs can be considered mechanism targeted rather than mutation specific, and, so far, most have had modest toxicity.
Included in this list are the agents decitabine and 5-azacitidine, which are standard therapy for MDS and also show significant clinical activity in AML. Each of these agents inhibits DNA methyltransferase 1 and shows clinical activity that is not predicted by the presence of particular mutations that alter DNA methylation. Although not proven to be superior to intensive cytotoxic approaches, as single agents, these drugs provide very tolerable and often effective therapy of AML.45 DNA methyltransferase 1 inhibitors (ie, HMAs) have thus emerged as a backbone for combination strategies in older patients and those considered at high risk for treatment failure and/or unacceptable toxicity with standard intensive approaches due to adverse genetics or comorbidity.
Novel HMAs
Guadecitabine (SGI-110) is a dinucleotide of decitabine and deoxyguanosine that shows similar potency but improved pharmacokinetic properties compared with decitabine. Specifically, guadecitabine is a prodrug of decitabine, and the generation of this compound represents its major mechanism of action. Unlike decitabine, however, guadecitabine is resistant to cytidine deaminase degradation, which results in a prolonged half-life. Clinical studies of guadecitabine show tolerability and clinical activity at a number of drug doses and administration schedules.46 Correlative studies from phase 1 testing showed the generation of hypomethylated DNA in target genes (eg, LINE1) across several drug doses and administration schedules.46 Thus, a number of doses and schedules have been studied to identify the optimal biologic dosing such that the prolonged half-life generates prolonged epigenetic effects rather than prolonged cytotoxicity. Indeed, the recommended phase 2 and 3 doses and regimens were determined from guadecitabine's pharmacodynamic activity and are well below the maximum tolerated doses of this agent.
The fficacy of guadecitabine at either 60 or 90 mg/m2 per day for 5 to 10 treatment days every 4 weeks was seen in 2 phase 2 studies. The first was a study of 103 patients with relapsed/refractory AML, nearly all of whom had had prior intensive chemotherapy. In this study, 23% of patients had CR, CRp, or CRi to guadecitabine, the median survival was 6.6 months, and 19% of patients were alive at 2 years.47 A second trial in 51 untreated AML patients who were ineligible for intensive induction showed a 37% CR rate, with an additional 20% experiencing CRp or CRi, and a median survival of 10.5 months.48 Like other HMAs, responses to guadecitabine occur slowly, with most happening after 3 cycles, and 20% of remissions occurring after 6 cycles. The toxicity of the drug primarily consisted of cytopenias and infections related to neutropenia. A phase 3 trial of guadecitabine compared with the investigator’s choice of chemotherapy for relapsed/refractory AML has been initiated (identifier NCT02920008).
A final exciting novel HMA to discuss is CC-486, which is an oral formulation of 5-azacitidine that has undergone extensive testing in MDS and a smaller number of AML patients. Although there are limited data for the clinical activity of CC-486 in AML, it is hoped that, if equivalence to parenteral azacitidine can be shown in the MDS realm, oral azacitidine might emerge as a drug of choice for combination regimens in AML. A phase 1/2 trial of CC-486 as maintenance therapy after allogeneic transplant for AML has been completed, and a phase 3 study of this drug as maintenance therapy after completion of intensive nontransplant chemotherapy is ongoing (identifier NCT01757535).
BET inhibitors, LSD1 inhibitors, and DOT1L inhibitors
Many promising novel agents in development for AML target niche areas of leukemogenesis. These include the epigenetic regulators bromodomain and extraterminal (BET) proteins, DOT1L, and LSD1.
BET family bromodomain proteins bind acetylated lysine residues on histones to alter transcription. The rationale for BET inhibitors as cancer therapeutics originally followed the discovery that MYC expression was regulated by the bromodomain protein, BRD4, and was modulated by the small molecule BET inhibitor, JQ1.49,50 Preclinical testing of JQ1 as well as short hairpins targeting BRD4 showed that AML cell lines, primary AML samples, and an MLL-AF9–containing AML murine model system showed growth arrest and/or induction of differentiation in response to BET inhibition.51 Based on these observations, clinical trials of a number of BET inhibitors in AML were initiated.51,52
Very few trials of BET inhibitors have been published, but so far, their clinical activity as single agents for relapsed/refractory AML has been modest. Still, it is notable that some CRs have been seen in a phase 1 study of OTX015, which is encouraging.53 This raises the question of whether biomarkers or deep sequencing of “exceptional responders” could potentially identify ideal patients for the approach. Alternatively, combinatorial approaches may be critical to capitalize on this approach, ideally choosing well-tolerated drugs with carefully established pharmacodynamic validation for such regimens.
Epigenetic targeting has also shown particular promise in AML cases featuring KMT2A (MLL) gene fusions. The KMT2A (MLL) gene on chromosome locus 11q23 normally encodes a methyltransferase in its SET domain. KMT2A’s methyltransferase facilitates its role as a transcriptional coactivator through trimethylation of histone H3 lysine 4 (H3K4me3). However, recurrent translocations of KMT2A with a large number of partner genes occur in ∼5% of AML cases and are associated with high relapse rates and poor survival. Mechanistically, KMT2A’s methyltransferase function is lost through translocations, and other H3K4 methyltransferases that antagonize KMT2A function become dominant. These include histone lysine-specific demethylase 1 (LSD1, KDM1A), which removes methyl groups from histone H3 lysine 4 and 9 residues, repressing transcription and strongly promoting differentiation block.54 LSD1 inhibitors disrupt the interaction between LSD1 and co-repressors, facilitating trimethylation of H3K4 and reactivation of transcription of a number of genes that regulate differentiation and cell cycle arrest/progression. These include CEBPa p21, and p27. LSD1 inhibitors have shown in vitro antileukemic activity but also striking hematopoietic toxicity in preclinical models.54-56 Clinical trials of LSD1 inhibitors have recently been initiated.
A second way that KMT2A fusions epigentically alter gene transcription is through the recruitment of novel histone methyltransferases, including disrupter of telomeric silencing 1-like (DOT1L).57 In this context, DOT1L catalyzes aberrant H3K79 methylation of MLL target gene loci with associated transcriptional activation of Hox genes and Meis1, and this confers stem-like properties in leukemogenesis.
The results of trials of the DOT1L inhibitor pinometostat (EPZ-5676) have recently been reported and, like BET inhibitors described above, showed occasional KMT2A-rearranged patients with dramatic antileukemic effects: 6 of 49 patients showed objective responses, characterized by CR (n = 2), partial remission (n = 1), or resolution of leukemia cutis (n = 3), and 9 patients showed clinical evidence of leukemic differentiation.58 A follow-up study performed in children with MLL-rearranged AML showed no protocol-defined responses, but 7 of 18 enrolled children did show evidence of reduced circulating or marrow tumor burden during therapy.59 Both studies showed acceptable toxicity of the agent, with only rare grade 3 toxicities. chromatin immunoprecipitation sequencing was performed on circulating and/or marrow blasts collected from patients in the cohort expansion groups to measure pharmacodynamic end points. These studies confirmed marked reduction in global H3K79me2 and HoxA9- and Meis1-specific methylation during therapy, suggesting the drug potently inhibited its target.
Taken together, the available data suggest that there may be a role for targeting epigenetic deregulation in MLL-rearranged AML and possibly other subsets using BET, LSD1 and/or DOT1L inhibitors. From the available clinical data, the optimal use of these agents most likely requires combination studies performed earlier in the disease course. Biomarkers of response and/or genetic predictors of response are keenly sought.
Targeted chemotherapy delivery
ADCs provide a method to deliver traditional cytotoxic agents (and/or radioisotopes) to leukemia cells, thus increasing dose intensity while simultaneously reducing toxicity. Gemtuzumab ozogamicin, the first FDA-approved ADC for cancer therapy, provides a cautionary tale in drug development, but fortunately one that appears to have a silver lining.
Immunophenotyping of AML by flow cytometry has allowed an immense number of epitopes to be characterized for their frequency, stability, and uniformity within and across AML specimens. Of these, CD33 has emerged as a logical target for leukemia therapy. CD33 expression is limited to myeloid progenitors and more differentiated blood cells, but is not present on normal hematopoietic stem cells. It also is expressed on leukemic blasts from >90% of AML patients. The CD33 protein has structural similarity to immunoreceptors, and its normal function is thought to serve as a negative regulator of immunoreceptor (ITAM) signal transduction. Clinical trials of humanized naked antibodies directed to CD33 (also known as HuM195, lintuzumab, or SGN-33) showed some clinical activity, but typically in patients with limited tumor burden and only through prolonged infusions.60 However, given that there was no improvement in response or survival in randomized trials when lintuzumab was combined with either LDAC or intensive chemotherapy, further development of the naked antibody was shelved.
Because antibodies like lintuzumab are rapidly internalized and degraded once bound to CD33, a new targeted therapeutic opportunity emerged. The fusion of cytotoxic drugs to antibodies via pH-sensitive linkers generated large molecules that were stable in the bloodstream, but degraded their linkers and dissociated from their toxins once internalized and exposed to the highly acidic milieu of the lysosome. Early-phase studies paired formulations of lintuzumab fused either to a pyrrolobenzodiazepine dimer (vadastuximab talirine, or SGN-33A) or, in later studies, to α particle emitting radioisotopes (eg, lintuzumab-225Ac). A similar anti-CD33 antibody, gemtuzumab, was also developed using the DNA intercalating antibiotic calechiamicin as its payload (GO). These compounds all showed activity as single agents in early phase testing. Indeed, in 2000, the FDA approved GO for the therapy of relapsed AML. This accelerated approval was based on data from 3 phase 2 studies where GO was used as a single agent as initial salvage therapy of first relapse; these studies in aggregate showed second remission rates of ∼25%.61 This made GO the first ADC approved for cancer therapy and the first targeted agent in non-M3 AML subgroups.
Because GO received accelerated approval based on single-arm, phase 2 data alone, a condition of full regulatory approval was the confirmation of clinical benefit from phase 3 studies. The first reported phase 3 trial of GO after accelerated approval was the SWOG S0106 study, in which GO at a dose of 6 mg/m2 was added to standard daunorubicin/cytarabine 7 + 3 (DA) and consolidation therapy in newly diagnosed AML patients <60 years of age followed by high-dose cytarabine and a second randomization to 3 monthly treatments with GO at a dose of 5 mg/m2 vs observation.62 This trial was closed early by its data and safety monitoring committee when a planned interim analysis showed that the addition of GO not only failed to improve CR or OS rates, but was also associated with a statistically significantly increase in the induction mortality rate (5% for GO + DA vs 1.4% for DA alone) and grade 4 toxicities (21% vs 12%, respectively). Of note, the control arm showed an exceptionally low induction mortality rate for a cooperative group trial. An additional safety concern that emerged from both trials and postmarketing experience with GO was an increase in the risk of hepatic sinusoidal obstructive syndrome (formerly known as veno-occlusive disease) associated with GO therapy.63 This toxicity appears to be dose dependent, with particularly higher rates observed with doses of 9 mg/m2. Although the toxicity observed in the S0106 trial was not specifically related to hepatic dysfunction, the lack of improvements in response or survival from this trial combined with emerging safety concerns led the FDA to recommend that GO be withdrawn from the market in 2010.
This might have ended the chapter on GO were it not for emerging data from several studies conducted outside the United States as well as pediatric data from US centers that showed that the withdrawal of GO may have been premature. A common thread to these studies was the use of lower doses overall and/or 3 mg/m2 doses delivered in multiple fractions. A children’s oncology group study in newly diagnosed children with AML showed improved remission and event-free survival rates from the addition of a single GO dose of 3 mg/m2 to standard intensive chemotherapy.64 However, this effect was entirely counterbalanced by increased treatment toxicity, leading to no improvement in OS. In contrast, the French ALFA-0701 study conducted in older adults showed more promising results.65 In this study, 280 newly diagnosed AML patients aged 50 to 70 years were randomly assigned to receive standard DA therapy with or without fractionated doses of GO (3 mg/m2 on days 1, 4, and 7 of each of 2 induction cycles and additional GO doses during consolidation). Although the CR rates did not differ by study arm, the trial showed statistically significant improvements in event-free survival and OS in the GO + DA arm without associated increases in toxicity. Overall, the report suggested that dose and schedule might play a significant role in the optimal use of GO in intensive combination regimens. A large, randomized study from the United Kingdom followed and suggested no benefit for GO overall.66 Still, a rather striking reduction in relapse rates occurred among core-binding factor AML patients, which contributed to a significant improvement in their survival.66 Additionally, several studies documented exquisite sensitivity of APL blasts to GO, and a regimen combining ATRA, arsenic trioxide, and a single dose of GO of either 3 or 9 mg/m2 has been extraordinarily effective for APL. Indeed, the CR, induction mortality, and OS rates were comparable to those of patients treated with ATRA plus idarubicin on a randomized comparison. Relapse of APL after frontline ATRA + arsenic trioxide + GO has been exceedingly unusual (4%) with long-term follow-up, including patients with presenting white blood cell count of >10 × 109/L.67,68
Summarizing all the available phase 3 data from 5 phase 3 trials in adults, a UK National Cancer Research Instiute meta-analysis studied 3325 patients treated in these studies.69 The meta-analysis showed a statistically significant reduction in relapse rates and improved OS for GO-treated patients across these trials, without appreciable increases in toxicity. The benefits appeared to be limited to patients with favorable or intermediate-risk karyotype, and patients treated on studies with 3 mg/m2 per dose or fraction experienced lower induction mortality. In light of this more favorable reassessment of randomized studies, GO was given full FDA approval in September 2017 for the therapy of CD33-positive AML, both in the frontline and relapsed settings.
Additional agents targeting CD33 have entered clinical development for AML, including vadastuximab talirine (SGN-33A), which is an ADC that fuses the antibody lintuzumab with a pyrrolobenzodiazepine dimer through a linker that is stable in the bloodstream but subject to protease cleavage in lysosomes. Early phase trials of vadastuximab talirine in relapsed patients showed appreciable response rates and low rates of extramedullary toxicity. More impressive perhaps were data from studies in which the drug was administered to previously untreated patients, particularly in combination with the HMAs 5-azacitidine or decitabine. In a multicenter, phase 1/ 2 study, the combination of a HMA plus vadastuximab talirine generated CR or CRi in 36 of 49 older patients (73%; CR: 43%; CrI: 31%; age range: 60-87 years, median age: 75 years) who either refused (25%) or, due to comorbidity, were deemed ineligible to receive induction chemotherapy (75% of participants).70 Although the reported follow-up was too short to comment meaningfully on survival, the median duration of response was >9 months, and high responses rates were observed in high-risk subgroups, such as those aged >75 years, those with an abnormal karyotype, or those with antecedent MDS. Hematologic toxicity was appreciable, which contributed to relatively frequent delays of treatment courses. However, extramedullary toxicity was modest, and the 30- and 60-day mortality rates in this study were 2% and 8%, respectively.
Although these single-arm data were quite promising, a randomized study of HMAs plus vadastuximab talirine vs placebo as frontline therapy of AML in patients not eligible for induction chemotherapy (identifier NCT02785900) was halted early due to unexpectedly high rates of early mortality and serious infection in the vadastuximab talirine arm. What is unclear is whether early toxicity in this approach will ultimately confer more durable responses and better survival with longer follow-up. It is also unknown if the combination of vadastuximab talirine plus an HMA is better suited for hardier populations who could better tolerate neutropenia-associated infections. Regardless, it seems unlikely that this will be answered by the present trial, and future development of vadastuximab talirine in AML is uncertain.
Encouraging data using radioimmunotherapeutic approaches to target CD33 have also been recently reported using 225Ac-lintuzumab.71 Like GO and vadastuximab talirine, 225Ac-lintuzumab (225Ac-HuM195) is an ADC that binds CD33 and is rapidly internalized, liberating the radioisotope 225Ac, which is retained inside the cell.72 Frontline studies of 225Ac-lintuzumab are ongoing, with phase 1 results of an ongoing phase 1/ 2 study showing significant clinical activity with minimal extramedullary toxicity when the ADC was given in combination with LDAC. Because all clinical responses occurred in the first treatment cycle, the authors concluded that LDAC did not contribute to response rates, and phase 2 development of the ADC as a single agent in untreated AML patients who are not candidates for induction chemotherapy is ongoing.
In addition to CD33-targeting agents, clinical trials of ADCs directed against epitopes other than CD33 are ongoing in AML, including agents targeting CD123 (IL-3Rα). These include ADCs such as SGN-123A and SL-401.
SL-401 is among the most clinically advanced ADCs targeting CD123. This compound links an antibody against CD123 to diphtheria toxin. Some observed side effects of SL-401 can be ascribed to diphtheria toxin, including capillary leak syndrome as well as relatively frequent hepatic transaminase elevation and/or hypoalbuminemia. The development of SL-401 in AML has been enriched for the rare variant, blastic plasmacytoid dendritic cell neoplasm, where marked overexpression of CD123 occurs with regularity. Administration of SL-401 daily or every other day for up to 6 infusions has shown rather striking clinical activity in patients ineligible for blastic plasmacytoid dendritic cell neoplasm chemotherapy or those who were relapsed/refractory, including 5 of 9 patients with CR.73 The activity of the drug and tolerability of multiple cycles of therapy is being tested in a multicenter phase 2 trial, and the preliminary data are encouraging.74 Additionally, studies in patients with AML in first or second remission will clarify if this drug can target residual AML populations and/or leukemia stem cells.
Combinations of novel agents in the precision medicine era
A critical question is what should be the optimal approach to ensure patients receive precision medicine diagnostics in an expeditious manner? Ideally, these results should guide therapy choice, including frontline trials targeting identified mutations. The C10603/RATIFY trial provides us with a proven blueprint for this strategy. But although RATIFY was successful, it also suffered from substantial logistic challenges and a considerably long period between enrollment and final data analysis. Given these limitations, should this trial really be the new model for targeted AML drug development?
A major factor that contributed to RATIFY’s success was the large-scale international collaboration of multiple cooperative groups, agreement on a common chemotherapy plan, and a rapid, straightforward, centrally performed diagnostic test for eligibility. Although it seemed groundbreaking at the time, it is comparably simple to use a PCR test for a common mutation using an assay that is easily standardized across centers. By contrast, multigene panel testing by NGS is labor intensive, requires highly specialized interpretive skill, is both time consuming and expensive, and can be hard to standardize across centers.
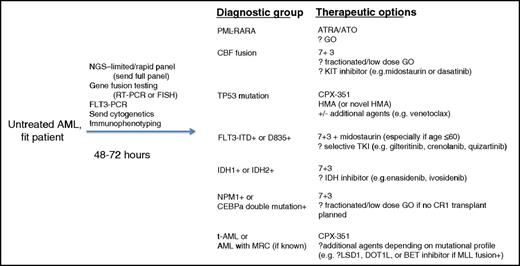
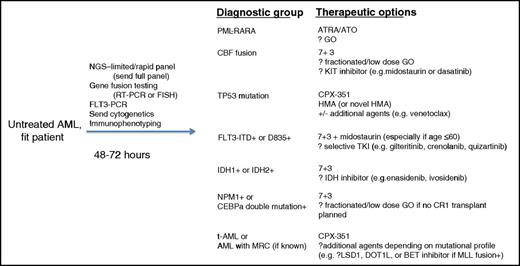
To be sure, NGS can be used for rapid diagnostics for multiple, actionable mutations, but typically only if relatively small panels are used for screening. With this approach, results can be read out within a few days and are not cost prohibitive. Some centers have already incorporated this approach into their diagnostic algorithm for new AML cases. These centers use a simultaneous, rapid, but limited NGS panel, FLT3-PCR, and concurrent reverse transcriptase-PCR or fluorescence in situ hybridization for prognostic/actionable mutations. This allocates newly diagnosed patients toward appropriate trials based on the presence of mutations such as FLT3, IDH1/2, TP53, PML-RARA, core-binding factor fusions, and NPM1. Although this is a good start, the approach studies too few genes to fully risk stratify patients for postremission therapy. Ideally, enrolled patients’ remaining specimens from diagnostic marrow sampling should also be used for more comprehensive sequencing panels that fully define baseline mutational complements (plus karyotyping). Because many studies require central laboratories to confirm the mutations of enrolled patients, it seems logical that multicenter studies should allow enrollment based on local results, so long as leftover extracted DNA can also be sent to central laboratories to confirm eligibility using trial-specific companion diagnostic tests after therapy has begun. Importantly, delays from mutation determination to the start of therapy should be minimized where possible. Figure 1 shows a proposed algorithm to allocate newly diagnosed patients into groups where novel drugs have either already shown benefits or are under investigation for potential benefit.
The flow diagram shows how integration of molecular diagnostics and NGS potentially can rapidly segregate patients into groups for whom particular and increasingly targeted therapies have shown benefit or are currently being tested. ATRA, all-trans retinoic acid; ATO, arsenic trioxide; CBF, core-binding factor; FISH, fluorescent in situ hybridization; GO, gemtuzumab ozogamicin; HMA, hypomethylating agent; MRC, myelodysplasia-related change; RT-PCR, reverse transcriptase-polymerase chain reaction; t-AML, therapy-related AML; 713, cytarabine by continuous infusion (7 doses) plus anthracycline (3 doses).
The flow diagram shows how integration of molecular diagnostics and NGS potentially can rapidly segregate patients into groups for whom particular and increasingly targeted therapies have shown benefit or are currently being tested. ATRA, all-trans retinoic acid; ATO, arsenic trioxide; CBF, core-binding factor; FISH, fluorescent in situ hybridization; GO, gemtuzumab ozogamicin; HMA, hypomethylating agent; MRC, myelodysplasia-related change; RT-PCR, reverse transcriptase-polymerase chain reaction; t-AML, therapy-related AML; 713, cytarabine by continuous infusion (7 doses) plus anthracycline (3 doses).
Alternatively, the field is testing so-called “umbrella” trials, such as the BEAT AML study. With this type of study, patients are enrolled into a single “master” protocol at the time of AML diagnosis and then assigned to appropriate arms based on diagnostic testing from central laboratories. These can incorporate rapid NGS, PCR, immunophenotypic, or other subgroup-defining tests to rationally allocate patients to appropriate trial arms. A master trial has the flexibility to open or close study arms with greater flexibility than what typically accompanies cooperative group or industry-sponsored research. Although this approach is still in the feasibility-testing realm, if successful, it could open targeted therapy to a much larger group of patients who would otherwise have to travel to centers offering specific trials for specific mutations.
Because each targeted therapy trial potentially enrolls a small sliver of the mutational pie, development of surrogate end points is critical because they may more rapidly, and with fewer enrolled patients, define successful regimens. RATIFY may have paved the way for targeted-therapy AML clinical trials in mutationally designed subsets, but it also required screening of >3200 patients to enroll 717 with FLT3 mutations. Less common mutations certainly will need far larger screens. As described above, measurable reductions in leukemic tumor burden can rapidly generate predictive data without waiting for survival or relapse, as long as the measurements are validated. Such approaches could include flow cytometry for MRD or quantitative assessments of the allele burdens of gene fusions, NPM1 mutation, or even drug target mutations. These tests seem to be the most promising surrogates for OS. MRD testing should be built into trials of targeted agents wherever possible, because it could dramatically reduce the timelines needed to estimate survival after novel targeted therapy. Importantly, because many novel targeted agents appear to induce differentiation of leukemic clone as a major mechanism of action, reduction in clone burden should not be a primary end point of early-phase, single-agent studies because it can underestimate the clinical activity signal of biologically active drugs.
It is encouraging that enasidenib received accelerated approval based on response, survival, and toxicity data from phase 2 studies. Enasidenib’s relatively low side-effect burden appears to be a key factor in using such data for approval. This may prove to be challenging, because combination regimens that will follow doubtless will have higher toxicity than single-agent studies. The experience of combining CD33 ADCs like GO or vadastuximab talirine with induction chemotherapy or HMAs highlights this issue.
And yet, despite all the exciting developments described earlier in this review, 2017 still largely finds the AML field adding novel agents to 7 + 3, as was done in the RATIFY study. One can only hope that the future of AML therapy ultimately will involve lower toxicity combinations that do not rely on the backbone of intensive cytotoxics, but it may take time to define ideal alternate regimens that incorporate targeted agents. How might we design such low-toxicity combination regimens?
Trials of FLT3 inhibitors provide some clues to address this question. Because FLT3-selective TKIs are both well tolerated and often modulate rather than eliminate the leukemic clone (ie, induce differentiation), they become interesting agents for low-intensity combination strategies. FLT3 inhibitors might show more substantial activity if paired with agents that help clear the FLT3-ITD–containing clone through some degree of leukemia-selective cytotoxicity. Could agents, such as BCL2 antagonists, synergize with FLT3 inhibitors to generate deeper treatment responses? Or would combination with an ADC achieve similar goals? Would combining midostaurin (or other FLT3 TKIs) with the recently approved CPX-351 further enhance response and survival in populations not studied in RATIFY, including patients >60 years of age or those with therapy-related or MDS-related AML who progressed after HMA therapy? Promising data combining sorafenib or midostaurin with azacitidine have already paved the way to multiple studies combing HMAs with more selective and potent inhibitors.75,76 And although the number of patients with both FLT3 and IDH mutations is small, combining IDH and FLT3 inhibitors appears to be low-hanging fruit.
Similarly, the dependence of IDH-mutated AML on BCL2 upregulation for survival appears to provide a tantalizing therapeutic opportunity to target 2 key biologic processes. However, combining IDH and BCL2 inhibition might potentially generate antagonism by eliminating BCL2 upregulation, as suggested from in vitro studies.40 Whether this actually occurs in patients is unknown from clinical studies. One could imagine sequential, rather than combined IDH- and BCL2-targeted therapy could yield different results. Careful trials will be required to ensure optimal treatment outcomes.
In conclusion, targeted therapy in AML is poised for true breakthroughs as multiple agents with novel mechanisms of action and low toxicity enter the marketplace. In much the same way arsenic and ATRA have all but eliminated the need for intensive chemotherapy approaches for APL, we can hope that intensive chemotherapy will one day only rarely be used for patients with AML. Ironically, as a first step, we are initially likely to see combinations like that from the RATIFY trial, where traditional intensive chemotherapy is combined with novel agents. This strategy almost undoubtedly will increase treatment side-effect burden. But ultimately it is hoped that combinations of multiple novel agents will eliminate the reliance on traditional cytotoxics and reduce side effects while maintaining, or increasing, efficacy. As well, when cytotoxics are required, it is hoped that novel formulations and/or novel delivery platforms can minimize extramedullary toxicity. Ultimately, this may shift the paradigm of remission-induction therapy for AML from an intensive, toxic, inpatient-focused approach to a largely outpatient approach and thereby offer effective therapy to a far larger number of patients.
Survival in AML is indeed increasing, including in high-risk subsets. Although much work remains to be done, a future where more cures are achieved with less treatment burden seems a realistic possibility for many AML patients.
This article was selected by the Blood Advances and Hematology 2017 American Society of Hematology Education Program editors for concurrent submission to Blood Advances and Hematology 2017. It is reprinted in Hematology Am Soc Hematol Educ Program. 2017;2017:54-65.
Authorship
Contribution: A.E.P. wrote the paper.
Conflict-of-interest disclosure: A.E.P. is on the Board of Directors or an advisory committee for Asana Biosciences and Actinium Pharmaceuticals and has consulted for Daiichi Sankyo, Astellas, Novartis, Pfizer, Arog, Seattle Genetics, Asana Biosciences, and Actinium Pharmaceuticals. Off-label drug use: This presentation includes novel agents in clinical development that do not yet have label indications in acute myeloid leukemia (AML). The use of sorafenib, azacitidine, or decitabine for AML therapy is off label.
Correspondence: Alexander E. Perl, Division of Hematology/Oncology, Abramson Cancer Center, University of Pennsylvania Perelman School of Medicine, PCAM 12 South Tower, 3400 Civic Center Blvd, Philadelphia, PA 19104; e-mail: alexander.perl@uphs.upenn.edu.