Key Points
PTS developed in 34% of children and young adults followed prospectively after a provoked DVT.
Low fibrinolysis, complete veno-occlusion, and high plasma serum amyloid A are candidate prognostic factors for pediatric PTS after DVT.
Abstract
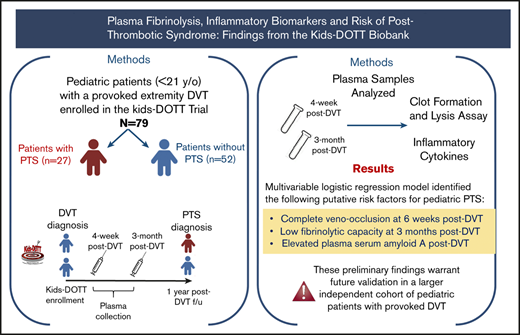
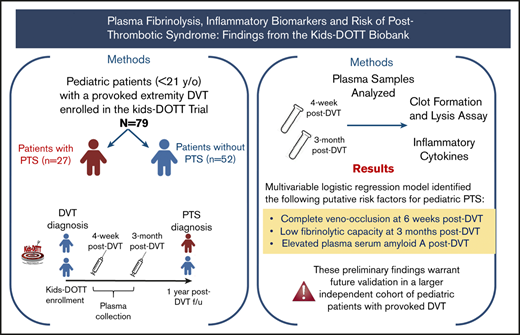
Plasma levels of markers of coagulation and inflammation have been identified as prognostic factors for adult postthrombotic syndrome (PTS). We aimed to determine whether plasma fibrinolytic capacity and cytokine levels during the first 3 months after provoked deep venous thrombosis (DVT) are associated with risk of PTS in young patients. We analyzed plasma biospecimens (6 weeks and 3 months after provoked DVT) and clinical data from a National Heart, Lung, and Blood Institute–sponsored multinational trial of anticoagulation for provoked venous thromboembolism in patients younger than age 21 years (Kids-DOTT). Patients with a provoked extremity DVT who had plasma samples available at both 6-week and 3-month post-DVT time points and PTS assessment at 1 year were included. We measured plasma fibrinolytic capacity using the Clot Formation and Lysis (CloFAL) assay and plasma cytokine levels by multiplex immunoassay. Logistic regression analyses evaluated prognostic associations with PTS. Seventy-nine patients were included (median age, 12.8 years; range, 0.04-20.8 years). PTS developed in 34%. Complete veno-occlusion at 6 weeks after diagnosis of DVT (odds ratio [OR], 3.12; 95% confidence interval [CI], 0.81-11.94; P = .097), low fibrinolytic capacity in plasma at 3 months post-DVT (OR, 2.71; 95% CI, 0.92-7.97; P = .07), and elevated serum amyloid A at 3 months post-DVT (OR, 2.85; 95% CI, 0.98-8.34; P = .055) were identified as putative prognostic factors for development of PTS. In multivariable logistic regression analysis, these factors did not retain a statistically significant independent association with PTS, but these preliminary results warrant further investigation in an independent data set to definitively evaluate these findings and identify additional potential prognostic factors for the development of PTS after a provoked DVT in young patients.
Introduction
Postthrombotic syndrome (PTS) is the most common long-term complication of pediatric venous thromboembolism (VTE), and it affects ∼1 in 4 children with a deep venous thrombosis (DVT) of the limbs.1 There is a paucity of knowledge on the prognostic factors that influence the risk for the development of PTS among pediatric patients, particularly among those with provoked DVT. In adults, elevated plasma levels of markers of coagulation, fibrinolysis, and inflammation, including D-dimer, factor VIII (FVIII), interleukin-6 (IL-6), C-reactive protein (CRP), and intracellular adhesion molecule-1 (ICAM-1), have been associated with the development of PTS in pilot studies.2-5 Among children, increased FVIII activity and D-dimer levels (both acutely and at 3 months after diagnosis of DVT) have been shown to be predictive of a composite adverse VTE outcome consisting of persistent thrombosis, VTE recurrence, or PTS.6 However, specific prognostic factors for pediatric PTS after a provoked DVT remain largely unknown, which hinders the development of risk-stratified therapeutic interventions aimed at preventing this complication in children.
The pathophysiology of PTS is not fully understood, but it is thought to be the result of a combination of venous blood reflux and venous hypertension in the setting of clot- and inflammation-induced venous valvular damage and the presence of impaired fibrinolysis that leads to residual vein obstruction and fibrosis.7 Previous work using the Clot Formation and Lysis (CloFAL) assay in a single-institution pediatric VTE cohort has shown overall improvement in acute hypercoagulability and hypofibrinolysis over the course of the first 3 months after VTE diagnosis; however, a small subgroup of these patients eventually develops an increase in plasma coagulability and/or decrease in fibrinolytic plasma capacity after an acute DVT episode.8 On the basis of our previous observations, we sought to investigate whether plasma fibrinolytic capacity and cytokine levels during the first 3 months after diagnosis of acute provoked DVT in patients younger than age 21 years are associated with the risk of PTS. We hypothesized that complete veno-occlusion, a decline in plasma fibrinolytic capacity, and increased inflammatory cytokines, including IL-6, are prognostic of PTS in young patients with a provoked DVT.
Methods
Study design
This analysis is based on a cohort study that included de-identified patient-level clinical data and banked plasma biospecimens collected at 6 weeks and 3 months after diagnosis of provoked VTE from a subset of participants in the ongoing National Heart, Lung, and Blood Institute (NHLBI)-sponsored Kids-DOTT multicenter trial.9 The study was approved by the local institutional review boards at participating sites, with signed informed consent/assent required for patient participation. The intent to identify clinical and laboratory-based prognostic factors for VTE outcomes in children was specified in the protocol and consent/assent documents.
The Kids-DOTT trial was initiated via a nested pilot and feasibility phase in 2007, followed by a rest-of-trial phase in 2013. Enrollment was completed in December 2019. The trial design has been previously reported in detail.9,10 This analysis included patients enrolled from 2007 through early 2019.
Participant eligibility
Inclusion criteria for the Kids-DOTT multicenter trial included age from birth (postconceptional age of ≥36 weeks) to <21 years, radiologic evidence of VTE within 30 days, and identification of a provoking clinical factor (eg, recent hospitalization, immobilization, traumatic injury, central venous catheterization, oral contraceptive pill administration, major infection) at the time of VTE diagnosis or symptom onset.
Exclusion criteria consisted of a previous episode of VTE, malignancy not in remission, congenital heart disease or other underlying condition requiring the use of chronic (ie, greater than 6 months) anticoagulation, systemic lupus erythematosus, pulmonary embolism not accompanied by DVT, use of or intent to use thrombolytic therapy, and presence of moderate or severe anticoagulant deficiency as defined by plasma antithrombin activity of <30 IU/dL or protein C or protein S activity of <20 IU/dL. Participants presenting with only a superficial venous thrombosis were also excluded.
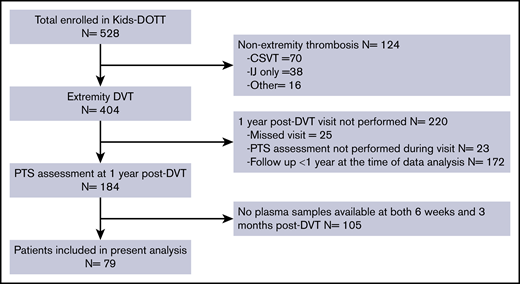
For the purposes of this analysis, the following were also excluded from the analytic population: patients in whom plasma samples had not been obtained at both the 6-week and 3-month post-VTE time points (thus, all patients included in this analysis had both 6-week and 3-month post-VTE plasma samples available for analysis), patients with a thrombosis not affecting the limbs or vena cava, and patients who did not have a PTS assessment performed at the 1-year post-VTE follow-up visit (Figure 1).
Blood sample collection, processing, and preparation for laboratory analyses
Whole blood was collected during follow-up visits at 6 weeks and 3 months after diagnosis of VTE via atraumatic peripheral venipuncture using minimal applied stasis into BD Vacutainer 3.2% buffered sodium citrate siliconized blood collection tubes. Sample processing occurred within 1 hour of collection. Samples were centrifuged at 2500g for 15 minutes at 4°C. The supernatant was then isolated and subjected to repeat centrifugation for 15 minutes at the aforementioned settings. The resulting platelet-poor plasma supernatant was pooled, aliquoted into propylene tubes, and frozen at −80°C in the SAM storage units (Hamilton, Reno, NV) of the College of American Pathologists–accredited Johns Hopkins All Children’s Hospital Pediatric Biorepository for long-term storage until time of assay. All plasma aliquots were treated with heparinase once they were thawed in preparation for the assay.
CloFAL assay procedure
Coagulative and fibrinolytic capacities were measured in vitro in platelet-poor plasma by using the CloFAL assay. The CloFAL assay is a turbidimetric test that serially monitors kinetic fibrin formation and dissolution in plasma after the addition of activators of coagulation (tissue factor [TF]) and fibrinolysis (tissue plasminogen activator [tPA]). The CloFAL assay methods underwent minor alteration from the previously described modification to the original method.8,11,12 In brief, all samples were pretreated with heparinase (Hepzyme, Siemens Healthcare Diagnostics, Deerfield, IL) before performing the assay. Then, plasma samples were loaded in quadruplicate wells of a 96-well round-bottom Nunc microassay plate (Thermo Fisher Scientific, Santa Clara, CA). Tris(hydroxymethyl)aminomethane (Tris)-buffered saline (pH 7.0) reagent, which provided citrate reversal with CaCl, coagulation activation with human recombinant lipidated TF (BioMedica Diagnostics, Windsor, NS, Canada), and fibrinolytic enhancement with recombinant human tPA (Reprokine, Tampa, FL), was added to 3 of the 4 wells for a given sample; Tris-buffered saline alone was added to the remaining well to serve as a blank. Final plasma concentrations were as follow: CaCl2, 17 mM; lipidated TF, 2 pM; and tPA, 450 ng/mL. Kinetic blanked dual-wavelength (405 and 630 nm) absorbance measurements were immediately obtained at 45-second intervals in a Perkin Elmer 2300 EnSpire Multilabel Reader for 3 hours, generating a clot formation and lysis waveform. (In nearly all cases, waveforms were complete within 1 hour.) Results were exported to Microsoft Excel for analysis. The assay standard was pooled normal adult plasma (George King Inc, Overland Park, KS).
Previously established measurements used to assess hypercoagulability consisted of the maximum amplitude of absorbance, which is directly obtained from blanked absorbance data, and the area under the curve (AUC) was calculated over the first 60 minutes (AUC0-60). In addition, fibrinolytic capacity was measured via the modified fibrinolytic index (FI2), which adjusts fibrinolytic capacity for the magnitude of clot formation.8,11,12
Plasma cytokines assay
Plasma levels of IL-6, IL-8, IL-10, vascular endothelial growth factor 1 (VEGF-1), CRP, serum amyloid A (SAA), vascular cell adhesion protein 1 (VCAM-1), and ICAM-1 were simultaneously measured using a commercially available V-Plex Human Biomarker 40-Plex panel (Meso Scale Discovery, Rockville, MD), according to the manufacturer’s instructions. These biomarkers were selected on the basis of our review of published literature. The Mesoscale Discovery V-Plex Plus Human Biomarker 40-Plex Kit (K15209G; Mesoscale Diagnostics, Rockville, MD) was performed according to the manufacturer’s recommendations. We used the following sample dilutions: vascular injury panel 2, 1250×; angiogenesis panel 1, 4×; chemokine panel 1, 4×; cytokine panel 1, 4×; proinflammatory panel 1, 4×. The average coefficients of variation for each panel were vascular injury panel, 1.57%; angiogenesis panel, 4.16%; chemokine panel, 3.96%; cytokine panel, 3.74%; and proinflammatory panel, 2.76%.
Clinical data collection
Clinical data were prospectively collected on patient and thrombus characteristics, clinical prothrombotic risk factors, anticoagulant therapy agents, follow-up duration, and development of PTS (among other exposure and outcome variables). Follow-up visits occurred at 6 weeks and 3, 6, 12, and 24 months after DVT diagnosis. The primary outcome was the development of PTS at 1 year after DVT diagnosis using the Manco-Johnson Instrument, in accordance with the International Society on Thrombosis and Haemostasis (ISTH) Scientific and Standardization Committee (SSC) guidelines for outcome definitions in pediatric VTE clinical research.13 Complete veno-occlusion at 6 weeks was defined as radiologically confirmed absence of flow in the entire venous segment of the index VTE. The reliability of this determination has been previously validated.9
All patients received therapeutic anticoagulation with low molecular weight heparin twice per day for a total duration of 6 weeks to 3 months after diagnosis of DVT, with therapeutic dose-monitoring by anti-FXa activity assay to achieve a goal level of 0.5 to 1 anti-FXa U/mL at 4 hours after dose, in accordance with international guidelines for antithrombotic therapy in children.14
Given the ongoing nature of the Kids-DOTT multicenter randomized clinical trial and the importance of maintaining equipoise throughout the trial, the investigators remained masked to the duration of anticoagulation for this analysis so that relationships between development of PTS and randomized duration of anticoagulation could not be prematurely determined. Data stewardship and honest brokerage were provided via the NHLBI U01-sponsored Kids-DOTT Data Coordinating Center (CPC Clinical Research, Aurora, CO) and the Johns Hopkins All Children’s Health Informatics Core.
Statistical analyses
Descriptive statistics were used to summarize data on patient characteristics and outcomes. Continuous variables were summarized as means with standard deviations and compared between patients (PTS positive) and controls (PTS negative) with independent Student t test or Mann-Whitney U test, as appropriate. Categorical variables were summarized as counts with percentages and compared using the χ2 test or Fisher’s exact test, as appropriate.
Associations between the CloFAL parameters, plasma inflammatory marker levels, and risk of PTS were determined by univariable logistic regression with Firth’s penalized likelihood approach (because of the small number of patients with PTS), to obtain odds ratios (ORs) and 95% confidence intervals (CIs). For the univariable analyses, each putative prognostic variable was analyzed as a tertile-based set of variables. The upper tertile was compared with the combined middle and lower tertiles for all variables, with the exception of the CloFAL FI2 for which the lower tertile was compared with the combined middle and upper tertiles based on its hypothesized and biologically plausible relationship with PTS. These categorizations helped to compare the association between low- and high-risk groups. Variables with a value of P < .1 in the univariable analysis were included in a multivariable logistical regression model after determining that there was no evidence of multicollinearity among the variables. SAS v 9.4 was used for all statistical analyses. All statistical tests were 2-sided, and a value of P < .05 was considered statistically significant.
Results
Figure 1 provides a CONSORT diagram of the analytic population. Of the 528 patients enrolled in the Kids-DOTT trial at the time of analysis, 404 had an extremity DVT and were eligible for this analysis. Of these, 79 patients were included in this study on the basis of having plasma samples available for analysis at both 6 weeks and 3 months after DVT and PTS assessment performed at 1 year after DVT.
Table 1 provides a summary of the demographic and DVT characteristics of the final population included in this analysis (n = 79) compared with the excluded population (n = 325). Median age was higher among the included patients compared with those who were excluded (12.9 vs 7.6 years; P = .007). There were no other statistically significant differences between the included and excluded populations.
Among the 79 patients included in this analysis, 46% percent were females. Central venous catheters were the provoking DVT factor in 58.2%. Most DVTs were located in the lower extremity (62%). Of the 49 patients with a lower-extremity DVT, 23 had an ileofemoral DVT, and 26 had a femoral-popliteal DVT. Radiologic assessment at 6 weeks after DVT diagnosis revealed complete veno-occlusion in 15.2% of patients.
Twenty-seven patients (34.2%) were diagnosed with PTS at the 1 year post-DVT follow-up visit; 3 of them had clinically significant PTS. Patients with PTS had a higher frequency of DVT in the lower extremity (74%) and of complete veno-occlusion at 6 weeks after DVT (25.9%) when compared with the overall population. Among patients with a lower-extremity DVT, the risk of PTS at 1 year was higher in patients with an ileofemoral DVT compared with those who had a femoral-popliteal DVT (47.8% vs 34.6%).
Table 2 shows the median levels of inflammatory markers for patients according to PTS status and follow-up time points (6-week and 3-month). There were no statistically significant differences in median plasma levels of inflammatory markers at 6 weeks and 3 months after DVT between PTS-positive and PTS-negative patient groups.
In univariable logistic regression analyses, the following 3 characteristics were identified as putative prognostic factors for the development of PTS at 1 year (Table 3): complete veno-occlusion at 6 weeks after diagnosis of DVT (OR, 3.29; 95% CI, 0.93-11.6; P = .06), plasma fibrinolytic capacity in plasma in the lowest tertile at 3 months after diagnosis of DVT (OR, 2.51; 95% CI, 0.93-6.78; P = .07), and SAA levels in the upper tertile at 3 months after diagnosis of DVT (OR, 2.33; 95% CI, 0.87-6.23; P = .09). In multivariable logistic regression analysis, none of these factors had a statistically significant, independent association with the risk of PTS (Table 4). In post hoc analyses, neither persistence of fibrinolytic capacity in the lowest tertile (ie, at both 6 weeks and 3 months) nor persistence of SAA levels in the upper tertile (ie, at both 6 weeks and 3 months) were significantly associated with risk of PTS.
Discussion
In this analysis of a multinational clinical trial–derived biobank, we have identified complete veno-occlusion at 6 weeks after diagnosis of provoked DVT in patients younger than age 21 years, low fibrinolytic capacity in plasma at 3 months after DVT, and increased plasma levels of SAA at 3 months as putative prognostic factors for the development of PTS. In multivariable analysis, these factors did not demonstrate an independent statistically significant association with PTS, but these preliminary findings do suggest that persistence of venous obstruction, impaired fibrinolysis, and systemic inflammation during the first 3 months after diagnosis of acute provoked DVT may contribute to the pathogenesis of PTS in young patients. Given the preliminary nature of these findings, these results require further validation in larger independent cohorts of pediatric patients with provoked DVT.
Our observation that impaired fibrinolysis during the first 3 months after diagnosis of provoked DVT is associated with increased risk of PTS is consistent with previous studies in adults with first-episode DVT, showing that those who developed PTS exhibited hypofibrinolysis during the first 3 months after DVT in association with increased plasma levels of thrombin-activatable fibrinolysis inhibitor.15 After an episode of venous thrombosis, the ensuing inflammatory response regulates endogenous fibrinolysis leading to thrombus reabsorption and recanalization. Impaired fibrinolysis can alter this process via failure of venous recanalization with a secondary increase in venous wall and valvular damage, development of blood flow obstruction, venous hypertension, and venous reflux, culminating in PTS.16
Among patients with a lower extremity DVT, iliofemoral thrombosis contributed substantially to the development of PTS, possibly reflecting a larger volume of residual vein obstruction compared with patients with femoral-popliteal thrombosis. We surmise that persistent veno-occlusion at 6 weeks may be linked to the presence of impaired or decreased fibrinolysis during the first 3 months after DVT and likely increases the risk of PTS through a similar mechanism. Along with ex vivo plasma hypofibrinoltic function, reduced in vitro clot permeability has been associated with the development of PTS in adults.17 Previous data suggest that clot structures formed from denser fiber networks that are relatively resistant to tissue-type plasminogen activator-induced lysis can lead to slower thrombus reabsorption and recanalization.15 Slow recanalization results in longer periods of outflow resistance and venous hypertension, which may lead to clinically overt PTS. By contrast, rapid thrombus resolution is thought to preserve valvular function.16,18
SAA is an acute phase reactant that is part of the innate immune system involved in immune activation and immunomodulation.19 Increased levels of SAA have been associated with the risk of VTE.20 In vitro studies have shown that SAA may contribute to a hypercoagulable state via several mechanisms, including direct binding to fibrin and promotion of amyloid formation in fibrin, induction of TF expression on monocytes and endothelial cells, and potentiation of a prothrombotic state in platelets.17,21 Our findings are novel in suggesting that increased plasma levels of SAA may also increase the risk of PTS among young patients with DVT. Other markers of inflammation, including IL-8, CRP, and adhesion molecules such as ICAM-1, have been associated with an increased risk for PTS and chronic venous disease in adult pilot studies, but we were unable to detect such an association in this analysis.
Both impaired fibrinolytic capacity and increased SAA levels at 3 months after DVT were associated with the risk of PTS, but we did not find a similar association at the 6-week time point. This finding is consistent with those of previous studies in adults that have shown significant associations of inflammatory markers such as IL-6 at 4 months after DVT and CRP at 12 months after DVT but a lack of association at earlier time points.3,5,22 Taken together, these observations may suggest that the prognostic utility and reliability of these biomarkers in relation to the chronic process of developing PTS is greater during the early chronic phase after DVT than during the acute or subacute phases.
Strengths of this study include the prospective follow-up of a well-defined, multinational population of patients with objectively diagnosed provoked DVT, the collection of samples at 2 different time points, which permitted us to evaluate the effect of the biomarkers of interest at different time points, the stringent quality assurance achieved via the specimen collection and storage procedures (overseen by a College of American Pathologists–accredited biorepository), and the systematic approach to the diagnosis of PTS, using 1 of 2 instruments recommended by the SSC of the ISTH for the diagnosis of PTS in patients younger than age 21 years.13 One limitation of our study is that our preliminary findings are not definitive and warrant confirmation and further evaluation in a larger study. Furthermore, given the inclusion criteria of the Kids-DOTT trial, these findings are applicable only to patients with provoked DVT, and it is possible that the prognostic factors for PTS development differ among patients with provoked and unprovoked DVT. We also used a targeted approach instead of a discovery approach to identify putative biomarkers via the use of a commercially available cytokine panel. This approach may have led us to miss other potential prognostic biomarkers of importance that were not included in our panel. Finally, it is possible that patients with PTS symptoms are more likely to come to their PTS assessment follow-up visit at 1 year after DVT, which may be a source of bias in our population. However, given that the primary end point of the Kids-DOTT trial is recurrent VTE within 1 year after index VTE, every effort was made to retain patients in the trial until their 1-year follow-up visit. To date, more than 70% of Kids-DOTT participants who were eligible for their 1-year post-VTE visit have completed this assessment. Despite these limitations, this study represents one of the largest (and one of only a few multicenter) prospective studies investigating both clinical and laboratory-based prognostic markers for pediatric PTS in patients with provoked DVT using a standardized PTS outcome measurement.
In summary, our study supports a potential role of systemic inflammation in the form of increased plasma levels of SAA, low plasma fibrinolytic capacity as measured by CLoFAL assay FI2, and persistent complete veno-occlusion in the pathogenesis of PTS after provoked DVT in young patients. These putative prognostic factors did not retain a statistically significant independent association with the risk of PTS in multivariable logistic regression analysis, but our preliminary results warrant future validation in larger independent populations that will permit the definitive evaluation of these findings and the identification of other potential prognostic factors for PTS.
For original data, please contact the corresponding author, Marisol Betensky, at marisol.betensky@jhmi.edu.
Acknowledgments
The authors thank the patients and families for their generous participation in the Kids-DOTT multicenter trial, and M. Gail Mueller of the All Children’s Research Institute for her excellent technical work in performing the CloFAL assay analyses.
This work (Kids-DOTT trial) was supported by grants from the Clinical Coordinating Center, Data Coordinating Center, National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) (1U01HL130048), a Research Supplement to Promote Diversity, a grant from the NIH/NHLBI (1K23HL084055), an American Society of Hematology Bridge Grant, a Johns Hopkins All Children’s Foundation Institutional Research Grant, and a Hemophilia and Thrombosis Research Society Thrombosis Studies Award.
Authorship
Contribution: N.A.G. designed the study; M.B. and N.A.G. enrolled patients and collected data; S.B. and A.D.E. performed the plasma cytokines assays; E.K.A. analyzed data; M.B., N.A.G., and A.D.E. interpreted the findings; M.B. and N.A.G. drafted the manuscript; and all authors provided critical revisions and approved the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A complete list of the members of the Kids-DOTT Investigator Group appears in the supplemental appendix.
Correspondence: Marisol Betensky, Johns Hopkins All Children’s Hospital, 501 6th Ave South, St Petersburg, FL 33701; e-mail: marisol.betensky@jhmi.edu.
References
Author notes
The full-text version of this article contains a data supplement.