Key Points
After 3-year follow-up, M+R continued to be well tolerated with modest efficacy in patients with R/R DLBCL.
First results for M+R + gemcitabine-oxaliplatin show that it was tolerable and induced responses in R/R DLBCL.
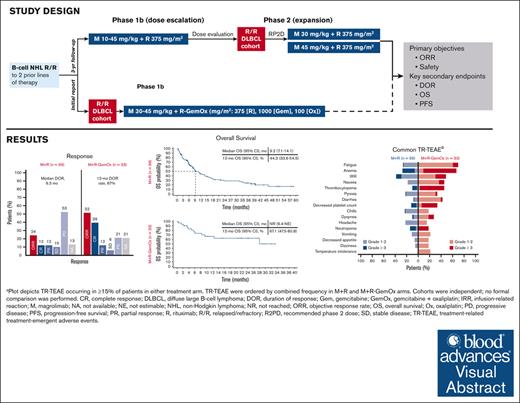
Visual Abstract
Patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) ineligible for available salvage therapies have limited options for long-term disease control, necessitating novel treatments. Previously, magrolimab (anti–cluster-of-differentiation-47 antibody) plus rituximab (M+R) demonstrated ability to induce complete responses (CR) in R/R DLBCL. Here, we report 3-year follow-up data from this phase 1b/2 study assessing long-term safety and efficacy of M+R, and initial safety and efficacy of M+R plus gemcitabine-oxaliplatin (M+R-GemOx), in R/R DLBCL. After magrolimab priming, 4 groups of patients received M+R, 10 to 45 mg/kg magrolimab with 375 mg/m2 rituximab; patients receiving M+R-GemOx received 30 or 45 mg/kg magrolimab with 375 mg/m2 rituximab, 1000 mg/m2 gemcitabine, and 100 mg/m2 oxaliplatin. Primary end points were treatment-emergent adverse events (TEAEs) and objective response rate (ORR). Secondary end points included duration of response (DOR), progression-free survival (PFS), and overall survival (OS). Of 132 patients treated, 99 received M+R and 33 received M+R-GemOx. Most common any-grade TEAEs were fatigue (M+R, 40%; M+R-GemOx, 70%), infusion-related reactions (M+R, 39%), or anemia (M+R-GemOx, 70%). Treatment-related TEAEs led to magrolimab discontinuation in 7% (M+R) and 6% (M+R-GemOx). One death was considered treatment related (M+R-GemOx, colitis). M+R ORR was 24% (CR, 12%), and median DOR was 9.3 months. Median PFS and OS were 1.8 and 9.2 months, respectively. M+R-GemOx ORR was 52% (CR, 39%); 12-month DOR rate was 66.6% (95% confidence interval, 33.1-86.1). Median PFS and OS were 3.9 months and not reached, respectively. These results demonstrate that M+R with/without GemOx is well tolerated, and M+R-GemOx has clinical activity in patients with R/R DLBCL. This trial was registered at www.clinicaltrials.gov as #NCT02953509.
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most prevalent lymphoid malignancy in adults, comprising >30% of non-Hodgkin lymphoma (NHL) cases.1 DLBCL is potentially curable with currently recommended first-line immunochemotherapy consisting of the anti–cluster-of-differentiation (CD) 20 antibody rituximab in combination with cyclophosphamide, doxorubicin, prednisone, and either vincristine or polatuzumab vedotin-piiq.2 Nevertheless, ∼30% to 40% of patients are either refractory to this treatment or later experience relapse.2 Second-line treatment for patients with DLBCL involves either high-dose chemotherapy (HDCT) and subsequent autologous stem cell transplantation (ASCT) or chimeric antigen receptor (CAR) T-cell therapy for those who are eligible,3 although new treatments (eg, bispecifics, monoclonal antibodies, and antibody–drug conjugates) have emerged in recent years.2,4 Neither of these therapies are generally accessible to everyone. ASCT requires a level of fitness and readiness to tolerate HDCT in addition to achieving disease remission; CAR T-cell therapy is currently only available at select centers and requires a certain level of disease control to allow enough time for apheresis and reinfusion. Both therapies provide ∼50% long-term remissions, with the other half of patients relapsing. For patients ineligible for intensive therapy or relapsing after ASCT, rituximab plus gemcitabine and oxaliplatin (GemOx) is an option despite limited clinical benefit due to lack of durable responses.5,6 Hence, there remains an unmet need in relapsed/refractory (R/R) DLBCL for therapies that provide long-term disease control.
Incorporation of newer agents on existing rituximab chemotherapy backbones may improve response. Magrolimab is a humanized monoclonal antibody designed to block CD47, a transmembrane protein overexpressed on cancer cells that enables phagocytic evasion by essentially acting as a “don’t-eat-me” signal.7-10 By blocking CD47, magrolimab unmasks the prophagocytic “eat-me” signal expressed by tumor cells.7,8,11 Preclinically, magrolimab has been demonstrated to synergize with rituximab in a model of NHL11; whereas magrolimab inhibits tumorigenic CD47 antiphagocytic signaling, rituximab mediates Fc activation of antibody-dependent cellular phagocytosis.7,8,11 Additionally, chemotherapy agents have the potential to increase CD47 expression12 and induce prophagocytic signals such as calreticulin.13,14
Phase 1b results from a phase 1b/2 study showed that magrolimab at the recommended phase 2 dose (30 mg/kg weekly) in combination with rituximab (M+R) was well tolerated and had encouraging activity in patients with R/R NHL, including DLBCL.15 Overall, the objective response rate (ORR) was 50%, with a complete response (CR) rate of 36% (N = 22 total patients; median follow-up, 6.2 months for DLBCL and 8.1 months for follicular lymphoma). In patients with R/R DLBCL (n = 15), the ORR was 40%, and the CR rate was 33%. Here, we report 3-year follow-up data from this phase 1b/2 study assessing the long-term safety and efficacy of M+R in patients with R/R DLBCL. Additionally, we present initial safety and efficacy results for patients with R/R DLBCL who received M+R-GemOx during phase 1b. Exploratory biomarker analyses also examined whether circulating tumor DNA (ctDNA) dynamics, expression of drug targets (CD20 and CD47), tumor penetration by magrolimab, and molecular subtypes correlated with clinical response.
Methods
Trial oversight and conduct
This trial was conducted in accordance with the protocol, the US Food and Drug Administration, the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Wse Good Clinical Practice guidelines, the Declaration of Helsinki, and any applicable local health authority and institutional review board/independent ethics committee requirements. All participants gave written informed consent.
Study design
This study (ClinicalTrials.gov identifier: NCT02953509) was an open-label, multicenter, phase 1b/2 trial investigating M+R and M+R-GemOx combinations in R/R B-cell NHL. Eligible patients (aged ≥18 years) had CD20-expressing R/R B-cell NHL, including histologically confirmed de novo or transformed DLBCL, and an Eastern Cooperative Oncology Group performance status of 0 to 2. In phases 1b and 2, patients eligible for M+R had R/R disease to ≥2 prior lines of therapy; in phase 2, at least 1 prior line must have contained an anti-CD20 antibody. In phase 1b, those who were eligible for M+R-GemOx were R/R to 1 to 3 prior lines of DLBCL-specific therapy (at least 1 including an anti-CD20 antibody) and either were not candidates for HDCT/ASCT or had relapsed after ASCT. Primary refractory patients (defined by failure to achieve a response to first-line therapy or progression within 3 months of completing first-line treatment) were excluded, but patients refractory to subsequent lines were eligible. Patients who relapsed after GemOx-containing treatment <12 months before study start were not permitted. Prior CAR T-cell therapy was not permitted.
Dose escalation followed a standard 3+3 study design15 (supplemental Figure 1). In phase 1b, patients received an IV priming dose of 1 mg/kg magrolimab on cycle 1, day 1 (each cycle = 28 days) to mitigate on-target anemia, followed by 10, 20, 30, or 45-mg/kg maintenance doses. The 10 to 30 mg/kg magrolimab maintenance doses were administered weekly starting on cycle 1, day 8. The 45 mg/kg maintenance doses were administered weekly in cycles 1 and 2, and every 2 weeks for cycles 3 and beyond. Patients enrolled in phase 1b who continued treatment in phase 2 were allowed to follow the recommended phase 2 dosing schedule.
In phase 2, 30 and 45-mg/kg magrolimab maintenance doses were explored further because no additional dose-limiting toxicities (DLTs) occurred, and steady-state dose levels were well above the targeted threshold.16 The phase 2 magrolimab dosing schedule was the same as that in the phase 1b, 45-mg/kg dose schedule: a priming dose on cycle 1, day 1; weekly maintenance dosing (30 or 45 mg/kg) during cycles 1 and 2, followed by maintenance doses every 2 weeks thereafter. Rituximab (375 mg/m2 IV) was administered weekly during the first cycle starting with day 8, followed by 1 dose monthly on day 1 of cycles 2 through 6, and then on day 1 of every other cycle beginning with cycle 8.
M+R-GemOx was explored in phase 1b with an initial safety dose-escalation phase followed by an expansion phase. Patients received a priming dose of 1 mg/kg magrolimab IV on day 1, followed by weekly (cycles 1-2) then biweekly (cycles ≥3) maintenance doses of 30 or 45 mg/kg, as described above for M+R; cycle 1 was 5 weeks long, and cycles 2 and later were 4 weeks long. The rituximab dosing schedule for the M+R-GemOx group was the same as previously described for the M+R group. Gemcitabine 1000 mg/m2 and oxaliplatin 100 mg/m2 were both administered IV on cycle 1, day 11 and cycle 1, day 23 and on days 2 and 15 of cycles 2 through 4; dosing was permitted beyond cycle 4, per investigator discretion, for a total of 8 doses. In both treatment groups, patients received M+R until progression, unacceptable toxicity, or study withdrawal.
End points
The primary objectives of this study were determination of the safety, tolerability, and efficacy (as measured by ORR) for both treatment combinations. Treatment-emergent adverse events (TEAEs), including DLTs (phase 1b), were investigator-assessed using common terminology criteria for adverse events (version 4.03). DLTs were defined as any grade ≥3 TEAE determined to be related to the study drug (magrolimab, rituximab, and/or GemOx) that occurs during the first 4 weeks of M+R treatment or during weeks 2 through 5 of M+R-GemOx treatment. Disease response was assessed by investigators according to the Lugano Classification for Lymphomas.17 Secondary end points included duration of response (DOR), progression-free survival (PFS), and overall survival (OS) of patients treated with either combination.
Exploratory analyses
Tumor and plasma samples were collected to conduct assessments of exploratory biomarkers of magrolimab activity and tumor penetration. Tumor biopsies were mandatory, when feasible, for all cohorts except patients treated with M+R in phase 1b. Tumor/lymph node biopsies were collected at screening and on cycle 2, day 8. If there was disease involvement of the bone marrow at screening, a bone marrow aspirate/biopsy was required in all patients before treatment on cycle 3, day 1. Optional repeat tumor biopsy and bone marrow aspirate/biopsy were collected at the time of disease progression or relapse for patients who achieved a partial response (PR) or CR. Immunohistochemistry (immunoglobulin G4 [IgG4], CD20, and CD47) was performed on tumor cells from biopsies to examine tumor penetration of magrolimab and determine whether baseline CD20 or CD47 staining was associated with clinical outcome.
Genetic classification of DLBCL subtypes was performed with LymphGen version 2.0 (https://llmpp.nih.gov/lymphgen/index.php) using inputs derived from whole-exome sequencing (WES) of tumor biopsies and matched peripheral blood mononuclear cells (PBMCs). WES on formalin-fixed paraffin-embedded tumor biopsies and matched PBMCs was performed by Fulgent Genetics. Library preparation was performed using the IDT xGen Exome version 1 kit and sequenced to a depth of 100× coverage (PBMC) or 200× coverage (tumor) using paired-end, dual-index, 2 × 150–base pair reads on the Illumina NovaSeq platform. Mutations were identified using a custom WES analysis pipeline with the Genome Analysis Toolkit best practices guideline, using the GRCh37 b37 reference genome. Copy number variations derived from WES data were evaluated using CNVkit version 0.9.10. Inputs for LymphGen were subjected to filtering and formatting in accordance with LymphGen instructions (supplemental File 1). Gene fusion information was set to “not available” unless the patient was specifically assessed for BCL2 and/or BCL6 fusion via fluorescence in situ hybridization.
ctDNA was monitored using a 16-plex ctDNA assay (Signatera RUO, Natera, Inc). For ctDNA analysis, formalin-fixed paraffin-embedded tumor tissues and matched normal blood samples (single nucleotide variants) were used. These assays were used to track the presence of ctDNA in the associated patients’ blood plasma. Plasma samples for ctDNA testing were collected on day 1 of cycles 1 through 4. ctDNA positivity was quantitatively reported in mean tumor molecules per milliliter of plasma.
Statistical analyses
All patients who received at least 1 dose of magrolimab were included in the efficacy analysis set; all patients who received at least 1 dose of any study drug were included in the safety analysis set. For continuous variables, mean, standard deviation, median, and range were calculated. For categorical variables, the frequency and percentage in each category were calculated, along with 95% confidence intervals (CIs), as appropriate. For time-to-event variables, Kaplan-Meier estimates and corresponding 2-sided 95% CIs for medians and quartiles were calculated.
ORR was defined as the proportion of patients with an objective response (ie, CR + PR) in the efficacy analysis set. DOR was measured from when the first objective response (ie, CR or PR) was met until the first date of objectively documented progressive disease (PD) or death due to any cause. PFS was measured from dose initiation until the first date of documented disease progression, by Lugano criteria,17 or death. OS was measured from dose initiation until death.
For immunohistochemical detection of IgG4, paired comparisons (screen vs cycle 2, day 8) were run for data points with complete pairs. Incomplete pairs (eg, a patient with only screen data) were excluded from statistical comparison. The H score for CD47 and CD20 staining at screening was compared between responders and nonresponders using the Wilcoxon rank-sum test.
Results
Patient disposition and baseline characteristics
As of 28 February 2022, 132 patients with R/R DLBCL were enrolled and received treatment. In total, 99 patients were treated with M+R (magrolimab maintenance doses: 10 mg/kg, n = 2; 20 mg/kg, n = 6; 30 mg/kg, n = 68; and 45 mg/kg, n = 23). In this treatment group, the median duration of magrolimab treatment was 1.6 months (range, 0.0-57.5). Ninety-one patients (91.9%) discontinued magrolimab and 90 (90.9%) rituximab, mainly because of PD (magrolimab, 66.7%; rituximab, 65.7%) and TEAEs (magrolimab, 12.1%; rituximab, 11.1%).
Thirty-three patients were treated with M+R-GemOx (magrolimab maintenance doses: 30 mg/kg, n = 26; 45 mg/kg, n = 7). In this treatment group, the median duration of magrolimab treatment was 2.6 months (range, 0.0-23.2). Twenty-seven patients (81.8%) discontinued magrolimab and rituximab, mainly because of PD (magrolimab, 39.4%; rituximab, 36.4%), TEAEs (magrolimab, 15.2%; rituximab, 18.2%), and physician decision (magrolimab, 12.1%; rituximab, 15.2%). Patients in this group received a median of 2.0 GemOx treatments (range, 1-4).
Baseline characteristics for both treatment groups are summarized in Table 1. The majority of patients (66.7%) were aged ≥65 years and male (62.9%). In the M+R group, patients received a median of 3 (range, 1-9) prior anticancer therapies, and 23.2% had prior ASCT; 78.8% had disease that was refractory to the last regimen, and 52.5% had primary refractory disease within 6 months of the last dose of first-line treatment. Patients with only 1 prior line of therapy were enrolled in earlier stages of the study, according to inclusion/exclusion criteria outlined in an earlier version of the protocol. In the M+R-GemOx group, patients received a median of 2 (range, 1-7) prior anticancer therapies, and 18.2% had prior ASCT; 42.4% were refractory to the last regimen, and 21.2% had disease that had become refractory within 6 months of the last dose of first-line treatment.
Safety
Almost all patients in both treatment groups (M+R, 99.0%; M+R-GemOx, 97.0%) experienced at least 1 any-grade TEAE, and the majority experienced at least 1 any-grade treatment-related TEAE (M+R, 83.8%; M+R-GemOx, 93.9%). In both treatment groups, anemia was the most common grade ≥3 TEAE (M+R, 26.3%; M+R-GemOx, 60.6%). Specific safety results by treatment group are summarized in the subsequent sections.
M+R
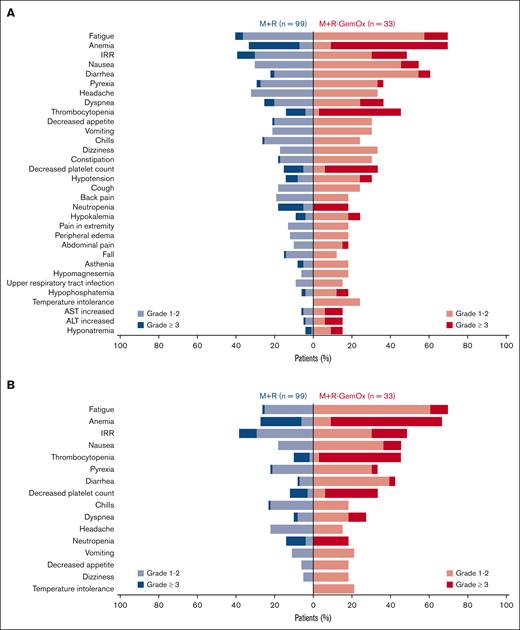
No DLTs occurred during the first 4 weeks of M+R treatment. The most common any-grade TEAEs in the M+R group were fatigue (40.4%), infusion-related reactions (IRRs; 39.4%), and anemia (33.3%) (Figure 1A); the most common any-grade treatment-related TEAEs were IRRs (38.4%), anemia (27.3%), and fatigue (26.3%; Figure 1B). The incidences of grade ≥3 TEAEs and serious TEAEs were 69.7% and 46.5%, respectively. Seven patients (7.1%) discontinued magrolimab because of treatment-related TEAEs (patients may have discontinued because of >1 treatment-related TEAE: grades 3/4 thrombocytopenia; grade 3 immune thrombocytopenia, leukopenia, neutropenia, acute myeloid leukemia; grade 2 pneumonitis; grade 1 malaise and fall). There were 12 deaths (8.3%) due to TEAEs; none were considered related to study treatment by the investigators. Of them, 8 deaths were due to PD, and 1 each due to TEAEs of atrial fibrillation/acute respiratory distress syndrome, gastric varices hemorrhage, “unknown cause,” and respiratory failure.
Summary of TEAEs in ≥15% of patients in either arm (safety analysis set). (A) TEAEs. (B) TEAEs related to any treatment. TEAEs in panels A and B ordered by combined frequency in M+R and M+R-GemOx arms. Treatment cohorts were independent; no formal comparison was performed. ALT, alanine aminotransferase; AST, aspartate aminotransferase.
Summary of TEAEs in ≥15% of patients in either arm (safety analysis set). (A) TEAEs. (B) TEAEs related to any treatment. TEAEs in panels A and B ordered by combined frequency in M+R and M+R-GemOx arms. Treatment cohorts were independent; no formal comparison was performed. ALT, alanine aminotransferase; AST, aspartate aminotransferase.
M+R-GemOx
The most common TEAEs in the M+R-GemOx group were anemia (69.7%), fatigue (69.7%), and diarrhea (60.6%; Figure 1A); the most common any-grade treatment-related TEAEs were fatigue (69.7%), anemia (66.7%), and IRRs (48.5%) (Figure 1B). The incidences of grade ≥3 TEAEs and serious TEAEs were 93.9% and 78.8%, respectively. Treatment-related TEAEs led to magrolimab discontinuation in 2 patients (6.1%) (1 grade 4 ventricular fibrillation, and 1 grade 5 colitis). The grade 4 ventricular fibrillation event was a DLT occurring in the 45-mg/kg cohort; no other DLTs were observed. There were 3 deaths (9.1%) in this treatment group due to TEAEs. Of them, 1 was due to PD and 1 each was due to TEAEs of COVID-19 and colitis; colitis (day 45) was considered to be related to M and/or GemOx.
Efficacy
In both treatment groups, responses were observed in the overall populations and across multiple high-risk subgroups, refractory disease, multiple lines due to refractoriness to prior therapy, age, and cell of origin (Tables 2 and 3). Specific efficacy results by treatment group are summarized in the subsequent sections.
M+R
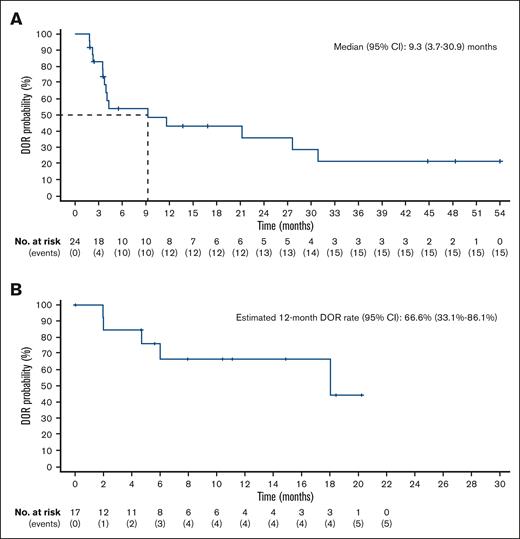
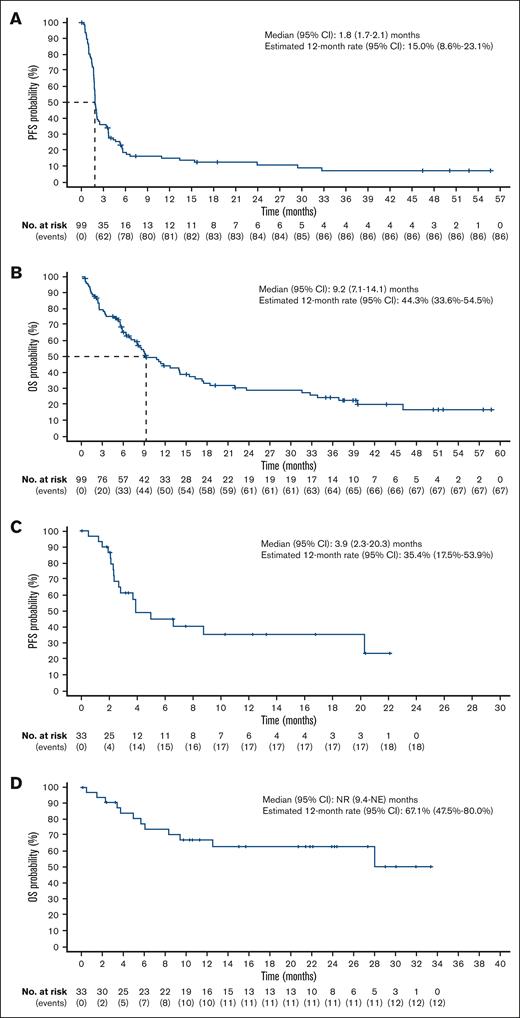
With a median follow-up of 7.9 months (range, 0.5-58.7), the ORR was 24.2%, including 12 patients (12.1%) with a CR (Table 2; supplemental Figures 2A and 3A). The median DOR was 9.3 months (95% CI, 3.7-30.9; Figure 2A; supplemental Figure 3B), and the median time to response was 1.8 months (range, 1.6-13.1). The median PFS was 1.8 months (95% CI, 1.7-2.1; Figure 3A), and the 12-month PFS rate was 15.0% (95% CI, 8.6-23.1). The median OS was 9.2 months (95% CI, 7.1-14.1; Figure 3B), and the 12-month OS rate was 44.3% (95% CI, 33.6-54.5).
DOR (efficacy analysis set). (A) M+R treatment group. (B) M+R-GemOx treatment group.
DOR (efficacy analysis set). (A) M+R treatment group. (B) M+R-GemOx treatment group.
PFS and OS (efficacy analysis set). (A) PFS, M+R treatment group. (B) OS, M+R treatment group. (C) PFS, M+R-GemOx treatment group. (D) OS, M+R-GemOx treatment group. NE, not estimable.
PFS and OS (efficacy analysis set). (A) PFS, M+R treatment group. (B) OS, M+R treatment group. (C) PFS, M+R-GemOx treatment group. (D) OS, M+R-GemOx treatment group. NE, not estimable.
M+R-GemOx
In this group, the ORR was 51.5%, with 13 patients (39.4%) achieving a CR, after a median follow-up of 11.3 months (range, 0.1-33.4) (Table 3; supplemental Figures 2B and 4A). The 12-month DOR rate was 66.6% (95% CI, 33.1-86.1; Figure 2B; supplemental Figure 4B), median time to response was 1.9 months (range, 1.8-3.4), and median duration of CR was not reached (NR; 95% CI, 6.0 to not estimable). The median PFS was 3.9 months (95% CI, 2.3-20.3; Figure 3C), and the 12-month PFS rate was 35.4% (95% CI, 17.5-53.9). The median OS was NR (95% CI, 9.40 to not estimable; Figure 3D), and the 12-month OS rate was 67.1% (95% CI, 47.5-80.8).
Exploratory analyses
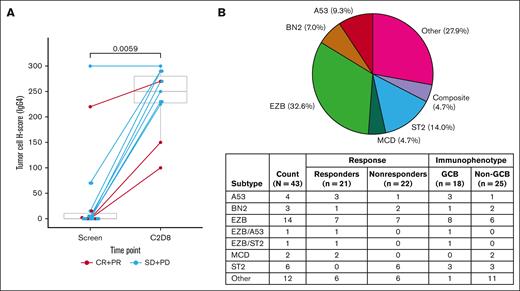
Twenty-eight patients had samples with CD20, CD47, or IgG4 staining. Paired comparisons (screen vs cycle 2, day 8) were only done for IgG4 (n = 11). For CD20 and CD47, only screening samples were analyzed (CD20, n = 23; CD47, n = 23). Baseline CD20 and CD47 staining were similar for responders and nonresponders (supplemental Figure 5). Magrolimab (via IgG4 staining) was detected in tumor biopsies after treatment (Figure 4A). The IgG4 H-score was close to 0 for the majority of patients at baseline and was higher at cycle 2, day 8 in responders and nonresponders alike.
Biomarker analyses. (A) Tumor cell immunohistochemistry H score for IgG4 (magrolimab) presence in tumor tissue biopsies. (B) LymphGen results. C, cycle; D, day; SD, stable disease.
Biomarker analyses. (A) Tumor cell immunohistochemistry H score for IgG4 (magrolimab) presence in tumor tissue biopsies. (B) LymphGen results. C, cycle; D, day; SD, stable disease.
Forty-three patients with WES data available were assigned genetic subtypes using the LymphGen algorithm. The overall classification rate was 72.1% (31/43 samples), including 2 samples classified as genetically composite, in line with other published uses of LymphGen.18 The majority of classified samples were EZB subtype (14/31, 45.2%), followed by ST2 subtype (6/31, 19.4%) and A53 (4/31, 12.9%). Only 1 of 18 (5.6%) GCB-DLBCL samples were unclassifiable, in comparison with 11 of 25 (44.0%) unclassifiable non-GCB samples. Of the GCB-DLBCL samples, EZB and EZB-composite samples were the most predominant (10/18, 55.6%). All 6 ST2 samples (100%) were from patients who were considered nonresponders (Figure 4B).
ctDNA data were collected from 9 patients (7 treated with M+R and 2 treated with M+R-GemOx), and most only had data from the first 2 cycles. Of them, 4 achieved a clinical response to treatment (2 CR, 2 PR) and 5 had PD. The 4 patients who achieved clinical response showed reductions of ctDNA, including 1 patient who achieved CR and had clearance of ctDNA at cycle 2, day 1 and cycle 3, day 1 (supplemental Figure 6). Four of 5 patients with PD were consistently ctDNA-positive and experienced either a rise in ctDNA or a decrease of <0.5-fold (supplemental Figure 6).
Discussion
Initial results from the phase 1b portion of this study demonstrated that M+R was well tolerated and induced CRs in patients with R/R DLBCL and rituximab-resistant disease.15 In this extended 3-year follow-up including phase 2 data, M+R continued to be well tolerated, with modest efficacy in patients with R/R DLBCL (ORR, 24%; CR, 12.1%) with no new safety signals observed. We also report initial results demonstrating the tolerability of M+R-GemOx in patients with R/R DLBCL, with modest efficacy.
There were no unexpected TEAEs in either treatment group, and their frequency attenuated with time; most occurred early after therapy (within 90 days of treatment initiation) and were manageable. The long-term safety/low-grade toxicity of M+R supports its combinability with other therapies, including GemOX, as assessed in this study. TEAEs observed in the M+R-GemOx group were generally consistent with those observed in previous studies of GemOx with/without rituximab in patients with R/R B-cell lymphomas, including DLBCL.5,6 As with previous magrolimab studies, on-target anemia was mitigated by use of a priming dose. Although anemia did still occur, hemoglobin normalized over time, consistent with prior observations showing increased hemoglobin levels over time with repeated magrolimab dosing.19 Regarding the treatment-related death in the present study, it is important to note that colitis is not known to be related to magrolimab use.
In both treatment groups, responses were seen across high-risk, heavily pretreated, and hard-to-treat subgroups (eg, older patients, aged ≥75 years). Extending the initial report of M+R in which median DOR had not been reached in patients with R/R DLBCL or indolent NHL,15 the current 3-year follow-up shows a median DOR of 9.3 months, a median PFS of 1.8 months, and a median OS of 9.2 months in patients with R/R DLBCL. With a longer follow-up and a larger sample size, the ORR for patients with R/R DLBCL treated with M+R was numerically lower than that observed in the initial report.15 The combination of M+R with GemOx at a median follow-up of 11.3 months resulted in modest responses (12-month DOR rate, 66.6%) and median OS that was NR at the time of data cutoff, regardless of the fact that many patients did not receive all chemotherapy cycles, lending credence to the activity of M+R. Although the ORR observed for patients treated with M+R-GemOx in this study is lower than that reported previously for R-GemOx in patients with R/R DLBCL,6 these treatments have, to our knowledge, not been compared in a head-to-head, randomized study, which limits interpretation. Nevertheless, the totality of the data support the exploration of CD47-based therapies in DLBCL.
Our biomarker analyses confirmed that magrolimab penetrates into tumor tissue. Additionally, although patient numbers were low, there was observable correlation between the clearance of ctDNA and objective response. There appeared to be no association between the achievement of a response after treatment and baseline levels of CD20/CD47 in tumor tissue. The relationships between local and systemic immune changes and response to M+R therapy warrant further study. LymphGen subtyping frequency/distribution results using WES data alone, or in conjunction with fluorescence in situ hybridization analysis of BCL2 or BCL6 gene fusion, were largely in line with those of previous publications. The dominant subtype found within these patients was EZB, followed by ST2 and A53. It is intriguing that 6 of 6 ST2 samples were from nonresponders, but given the small sample size, caution is advised when interpreting the data.
Since the inception of this study, novel treatments, such as CAR T cells (eg, axicabtagene ciloleucel, lisocabtagene maraleucel, and tisagenlecleucel), antibody-drug conjugates (eg, polatuzumab vedotin and loncastuximab tesirine), monoclonal antibodies (eg, tafasitamab), small-molecule inhibitors (eg, selinexor), and bispecific T-cell engagers (eg, epcoritamab and glofitamab), have become approved options for treating patients with R/R DLBCL.4 Nonetheless, outcomes remain poor for patients with refractory disease after ≥2 regimens and extremely poor for primary refractory disease or early relapse within 12 months of completion of first-line therapy.4 In addition, options such as CAR T-cell therapy remain limited to specialized centers and are not widely available. Our current results contribute to the growing understanding of combination regimens involving monoclonal antibodies aiming to achieve better efficacy and safety outcomes for patients with R/R DLBCL. Although our results support the long-term safety of M+R and show that M+R-GemOx is clinically active in R/R DLBCL and able to achieve remission without ASCT or CAR T-cell therapy in heavily pretreated patients with R/R DLBCL, this interpretation is limited by the lack of study randomization. Because all randomized studies of magrolimab in AML/MDS have been negative, no further development is being pursued. In the rapidly changing landscape of therapies for R/R DLBCL, the optimal role of CD47 blockade remains to be determined. Additional studies are needed to identify synergistic combinations and predictors of response.
Acknowledgments
The authors thank Himanshu Sethi (Natera, Inc) for his contributions to the biomarker analyses. Medical writing support for the development of this manuscript, under the direction of the authors, was provided by Miranda Bader-Goodman of Ashfield MedComms, an Inizio company, and funded by Gilead Sciences, Inc.
This study was funded by Gilead Sciences, Inc.
Authorship
Contribution: J.E.M., A.A., L.P., G.P.C., I.W.F., N.G., C.K., M.K., A.M., M.R., C.R., S.M.S., and R.A. contributed to data collection; G.H.-K. and Y.H. performed statistical analysis; Y.Z. participated in biomarker exploratory analysis; G.P.C. and R.A. led the study; and all authors had full access to all relevant data in the study, and have read, provided critical revisions, and approved the manuscript.
The current affiliation for C.R. is Department of Clinical Sciences, Obsidian Therapeutics, Redwood City, CA.
All authors confirm that they meet International Committee of Medical Journal Editors authorship criteria.
Conflict-of-interest disclosure: J.E.M.’s institution has received research funding on his behalf from Gilead Sciences, Inc, Atara Bio, CRISPR Therapeutics, Precision Biosciences, and Scripps Research Institute. A.A.’s institution has received research funding on his behalf from Forty Seven and Gilead Sciences, Inc. L.P. has received honoraria from Pfizer and Roche, and has received travel, accommodations, and/or expenses from Novartis. G.P.C. has received honoraria for speaker or consultancy work from Roche, Takeda, Kite Pharma/Gilead Sciences, Incyte, AstraZeneca, BeiGene, Novartis, SecuraBio, and AbbVie, and research funding from Pfizer, BeiGene, AstraZeneca, Amgen, Inc, and Bristol Myers Squibb. I.W.F. reports consultancy for AbbVie, AstraZeneca, BeiGene, Century Therapeutics, Genentech, Inc, Genmab, Hutchison MediPharma, Iksuda Therapeutics, InnoCare Pharma, Janssen, Kite Pharma, MorphoSys, Myeloid Therapeutics, Novartis, Nurix Therapeutics, Pharmacyclics, F. Hoffmann-La Roche Ltd, Secura Bio, Servier Pharmaceuticals, Takeda, TG Therapeutics, Verastem, Vincerx Pharma, and Xencor, and institutional research grants from AbbVie, Acerta Pharma, Agios, ArQule, AstraZeneca, BeiGene, Biopath, Bristol Myers Squibb, Calibr, Cancer and Leukemia Group B, Celgene, City of Hope National Medical Center, Constellation Pharmaceuticals, Curis, CTI Biopharma, Epizyme, Fate Therapeutics, Forma Therapeutics, Forty Seven, Genentech, Inc, Gilead Sciences, Inc, InnoCare Pharma, IGM Biosciences, Incyte, Infinity Pharmaceuticals, Janssen, Kite Pharma, Loxo, Merck, Millennium Pharmaceuticals, MorphoSys, Myeloid Therapeutics, Novartis, Nurix, Pfizer, Pharmacyclics, Portola Pharmaceuticals, Rhizen Pharmaceuticals, F. Hoffmann-La Roche Ltd, Seattle Genetics, Tessa Therapeutics, TCR2 Therapeutics, TG Therapeutics, Trillium Therapeutics, Triphase Research and Development Corp, Unum Therapeutics, and Verastem. N.G. has received consulting fees from Seagen, TG Therapeutics, AstraZeneca, Pharmacyclics, Janssen, Bristol Myers Squibb, Gilead Sciences, Inc, Kite Pharma, Syncopation, Lava Therapeutics, BeiGene, Incyte, Karyopharm, Roche/Genentech, Inc, Novartis, Loxo Oncology, Genmab, Adaptive Biotech, and ADC Therapeutics; previously served on speakers' bureaus for Gilead Sciences, Inc, AstraZeneca, Bristol Myers Squibb, Phamacyclics, Janssen, and Epizyme; and received research funding from TG Therapeutics, Roche/Genentech, Bristol Myers Squibb, Gilead Sciences, Inc, MorphoSys, and AbbVie. C.K. has received honoraria from Roche, Gilead Sciences, Inc, Merck Sharp and Dohme, AstraZeneca, Takeda, BeiGene, and Bristol Myer Squibb. M.K. has received consultancy fees from Roche, Antegene, and Genor Biopharm. A.M. has received research funding from Incyte Corp, Takeda, Forty Seven/Gilead Sciences, Juno Pharmaceuticals/Bristol Myers Squibb, Celgene/Bristol Myers Squibb, Innate Pharmaceuticals, Seattle Genetics, TG Therapeutics, Affimed, Merck, Kite Pharma/Gilead Sciences, F. Hoffmann-La Roche Ltd/Genentech, Inc, and ADC Therapeutics; consulting fees from Gilead Sciences, Inc, Seattle Genetics, Incyte Corp, MorphoSys, TG Therapeutics, Kyowa Kirin, BeiGene, F. Hoffmann-La Roche Ltd/Genentech, Inc, and ADC Therapeutics; and served on the speakers' bureaus for Incyte Corp/MorphoSys, BeiGene, Ipsen, and Kyowa Kirin. G.H.K. and Y.H. are employed by Gilead Sciences, Inc, and hold stock in Gilead Sciences, Inc. Y.Z. is employed by Gilead Sciences, Inc, and holds stock in Gilead Sciences, Inc, and Allogene Therapeutics, Inc. C.R. was employed by Gilead Sciences, Inc, at the time of the study and held stock in Gilead Sciences, Inc, and Alphabet Inc, Class A. S.M.S. reports consultancy for MorphoSys/Incyte, Janssen, Bristol Myers Squibb, Karyopharm, TG Therapeutics, and Celgene, and received research funding from FortySeven, TG Therapeutics, Pharmacyclics, Acerta, Karyopharm, Portola, Celgene, Novartis, Roche/Genentech, and Epizyme. R.A. has received research funding from BeiGene, Merck, Roche/Genentech, Inc, Seattle Genetics, ADC Therapeutics, Phamacyclics, Cyteir, and Daiichi Sankyo, and has served on advisory boards for Roche/Genentech, MorphoSys, and Epizyme. M.R. declares no competing financial interests.
Correspondence: Joseph E. Maakaron, Division of Hematology, Oncology and Transplantation, Department of Medicine, University of Minnesota, 420 Delaware St SE, MMC 480, Minneapolis, MN 55455; email: maaka001@umn.edu.
References
Author notes
Gilead Sciences shares anonymized individual patient data upon request or as required by law or regulation with qualified external researchers on the basis of submitted curriculum vitae and reflecting nonconflict of interest. The proposal must also include a statistician. Approval of such requests is at Gilead Science's discretion and is dependent on the nature of the request, the merit of the research proposed, the availability of the data, and the intended use of the data. Data requests should be sent to datarequest@gilead.com.
The full-text version of this article contains a data supplement.