Key Points
The CLL comorbidity index demonstrates prognostic significance in a large patient cohort, justifying its use in clinical care and research.
The CLL comorbidity index associates with time to first treatment, event-free survival, and overall survival in treatment-naive patients with CLL.
Abstract
The chronic lymphocytic leukemia comorbidity index (CLL-CI) is an efficient, CLL-specific tool derived from the Cumulative Illness Rating Scale. The CLL-CI is based on the assessment of the organ systems found to be most strongly associated with event-free survival (EFS) in CLL: vascular, upper gastrointestinal, and endocrine, at the time of initiation of CLL therapy. The CLL-CI categorizes patients into low, intermediate, and high risk groups. In the present study, we have employed the CLL-CI in a population-based cohort comprising 4975 patients with CLL. We demonstrate that CLL-CI retains prognostic significance in this large cohort and is associated with overall survival (OS) and EFS from time of first therapy. Furthermore, CLL-CI associates with OS, EFS, and time to first treatment from diagnosis independently of the CLL International Prognostic Index. These findings support the use of the CLL-CI both in research and in clinical practice.
Introduction
Advanced age and comorbid medical conditions are common and may influence outcomes in chronic lymphocytic leukemia (CLL).1,2 The International Workshop on CLL 2018 guidelines recommend assessment of comorbidities in patients enrolled in clinical trials,1 which is most commonly done using the Cumulative Illness Rating Scale (CIRS).3 We and others have previously demonstrated that CIRS correlates with survival and tolerance of therapy in CLL and non-Hodgkin lymphomas, including patients treated with chemoimmunotherapy, targeted agents, and chimeric antigen receptor T-cell therapy.4- 7 Despite the widespread use of CIRS in CLL research, it has not become part of common clinical practice.
The ideal method for measuring comorbidities in patients with CLL, particularly in a fast-paced clinical practice setting, has not been established. Furthermore, it remains unknown which comorbidities are most relevant to CLL outcomes. An analysis of the Danish CLL Register demonstrated an association between nearly all individual comorbidities and overall survival (OS),8 whereas findings from smaller studies regarding non-Hodgkin lymphomas are inconsistent.2,7,9 To address this matter, using a machine learning ensemble approach, we recently developed the CLL comorbidity index (CLL-CI) which is a user-friendly tool designed for clinical practice.10 We identified vascular, upper gastrointestinal, and endocrine CIRS categories as the most strongly associated with event-free survival (EFS) from time of treatment. These categories were combined to create the CLL-CI score, with each comorbidity category adding 1 point (0 = low risk; 1 = intermediate risk; 2-3 = high risk). The present study further investigates the clinical impact of the CLL-CI on EFS, time to first treatment (TTFT), and OS, at diagnosis and initiation of therapy, using a population-based cohort.
Methods
All patients registered with CLL in the Danish National CLL Register between 2008 and 2018 were included in the study.11 Baseline characteristics and information on first therapy were available from the CLL register, and further detailed information on treatment was obtained for a geographically defined subgroup through review of medical records. Information on comorbidities was collected from the Danish National Prescription Register and the Danish National Patient Register with look-back periods of 1 year and up to 20 years, respectively.12,13 Codes corresponding to comorbidities are listed in supplemental Table 1.3,10 CLL-CI was calculated at time of diagnosis and at time of first-line treatment. Data were linked across registers using a personal identification number unique to every citizen.14
Analyses were stratified based on CLL-CI score. χ2 and Kruskal–Wallis tests were performed to test for differences in characteristics across groups. Kaplan-Meier survival curves with associated P values were computed for OS and EFS (defined as time to death or next therapy) from 1 month after diagnosis and from the time of initiation of first-line therapy (OS2 and EFS2). Cumulative incidence curves and Fine-Gray risk regressions were used to study TTFT from time of diagnosis, treating death as a competing risk. Hazard ratios were calculated using multivariable Cox regressions for OS, EFS, and TTFT from diagnosis, adjusting for sex and CLL International Prognostic Index (CLL-IPI),15 both as score and using the individual components of the CLL-IPI. Multivariable Cox regressions were performed for OS2 and EFS2, adjusting for age, immunoglobulin heavy-chain variable region gene (IGHV) mutational status, and treatment regimen. Data analysis was performed using SAS software, version 9.4 (SAS Institute, Cary, NC) and R software version 3.5.2 on servers hosted by the Danish Health Data Authority.
The study was approved by the Danish Health and Medicine Authorities (jr. no. 3-3013-1141/1) and the Danish Data Protection Agency (jr. no. RH-2015-96 03856).
Results and discussion
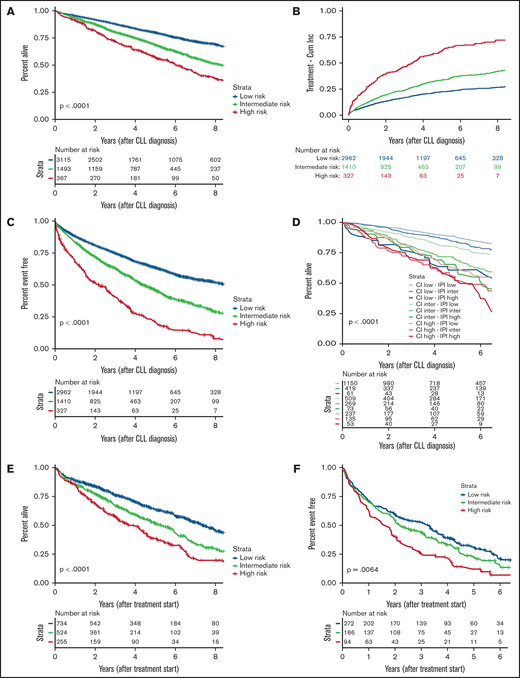
Baseline characteristics at time of CLL diagnosis for 4975 patients included in the study are presented in Table 1. In all, 63%, 30%, and 7% of patients had low, intermediate, and high risk CLL-CI, respectively. CLL-CI was associated with OS, with a median OS not reached, 8.5 years, and 6.0 years for low-, intermediate-, and high-risk patients, respectively (Figure 1A). CLL-CI was associated with TTFT, with 56% of high-risk patients being treated within 4 years compared with 20% to 30% of low- and intermediate-risk patients (Figure 1B). All comorbidity categories were individually associated with TTFT (supplemental Figure 1). CLL-CI was associated with EFS, with a median EFS of 8.4, 4.4, and 2.2 years for low-, intermediate-, and high-risk patients, respectively (Figure 1C). The association with OS, EFS, and TTFT was independent of sex and CLL-IPI (supplemental Tables 2 and 3). Patients with high risk in either or both CLL-CI and CLL-IPI had the poorest OS (Figure 1D).
Baseline data from time of CLL diagnosis for 4975 patients from the Danish CLL register diagnosed with CLL between 2008 and 2018
| . | Low risk (n = 3115) . | Intermediate risk (n = 1493) . | High risk (n = 367) . | Overall (n = 4975) . | P . |
|---|---|---|---|---|---|
| Follow-up (y) | <.0001 | ||||
| Median [Q1, Q3] | 4.55 [2.43, 7.11] | 4.21 [2.22, 6.57] | 3.90 [1.86, 6.23] | 4.39 [2.31, 6.88] | |
| Sex | .0042 | ||||
| Female (%) | 1270 (40.8) | 533 (35.7) | 142 (38.7) | 1945 (39.1) | |
| Male (%) | 1845 (59.2) | 960 (64.3) | 225 (61.3) | 3030 (60.9) | |
| Age at diagnosis (y) | <.0001 | ||||
| Median [Q1, Q3] | 68.9 [61.6, 76.1] | 73.2 [66.1, 80.0] | 75.1 [68.3, 80.7] | 70.7 [63.3, 78.1] | |
| Endocrinological disease | <.0001 | ||||
| Yes (%) | 0 (0) | 187 (12.5) | 204 (55.6) | 391 (7.9) | |
| No (%) | 3115 (100) | 1306 (87.5) | 163 (44.4) | 4584 (92.1) | |
| Upper gastrointestinal disease | <.0001 | ||||
| Yes (%) | 0 (0) | 216 (14.5) | 237 (64.6) | 453 (9.1) | |
| No (%) | 3115 (100) | 1277 (85.5) | 130 (35.4) | 4522 (90.9) | |
| Vascular disease | <.0001 | ||||
| Yes (%) | 0 (0) | 1090 (73.0) | 334 (91.0) | 1424 (28.6) | |
| No (%) | 3115 (100) | 403 (27.0) | 33 (9.0) | 3551 (71.4) | |
| IGHV status | <.0001 | ||||
| Mutated (%) | 1765 (56.7) | 734 (49.2) | 139 (37.9) | 2638 (53.0) | |
| Unmutated (%) | 701 (22.5) | 379 (25.4) | 117 (31.9) | 1197 (24.1) | |
| Missing (%) | 649 (20.8) | 380 (25.5) | 111 (30.2) | 1140 (22.9) | |
| Del(17p) | .0009 | ||||
| No (%) | 2606 (83.7) | 1181 (79.1) | 278 (75.7) | 4065 (81.7) | |
| Yes (%) | 141 (4.5) | 76 (5.1) | 32 (8.7) | 249 (5.0) | |
| Missing (%) | 368 (11.8) | 236 (15.8) | 57 (15.5) | 661 (13.3) | |
| Binet stage | <.0001 | ||||
| A (%) | 2572 (82.6) | 1216 (81.4) | 259 (70.6) | 4047 (81.3) | |
| B (%) | 393 (12.6) | 201 (13.5) | 69 (18.8) | 663 (13.3) | |
| C (%) | 150 (4.8) | 76 (5.1) | 39 (10.6) | 265 (5.3) | |
| β2-microglobulin >4.0 mg/L | <.0001 | ||||
| No (%) | 2134 (68.5) | 915 (61.3) | 180 (49.0) | 3229 (64.9) | |
| Yes (%) | 269 (8.6) | 195 (13.1) | 79 (21.5) | 543 (10.9) | |
| Missing (%) | 712 (22.9) | 383 (25.7) | 108 (29.4) | 1203 (24.2) | |
| CLL-IPI | <.0001 | ||||
| Low (%) | 1150 (36.9) | 419 (28.1) | 61 (16.6) | 1630 (32.8) | |
| Intermediate (%) | 509 (16.3) | 269 (18.0) | 73 (19.9) | 851 (17.1) | |
| High (%) | 192 (6.2) | 115 (7.7) | 47 (12.8) | 354 (7.1) | |
| Very high (%) | 45 (1.4) | 20 (1.3) | 6 (1.6) | 71 (1.4) | |
| Missing (%) | 1219 (39.1) | 670 (44.9) | 180 (49.0) | 2069 (41.6) | |
| . | Low risk (n = 3115) . | Intermediate risk (n = 1493) . | High risk (n = 367) . | Overall (n = 4975) . | P . |
|---|---|---|---|---|---|
| Follow-up (y) | <.0001 | ||||
| Median [Q1, Q3] | 4.55 [2.43, 7.11] | 4.21 [2.22, 6.57] | 3.90 [1.86, 6.23] | 4.39 [2.31, 6.88] | |
| Sex | .0042 | ||||
| Female (%) | 1270 (40.8) | 533 (35.7) | 142 (38.7) | 1945 (39.1) | |
| Male (%) | 1845 (59.2) | 960 (64.3) | 225 (61.3) | 3030 (60.9) | |
| Age at diagnosis (y) | <.0001 | ||||
| Median [Q1, Q3] | 68.9 [61.6, 76.1] | 73.2 [66.1, 80.0] | 75.1 [68.3, 80.7] | 70.7 [63.3, 78.1] | |
| Endocrinological disease | <.0001 | ||||
| Yes (%) | 0 (0) | 187 (12.5) | 204 (55.6) | 391 (7.9) | |
| No (%) | 3115 (100) | 1306 (87.5) | 163 (44.4) | 4584 (92.1) | |
| Upper gastrointestinal disease | <.0001 | ||||
| Yes (%) | 0 (0) | 216 (14.5) | 237 (64.6) | 453 (9.1) | |
| No (%) | 3115 (100) | 1277 (85.5) | 130 (35.4) | 4522 (90.9) | |
| Vascular disease | <.0001 | ||||
| Yes (%) | 0 (0) | 1090 (73.0) | 334 (91.0) | 1424 (28.6) | |
| No (%) | 3115 (100) | 403 (27.0) | 33 (9.0) | 3551 (71.4) | |
| IGHV status | <.0001 | ||||
| Mutated (%) | 1765 (56.7) | 734 (49.2) | 139 (37.9) | 2638 (53.0) | |
| Unmutated (%) | 701 (22.5) | 379 (25.4) | 117 (31.9) | 1197 (24.1) | |
| Missing (%) | 649 (20.8) | 380 (25.5) | 111 (30.2) | 1140 (22.9) | |
| Del(17p) | .0009 | ||||
| No (%) | 2606 (83.7) | 1181 (79.1) | 278 (75.7) | 4065 (81.7) | |
| Yes (%) | 141 (4.5) | 76 (5.1) | 32 (8.7) | 249 (5.0) | |
| Missing (%) | 368 (11.8) | 236 (15.8) | 57 (15.5) | 661 (13.3) | |
| Binet stage | <.0001 | ||||
| A (%) | 2572 (82.6) | 1216 (81.4) | 259 (70.6) | 4047 (81.3) | |
| B (%) | 393 (12.6) | 201 (13.5) | 69 (18.8) | 663 (13.3) | |
| C (%) | 150 (4.8) | 76 (5.1) | 39 (10.6) | 265 (5.3) | |
| β2-microglobulin >4.0 mg/L | <.0001 | ||||
| No (%) | 2134 (68.5) | 915 (61.3) | 180 (49.0) | 3229 (64.9) | |
| Yes (%) | 269 (8.6) | 195 (13.1) | 79 (21.5) | 543 (10.9) | |
| Missing (%) | 712 (22.9) | 383 (25.7) | 108 (29.4) | 1203 (24.2) | |
| CLL-IPI | <.0001 | ||||
| Low (%) | 1150 (36.9) | 419 (28.1) | 61 (16.6) | 1630 (32.8) | |
| Intermediate (%) | 509 (16.3) | 269 (18.0) | 73 (19.9) | 851 (17.1) | |
| High (%) | 192 (6.2) | 115 (7.7) | 47 (12.8) | 354 (7.1) | |
| Very high (%) | 45 (1.4) | 20 (1.3) | 6 (1.6) | 71 (1.4) | |
| Missing (%) | 1219 (39.1) | 670 (44.9) | 180 (49.0) | 2069 (41.6) | |
Patients are grouped by CLL comorbidity index category.
Survival and treatment outcomes according to CLL-CI. (A) OS from time of diagnosis. (B) TTFT from time of diagnosis, treating death as a competing risk. (C) EFS from time of diagnosis. (D) OS from time of diagnosis further stratified by CLL-IPI. (E) OS2 from time of first-line treatment. (F) EFS2 from time of first-line treatment. The x-axis in (B) and (D) differs from other panels.
Survival and treatment outcomes according to CLL-CI. (A) OS from time of diagnosis. (B) TTFT from time of diagnosis, treating death as a competing risk. (C) EFS from time of diagnosis. (D) OS from time of diagnosis further stratified by CLL-IPI. (E) OS2 from time of first-line treatment. (F) EFS2 from time of first-line treatment. The x-axis in (B) and (D) differs from other panels.
In total, 1513 patients received first-line treatment during follow-up (supplemental Table 4). Data from medical record review were available for 552 patients; information on targeted therapy was only available for these patients, of whom 6% received targeted agents. CLL-CI was associated with OS2 independently of IGHV status, age, and treatment regimen, with a median OS2 of 8.2, 6.0, and 4.4 years for low-, intermediate-, and high-risk patients, respectively (supplemental Table 5; Figure 1E). Similarly, CLL-CI was associated with EFS2, with a median EFS2 of 3.6, 2.9, and 1.9 years, respectively, although it did not retain significance after adjusting for IGHV status, age, and treatment regimen (supplemental Table 5; Figure 1F).
In this study, patients were assigned treatment regimens by treating physicians based on age, comorbidity, and patient preference. Differences in survival by type of treatment, particularly patients treated with targeted therapies, who were underrepresented in this study, could influence survival and limit the generalizability of these results. Whereas our findings demonstrate that CLL-CI can be applied also for cohorts predominantly treated with chemoimmunotherapy, the extrapolation of our results may be limited by the small number receiving targeted agents. However, 28% of patients receiving second-line treatment were treated with targeted agents.
In addition to associating with EFS and OS from time of diagnosis independently of CLL-IPI, we identified high-risk CLL-CI patients as having a shorter TTFT compared with low- and intermediate-risk patients. The underlying cause remains to be investigated; however, adverse prognostic biomarkers were more common in the CLL-CI high-risk group, suggesting the possibility of underlying mechanistic associations between comorbidities and aggressiveness of CLL.16 This could be due to underlying factors that influence both CLL biology and the development of comorbidities or the possibility that aggressive CLL causes comorbidities. Our working hypothesis is that the biological link among the CLL-CI, high-risk biomarkers, and shorter survival is chronic inflammation and immune dysfunction caused by metabolic syndrome, vascular disease, and dysbiosis. The endocrine category of the CLL-CI includes diabetes and obesity, which are features of metabolic syndrome, a well-established risk factor for the development of multiple cancer types that has been shown to influence cancer biology and the tumor microenvironment.17 Furthermore, most conditions included in the vascular category are also related to atherosclerosis and dyslipidemia, other features of metabolic syndrome. Major vascular events have also been demonstrated to accelerate cancer progression by modulating the immune system.18 Upper gastrointestinal disease, the third category in the CLL-CI, is associated with alterations in the intestinal microbiome.19 Decreased intestinal microbial biodiversity may be more frequent in patients with CLL.20,21 It is associated with inferior response to immunotherapy in patients with certain cancers22 and possibly in patients with CLL who receive chemotherapy.23 We are currently investigating these hypotheses.
It is also important to consider the CLL-CI in the context of other prognostic scales. Several prognostic indices have been developed for CLL that are specific to treatment settings and therapeutic classes but do not include a measure of comorbidity.24-27 Although the CLL-CI does add prognostic information to the CLL-IPI for all therapies currently evaluated, assessment of the influence of comorbidities alongside other prognostic scales is needed. Although prognostic factors should remain key for treatment decisions, clinical trial data from pivotal phase 3 trials with novel targeted agents versus chemoimmunotherapy should be reanalyzed with addition of CLL-CI to assess the optimal treatment of patients according to CLL-CI. Ultimately, however, prospective clinical trials are needed to define the optimal treatment of these patients.
In this study, we illustrate the feasibility of assessing the CLL-CI through register data. Findings support the use of the CLL-CI in both research and clinical practice as a quick and easy-to-use tool for assessing comorbidity in newly diagnosed patients with CLL as well as in patients requiring treatment.
Acknowledgments
The authors thank Erika Nodin for her assistance in identifying surgical procedure codes and Caspar da Cunha-Bang and Klaus Rostgaard for comments that improved this study.
This work was supported in part by grants from Novo Nordisk Foundation (NNF16OC0019302) (C.U.N.) and Neye Fonden (H.H.). A.V.D. is a Leukemia and Lymphoma Society Clinical Scholar (#2319-19).
Authorship
Contribution: E.C.R., M.J.G., H.H., A.V.D., and C.U.N. designed the research; H.F. and C.U.N. contributed patients; E.C.R. and N.V. collected the data; E.C.R. analyzed the data; E.C.R. and M.J.G. wrote the first draft of the paper; and all authors discussed the results and contributed to the final manuscript.
Conflict-of-interest disclosure: E.C.R. received consultancy fees or travel grants from AbbVie, Janssen Pharmaceuticals, and AstraZeneca. H.F. received support outside this work from Alexion, Gilead, AbbVie, Janssen Pharmaceuticals, and Novartis. H.H. received support from Neye Fonden outside this work. A.V.D. received consulting fees from AstraZeneca, AbbVie, BeiGene, Verastem Oncology, Genentech, TG Therapeutics, Nurix, Bayer Oncology, and Pharmacyclics and has ongoing research funding from AstraZeneca, Takeda Oncology, Gilead Sciences, Bayer Oncology, Genentech, SecuraBio, MEI, TG Therapeutics, and Bristol Myers Squibb all outside of this work. C.U.N. received support from Novo Nordisk Foundation (NNF16OC0019302) within this work and received support, consultancy fees, or travel grants from AbbVie, Gilead, Janssen Pharmaceuticals, Roche, CSL Behring, Acerta, Genmab, Sunesis Pharmaceuticals, and AstraZeneca outside this work. The remaining authors declare no competing financial interests.
Correspondence: Carsten U. Niemann, Department of Hematology, Rigshospitalet, Copenhagen University Hospital, Blegdamsvej 9, DK-2100 Copenhagen, Denmark; e-mail: carsten.utoft.niemann@regionh.dk.
References
Author notes
E.C.R. and M.J.G. contributed equally to this study.
Requests for data sharing may be submitted to Carsten U. Niemann (carsten.utoft. niemann@regionh.dk).
The full-text version of this article contains a data supplement.