Key Points
Fellows should have a methodology for PBS review and be competent in identifying morphology suggestive of both common and morbid diagnoses.
Curricular emphasis should be placed on the competency of identifying morphologic features of acute leukemias and hemolytic anemias.
Abstract
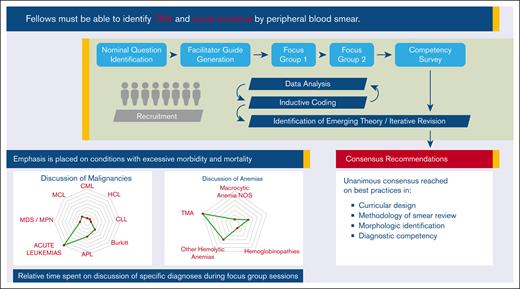
Graduate medical education training in hematology in North America is accredited by the Accreditation Council for Graduate Medical Education (ACGME). Trainees routinely review peripheral blood smears (PBS) in providing clinical care. Competency in PBS review at graduation is required by the ACGME. However, there are no consensus guidelines on best practices surrounding PBS review, education, or competency. We describe the generation of proposed theory and the consensus recommendations developed through a multi-institutional focus group, developed using constructivist grounded theory and a modified nominal group technique. Eight academic hematologists, spanning classical and malignant hematology, enrolled and participated in 2 one-hour focus groups. All routinely worked with fellows and half had formally instructed trainees on PBS interpretation. Focus group data were analyzed using mixed-methods techniques. Tenets of emerging theory were identified through inductive coding. Consensus recommendations (CR) were generated. Participants reviewed CR in an iterative fashion until consensus was reached. Strong consensus was reached on multiple aspects of PBS education. All agreed that trainees should learn PBS review through a systematic approach. Group discussion focused on disorders of red and white blood cells. The diagnoses of acute leukemia and thrombotic microangiopathies were most commonly discussed, with specific emphasis on disorders in which prompt recognition was required to avert significant patient morbidity. These CR offer external validity to future research and curricular development for both PBS review and other visuospatial tasks in medical education.
Introduction
The interpretation of peripheral blood smear (PBS) morphology is a core skill of the practicing hematologist and plays a key role in their ability to provide a timely diagnosis. The morphologic evaluation can reveal pathologic findings, which allow for timely diagnosis and rapid treatment for intracellular parasitic infections, hemolytic anemias, suspected thrombotic microangiopathies (TMA), and acute leukemias.1-4 However, the absence of pathologic findings required when diagnoses of exclusion, such as immune thrombocytopenia purpura, are under consideration.5
Identification of pathologic morphology on PBS is an acquired skill that requires iterative visuospatial training to allow for high fidelity object recognition. Object recognition theories suggest that iterative training and the repetitive exposure to unique combinations of visual stimuli, including shapes, contours, colors, and textures, are needed to develop rapid object recognition with retained fidelity.6-8 Hematologists in the United States hone these skills during fellowship training.
In North America, graduate medical education (GME) training programs are accredited by the Accreditation Council for Graduate Medical Education (ACGME). During the training, fellows routinely order and interpret PBSs under the supervision of an attending hematologist.9 The ACGME outlines fellowship specific milestones across several domains in an effort to ensure a minimum level of clinical exposure and competency across programs. The ACGME milestones for hematology mandate competency in the “interpretation of peripheral blood smears.”10 Despite this mandate, there neither is an established “gold standard,” nor are there published, peer-reviewed recommendations on the methodology of teaching PBS review.
Other medical specialties require trainees to be competent in the interpretation of analogous visuospatial tasks. Examples include the interpretation of radiographic images (radiology, pulmonology, and internal medicine), echocardiography (cardiology), anatomic pathology (pathology), and urine sediment (nephrology). Clinical competency in the use of echocardiographic imaging is among the most granular and developed among these, but is still largely based on expert consensus.11,12 There are no agreed upon interdisciplinary best practices in skill acquisition in object recognition despite the seemingly ubiquitous nature of visuospatial skill mastery at the GME level.
We convened a focus group of academic hematologists, well-versed in the clinical application and teaching of PBS review with the goal to develop a theoretical framework for PBS education at the GME level. Here, we describe proposed theory and the consensus recommendations (CR) of a multiinstitutional focus group, developed using constructivist grounded theory and modified nominal group technique (NGT).
Methods
A comprehensive literature review was completed using online databases and the assistance of an academic librarian to elucidate the current status of accepted theory on PBS review and analogous object recognition tasks at the GME level. No society guidelines or peer-reviewed literature on the ideal curricular structure, methodology of PBS review, or specific morphologic features and diagnoses necessary for fellow competency were found. The use of constructivist grounded theory was chosen given the paucity of empirical evidence and accepted theory on the subject. A modified NGT approach was selected to offer the greatest opportunity for robust and thorough idea generation. Study design was conducted using best practices published previously.13,14 This research was reviewed and deemed educationally exempted research by the institutional review board at Beth Israel Deaconess Medical Center.
Candidate focus group participants were academic hematologists with extensive personal expertise in the use of PBS review to aid in the identification of conditions commonly encountered in classical and malignant hematology. We sought to identify a sample of medical educators in the field of hematology who were wellversed in educational theory, hematology fellowship training, and instruction of PBS review. Total accrual was set between 5 and 10 participants. Prospective participants were identified through faculty lists from the American Society of Hematology Medical Educator Institute and the American Society of Hematology review series. Focus group participants provided verbal consent to be recorded during each session.
Nominal questions were developed by MC and included: (1) What are the best practices and methodology for PBS review? (2) What constitutes fellow competency in PBS at graduation? (3) Which domains of PBS should be evaluated by educators?
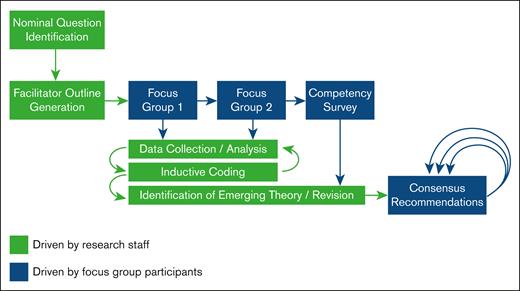
Generation of theory was accomplished through 2 focus group sessions. The minimum number of sessions were specified a priori (Figure 1). Termination of the focus group portion of the study was planned to occur when consensus was reached. Weak consensus and strong consensus were prespecified as 50% to 69% and 70% to 100% participant agreement, respectively.
Focus group 1 was conducted through a virtual meeting platform (Zoom, San Jose, CA) using a brief semistructured facilitator outline developed by MC (supplemental Appendix). Audiovisual recording was obtained using the videoconferencing platform and transcribed using online software (TEMI, San Francisco, CA). Transcripts were manually reviewed and edited for accuracy by MC. The facilitator guide for session 1 was created based on personal experience with PBS review and education. The specific topics of clinically relevant hematologic diagnoses and PBS morphologies were identified as possible discussion points before the focus group. A working list of diagnoses and morphologies was created through review of published hematology text books and online resources.15-19 This list was provided to participants at the end of session 1 to drive discussion at a more granular level.
Emergent categories were developed using participant statements through inductive coding in an iterative fashion. Statements were analyzed using mixed-methods analysis to give further insight into the relative time spent on discussion of each category and subcategory. These data were used to develop a semistructured facilitator guide for session 2. Categories and emerging tenets of the potential theory were reviewed with participants at the beginning of this session. Discussion of potential CR was directed by participants. Recording and transcription were completed as in session 1.
An updated list of prospective morphologies and diagnoses was distributed via email to participants after session 2. For each domain, each participant was assigned the level of training at which they felt a practitioner should have attained competency. These levels are as follows: (1) medical student, (2) internal medicine resident, (3) hematology fellow, (4) practicing hematologist (generalized), and (5) practicing hematologist (subspecialized). Rating levels 1 through 3 (medical student through fellow) were categorized as “required for fellow competency” whereas rating levels 4 and 5 were considered “aspirational.” Interrater reliability was assessed using percent agreement and a free-marginal multirater kappa statistics.20 The rating levels 4 and 5 were selected given the lack of a priori bias on the relative prevalence in each category of competency.
Potential CR were developed after the analysis of the focus group 2 transcript and the returned morphology and diagnosis list. Initial CR were disseminated to participants for revision and validation. Participants were asked to either agree with the proposed recommendation as written or disagree and offer textual edits. Participants were offered the ability to propose new recommendations or remove recommendations altogether. At least 2 rounds of iterative feedback were prespecified. Feedback was obtained via email. M.L.C. reviewed emails, anonymized feedback, and revised statements before each subsequent round of review.
Results
Study participants
In total, 12 academic hematologists were invited to participate in the focus group. Eight participants (3 female and 5 male) were enrolled (Table 1). The mean duration of post fellowship practice was 15.1 years (range, 5-33). The clinical focus of the participants spanned both classical and malignant hematology. All participants routinely worked with fellows. Half of them had previously, or were currently, responsible for teaching PBS interpretation to trainees. Attendance of focus group 1 and 2 was 87.5%. No participant missed >1 focus group session.
Participant demographics
| Age, mean (range), y | 48.0 (36-65) |
| Female gender, n (%) | 3 (37.5) |
| Years of practice, mean (range), y | 15.1 (5-33) |
| Proportion of time spent practicing classical hematology, mean (range) | 45.5 (0-95) |
| Formal teaching experience in PBS interpretation, n (%) | |
| Yes | 4 (50%) |
| Number of patients seen weekly, n (%) | |
| 20-29 | 2 (25) |
| 30-39 | 4 (50) |
| >40 | 2 (25) |
| Number of PBS reviewed annually, n (%) | |
| <25 | 1 (12.5) |
| 25-49 | 1 (12.5) |
| 50-75 | 3 (37.5) |
| >75 | 3 (37.5) |
| Age, mean (range), y | 48.0 (36-65) |
| Female gender, n (%) | 3 (37.5) |
| Years of practice, mean (range), y | 15.1 (5-33) |
| Proportion of time spent practicing classical hematology, mean (range) | 45.5 (0-95) |
| Formal teaching experience in PBS interpretation, n (%) | |
| Yes | 4 (50%) |
| Number of patients seen weekly, n (%) | |
| 20-29 | 2 (25) |
| 30-39 | 4 (50) |
| >40 | 2 (25) |
| Number of PBS reviewed annually, n (%) | |
| <25 | 1 (12.5) |
| 25-49 | 1 (12.5) |
| 50-75 | 3 (37.5) |
| >75 | 3 (37.5) |
Proposed PBS review consensus statements
| Curricular considerations | |
| 1 | Education across the fellowship should incorporate both slides derived from patients under the care of the fellow as well as slides from formal slide libraries of high yield morphologies |
| 2 | Trainees should be well versed in the description of normal and pathologic nuclear and cytoplasmic characteristics |
| 3 | Curricula should include education on how PBS review can augment, or potentially eliminate the need for, more advanced testing |
| 4 | Discussions of the practical use of PBS review should occur within the context of the medical system as a whole with specific attention devoted to discussions of:(a)Avoiding clinically relevant delays in diagnosis and treatment(b)Providing care in resource limited settings(c)Cost of care and financial toxicity of advanced diagnostic testing |
| 5 | Trainees should be aware of and familiar with intracellular parasites (malaria, babesia, ehrlichia/anaplasma) regardless of their geographic location of training |
| Method of review | |
| 1 | Trainees should be taught to systematically review a PBS. This includes specific education on identification of the monolayer, use of various magnifications, switching between magnification, and systematic review of each cell line |
| 2 | Learners should be competent in the personal use of a compound light microscope, and should receive hands on training throughout fellowship |
| 3 | Learners should be made aware of limitations associated with the use of digital and remote microscopy use |
| Morphology | |
| 1 | Emphasis should be placed on(a)Disorders where correct and timely diagnosis is paramount to avoiding significant patient morbidity, acute decompensation, or death(b)Commonly encountered diagnoses |
| 2 | Trainees should be able to identify features of normal PBSs |
| 3 | Specific curricular emphasis should be placed on the morphologic presentation of acute leukemias and hemolytic anemias, including TMA |
| Disorders of white blood cells | |
| Trainees should be able to: | |
| 1 | Distinguish reactive leukocytosis from malignant processes |
| 2 | Identify blasts and myeloid precursors |
| 3 | Recognize evidence of myeloid dysplasia in peripheral blood |
| 4 | Identify the following cells on a PBS: atypical (reactive) lymphocytes, large granular lymphocytes, mature lymphocytes, mature myeloid cells, and immature myeloid precursors |
| 5 | Identify circulating promyelocytes, specifically in the context of suspected acute promyelocytic leukemia |
| Disorders of red blood cells | |
| Trainees should be able to: | |
| 1 | Readily identify peripheral smear evidence of TMA, with specific emphasis on identification of schistocytes |
| 2 | Hypothesize the mechanism of hemolytic anemia based upon red blood cell morphology and the presence of poikilocytes |
| 3 | Identify sickle cell morphology |
| 4 | Identify morphologic findings seen in thalassemias, specifically in the absence of other clinical data such as family history, hemoglobin electrophoresis, and genetic testing |
| Disorders of platelets | |
| Trainees should be able to: | |
| 1 | Identify platelet clumping (satellitism) |
| 2 | Recognize variation in platelet size |
| 3 | Identify relative thrombocytosis or thrombocytopenia |
| All statements had unanimous consensus and exceeded the prespecified threshold (>70%) for strong consensus. | |
| Curricular considerations | |
| 1 | Education across the fellowship should incorporate both slides derived from patients under the care of the fellow as well as slides from formal slide libraries of high yield morphologies |
| 2 | Trainees should be well versed in the description of normal and pathologic nuclear and cytoplasmic characteristics |
| 3 | Curricula should include education on how PBS review can augment, or potentially eliminate the need for, more advanced testing |
| 4 | Discussions of the practical use of PBS review should occur within the context of the medical system as a whole with specific attention devoted to discussions of:(a)Avoiding clinically relevant delays in diagnosis and treatment(b)Providing care in resource limited settings(c)Cost of care and financial toxicity of advanced diagnostic testing |
| 5 | Trainees should be aware of and familiar with intracellular parasites (malaria, babesia, ehrlichia/anaplasma) regardless of their geographic location of training |
| Method of review | |
| 1 | Trainees should be taught to systematically review a PBS. This includes specific education on identification of the monolayer, use of various magnifications, switching between magnification, and systematic review of each cell line |
| 2 | Learners should be competent in the personal use of a compound light microscope, and should receive hands on training throughout fellowship |
| 3 | Learners should be made aware of limitations associated with the use of digital and remote microscopy use |
| Morphology | |
| 1 | Emphasis should be placed on(a)Disorders where correct and timely diagnosis is paramount to avoiding significant patient morbidity, acute decompensation, or death(b)Commonly encountered diagnoses |
| 2 | Trainees should be able to identify features of normal PBSs |
| 3 | Specific curricular emphasis should be placed on the morphologic presentation of acute leukemias and hemolytic anemias, including TMA |
| Disorders of white blood cells | |
| Trainees should be able to: | |
| 1 | Distinguish reactive leukocytosis from malignant processes |
| 2 | Identify blasts and myeloid precursors |
| 3 | Recognize evidence of myeloid dysplasia in peripheral blood |
| 4 | Identify the following cells on a PBS: atypical (reactive) lymphocytes, large granular lymphocytes, mature lymphocytes, mature myeloid cells, and immature myeloid precursors |
| 5 | Identify circulating promyelocytes, specifically in the context of suspected acute promyelocytic leukemia |
| Disorders of red blood cells | |
| Trainees should be able to: | |
| 1 | Readily identify peripheral smear evidence of TMA, with specific emphasis on identification of schistocytes |
| 2 | Hypothesize the mechanism of hemolytic anemia based upon red blood cell morphology and the presence of poikilocytes |
| 3 | Identify sickle cell morphology |
| 4 | Identify morphologic findings seen in thalassemias, specifically in the absence of other clinical data such as family history, hemoglobin electrophoresis, and genetic testing |
| Disorders of platelets | |
| Trainees should be able to: | |
| 1 | Identify platelet clumping (satellitism) |
| 2 | Recognize variation in platelet size |
| 3 | Identify relative thrombocytosis or thrombocytopenia |
| All statements had unanimous consensus and exceeded the prespecified threshold (>70%) for strong consensus. | |
Focus group results
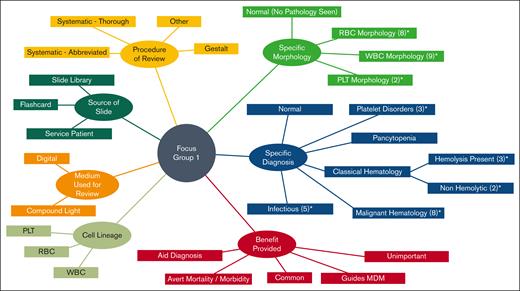
Transcribed statements from focus group 1 were coded thematically in an iterative fashion. Individual statements could be coded in several thematic categories if multiple dimensions were identified. Major emerging thematic categories included benefit provided by PBS review, cell lineage, medium used for PBS review, procedure of PBS review, source of slide, specific diagnosis, and specific morphology (Figure 2). Subtopics were developed within each theme.
Participant statement coding. Statements were categorized and subcategorized following inductive coding. Seven emerging domains of theory are shown. Subdomains are noted where applicable. ∗Further subcategorization can be found in the supplemental Data. The number of further subcategories are noted in parentheses.
Participant statement coding. Statements were categorized and subcategorized following inductive coding. Seven emerging domains of theory are shown. Subdomains are noted where applicable. ∗Further subcategorization can be found in the supplemental Data. The number of further subcategories are noted in parentheses.
Most discussion centered on specific cell lineage (32.8% of the statements), specific diagnosis (39.7% of the statements), and specific morphology (26.0% of the statements). The procedure of PBS review was discussed the least (9.2% of the statements).
Participants reported the majority of their slides for PBS teaching as having originated from clinic or consult service patients currently being seen by the educator or trainee. Some voiced the importance of reviewing PBSs from collated slide libraries to ensure that trainees get a full breadth of exposure. Thorough systematic review was most commonly discussed as the appropriate method for trainee review, whereas some noted abbreviated methods were used in clinical practice by attending hematologists.
White blood cells and red blood cells accounted for the vast majority of cell lineage–based discussion (48.8% and 41.9%, respectively). The most commonly discussed morphologies were schistocytes, spherocytes, blasts, and macro-ovalocytes (supplemental Appendix). Acute leukemia (including acute promyelocytic leukemia), TMA, and hemolytic anemias were the most discussed diagnostic subcategories.
Several benefits of PBS review were stated. First, PBS review is often available at the time of consultation which can improve time to initial diagnosis. The rapid availability to review PBS is specifically important because it pertains to confirming or refuting “can’t miss diagnoses” that convey a high likelihood of morbidity or mortality if misdiagnosed. Furthermore, the identification of morphologic characteristics informs Bayesian reasoning and aid in clinical decision making, and in turn, allows for early initiation of therapeutic interventions.
Scope of fellow competency
A total of 50 morphologic features and 26 morphologic diagnoses were coded by all 8 participants as either being required for fellow competency or as aspirational (Tables 3 and 4). Substantial interrater agreement was noted for each (k = 0.76 and k = 0.68, respectively). The percentage of interrater agreement on morphology was 87.8% and for morphologic diagnoses, 84.2%. Only 4 morphologic features (4/50, 8%) and 6 diagnoses (6/26, 23%) were felt to be beyond the level of competency for a graduating hematology fellow. These features included Sézary cells, Pappenheimer bodies, hypogranular platelets, and the distinction between monocytes and monoblasts. Identification of mantle cell lymphoma in circulation, myelodysplastic syndrome, May-Hegglin anomaly, T-cell leukemias, and the differentiation of acute myeloid leukemia from acute lymphoblastic leukemia, were said to be aspirational.
Proposed morphologies required for fellow competency at graduation
| White blood cells . | Red blood cells . | Platelets . |
|---|---|---|
| Atypical lymphocyte (reactive) | Acanthocyte | Platelet clumping (satellitism) |
| Band | Agglutination (RBC) | Platelet (giant) |
| Basophil | Basophilic stippling | Platelet (normal) |
| Blast (undifferentiated) | Bite cell | Thrombocytopenia |
| Döhle bodies | Blister cell | |
| Dysplastic neutrophil | Burr cell | |
| Eosinophil | Heinz body | |
| Hairy cell | Howell-Jolly body | |
| Hypersegmented neutrophil | Hypochromia | |
| Hypogranular neutrophil | Macrocytic | |
| LGL | Microcyte | |
| Lymphocyte (mature) | Nucleated RBC | |
| Metamyelocyte | Ovalocyte | |
| Morula (inclusion) | Polychromatophil | |
| Myeloblast with Auer rod | Ring form (malaria) | |
| Myelocyte | Schistocyte | |
| Neutrophil | Sickle cell | |
| Neutrophil with toxic granulation | Spherocyte | |
| Plasma cell | Stomatocyte | |
| Promyelocyte | Target cell | |
| Teardrop (dacrocyte) | ||
| Tetrad (babesia) |
| White blood cells . | Red blood cells . | Platelets . |
|---|---|---|
| Atypical lymphocyte (reactive) | Acanthocyte | Platelet clumping (satellitism) |
| Band | Agglutination (RBC) | Platelet (giant) |
| Basophil | Basophilic stippling | Platelet (normal) |
| Blast (undifferentiated) | Bite cell | Thrombocytopenia |
| Döhle bodies | Blister cell | |
| Dysplastic neutrophil | Burr cell | |
| Eosinophil | Heinz body | |
| Hairy cell | Howell-Jolly body | |
| Hypersegmented neutrophil | Hypochromia | |
| Hypogranular neutrophil | Macrocytic | |
| LGL | Microcyte | |
| Lymphocyte (mature) | Nucleated RBC | |
| Metamyelocyte | Ovalocyte | |
| Morula (inclusion) | Polychromatophil | |
| Myeloblast with Auer rod | Ring form (malaria) | |
| Myelocyte | Schistocyte | |
| Neutrophil | Sickle cell | |
| Neutrophil with toxic granulation | Spherocyte | |
| Plasma cell | Stomatocyte | |
| Promyelocyte | Target cell | |
| Teardrop (dacrocyte) | ||
| Tetrad (babesia) |
LGL, large granular lymphocyte; RBC, red blood cells.
Proposed diagnoses required for fellow competency at graduation
| Acute leukemia |
| Acute promyelocytic anemia |
| Anaplasmosis/ehrlichiosis |
| Anemia - AIHA |
| Anemia - iron deficiency |
| Anemia - megaloblastic |
| Atypical lymphocytosis |
| Babesiosis |
| CLL |
| CML |
| Dimorphic RBC population (previous transfusion) |
| Hairy cell leukemia |
| ITP |
| Malaria |
| Myelophthisic anemia |
| Normal PBS |
| Platelet clumping |
| Reactive leukocytosis |
| Sickle cell anemia |
| Thalassemia |
| TMA/MAHA |
| Acute leukemia |
| Acute promyelocytic anemia |
| Anaplasmosis/ehrlichiosis |
| Anemia - AIHA |
| Anemia - iron deficiency |
| Anemia - megaloblastic |
| Atypical lymphocytosis |
| Babesiosis |
| CLL |
| CML |
| Dimorphic RBC population (previous transfusion) |
| Hairy cell leukemia |
| ITP |
| Malaria |
| Myelophthisic anemia |
| Normal PBS |
| Platelet clumping |
| Reactive leukocytosis |
| Sickle cell anemia |
| Thalassemia |
| TMA/MAHA |
AIHA, autoimmune hemolytic anemia; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; ITP, immune thrombocytopenia purpura; MAHA, microangiopathic hemolytic anemia.
Consensus recommendation generation
Previously coded data were used to develop 4 domains of recommendations, ie, curricular considerations, method of PBS review, morphologic considerations, and specific disorders. Disorders were further subcategorized into disorders of white blood cells, red blood cells, and platelets. Response rates per round of revision were 87.5%, 87.5%, and 100%.
Strong and unanimous consensus was reached on multiple aspects of PBS education, including curricular considerations, method of review, and morphology (Table 2). All agreed that trainees should learn PBS review through a structured approach that includes the identification of monolayer, use of various magnifications, switching between magnifications, and systematic review of each cell line. Procurement of PBS slides should encompass both patients under the care of the trainee and slide “libraries” to ensure all trainees see similar morphology regardless of personal experience on ward and consult rotations.
Ideal curricula should include education on how PBS review can augment or eliminate the need for more advanced testing and should include discussions on the practical use of PBS within the context of resource limited vs resource rich settings. Trainees should be aware of the growing use of digital microscopy and understand the benefits and limitations of digital microscopy.
Trainees should be able to name and identify common cytoplasmic and nuclear features that aid in diagnosis. CR on individual disorders of white blood cells, red blood cells, and platelets can be seen in Table 2. Participants agreed that specific emphasis should be placed on disorders in which correct and timely diagnosis is paramount to avoiding significant patient morbidity, acute decompensation, or death. Acute leukemias and hemolytic anemias, specifically TMA, were felt to warrant explicit curricular emphasis. Conversely, fellows should also be competent in the recognition of commonly encountered diagnoses that are more indolent in nature, eg, iron deficiency anemia. However, consensus was not reached on how to balance education in these competing interests.
Discussion
Interpretation of the PBS is an essential skill of a practicing hematologist. To the best of our knowledge, through this study we have developed and proposed CR that are the first to appear in a peer-reviewed publication. The methodology described herein offers a potential framework for others to discuss and propose consensus on analogous visuospatial and object recognition tasks within the medical specialties.
Several themes emerge from our CR. First, all fellows in ACGME accredited hematology and hematology-oncology training programs should meet minimum levels of competency upon graduation. A trainee’s desire to specialize in a nonhematology focused field should not obviate the need for training in PBS review. Learners are likely to benefit most from interactions with a core group of educators. The exact qualifications and scope of practice of these educators is best determined locally because it is possible that there will be significant variability in expertise among clinical hematologists and hematopathologists across training programs. Curricula should be designed to ensure a broad level of education, and when possible, incorporate patient cases under trainee care. The use of “slide libraries” is of specific importance in the case of rare diagnoses, or common diagnoses that may not be seen owing to referral bias. Specifically, a trainee may not encounter patients with sickle cell disease, or endemic parasitic infections unless they are trained at a center with sufficient sample volume.
Manual review of the PBS via light microscopy or digital whole slide imaging is strongly preferred over single high-power field images. Independent use of the compound light microscope is a mandatory skill that should be attained by graduation. Expertise in the identification of normal morphology aids in the recognition of more subtle pathology on PBS. Trainees should be wellversed in the identification of both normal and pathologic cytoplasmic and nuclear characteristics. The identification of staining and preparation artifact is necessary to allow for proper clinical reasoning. Curricula should emphasize the utility of PBS in the context of contemporary testing as it can augment or eliminate the need for other diagnostic testing, minimize medical waste, and reduce time to diagnosis. Adept fellows will contextualize PBS morphology within the greater clinical context of the patient’s clinical history, laboratory, and pathologic data; and harbor an understanding of how positive and negative PBS findings affect Bayesian reasoning. Trainees should have a thorough and reproducible methodologic approach to PBS evaluation, although all educators need not be expected to teach a uniform approach across all ACGME training institutions. Specific emphasis should be placed on distinction of malignant and benign etiologies of leukocytosis and lymphocytosis. Finally, trainees should identify morphology suggestive of hemolytic anemias and suspect specific diagnoses based on PBS review with otherwise limited clinical information. In the institutions, participants practice with high resource availability and low exposure to tropical diseases. It was felt that the outsized global impact of malaria (247 million cases, and 619 000 deaths in 2021) warranted specific attention.21
Broad consensus existed on the specific morphologies and diagnoses within the fellow’s purview. This is an important development that can guide PBS curricular design (Tables 3 and 4). The high interrater agreement on included morphology and diagnoses indicates that hematologists likely have a shared mental model of what constitutes fellow competency, despite the lack of current formally accepted theory.
Qualitative data from the focus group sessions offer potential insights into the importance that participants place in various aspects of fellow competency. The high proportion of time spent on the specific diagnoses of acute leukemia and TMA possibly indicates a bias among attending hematologists to place heightened emphasis on the recognition of these conditions. The domains of PBS review do not appear to be weighted equally in the minds of hematologists, with an excess of attention focused on conditions that predispose patients to a high risk of short-term morbidity and mortality. Similarly, the relatively minimal discussion on the identification of abnormal platelet morphology and primary disorders of platelets potentially indicates a relative perceived lack of importance.
The utility of an agreed upon definition of competency has applications that extend beyond curricular development and include the validation of assessment tools and new technologies. More than half of the participants in this study are currently using remote digital microscopy or whole slide imaging (WSI) in clinical practice. WSI platforms with artificial intelligence augmented cellular recognition algorithms are Food and Drug Administration approved and may become part of routine clinical practice.22-24 Future trainees are likely to participate in curricular activities aimed at developing competency with these platforms. Validated consensus on best practices of PBS education are a necessary part of the evolution and use of new platforms for educational purpose and for assessment.
There are several limitations to be acknowledged in our study. First, our results pertain to the clinical hematology fellow within the United States. Our results may or may not apply to parallel fields, such as hematopathology and may not apply to clinical hematology in other countries.
Second, there are several limitations related to the characteristics of the cohort. All participants were academic hematologists, selected through a convenience sampling. Ascertainment bias may lead to a skewed description of the utility of PBS review. Of the 6 invited participants who were identified as female, only 3 participated. Our cohort mirrors the gender disparity seen within the hematology and oncology workforce as well as female representation in board review courses.25,26 Reasons for underrepresentation are multifaceted.27 Commentary on gender disparities and their impact on PBS education were solicited from female participants. None reported gender disparities within this area. Participants were older than their implied trainees. Participant’s age ranged from 36 to 65 years despite approximately all current trainees being millennials. The evolution of education for millennial learners and the benefit from contemporary methodology, such as e-learning, gamification, peer to peer teaching, and teaching via social media, is well described.28 The qualifications of participants (4 program directors and 4 American Society of Hematology Medical Educator Institute faculty) likely mitigate this discrepancy in age. The sole practice setting for participants was the academic medical center. Further investigation into the differences in the methodology, utility, and application of PBS review in clinical practice between academic and community hematologists is warranted.
Third, there are limitations that are generalizable to all NGT studies. These include the potential for 1 group member to dominate discussion and the associated social pressures and lack of anonymity that may discourage completely open discussion particularly around points of controversy. The lack of independent time for reflection and response is unique to NGT when compared with the Delphi method. Participants were provided several weeks between focus group sessions and were asked to participate in iterative ranking and statement revision following focus group 2 in an effort to minimize this effect.
Fourth, our study only examined the perspectives of educators, and was not designed to understand the learner’s perspective or the mechanisms of cognitive processing leading to skill acquisition. Participants lacked agreement on when individual competency in PBS skills were acquired (supplemental Data). In the most disparate cases, responses indicated that the range of expected training level at skill acquisition and competency may span from the undergraduate medical education level through attending hematologist. It is possible that this is a result of bias, specifically “the curse of knowledge” and ascertainment bias if raters teach PBS review only at the undergraduate medical education or GME-level.
Fifth, is the philosophical argument that the skill of PBS evaluation is required for only a subset of hematology-oncology fellowship graduates. We dispute this characterization and suggest that our biases as academic hematologists skew our perception in this regard. Arguments against rigorous education in PBS review include the assumption that many trainees will focus on oncology, the proposed trend toward more specialization within hematology, and the increasing accessibility of hematopathology review. These are important considerations, and admittedly, dual board certification in hematology and oncology is not required for fellows participating in ACGME programs. However, approximately one-third of 2018 graduates from combined hematology-oncology training programs planned on having a career in hematology alone whereas another approximately one-third planned on having a combined career in hematology and oncology.29 Furthermore, only half of the graduating fellows desire to enter into practice at an academic center, and thousands of board certified physicians provide hematology consultative care in a private practice model.30 This characterization further ignores the near essential function that fellows provide in many academic settings during their tenure.31,32 As 1 participant remarked “… I want the fellows to be competent while they're in our fellowship program, because they're taking call at night, they're taking call on the weekends …”.
We suggest that PBS review is an essential skill for all hematology trainees regardless of professional aspirations or potential disease specification within hematology-oncology. Hematology fellowships would benefit from the adoption of formal guidelines that clearly delineate what constitutes competency in PBS review at the time of graduation. Adoption of peer-reviewed consensus would lend external validity to innovative and rigorous research within PBS education and assessment.
Authorship
Contribution: M.L.C., J.B., and J.A.F. contributed to the study design; M.L.C. designed and facilitated focus group discussions (all but M.L.C. and J.B. participated in the focus group sessions), wrote the manuscript, and performed statistical analysis; and all authors read and agreed on the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Matthew L. Chase, Division of Hematology and Hematologic Malignancies and Division of Medical Oncology, Beth Israel Deaconess Medical Center, 330 Brookline Ave, Boston, MA 02131; e-mail: mlchase@bidmc.harvard.edu.
References
Author notes
Data are available on request from the corresponding author, Matthew L. Chase (mlchase@bidmc.harvard.edu).
The full-text version of this article contains a data supplement.