Key Points
EPO induction in the kidney, but not the liver, is essential for the therapeutic effects of HIF activators (HIF-PHIs) in renal anemia.
HIF-PHIs indirectly, but not directly, suppress hepcidin production through EPO induction in the kidney.
Abstract
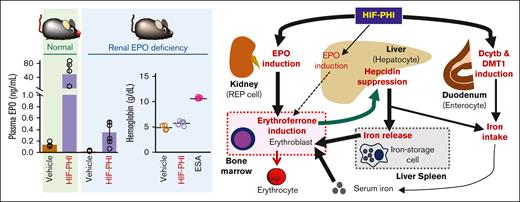
The erythroid growth factor erythropoietin (EPO) is mainly produced by the kidneys in adult mammals and induces expansion of erythroid cells and iron use for hemoglobin synthesis. The liver also produces EPO at a lower level than the kidneys. Renal and hepatic EPO production is fundamentally regulated by hypoxia-inducible transcription factors (HIFs) in a hypoxia/anemia-inducible manner. Recently, small compounds that activate HIFs and EPO production in the kidneys by inhibiting HIF-prolyl hydroxylases (HIF-PHIs) have been launched to treat EPO-deficiency anemia in patients with kidney disease. However, the roles of the liver in the HIF-PHI–mediated induction of erythropoiesis and iron mobilization remain controversial. Here, to elucidate the liver contributions to the therapeutic effects of HIF-PHIs, genetically modified mouse lines lacking renal EPO-production ability were analyzed. In the mutant mice, HIF-PHI administration marginally increased plasma EPO concentrations and peripheral erythrocytes by inducing hepatic EPO production. The effects of HIF-PHIs on the mobilization of stored iron and on the suppression of hepatic hepcidin, an inhibitory molecule for iron release from iron-storage cells, were not observed in the mutant mice. These findings demonstrate that adequate induction of EPO mainly in the kidney is essential for achieving the full therapeutic effects of HIF-PHIs, which include hepcidin suppression. The data also show that HIF-PHIs directly induce the expression of duodenal genes related to dietary iron intake. Furthermore, hepatic EPO induction is considered to partially contribute to the erythropoietic effects of HIF-PHIs but to be insufficient to compensate for the abundant EPO induction by the kidneys.
Introduction
Erythropoietin (EPO), an essential growth factor for erythroid cells, is produced mainly from renal interstitial fibroblasts (renal EPO-producing [REP] cells) and secondarily from hepatocytes in adult mammals.1-3 EPO production is fundamentally regulated at the EPO gene transcription level in a hypoxia-inducible manner.4 As hypoxia-dependent transcription is generally controlled by hypoxia-inducible transcription factor 1α (HIF1α) and/or HIF2α, Epo gene expression is induced by HIF2α either in REP cells or hepatocytes.5-7 HIFα proteins are hydroxylated by prolyl-hydroxylase domain–containing proteins (PHDs) and then degraded through the ubiquitin-proteasome pathway under normal oxygen conditions (normoxia).8-10 Because PHDs require oxygen molecules for their catalytic activity, hypoxia inactivates PHDs and stabilizes HIFα proteins as active transcription factors.
Kidney disease conditions impair the EPO-production ability of REP cells and reciprocally induce hepatic EPO production.11,12 However, chronic kidney disease often accompanies EPO-deficiency anemia (renal anemia) due to insufficient EPO production in the liver to compensate for the loss of renal EPO production.13 To treat renal anemia, erythropoiesis-stimulating agents (ESAs), derivatives of recombinant human EPO, have been used for >30 years. However, ESAs are often not suitable to patients with renal anemia with functional iron deficiency with high-level hepatic production of hepcidin, a negative regulator of iron excretion from iron-storage cells, which causes insufficient hemoglobin production in erythroid cells.14
We previously reported that renal anemia is caused by constitutive activation of PHDs in REP cells under kidney disease conditions, which leads to permanent suppression of HIF2α and inadequate production of EPO.7 Therefore, small molecules inhibiting PHDs have been anticipated as potential treatments for renal anemia. Since 2019, HIF-prolyl hydroxylase inhibitors (HIF-PHIs) have been developed and launched for renal anemia treatment, in which ESAs are gradually replaced with HIF-PHIs. In patients with renal anemia, HIF-PHIs are considered to restore EPO production in injured kidneys by suppressing activated PHDs. Alternatively, instead of injured kidneys, intact livers of patients with kidney disease may contribute to EPO induction by HIF-PHIs.11,12 In fact, in situ hybridization of mouse tissues demonstrated that HIF-PHIs induce Epo gene expression in REP cells but not in other cell types, under either healthy or disease conditions.15-17
HIF-PHIs are expected to improve not only EPO levels but also iron metabolism because HIF activation induces the expression of genes related to iron transport, such as the Cybrd1 (duodenal cytochrome b), Slc11a2 (divalent metal transporter 1), and Slc40a1 (ferroportin) genes.18,19 Systemic iron metabolism is mainly regulated by hepcidin, an antimicrobial peptide secreted from hepatocytes.20 Hepcidin suppresses iron release into blood from iron-storage cells such as macrophages and hepatocytes as well as duodenal enterocytes that absorb iron from food.21 Hepatic hepcidin production is enhanced under infective or inflammatory conditions as well as iron overload conditions. To use iron for hemoglobin synthesis during erythropoiesis, hepcidin gene (Hamp) expression in hepatocytes is suppressed by erythroferrone, which is secreted from erythroblasts receiving EPO.22 Therefore, elevated concentrations of plasma hepcidin, which are often caused by the inflammatory milieu in patients with kidney disease, may lead to ESA-resistant anemia by blocking mobilization of stored iron.23 In ESA-resistant anemia, ESA-induced erythroferrone is considered to be ineffective in suppressing hepcidin production, which is constitutively activated by inflammatory conditions.
Clinical studies have reported that hepcidin and ferritin levels are decreased in patients with renal anemia treated with HIF-PHIs compared with those in patients treated with ESAs.24 Based on these facts, the Asian Pacific Society of Nephrology recommends the use of HIF-PHIs for renal anemia treatment in patients who are hyporesponsive to ESAs.25 However, little is known about how hypoxia signaling regulates hepcidin production,26 and whether HIF-PHIs suppress hepcidin production in hepatocytes directly via HIF activation or indirectly via the EPO-erythroferrone cascade is controversial.6,27 To elucidate the contribution of hepatic EPO induction to the therapeutic effects of HIF-PHI and to clarify the regulatory mechanisms of HIF-PHI–mediated hepcidin suppression, this study examined responses to HIF-PHI administration in genetically modified mouse lines lacking renal EPO-production ability, which we established.28,29 Data from the mutant mice demonstrate that both erythropoiesis and hepcidin suppression are induced by HIF-PHIs, primarily through EPO induction in the kidneys, and that HIF-PHIs directly induce the expression of duodenal genes related to dietary iron intake.
Methods
Animal ethics
All animal experiments were approved by the Institutional Animal Care and Use Committee of Tohoku University (approval number 2020-MdA-078).
Mice
ISAM (inherited superanemic mutant; EpoGFP/GFP:Tg3.3K-EpoE genotype)28 and AnRED (anemic model mice with renal EPO deficiency; EpoGFP/GFP:TgdCURE-Epo genotype)29 mice aged 12 to 15 weeks with a C57BL/6 background were used as renal EPO-deficiency models, which are Epo-gene knockout mice rescued from lethal anemia by a short and a long Epo transgene, respectively. Because both transgenes lack the regulatory regions for renal Epo gene expression, both mouse lines exhibit adult-onset severe anemia. Littermate heterozygous mutant (Epo+/GFP:Tg3.3K-EpoE or Epo+/GFP:TgdCURE-Epo) mice were used as the control mice.
HIF-PHIs
Mice were intraperitoneally injected with GSK360A (50 mg/kg body weight; Toronto Research Chemicals, Toronto, ON) or roxadustat (200 mg/kg; 5A Pharmatech, Hong Kong) after reconstitution with water containing glucose (2% w/v) and NaOH (0.5 mol/L).15,16 For continuous administration, GSK360A (50 mg/kg) was injected daily for 5 days.
ESA
Continuous EPO receptor activator (C.E.R.A., Chugai Pharmaceutical, Tokyo)30 in phosphate-buffered saline containing 0.02% Tween 80 was subcutaneously injected into mice at a dose of 3.0 μg/kg body weight, 6 hours or 7 days before euthanasia.
Blood analyses
Peripheral blood (∼0.3 mL) was taken from the submandibular vein of mice and mixed with 5 μL EDTA (0.5 mol/L). Blood indices were measured using an automatic blood analyzer (Nihon Koden, Tokyo). Serum iron concentrations were measured using a ferrozine-based assay (Iron Assay Kit LS, Metallogenics, Tokyo).15 To measure plasma EPO concentrations, blood samples were centrifuged at 1500g for 10 minutes, and the supernatants (plasma) were applied to a Quantikine EPO ELISA kit (R&D Systems, Minneapolis, MN).
Reverse transcription polymerase chain reaction (RT-PCR)
Total RNA was extracted from mouse organs with ISOGEN reagent (Nippon Gene, Tokyo) and reverse transcribed using SuperScript IV with random hexamers (Thermo Fisher, Waltham, MA). Quantitative PCR was performed using gene-specific primers (primer sequences are upon request) with SYBR green reagent (Roche, Basel, Switzerland) on a LightCycler system (Roche).30 The expression level of each gene was normalized to Actb expression levels. To investigate Epo transgene (Tg3.3K-EpoE) expression, semiquantitative PCR was conducted using a primer pair that detects transgenic Epo messenger RNA (mRNA) as a band500 base pairs shorter than the endogenous Epo mRNA–derived PCR product.28 DNA products after various cycles of PCR were electrophoresed in 2% agarose gels, and the expression levels were estimated by comparing the band intensities that were quantified using ImageJ software (National Institute of Health, Bethesda, MD).
Histological analyses
The livers and spleens of mice were embedded in paraffin after fixation with 10% formalin for 24 hours at 4°C. Iron deposition in the tissue sections (3-μm thickness) prepared from the paraffin blocks was detected using a Berlin-blue staining kit (Wako, Osaka), and counterstaining was performed with Nuclear Fast Red (Sigma Aldrich, St. Louis, MO). Berlin-blue–positive areas in the tissue section images, captured by a microscope (BZ-X800, Keyence, Osaka, Japan), were quantified using ImageJ software.15
Statistics
Statistical significance was determined by the Tukey-Kramer test or unpaired Student t test for comparison of multiple groups and 2 groups, respectively. Correlations were calculated by Pearson correlation coefficients.
Results
EPO induction by HIF-PHIs is attenuated in mutant mouse lines lacking renal EPO-production ability
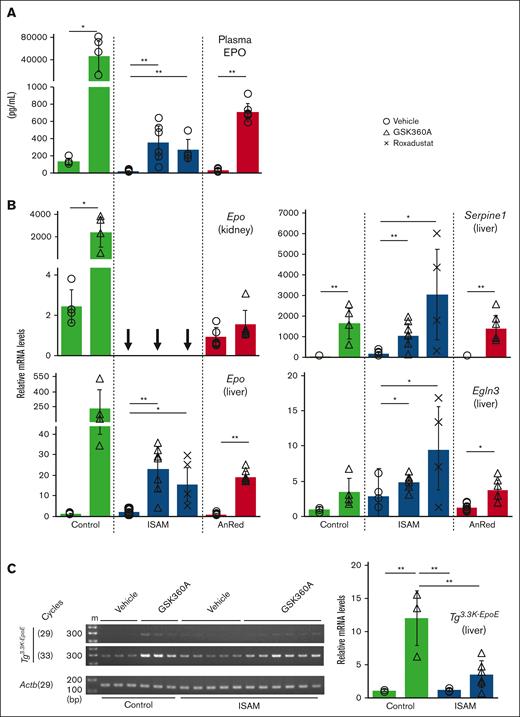
To examine the contribution of renal and hepatic EPO production to the induction of plasma EPO concentrations in mice treated with HIF-PHIs, we used genetically modified mouse lines (ISAM and AnRED) lacking EPO-production ability in the kidneys.28,29 Because ISAM and AnRED mouse lines are Epo-knockout mice integrated with short and long Epo transgenes lacking renal enhancers, respectively, their renal EPO expression is expected to be unresponsive to HIF-PHIs. In agreement with our previous reports,28,29 the plasma EPO concentrations of both mutant mouse lines were lower than those in the control mice before HIF-PHI injection (Figure 1A).
EPO induction by HIF-PHIs is attenuated in the ISAM and AnRED mutant mouse lines. (A) Plasma EPO concentrations in the control, ISAM, or AnRED mice at 6 hours after injection of vehicle, GSK360A (50 mg/kg), or roxadustat (200 mg/kg). (B) mRNA expression levels of the Epo, Serpine1, and Egln3 genes in the kidneys or livers of control, ISAM, or AnRED mice at 6 hours after injection of vehicle, GSK360A (50 mg/kg), or roxadustat (200 mg/kg). (C) A semiquantitative RT-PCR analysis was conducted to examine the expression levels of the Epo transgene (Tg3.3K-EpoE) in the livers of control and ISAM mice at 6 hours after injection of vehicle or GSK360A (50 mg/kg). Based on the band intensities after agarose electrophoresis (representative images of 29- and 33-cycle PCR products are shown in the left panel), the expression levels were estimated (right) after normalization to Actb expression levels. m, size markers. The average mRNA expression levels in the livers of vehicle-treated control mice were normalized to 1 for each gene in panels B-C. Arrows indicate undetectable levels. ∗P < .05 or ∗∗P < .01 calculated by Student t test (control, AnRED, and ISAM in panel A-C) or Tukey-Kramer test (ISAM in panel B).
EPO induction by HIF-PHIs is attenuated in the ISAM and AnRED mutant mouse lines. (A) Plasma EPO concentrations in the control, ISAM, or AnRED mice at 6 hours after injection of vehicle, GSK360A (50 mg/kg), or roxadustat (200 mg/kg). (B) mRNA expression levels of the Epo, Serpine1, and Egln3 genes in the kidneys or livers of control, ISAM, or AnRED mice at 6 hours after injection of vehicle, GSK360A (50 mg/kg), or roxadustat (200 mg/kg). (C) A semiquantitative RT-PCR analysis was conducted to examine the expression levels of the Epo transgene (Tg3.3K-EpoE) in the livers of control and ISAM mice at 6 hours after injection of vehicle or GSK360A (50 mg/kg). Based on the band intensities after agarose electrophoresis (representative images of 29- and 33-cycle PCR products are shown in the left panel), the expression levels were estimated (right) after normalization to Actb expression levels. m, size markers. The average mRNA expression levels in the livers of vehicle-treated control mice were normalized to 1 for each gene in panels B-C. Arrows indicate undetectable levels. ∗P < .05 or ∗∗P < .01 calculated by Student t test (control, AnRED, and ISAM in panel A-C) or Tukey-Kramer test (ISAM in panel B).
To detect the apparent effects of HIF-PHIs in mice, roxadustat was administered at a higher dose (200 mg/kg) than GSK360A (50 mg/kg), which is a research reagent with higher efficacy than medical reagents such as roxadustat.16 Both HIF-PHIs swiftly induced plasma EPO concentrations in the mutant mice, 6 hours after administration (Figure 1A). However, the induced concentrations were comparable with those in normal mice and 50- to 100-fold lower than those in the control mice injected with HIF-PHIs.
As expected, Epo mRNA levels in the kidneys were undetectable in ISAM mice and very low in AnRED mice regardless of HIF-PHI administration compared with those in the control mice, in which HIF-PHIs dramatically (∼1000-fold) induced Epo gene expression within 6 hours (Figure 1B). The basal Epo mRNA levels in livers were slightly higher in the mutant mouse lines than in the control mice, as reported previously (Figure 1B).28,29 HIF-PHIs significantly induced hepatic Epo gene expression, although the induction levels in the mutant mice were 10-fold lower than those in the control mice. Significant induction of hypoxic markers (Egln3 and Serpine1) in the livers confirmed that HIF-PHIs were effective without discriminating between the control mice and anemic mutant mouse lines, which exhibit chronic and systemic hypoxia (Figure 1B).
Two independent mouse lines bearing distinct Epo transgenes exhibited similar hepatic Epo gene expression levels after HIF-PHI treatment, which were 10-fold lower than those found in control mice (Figure 1B). To confirm the attenuated response of the Epo gene to HIF-PHIs in the livers of mice with chronic anemia, the expression levels of the Epo transgene (Tg3.3K-EpoE) were inspected in the control and ISAM livers by semiquantitative RT-PCR using primers that specifically detect transgene expression.28 As expected, the transgene expression levels after GSK360A treatment were significantly lower in ISAM mice than in the control mice (Figure 1C). The semiquantitative RT-PCR data showed smaller differences in the expression levels than the quantitative RT-PCR data because of its small dynamic range. These data suggest that long-term activation of Epo gene expression under chronic anemia conditions weakens the response of hepatic EPO production to further pharmacological HIF activation.
If the attenuated response of Epo gene induction to HIF-PHIs was not observed in the anemic mice, Epo gene expression levels in the mutant livers could increase to comparable levels in the livers of HIF-PHI–treated control mice (∼10-fold increase). However, the increased levels are estimated to be 10-fold inferior to those observed in the control mice because the plasma EPO levels of the HIF-PHI–treated mutant mice are 100-fold lower than those of the HIF-PHI–treated control mice (Figure 1A). Consequently, these data show that the kidney but not the other organs mainly contributes to EPO production in response to HIF-PHI administration.
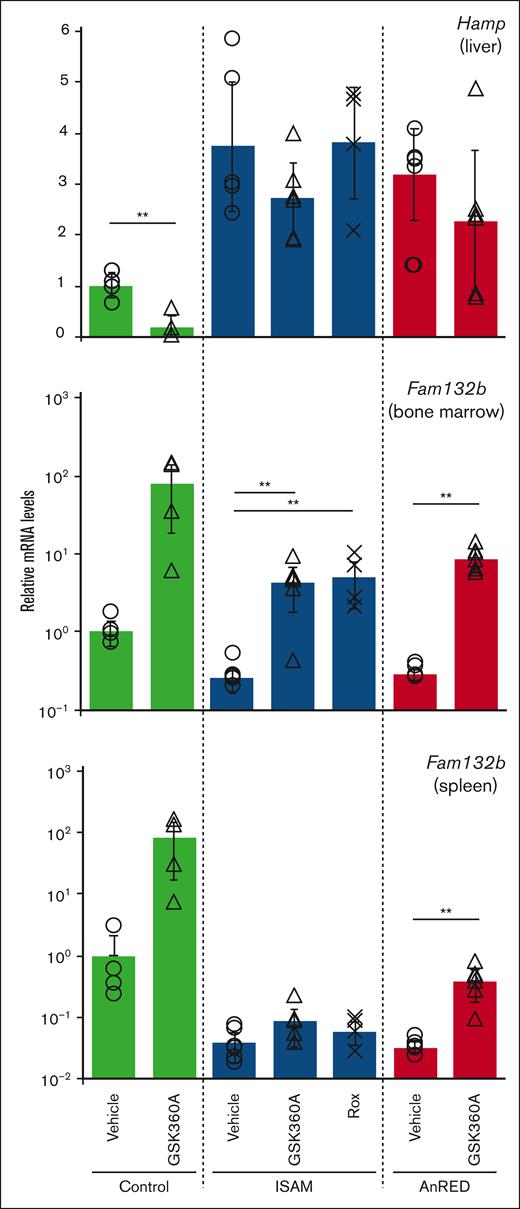
HIF-PHIs require renal EPO induction to suppress hepcidin expression
Reduced EPO production results in inactivation of iron use for hemoglobin synthesis in erythroid cells, followed by a relative iron overload state that strongly induces the expression of hepcidin in the liver.30 Under hypoxic conditions, hepatic Hamp expression is considered to be suppressed by erythroferrone, which is secreted from erythroblasts receiving EPO.31 Alternatively, HIFα proteins are thought to directly control the expression of the Hamp gene in hepatocytes.32,33 Indeed, hepatic expression of the hepcidin gene (Hamp) was elevated in ISAM and AnRED mice (Figure 2).
Hepcidin expression levels are unaffected by HIF-PHIs in the ISAM and AnRED mutant mouse lines.Hamp (hepcidin) and Fam132b (erythroferrone) mRNA expression in the livers, bone marrow, and spleens was analyzed in the control, ISAM, or AnRED mice at 6 hours after injection of GSK360A (50 mg/kg) or roxadustat (Rox, 200 mg/kg). In each graph, the average expression levels in the vehicle-treated control mice were normalized to 1. ∗P< .05 or ∗∗P < .01 calculated by Student t test (Control and AnRED) or Tukey-Kramer test (ISAM).
Hepcidin expression levels are unaffected by HIF-PHIs in the ISAM and AnRED mutant mouse lines.Hamp (hepcidin) and Fam132b (erythroferrone) mRNA expression in the livers, bone marrow, and spleens was analyzed in the control, ISAM, or AnRED mice at 6 hours after injection of GSK360A (50 mg/kg) or roxadustat (Rox, 200 mg/kg). In each graph, the average expression levels in the vehicle-treated control mice were normalized to 1. ∗P< .05 or ∗∗P < .01 calculated by Student t test (Control and AnRED) or Tukey-Kramer test (ISAM).
HIF-PHI injection into ISAM and AnRED mice revealed that, without sufficient EPO production, HIF-PHIs are ineffective in modulating hepcidin expression (Figure 2). In addition, induction of erythroferrone gene (Fam132b) expression in the spleen and bone marrow, both of which are the major erythropoietic organs in mice, was enhanced ∼100-fold at 6 hours after HIF-PHI administration in the control mice, whereas the induction levels were decreased up to 10-fold in the mutant mice (Figure 2). These data suggest that hypoxia signaling and/or HIFα proteins in hepatocytes indirectly, and not directly, suppress Hamp expression by inducing renal EPO production, which dramatically elevates erythroid expression of the major Hamp suppressor erythroferrone.
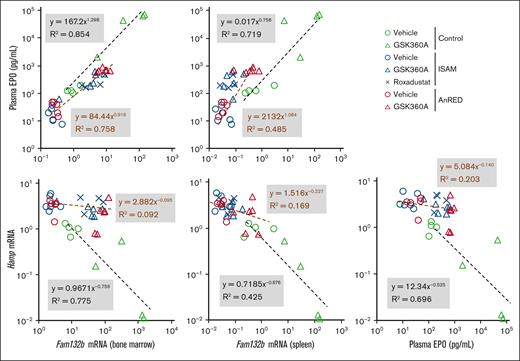
To confirm that Hamp expression is primarily regulated by the EPO-erythroferrone axis, the relationships among hepatic Hamp mRNA levels, plasma EPO concentrations, bone marrow Fam132b mRNA levels, and splenic Fam132b mRNA levels were investigated. As shown in the scatter plots (Figure 3), all 4 parameters were well correlated with each other (R2 > 0.70) except hepatic Hamp and splenic Fam132b (R2 = 0.42) in the control mice with or without HIF-PHIs. However, in the anemic mutant mice, there were no correlations among the parameters except between EPO and bone marrow Fam132b (R2 = 0.76, Figure 3), suggesting that low-level EPO induction by HIF-PHIs was insufficient to alter Fam132b and Hamp expression. Moreover, the data indicate the existence of a threshold level of the plasma EPO concentration, between 0.1 and 1.0 ng/mL, for the initiation of hepatic hepcidin production suppression, whereas ∼40 ng/mL plasma EPO is needed to decrease the hepcidin expression levels to the levels found in the HIF-PHI–treated control mice (lower right panel in Figure 3). These data strengthen our argument that HIF-PHIs indirectly suppress Hamp expression by activating EPO-erythroferrone signaling.
HIF-PHIs suppress hepcidin expression in a manner dependent on the induction levels of EPO and erythroferrone expression. Scatter plots of the relationships between EPO concentrations in plasma (Figure 1A), Fam132b (erythroferrone) mRNA levels in the bone marrow, Fam132b mRNA levels in the spleen, and Hamp (hepcidin) mRNA levels in the liver (Figure 2). The correlations between the parameters in each graph were analyzed with the Pearson correlation coefficient in the control (green) and mutant (ISAM, blue; AnRED, red) mouse lines, which were treated with vehicle (circles), GSK360A (triangles), or roxadustat (crosses).
HIF-PHIs suppress hepcidin expression in a manner dependent on the induction levels of EPO and erythroferrone expression. Scatter plots of the relationships between EPO concentrations in plasma (Figure 1A), Fam132b (erythroferrone) mRNA levels in the bone marrow, Fam132b mRNA levels in the spleen, and Hamp (hepcidin) mRNA levels in the liver (Figure 2). The correlations between the parameters in each graph were analyzed with the Pearson correlation coefficient in the control (green) and mutant (ISAM, blue; AnRED, red) mouse lines, which were treated with vehicle (circles), GSK360A (triangles), or roxadustat (crosses).
The erythropoietic effects of HIF-PHIs are attenuated by renal EPO deficiency
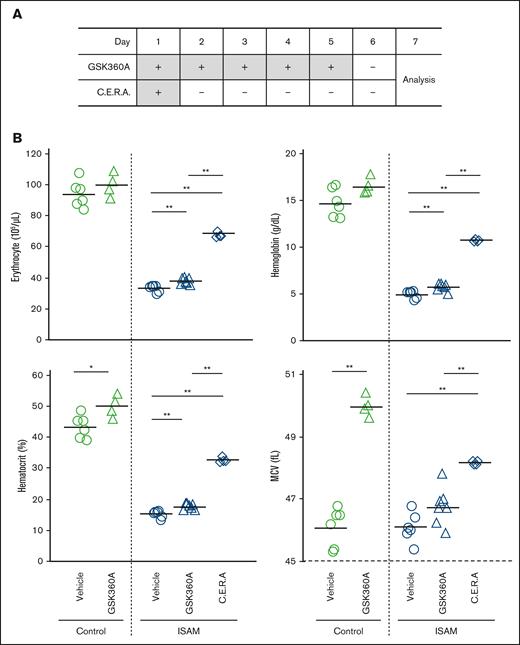
To examine the necessity of renal EPO induction for the therapeutic effects of HIF-PHIs, iron use and erythropoiesis in ISAM mice injected with GSK360A every day for 5 days were analyzed (Figure 4A). Because 2 independent mouse lines (ISAM and AnRED) with distinct Epo transgenes exhibited similar responses to HIF-PHIs, the gene expression profiles found in this study were considered to be common in animal to which HIF-PHI had been administered. Therefore, only ISAM mice were analyzed hereafter. In contrast to the control mice in which continuous GSK360A administration resulted in marginal increases in erythrocyte numbers, hemoglobin concentrations, and hematocrit levels, GSK360A-mediated induction of all 3 erythropoietic parameters in the anemic ISAM mice was statistically significantly different (P < .01, Figure 4B). However, GSK360A was highly insufficient at correcting the anemic phenotype, whereas 1 dose of a long-acting ESA (C.E.R.A.) almost completely ameliorated the anemia (Figure 4B).30
The erythropoietic effects of GSK360A are attenuated in ISAM mice. (A) A scheme of daily injection of GSK360A for 5 days. ISAM mice treated with C.E.R.A. were analyzed as positive controls, in which erythropoiesis was induced. (B) The number of erythrocytes, hemoglobin, hematocrit, and MCV were analyzed 2 days after the final injection of GSK360A. ∗P < .05 or ∗∗P < .01 calculated by Student t test (control) or Tukey-Kramer test (ISAM).
The erythropoietic effects of GSK360A are attenuated in ISAM mice. (A) A scheme of daily injection of GSK360A for 5 days. ISAM mice treated with C.E.R.A. were analyzed as positive controls, in which erythropoiesis was induced. (B) The number of erythrocytes, hemoglobin, hematocrit, and MCV were analyzed 2 days after the final injection of GSK360A. ∗P < .05 or ∗∗P < .01 calculated by Student t test (control) or Tukey-Kramer test (ISAM).
Mean corpuscular volume (MCV), which reflects the real-time activity of erythropoiesis, was also examined in ISAM mice after continuous injection of GSK360A. The MCV elevation was higher in the nonanemic control mice than in ISAM mice (Figure 4B), indicating that renal EPO induction was needed to fully activate erythropoiesis by GSK360A, in agreement with the data on plasma EPO concentrations (Figure 1A). As ESA administration was previously reported to increase MCV without significant impacts on the other erythropoietic parameters in normal mice,34 GSK360A treatment significantly upregulated MCV in the control mice without altering the erythrocyte counts or hemoglobin concentrations (Figure 4B). These data demonstrate that the erythropoietic effects of HIF-PHIs are attenuated by renal EPO deficiency.
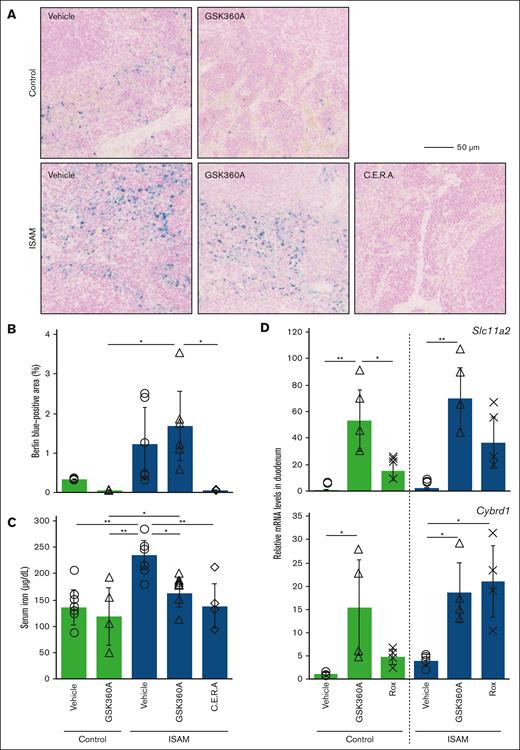
HIF-PHIs require renal EPO induction for mobilization of stored iron but not for induction of serum iron use and duodenal gene expression related to iron intake
Next, iron metabolism after GSK360A treatment was inspected in the control and ISAM mice. Compared with the spleens of the control mice, intense iron deposition was observed in the spleens of ISAM mice due to relative iron overload, which was caused by impaired erythropoietic activity (Figure 5A-B).30 Berlin-blue staining also demonstrated that splenic iron deposition was eliminated by GSK360A in the control mice, whereas it was unchanged in the ISAM mice. Because C.E.R.A. almost completely reduced the iron deposition in ISAM mice (Figure 5A-B), GSK360A treatment was considered to induce insufficient levels of EPO to mobilize stored iron without renal EPO induction.
GSK360A-mediated mobilization of stored iron in the spleen is blocked in ISAM mice. (A) Berlin-blue staining detected iron deposition in spleen sections of the control or ISAM mice, 2 days after the final injection of GSK360A (Figure 4A). The scale bar indicates 50 μm. (B) The percentage of Berlin-blue–positive areas in each spleen section was quantified. (C) Serum concentrations of iron were measured 2 days after the final injection of GSK360A (Figure 4A). Data from C.E.R.A.–treated ISAM mice were used as positive controls for panels A-C. (D) The mRNA expression in the duodenums was analyzed in control or ISAM mice at 6 hours after injection of GSK360A (50 mg/kg) or roxadustat (200 mg/kg). In each graph, the average mRNA expression levels in the vehicle-treated control mice were normalized to 1. ∗P < .05 and ∗∗P < .01 determined by the Tukey-Kramer test.
GSK360A-mediated mobilization of stored iron in the spleen is blocked in ISAM mice. (A) Berlin-blue staining detected iron deposition in spleen sections of the control or ISAM mice, 2 days after the final injection of GSK360A (Figure 4A). The scale bar indicates 50 μm. (B) The percentage of Berlin-blue–positive areas in each spleen section was quantified. (C) Serum concentrations of iron were measured 2 days after the final injection of GSK360A (Figure 4A). Data from C.E.R.A.–treated ISAM mice were used as positive controls for panels A-C. (D) The mRNA expression in the duodenums was analyzed in control or ISAM mice at 6 hours after injection of GSK360A (50 mg/kg) or roxadustat (200 mg/kg). In each graph, the average mRNA expression levels in the vehicle-treated control mice were normalized to 1. ∗P < .05 and ∗∗P < .01 determined by the Tukey-Kramer test.
The elevated iron concentrations in ISAM blood were significantly decreased to normal levels after GSK360A treatment (Figure 5C). These data indicate that hepatic EPO induction by HIF-PHIs is sufficient to mobilize serum iron for hemoglobin synthesis even under high-level hepcidin conditions, whereas high-level EPO induction in the kidneys is required for mobilizing stored iron by suppressing hepatic hepcidin production. In fact, HIF-PHI treatment slightly increased hemoglobin and erythrocyte concentrations in ISAM mice, although the induction was weaker than that induced by ESA (Figure 4B).
Finally, we examined the expression of genes related to iron intake in the ISAM duodenums before HIF-PHIs altered serum iron concentrations (6 hours after HIF-PHI injection). Both GSK360A and roxadustat significantly induced expression of the Cybrd1 and Slc11a2 genes in the duodenums of ISAM mice as well as in the duodenums of the control mice (Figure 5D). These findings suggest that HIF-PHIs directly induce the expression of duodenal genes essential for dietary iron intake in a manner independent of EPO induction.
Discussion
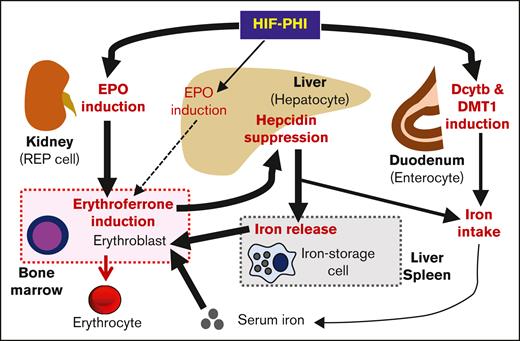
HIF-PHIs have been used since 2019 for renal anemia treatment, and their beneficial therapeutic effects have been verified. However, the mechanism by which HIF-PHIs correct anemia is controversial. Little is still known about how HIF-PHIs induce expression of the EPO gene exclusively among hundreds of HIF-target genes,35 how HIF-PHIs revive EPO gene expression in renal myofibroblasts lacking EPO-production ability,17,36 how HIF-PHIs improve iron metabolism,37 and how extrarenal EPO induction contributes to the therapeutic effects of HIF-PHIs.38 This study, using genetically modified mice, demonstrated that HIF-PHIs induce erythropoiesis and mobilize stored iron in a manner mostly dependent on renal EPO induction (Figure 6). Accordingly, to optimize the effect of HIF-PHIs in renal anemia treatment, the population of REP cells remaining in injured kidneys is critical, although the cells are seriously reduced.
Scheme of the mechanism by which HIF-PHI induces erythropoiesis and iron mobilization. This study, using mutant mouse lines in which the Epo gene is modified, demonstrates that HIF-PHIs induce erythropoiesis primarily by activating renal Epo gene expression. Hepatic EPO induction contributes marginally to the therapeutic effects of HIF-PHIs. HIF-PHIs directly regulate neither hepcidin expression in the liver nor the mobilization of stored iron. Hepatic hepcidin expression is fundamentally suppressed by erythroferrone, which is secreted from erythroblasts stimulated by EPO. Hepcidin suppression results in the induction of iron release from iron-storage cells. Erythroblasts use serum iron for hemoglobin synthesis without hepcidin suppression. Regardless of EPO induction, HIF-PHIs directly drive the duodenal induction of duodenal cytochrome b and divalent metal transporter 1, which promote iron intake from food in coordination with hepcidin suppression.
Scheme of the mechanism by which HIF-PHI induces erythropoiesis and iron mobilization. This study, using mutant mouse lines in which the Epo gene is modified, demonstrates that HIF-PHIs induce erythropoiesis primarily by activating renal Epo gene expression. Hepatic EPO induction contributes marginally to the therapeutic effects of HIF-PHIs. HIF-PHIs directly regulate neither hepcidin expression in the liver nor the mobilization of stored iron. Hepatic hepcidin expression is fundamentally suppressed by erythroferrone, which is secreted from erythroblasts stimulated by EPO. Hepcidin suppression results in the induction of iron release from iron-storage cells. Erythroblasts use serum iron for hemoglobin synthesis without hepcidin suppression. Regardless of EPO induction, HIF-PHIs directly drive the duodenal induction of duodenal cytochrome b and divalent metal transporter 1, which promote iron intake from food in coordination with hepcidin suppression.
The anemia mouse models lacking renal EPO production, which we generated,28,29 clearly demonstrated that the contribution of hepatic EPO induction to plasma EPO increase is marginal in mice subjected to HIF-PHIs, and ∼90% of plasma EPO was estimated to be derived from the kidneys. The regulatory mechanism of Epo gene expression in hepatocytes is distinct from that in REP cells,4,6,7,28,29,39,40 and the difference is considered to make the EPO induction levels different between the liver and kidney. In agreement with these data, it has been estimated that, in healthy humans, up to 10% of total plasma EPO is derived from the liver, under either normoxic or hypoxic conditions.41,42 Furthermore, HIF-PHI–inducible plasma EPO concentrations are lower in patients who are anephric than in those who are nephric with end-stage kidney disease.38
Of note, the increases in hemoglobin and erythrocyte levels in the anemia mice model after HIF-PHI treatment were marginal but statistically significant. Moreover, in patients with kidney disease who require hemodialysis but not ESA, the contribution of liver-derived EPO increases to almost half of plasma EPO.10 Therefore, for renal anemia treatment, it may be plausible to pharmacologically induce hepatic EPO production instead of in injured kidneys, although the efficacy is predicted to be low compared with renal EPO induction. In this regard, HIF-PHIs specifically targeting livers have been developed to avoid potential risks associated with pleiotropic and undesired effects induced by systemic HIF activation.43,44
This study indicates that pharmacological PHD inhibition in hepatocytes induces low-level EPO induction that is insufficient for full activation of erythropoiesis. In contrast, genetic abrogation or knockdown of PHDs in hepatocytes was previously reported to result in drastic EPO induction sufficient for polycythemia development, with almost complete suppression of hepatic hepcidin expression.6,45,46 However, the intense and constitutive activation of HIFs in hepatocytes causes not only abundant EPO production but also lethal steatosis in mice. Consequently, HIF activity should be fine-tuned to safely and effectively apply HIF-PHIs for renal anemia treatment through the induction of hepatic EPO production. Compared with genetic PHD inactivation, this study proposes that pharmacological PHD inhibition mildly and transiently affects HIF activity in hepatocytes. In addition, the weak response of erythropoiesis and hepcidin suppression in the anemic mutant mice is much more likely due to reduced total EPO production than to the qualitative differences between renal EPO and hepatic EPO.
Our data indicate that HIF-PHIs induce hepatic Epo gene expression at lower levels in the anemic mice than in the control mice. Consistently, we recently reported that another HIF-PHI, molidustat, marginally induces hepatic Epo gene expression and an increase in plasma EPO concentrations in ISAM mice.47 These data suggest that chronic anemia/hypoxia in the anemic models28 may attenuate hepatic EPO induction in response to HIF-PHIs by activating negative feedback regulation of the hypoxia-response pathway. Indeed, feedback mechanisms to avoid excessive activation of hypoxia-inducible gene expression have been identified, in which HIFs induce the expression of genes for HIF suppressors, including PHD2 and PHD3.45 The hepatic expression of HIF-target genes (Serpine1 and Egln3) other than Epo in the mutant mice tends to be induced by anemic hypoxia, and HIF-PHIs further elevate the expression levels to levels comparable with those found in the HIF-PHI–treated control mice. Therefore, not only general feedback mechanisms but also epigenetic mechanisms specific to the Epo gene are suggested to be involved in the attenuated response to HIF-PHIs under chronic anemia conditions. The attenuated response in the anemic mice suggests that the therapeutic effects of HIF-PHIs through the induction of hepatic EPO production are weakened in patients with renal anemia.
One of the most serious issues in renal anemia treatment is ESA resistance due to functional iron deficiency caused by inflammation-related overproduction of hepcidin.48 Because hepcidin blocks ferroportin-mediated iron export from iron-storage cells, iron use for hemoglobin synthesis that is essential for erythropoiesis promoted by EPO is not possible under high-level hepcidin conditions.49 Intriguingly, our data indicate that high hepcidin levels prevent the use of stored iron but not serum iron (Figure 6). In addition, the decrease in the serum iron of GSK360A-treated ISAM mice indicates that HIF-PHIs also correct transferrin saturation, similar to the results found with ESAs, which increase the unsaturated iron binding capacity of transferrin in ISAM mice.30 These facts suggest that optimal iron administration may improve the therapeutic efficacy of HIF-PHIs and ESAs for patients with renal anemia with high hepcidin levels.
Recently, accumulated clinical evidence has shown that, compared with ESAs, HIF-PHIs efficiently decrease blood hepcidin concentrations in patients with renal anemia.24 Regarding the mechanism of HIF-PHI–mediated hepcidin suppression, HIFs were expected to directly inhibit hepcidin expression in the liver.33,50,51 However, recent genetic approaches have elucidated that HIFs indirectly suppress transcription of the Hamp gene in vivo by activating the EPO-erythroferrone cascade (Figure 6).27,30,52 This latter mechanism is supported by data from this study that show that hepcidin expression remains high without sufficient induction of EPO and erythroferrone in mice treated with HIF-PHIs.
ISAM mice also demonstrated that HIF-PHIs directly (not indirectly through activation of Epo gene expression) induce the expression of duodenal genes (Slc11a2 and Cybrd1) related to dietary iron intake into enterocytes that are well-known HIF2α-target genes as well as the Epo gene (Figure 6).19 Because HIF2α activation in the duodenum induces these 2 genes exclusively in lumen epithelial cells,53,54 HIF-PHI administration is expected to induce the tissue-specific expression of the genes. Furthermore, these data demonstrate that HIF-PHIs enhance HIF activities in the duodenum epithelium, which is known as 1 of the most hypoxic tissues in healthy animals.55
Because hepcidin suppresses iron intake from duodenal enterocytes into the blood,56 HIF-PHIs are believed to seamlessly induce use of dietary iron for hemoglobin synthesis through combinatory stimulation of duodenal gene expression for dietary iron intake and renal EPO induction for hepatic hepcidin suppression (Figure 6). Consequently, we propose that the induction of these duodenal genes is a therapeutic advantage of HIF-PHIs compared with ESAs for treatment of renal anemia.
Although basic studies insist that HIF-PHIs need to highly induce EPO production to suppress hepcidin levels, as described earlier, it has been clinically revealed that HIF-PHIs are more effective for hepcidin reduction than ESAs.24 This discrepancy suggests that inflammatory conditions, which were excluded in the experiments of the aforementioned studies and this study, are relevant in hepcidin regulation in livers. In fact, regarding hepcidin regulation, the induction effect of inflammation is superior to the suppression effect of erythroferrone.57 Furthermore, HIFs are widely related to inflammation, and HIF-PHIs ameliorate inflammation via HIF activation in inflammatory cells.58 Hence, we surmise that HIF-PHIs suppress hepcidin overproduction by mitigating inflammatory conditions.59
This study used 2 representative HIF-PHIs to understand the mechanism of the effects of HIF-PHIs on erythropoietic induction and found that the drugs exert fundamentally similar effects. In contrast, the tissue distribution and pharmacodynamics are considered to differ among the HIF-PHIs.60 Indeed, our data show that GSK360A and roxadustat induce the expression of duodenal genes to different levels. Therefore, further studies with various HIF-PHIs other than GSK360A and roxadustat are desired to elucidate the drug-specific effects of HIF-PHIs. In summary, our mouse models demonstrate that HIF-PHIs require renal EPO induction to achieve full therapeutic effects, including hemoglobin synthesis, erythroid maturation, and hepcidin suppression. In contrast, hepatic EPO induction partially contributes to the erythropoietic effects of HIF-PHIs, although it is insufficient to compensate for abundant EPO induction by the kidneys. These findings are helpful when considering the clinical use of HIF-PHIs or ESAs in patients with end-stage renal disease or those who are anephric, who almost completely lack intact REP cells.
Acknowledgments
The authors thank Atsuko Konuma and Erika Maruyama (Tohoku University) for technical help as well as the Biomedical Research Core and Centre for Laboratory Animal Research of Tohoku University.
This study was supported, in part, by MEXT/JSPS KAKENHI (21H02676 and 22K193960), the Japan Agency for Medical Research and Development (DNW-22018), the Uehara Memorial Foundation, the Takeda Science Foundation (N.S.), and the Advanced Graduate Program for Future Medicine and Health Care at Tohoku University (T.N.).
T.N. was a research fellow of the Japan Society for the Promotion of Science (21J21957).
The funders had no role in this study.
Authorship
Contribution: T.N. and N.S. developed the project and designed the study; T.N., Y.I., K.K., and N.S. performed the experiments and analyzed the data; T.N. and N.S. constructed the figures and wrote the manuscript; T.N., I.H., K.K., and N.S. provided animal models; K.K., Y.M., and Y.T. provided chemical compounds; N.S. and M.Y. supervised the project; and all authors discussed the results and suggested revisions.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Norio Suzuki, Applied Oxygen Physiology Project, New Industry Creation Hatchery Center, Tohoku University, Seiryo-machi 2-1, Aoba-ku, Sendai, Miyagi 980-8575, Japan; e-mail: sunorio@med.tohoku.ac.jp.
References
Author notes
Data are available on request from the corresponding author, Norio Suzuki (sunorio@med.tohoku.ac.jp).