Key Points
S1P declines during RBC storage. S1P supplementation to human or murine RBCs boosts energy metabolism at the expense of antioxidant pathways.
S1P worsens and Sphk1 KO, or hypoxia, promote stored RBC posttransfusion recoveries.
Abstract
Blood storage promotes the rapid depletion of red blood cell (RBC) high-energy adenosine triphosphate (ATP) and 2,3-diphosphoglycerate (DPG), which are critical regulators of erythrocyte physiology and function, as well as oxygen kinetics and posttransfusion survival. Sphingosine-1-phosphate (S1P) promotes fluxes through glycolysis. We hypothesized that S1P supplementation to stored RBC units would improve energy metabolism and posttransfusion recovery. We quantified S1P in 1929 samples (n = 643, storage days 10, 23, and 42) from the REDS RBC Omics study. We then supplemented human and murine RBCs from good storer (C57BL6/J) and poor storer strains (FVB) with S1P (1, 5, and 10 μM) before measurements of metabolism and posttransfusion recovery. Similar experiments were repeated for mice with genetic ablation of the S1P biosynthetic pathway (sphingosine kinase 1 [Sphk1] knockout [KO]). Sample analyses included metabolomics at steady state, tracing experiments with 1,2,3-13C3-glucose, proteomics, and analysis of end-of-storage posttransfusion recovery, under normoxic and hypoxic storage conditions. Storage promoted decreases in S1P levels, which were the highest in units donated by female or older donors. Supplementation of S1P to human and murine RBCs boosted the steady-state levels of glycolytic metabolites and glycolytic fluxes, ie the generation of ATP and DPG, at the expense of the pentose phosphate pathway. Lower posttransfusion recovery was observed upon S1P supplementation. All these phenomena were reversed in Sphk1 KO mice or with hypoxic storage. S1P is a positive regulator of energy metabolism and a negative regulator of antioxidant metabolism in stored RBCs, resulting in lower posttransfusion recoveries in murine models.
Introduction
Red blood cell (RBC) transfusion is a life-saving intervention for millions of recipients worldwide every year. However, the quality of packed RBC products declines during storage in the blood bank, which promotes a series of morphological1,2 and biochemical changes3 that ultimately affect erythrocyte physiology and posttransfusion performances. The quality of stored RBCs, as per the US Food and Drug Administration (FDA) and the European Council guidelines, is defined by hemolytic propensity and the capacity of transfused RBCs to circulate at 24 hours after transfusion (henceforth, posttransfusion recovery [PTR]); these 2 parameters increase and decrease, respectively, as a function of storage duration.3
It has been argued that oxidative stress is the main driver of the storage lesion.4 RBCs are well equipped to counteract oxidant stress through different systems, among which the pentose phosphate pathway (PPP) represents a critical lynchpin. The PPP is the main pathway generating the key reducing equivalent nicotinamide adenine dinucleotide phosphate, NADPH, which participates in the scavenging of reactive oxygen species and recycling of oxidized soluble small molecules (for example, the glutathione system) and enzyme-catalyzed antioxidant batteries.5 Glucose-6-phosphate dehydrogenase (G6PD) is the rate-limiting enzyme of the PPP, and it is highly polymorphic in humans.6 Of note, antioxidant capacity,7 storage quality,8 hemolytic propensity,9 PTRs,10 and posttransfusion hemoglobin increments11 are poorer in packed RBCs donated by volunteers suffering from G6PD deficiency, a condition that affects ∼500 million individuals to a variable extent, owing to a plethora of genetic mutations, all resulting in a hypomorphic or unstable G6PD enzyme.6 Because G6PD is a chromosome X–linked gene, whose activity declines with age12 and affects lifespan in mammals,13 it is interesting to note that donor sex and age8,14,15 affect RBC antioxidant capacity and posttransfusion RBC performances beyond the chronological age of the unit, that is, the days elapsed since the time of donation.16,17
Others have noted that rapid depletion of high-energy phosphate compounds (adenosine triphosphate [ATP] and 2,3-diphosphoglycerate [DPG]) is a hallmark of the RBC metabolic storage lesion.18 ATP consumption is accompanied by dysregulated calcium ion pumps,19 resulting in intracellular calcium accumulation and eryptosis.20 Reductions in ATP deprive erythrocytes of a rate-limiting substrate for phosphorylation of structural membrane proteins, which is critical to morphological homeostasis of the stored RBC.21 By fueling ATP-dependent flippases, ATP depletion in the stored RBC results in phosphatidylserine exposure to the outer membrane leaflet and untimely removal upon transfusion.3,22,23 DPG exhaustion by storage week 2 to 3 is mechanistically linked to altered oxygen kinetics.22 Indeed, depletion of DPG levels promotes increases in oxygen saturation (SO2) by shifting the oxygen dissociation curve to the left,24 which in turn promotes the concomitant storage-dependent formation of reactive oxygen species2 that are triggered by Haber-Weiss chemistry in the presence of elevated O2 levels. Indeed, heterogeneity in baseline SO2 levels after processing is associated with heterogeneity in storage quality,25 to the extent that SO2 manipulation by hypoxic storage improves energy metabolism, prevents the oxidative storage lesion,26,27 and boosts PTRs in randomized clinical trials in humans,28 as well as transfusion efficacy in rodent models of trauma and shock.29 Among the mechanisms identified as key drivers of the benefits of hypoxic storage is the alkalinization of intracellular pH,30 and the mitigation of cysteine oxidation27 and asparagine deamidation26 of key glycolytic enzymes. These factors, combined with deoxyhemoglobin competitive binding to the N-terminus of band 3 that displaces otherwise bound/inhibited glycolytic enzymes,31-33 all contribute to boosting glycolysis and ATP generation capacity in hypoxically stored RBCs, which ultimately preserves oxygen kinetics of these products.34 Of note, even though DPG and ATP synthesis is slowly restored upon transfusion in vivo,35 the kinetics may be insufficient to meet the oxygen requirements in the hypoxic, massively transfused recipient (for example, patients with trauma).
In previous mechanistic studies on high-altitude hypoxia and sickle cell disease,36,37 we showed that sphingosine-1-phosphate (S1P) supplementation promotes fluxes through glycolysis by mediating hemoglobin binding to the N-terminus domain of band 3,37 thereby displacing glycolytic enzymes, otherwise inhibited by competitive binding to the very same domain of band 3.32,33 By promoting glucose oxidation through glycolysis and the Rapoport-Luebering shunt, S1P supplementation promotes the synthesis of ATP and DPG. Exposure to hypoxia (in vivo or in vitro) promotes S1P synthesis by RBC sphingosine kinase 1 (Sphk1), which is critical to metabolic adaptations to high-altitude or pathological hypoxia (for example, chronic kidney disease).37,38 However, previous studies have shown that storage is accompanied by declines in S1P levels (down to 19% of fresh values in day-30 units39), suggesting that exogenous supplementation of S1P could be leveraged as a metabolic intervention in stored RBC units. Other studies, however, have either shown no storage-dependent change40 or additive solution-dependent increases/decreases in S1P levels.41 In light of this, first of all, we leveraged the largest sample set amenable for S1P assessment from the REDS RBC Omics study,42 a longitudinal study on ∼2000 samples from 643 blood donors. After confirming that storage causes a decline in S1P levels in RBC units, especially those donated by donors characterized by extreme hemolytic propensity from the REDS RBC Omics cohort,42 we hypothesized that supplementation of S1P to human and murine packed RBCs would improve storage quality, whereas genetic ablation of Sphk1 would impair S1P biosynthesis and, consequently, exacerbate the storage lesion by negatively affecting glycolysis (and thus ATP and DPG synthesis).
Methods
REDS RBC Omics study participants and samples
RBC Omics was conducted under regulations applicable to all human subject research supported by federal agencies as well as the requirements for blood product manipulation specified and approved by the FDA. The data coordinating center (RTI International) of REDS was responsible for the overall compliance of human participant regulatory protocols including institutional review board approval from each participating blood center, from the REDS Central Laboratory (Vitalant Research Institute), and from the data coordinating center, as previously detailed.8,41 Donors were enrolled at the 4 participating REDS US blood centers. Overall, 13 403 individuals aged ≥18 years provided informed consent to participate in the study. Hemolysis parameters (spontaneous, oxidative, or osmotic) were evaluated on stored RBCs from these donors after ∼39 to 42 days of storage. Extreme hemolyzers (5th and 95th percentile) from the donors tested for end-of-storage oxidative hemolysis were asked to donate a second unit of blood. These units were sterilely sampled for metabolomics analysis (n = 643, storage days 10, 23, and 42). Blood collection, sample processing, and other aspects of the screening and recall phases of the RBC Omics Study have been extensively described.9,14
Human RBC incubation with D7-S1P
RBC storage with S1P
Whole blood units were donated by 10 healthy donor volunteers in CP2D (Haemonetics, Boston, MA). Two pools of 5 units were made, upon leukofiltration, plasma removal, and suspension in AS-3 additive solution, with or without supplementation of S1P (product #MFCD00270077; CAS #26993-30-6; Sigma Aldrich, St. Louis, MO) at 1, 5, or 10 μM.
Mouse blood collection, storage under hypoxic and normoxic conditions, and PTR
All murine experimental protocols were approved by the University of Virginia IACUC on 22 April 2019 (protocol n: 4269). Mouse strains C57BL6/J, FVB and Sphk1 knockout (KO) have been previously described.45,46 Murine RBC storage (for 3 and 6 days for FVB mice, and 12 days for C57BL6/J mice), transfusion, and PTR determinations were carried out as previously described, with minor modifications.46 Whole blood was drawn by cardiac puncture under sterile conditions into CPDA-1, centrifuged, and the hematocrit was adjusted to 75% by removing supernatant. In a subset of experiments, units were supplemented with 5 μM S1P. For hypoxic storage, murine RBCs were bubbled with nitrogen gas in a glove box until SO2 <50% before storage, whereas normoxic counterparts reached SO2 >95% by the end of the storage period. Sealed “units” were preserved at 37°C for 1 hour and stored at 4°C for 7 and 12 days. RBCs from C57BL6/J mice were used as the test population and subjected to different storage conditions. UBC-GFP mice (stock #004353) were used as recipients to allow visualization of the test cells in the nonfluorescent gate. To control for differences in transfusion and phlebotomy, RBCs from ROSA26-LCB-mCHERRY mice (mCHERRY) were used as a tracer RBC population (never stored) and were added to stored RBCs immediately before transfusion, as recently described.47 PTR was calculated by dividing the posttransfusion ratio (test:tracer) by the pretransfusion ratio (test:tracer).48 A single PTR value >100% was calculated across all replicates in all experiments, which was explained by the tracer population being damaged and/or outperformed by the test population. Because PTR >100% is not biologically meaningful, this value was set to an absolute value of 100%, as standard practice in the field. At the time of transfusion, blood samples were frozen in liquid nitrogen and stored at −80°C until subsequent analysis.
Glucose tracing experiments
RBCs (100 μL) from all the mouse strains investigated in this study were incubated at 37°C for 1 hour in the presence of 1,2,3-13C3-glucose (5 mM, Cambridge Isotopes, product #CLM-4673) and stored for 7 and 12 days before determination of lactate isotopologues +2/+3 (as markers of PPP-to-glycolysis fluxes), as described.27
Ultra-high-performance liquid chromatography (UHPLC)-mass spectrometry metabolomics
Frozen RBC aliquots (50 μL) were extracted 1:10 in ice cold extraction solution (methanol:acetonitrile:water, 5:3:2 v/v/v).26 Samples were vortexed and insoluble material pelleted, as previously described.49 Analyses were performed using a Vanquish UHPLC coupled online to a Q Exactive mass spectrometer (Thermo Fisher, Bremen, Germany). Samples were analyzed using a 150 and 5 minute gradient-based method,49 as previously described.51,52 S1P measurements were performed via the same platform described earlier, as validated in prior technical notes52 and RBC-centric studies on S1P,37,38 with the auxilium of stable isotope–labeled internal standards (D7-S1P, product #860659, Avanti Lipids). Data analysis was performed through the auxilium of the software MAVEN.53 Graphs and statistical analyses (either two-way analysis of variance [ANOVA] or repeated-measures ANOVA) were prepared with GraphPad Prism 8.0 (GraphPad Software, Inc, La Jolla, CA), GENE E (Broad Institute, Cambridge, MA), and MetaboAnalyst 5.0.54 All raw data are available from the corresponding author upon reasonable request.
Results
RBC S1P declines with storage and is higher in packed RBCs from female and older donors
As part of the REDS-III RBC Omics study, we analyzed packed RBC samples from 643 donors, at 3 storage time points (ie, days 10, 23, and 42; Figure 1A). These donors were selected among an original cohort of 13 403 healthy volunteers enrolled at 4 different blood centers across the United States and tested for RBC hemolytic propensity (spontaneous, following oxidant, or osmotic insults). Subjects whose RBCs tested in the 5th and 95th percentile for hemolytic propensity were contacted and invited to donate a second unit of blood, for a total of 1929 samples tested in this study. Measurements of S1P from packed RBC units in this study showed a progressive depletion of this metabolite as a function of storage duration (Figure 1B). Such measurements were performed via UHPLC-mass spectrometry, based on accurate intact mass and retention times validated against unlabeled or deuterium-labeled commercial standards (supplemental Figure 1A-B), which also confirmed RBC capacity to take up exogenous S1P in a dose-response manner (supplemental Figure 1C).
RBC S1P decreases during storage and is higher in packed RBCs from female and older donors. (A) An overview of the REDS-IV RBC Omics program is provided in panel A. (B-C) As part of the recalled donor arm of the study, 1929 units from 643 extreme hemolyzing donors were tested for RBC S1P levels (AUs, which were found to decrease during storage (B), and were lower early on during storage in AS-3 packed RBC units (AU) (C). (D-E) Higher levels of S1P were observed in blood donated by female donors (box and whisker plot; median ± ranges[D]), older donors (volcano plot of metabolic correlates to age across all blood donors tested in this study; x-axis indicates log2-fold changes per unit of age for each metabolite and the y-axis indicates the negative log10 of q-values for such correlations [E]), independent storage duration and additive. Asterisks indicate significance (ANOVA with multiple column comparisons; ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001). AU, arbitrary unit.
RBC S1P decreases during storage and is higher in packed RBCs from female and older donors. (A) An overview of the REDS-IV RBC Omics program is provided in panel A. (B-C) As part of the recalled donor arm of the study, 1929 units from 643 extreme hemolyzing donors were tested for RBC S1P levels (AUs, which were found to decrease during storage (B), and were lower early on during storage in AS-3 packed RBC units (AU) (C). (D-E) Higher levels of S1P were observed in blood donated by female donors (box and whisker plot; median ± ranges[D]), older donors (volcano plot of metabolic correlates to age across all blood donors tested in this study; x-axis indicates log2-fold changes per unit of age for each metabolite and the y-axis indicates the negative log10 of q-values for such correlations [E]), independent storage duration and additive. Asterisks indicate significance (ANOVA with multiple column comparisons; ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001). AU, arbitrary unit.
In the REDS-III RBC Omics cohort, S1P was nonnormally distributed across all blood donors at the end of storage (supplemental Figure 2A). Identification of donors in the bottom or top 5% based on S1P levels (supplemental Figure 2B) resulted in the identification of 2 separate groups across storage within the REDS-III RBC Omics cohort. Heat map representation of the top 50 metabolites based on donor S1P levels (supplemental Figure 2C) indicated a positive association between elevated S1P and glycolytic metabolites (fructose bisphosphate, bisphosphoglycerate, phosphoglycerate, phosphoenolpyruvate; supplemental Figure 3), markers of oxidant stress (glutathione disulfide, methionine sulfoxide), and several acylcarnitines, and a negative association with PPP metabolites (6-phosphogluconate, pentose phosphate). Notably, factors like additive solution, donor sex, and age were all associated with an effect on RBC S1P levels, independent of storage duration (Figure 1C-E). Specifically, RBCs stored in additive solution 1, from female and older donors were found to have higher levels of S1P (Figure 1C-E).
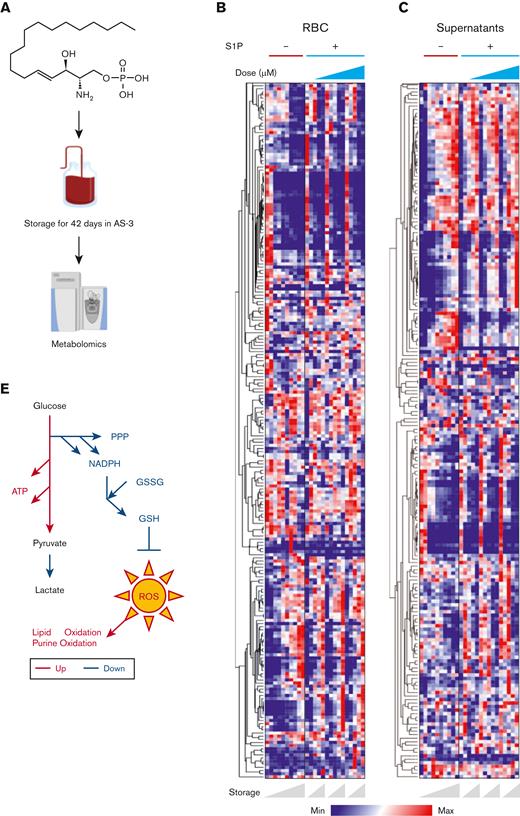
Storage of human RBCs with S1P promotes glycolysis and generation of ATP, at the expense of steady-state levels of metabolites from the PPP and other antioxidant pathways
Previous studies have shown that quality of RBCs declines with storage, as determined by increased hemolytic propensity14 and reduction in PTRs.35,55 Here, S1P decreases were observed as a function of storage duration (Figure 1B). Packed RBCs from female and older donors, all showing higher levels of S1P independent of storage time, have previously been reported to have lower hemolysis,14 metabolic dysregulation,8 and promote higher hemoglobin increments upon transfusion.11,15 Based on these results, we hypothesized that lower levels of RBC S1P are associated with metabolic impairment of ATP and DPG generation capacity, and that storage quality of human RBCs could be improved by supplementation of S1P to storage additives. To test this hypothesis, human packed RBCs were stored in AS-3, either untreated or supplemented with 1, 5, or 10 μM of S1P (Figure 2A). These doses were chosen to recapitulate the ranges in human RBCs exposed to high-altitude hypoxia,37 while remaining below the critical micelle concentration of S1P in aqueous solution (12 μM).56 Statistical analyses, including time-series ANOVA as a function of S1P supplementation dose, revealed a significant impact of S1P on stored human RBC metabolism and supernatants (heat maps in Figure 2B-C, respectively). Notably, S1P did promote increases in the steady-state levels of ATP and glycolytic metabolites (pyruvate, Figure 2D); however, decreases in the steady-state levels of PPP metabolites were observed in a dose-response manner (for example, ribose phosphate and pentose phosphate isomers; sedoheptulose phosphate; Figure 2D). Consistently, we observed decreases in total glutathione (pools of reduced and oxidized), and increases in free long-chain polyunsaturated and highly unsaturated fatty acids (C18:1, 18:3, 20:3, 20:5, 22:5, and 22:6), markers of oxidant stress–induced fatty acid desaturase activity,57 as a function of S1P levels (Figure 2D). Similarly, in S1P-supplemented RBCs we observed an accumulation of oxylipins, including leukotrienes (LTA4 and LTB4) and hydroxyeicosatetraenoic acids, as well as oxidized purines (for example, hypoxanthine), markers of poor PTR in both mice48 and humans58 (Figure 2D). In brief, storage in presence of S1P did boost glycolysis and ATP levels, at the expense of the antioxidant system, that is, the PPP and glutathione pools, and purine and lipid oxidation (Figure 2E).
Storage of human RBCs with S1P promotes glycolysis and generation of ATP, at the expense of steady-state levels of metabolites from the PPP and other antioxidant pathways. (A) Human packed RBCs were stored in AS-3, either untreated or supplemented with 1, 5, or 10 μM of S1P. (B-C) Heat maps from metabolomics analyses of RBCs and supernatants from this experiment are shown in panels B and C, respectively. (D) Line plots (median ± ranges) for representative metabolites in glycolysis (pyruvate), ATP, PPP metabolites (ribose phosphate and pentose phosphate isobars, sedoheptulose phosphate), total glutathione (pools of reduced and oxidized), free fatty acids, and leukotrienes (LTA4 and LTB4). (E) A schematic representation of the results.
Storage of human RBCs with S1P promotes glycolysis and generation of ATP, at the expense of steady-state levels of metabolites from the PPP and other antioxidant pathways. (A) Human packed RBCs were stored in AS-3, either untreated or supplemented with 1, 5, or 10 μM of S1P. (B-C) Heat maps from metabolomics analyses of RBCs and supernatants from this experiment are shown in panels B and C, respectively. (D) Line plots (median ± ranges) for representative metabolites in glycolysis (pyruvate), ATP, PPP metabolites (ribose phosphate and pentose phosphate isobars, sedoheptulose phosphate), total glutathione (pools of reduced and oxidized), free fatty acids, and leukotrienes (LTA4 and LTB4). (E) A schematic representation of the results.
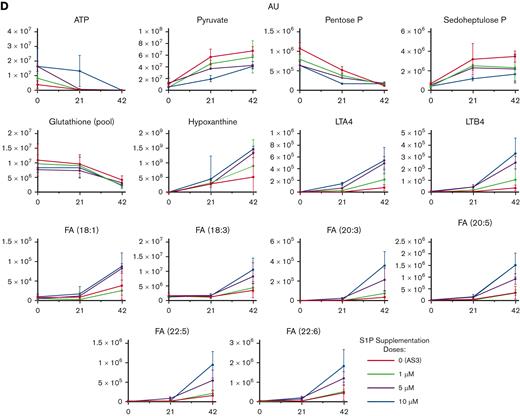
Mouse RBC storage upon supplementation of S1P decreases PTR
To further validate these findings in a tractable animal model, we performed similar storage experiments in mice, in which PTR studies are more easily executed and mechanistic intervention (for example, via genetic ablation of the S1P biosynthetic pathway) are amenable to testing. Cognizant that not all mouse strain RBCs store similarly,46 we performed follow-up studies on multiple mouse strains. Indeed, some mouse strains have been previously46,48 labeled as good storers, because of their elevated PTRs (for example, C57BL6/J), whereas other mouse strains are characterized by an exacerbated metabolic storage lesion and poor PTRs (FVB).46 Therefore, S1P supplementation (5 μM) was performed both in good and poor storer strains (Figure 3A), resulting in lower PTRs in both strain types upon S1P supplementation (Figure 3B-C). An overview of the murine protocol for measurements of PTR with the combined use of UBC-GFP recipient mice and mCHERRY reporter cells is provided in supplemental Figure 4A-C, along with representative scatter plots from flow cytometry experiments. Poorer storage quality in S1P-supplemented RBCs was associated with a measurable effect on glycolysis, and free and acyl-conjugated carnitines in both good storer C57BL/6 and poor storer FVB mice (heat maps in Figure 3D-E, respectively).
Mouse RBC storage upon supplementation of S1P decreases post-transfusion recovery. Post transfusion recovery studies were performed in FVB and C57BL/6 mice upon storage of RBCs for 3 and 6 days in presence or absence of exogenously supplemented S1P (5 μM) (A). Decreases in PTR (median ± ranges) were observed in S1P supplemented mice for 3 and 6 days (B-C). S1P had a measurable effect on stored RBC glycolysis, free and acyl-conjugated carnitines in both good storer C57BL/6 and poor storer FVB mice over storage duration (heat maps in panels D and E, respectively, showing triplicate metabolite measurements at storage days 3 and 6).
Mouse RBC storage upon supplementation of S1P decreases post-transfusion recovery. Post transfusion recovery studies were performed in FVB and C57BL/6 mice upon storage of RBCs for 3 and 6 days in presence or absence of exogenously supplemented S1P (5 μM) (A). Decreases in PTR (median ± ranges) were observed in S1P supplemented mice for 3 and 6 days (B-C). S1P had a measurable effect on stored RBC glycolysis, free and acyl-conjugated carnitines in both good storer C57BL/6 and poor storer FVB mice over storage duration (heat maps in panels D and E, respectively, showing triplicate metabolite measurements at storage days 3 and 6).
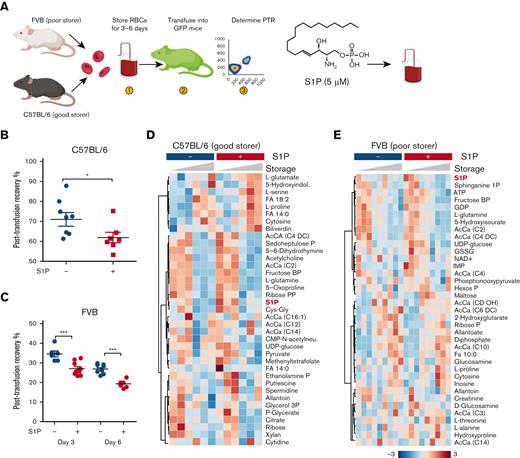
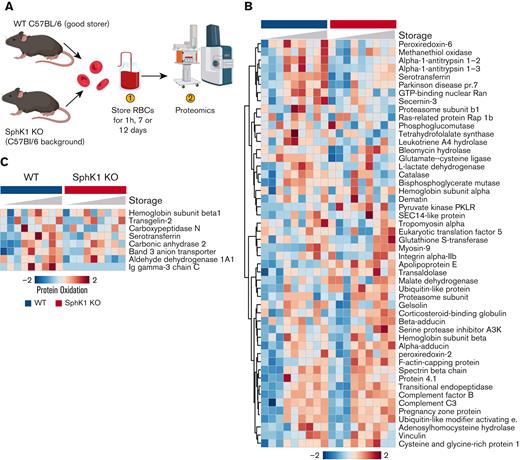
Genetic ablation of S1P biosynthesis in Sphk1 KO mice is associated with improved storage quality
Given the negative effect of S1P supplementation on human and murine RBC storage quality, we hypothesized that an opposite, beneficial effect would be observed in response to genetic ablation of the S1P biosynthetic pathway in Sphk1 KO mice. To test this hypothesis, RBCs from wild-type (WT) C57BL/6 and Sphk1 KO mice were stored (Figure 4A), which resulted in a beneficial effect on storage-induced depletion of acylcarnitines and glutathione pools, and mitigation of free fatty acid and purine oxidation product accumulation (allantoate, heat map in Figure 4B). Confirming Sphk1 genetic ablation, significantly lower levels of RBC S1P were observed in these mice (Sphk1 mice had ∼30% of S1P levels of WT mice at baseline - Figure 4C). Sphk1 KO stored RBCs were also characterized by lower levels of glycolytic metabolites (glucose-6-phosphate and hexose phosphate isomers, fructose bisphosphate, glyceraldehyde-3-phosphate, and DPG) and higher levels of PPP metabolites (6-phosphogluconate, sedoheptulose phosphate; Figure 4D). Consistent with the beneficial effect of decreased S1P levels, Sphk1 mice (already with a C57BL6/J good storer background) had higher PTR (P < .05) than WT good storer mice (Figure 4E).
Improved PTR and antioxidant metabolism in RBCs from Sphk1 KO mice. (A-C) Storage of mouse RBCs from WT C57BL/6 and Sphk1 KO mice (A) resulted in altered metabolism (heat map in panel B), including significantly lower levels of RBC S1P (C), as expected. (D) Specifically, Sphk1 KO stored RBCs were characterized by lower levels of glycolytic metabolites (hexose phosphate, fructose bisphosphate, glyceraldehyde-3-phosphate, and DPG) and higher levels of PPP metabolites (6-phosphogluconate, sedoheptulose phosphate). Sphk1 mice had higher PTR (P < .05) than WT good storer mice (median ± ranges) (E). In panel E, 1 data point for PTR in Sphk1 mice was set to 100%, as explained in “Materials and methods.”
Improved PTR and antioxidant metabolism in RBCs from Sphk1 KO mice. (A-C) Storage of mouse RBCs from WT C57BL/6 and Sphk1 KO mice (A) resulted in altered metabolism (heat map in panel B), including significantly lower levels of RBC S1P (C), as expected. (D) Specifically, Sphk1 KO stored RBCs were characterized by lower levels of glycolytic metabolites (hexose phosphate, fructose bisphosphate, glyceraldehyde-3-phosphate, and DPG) and higher levels of PPP metabolites (6-phosphogluconate, sedoheptulose phosphate). Sphk1 mice had higher PTR (P < .05) than WT good storer mice (median ± ranges) (E). In panel E, 1 data point for PTR in Sphk1 mice was set to 100%, as explained in “Materials and methods.”
Consistent with increased antioxidant capacity and improved metabolic phenotypes and PTRs, Sphk1 mice were characterized by a mitigated storage lesion to the proteome (Figure 5A-B). Specifically, significantly lower levels of oxidized proteins (cysteine and methionine oxidation) were observed in Sphk1 KO mice, including the most abundant cytosolic and membrane proteins, hemoglobin subunit beta 1 and band-3 anion transporter, respectively (Figure 5C).
Impact of Sphk1 KO on the stored RBC proteome. Stored RBCs from Sphk1 mice (A) have lower alterations to the proteome (heat map in panel B), including protein oxidation (heat map in panel C).
Impact of Sphk1 KO on the stored RBC proteome. Stored RBCs from Sphk1 mice (A) have lower alterations to the proteome (heat map in panel B), including protein oxidation (heat map in panel C).
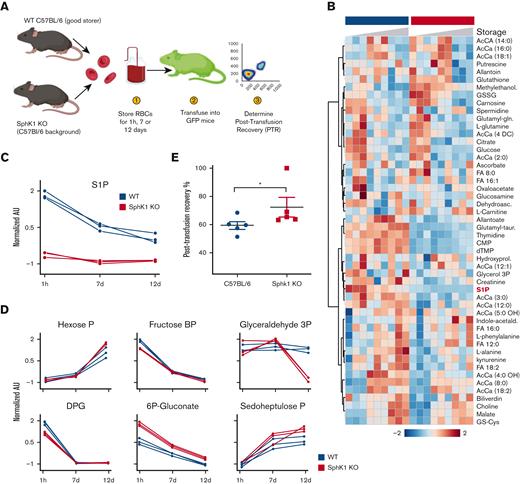
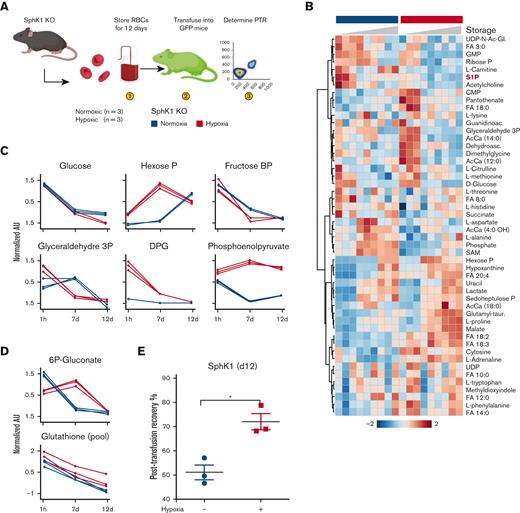
Hypoxic storage of Sphk1 KO RBCs normalizes glycolytic fluxes while preserving fluxes through the PPP, thus further boosting PTRs
Hypoxic storage of human28 and murine (publication forthcoming) RBCs mitigates the metabolic storage lesion and boosts PTRs by promoting glycolysis and mitigating the oxidative storage lesion. Given the apparent effect of Sphk1 on boosting the PPP at the expenses of glycolysis, we hypothesized that altered glucose-oxidation fluxes would be normalized in Sphk1 KO mice by storage in hypoxia (Figure 6A), with consequent benefits on PTRs. Although metabolic effects of hypoxic storage of WT RBCs have recently been described (publication forthcoming), hypoxic Sphk1 KO were found to have significantly different metabolism (Figure 6B). Specifically, compared with their normoxic counterparts, hypoxic Sphk1 KO RBCs had higher glucose consumption, as well as increased levels of multiple glycolytic metabolites (hexose phosphate, DPG, phosphoenolpyruvate; Figure 6C). These changes were not accompanied by decreases in the levels of PPP metabolites (6-phosphogluconate) and total glutathione pools, which were higher in the hypoxic Sphk1 KO mouse RBCs (Figure 6D). These metabolic effects were accompanied by significant improvements in PTRs (Figure 6E).
Impact of hypoxic storage and Sphk1 KO on the stored RBC metabolome. Storage of Sphk1 mouse RBCs under hypoxic conditions (A) further improves the metabolic benefits (heat map in B) of either treatment alone by boosting glycolysis (C), glutathione pools without depressing the PPP (D) and PTR (median ± ranges) (E).
Impact of hypoxic storage and Sphk1 KO on the stored RBC metabolome. Storage of Sphk1 mouse RBCs under hypoxic conditions (A) further improves the metabolic benefits (heat map in B) of either treatment alone by boosting glycolysis (C), glutathione pools without depressing the PPP (D) and PTR (median ± ranges) (E).
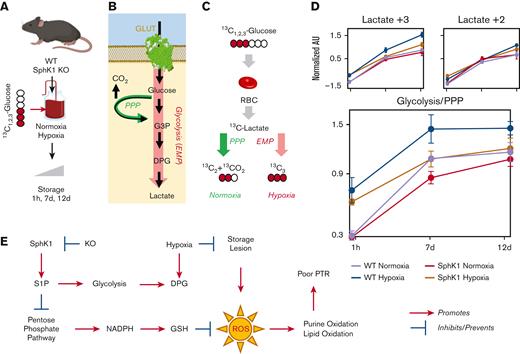
To further confirm the metabolic mechanism driving these observations, we performed tracing experiments with 1,2,3-13C3-glucose (Figure 7A). This approach affords discrimination of metabolic fluxes through glycolysis and the PPP (Figure 7B) via determination of the ratio of +3 and +2 lactate isotopologues (Figure 7C), as previously described.27,32,33 Results clearly indicate that, compared with WT normoxic RBCs, hypoxic WT RBCs had significantly elevated lactate +3 and glycolysis/PPP ratios (Figure 7D). Sphk1 KO mice had slower fluxes through glycolysis compared with WT normoxic and hypoxic RBCs. However, hypoxic Sphk1 KO RBCs had comparable fluxes through glycolysis to WT normoxic RBCs (Figure 7D), despite lower overall storage-induced accumulation of markers of oxidant stress (Figure 6).
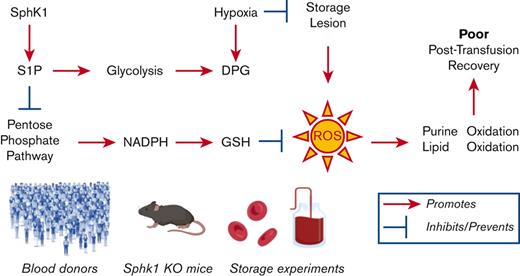
Sphk1 and hypoxia impact metabolic fluxes through glycolysis and the pentose phosphate pathway in stored murine RBCs. Tracing experiments with 1,2,3-13C3-glucose in stored RBCs from WT and Sphk1 mice (A) afford discrimination of metabolic fluxes through glycolysis and the PPP (B) via determination of the ratio of +3 and +2 lactate isotopologues (C). Increases in glycolysis were observed in hypoxia in WT mice but not in Sphk1 mice. (D) However, glycolysis/PPP ratios were basally lower in Sphk1 mice than in controls and were increased by storage in hypoxia in both groups (despite Sphk1 preserving higher PPP activation compared with WT) (median ± ranges). (E) A summary overview of the main findings of this study is provided.
Sphk1 and hypoxia impact metabolic fluxes through glycolysis and the pentose phosphate pathway in stored murine RBCs. Tracing experiments with 1,2,3-13C3-glucose in stored RBCs from WT and Sphk1 mice (A) afford discrimination of metabolic fluxes through glycolysis and the PPP (B) via determination of the ratio of +3 and +2 lactate isotopologues (C). Increases in glycolysis were observed in hypoxia in WT mice but not in Sphk1 mice. (D) However, glycolysis/PPP ratios were basally lower in Sphk1 mice than in controls and were increased by storage in hypoxia in both groups (despite Sphk1 preserving higher PPP activation compared with WT) (median ± ranges). (E) A summary overview of the main findings of this study is provided.
Discussion
In this study, we delved into the role of S1P in RBC storage quality. The underlying hypothesis was that storage depletes ATP and DPG pools, and that S1P can boost ATP and DPG synthesis by promoting metabolic fluxes through glycolysis.37 Because the literature was controversial on the impact of storage on RBC S1P levels, either reporting declines,39 no change,40 or increases with some additives,41 we performed S1P measurements on, to our knowledge, the largest longitudinal sample set of stored RBC samples available to date (∼2000 samples from 643 donors at 3 time points) to confirm that S1P levels do decrease with storage. Notably, we also observed higher levels of S1P, independent of storage duration, in better-storing units (donors with lower hemolytic propensity14), including units from female and older donors. To test the hypothesis that S1P improves RBC storage quality, we either supplemented human and murine RBCs with S1P before storage, or relied on mice lacking the capacity to synthesize S1P (Sphk1 KO). As a result, PTR, proteomics, and steady state and tracing metabolomics experiments all suggest that S1P does indeed boost glycolysis and ATP and DPG generation in stored human and murine RBCs; however, it does so at the expenses of metabolic fluxes through the PPP. This metabolic rewiring comes at the cost of a decreased antioxidant capacity and increased storage-induced oxidation of proteins, lipids, and purines. Indeed, S1P supplementation was associated with increases in the levels of (i) purine oxidation products (hypoxanthine), the result of oxidative stress–activated adenosine monophosphate deaminase 358; (ii) free polyunsaturated fatty acids, the result of oxidant stress–induced fatty acid desaturase activation57; (iii) oxylipins, the result of lipid peroxidation events triggered by dysregulated iron metabolism48; and (iv) thiol groups, histidine and asparagine oxidation in hemoglobin (at cysteine beta 93)59,60 and band 3,26 all critical regulators of RBC function and structure. Of note, all of these aforementioned lesions have previously been associated with poorer PTRs,32,48,57-60 which is what we observed in S1P-supplemented murine units. Genetic manipulation of Sphk1,45 the rate-limiting step in S1P biosynthesis in mature RBCs, counteracts these phenomena, whereas hypoxia boosts glycolysis while normalizing fluxes through glycolysis in Sphk1 KO mice and preventing oxidative metabolic lesions (findings summarized in the schematic in Figure 7E).
Notably, our results suggest that S1P supplementation phenocopies G6PD deficiency, in which a boost in energy metabolism is accompanied by suppressed fluxes through the PPP; as a result G6PD-deficient RBCs are characterized by an increase in oxidant stress to metabolites, proteins, and lipids,7,8 and a negative impact on PTRs.10 Because G6PD activity (and thus PPP fluxes) have previously been reported to decline with age,12 it is interesting to note that, in this study, S1P levels were observed to be positively correlated with donor age. However, it must be noted that healthy, frequent blood donors were enrolled in the REDS study, which biases the population toward subjects with lower propensity to hemolyze following oxidant insults, as reported.61 In addition, because higher G6PD expression and activity levels are associated with longer lifespan,13 a survival bias may exist in older donors who are healthy enough to donate blood frequently. In female blood donors, the negative effect of S1P on PPP activation may be instead counteracted by increased chromosome X–linked G6PD protein dosage, whereby RBC protein levels and activity are higher compared with males despite chromosome-X inactivation.62 In addition, it is worth noting that prior studies on the blood donor exposome have shown how over-the-counter drugs that are not grounds for blood donor deferral (for example, proton pump inhibitors) can boost RBC S1P levels.63 Similarly, it is worth noting that although no genetic polymorphism in Sphk1 was observed to be associated with RBC hemolytic propensity in prior large GWAS studies (for example, REDS III),9 variation in the MFSD2b gene64 (an S1P transporter) was significantly associated with osmotic fragility of the stored RBC.9 Indeed, erythrocytes efficiently utilize exogenous sphingosines for S1P synthesis and export via Mfsd2b.44 The combination of sphingolipid uptake, here validated with deuterium-labeled S1P dose-response incubation experiments, and RBC-specific37 Sphk1 activity regulates not just intraerythrocytic levels of SIP, with RBCs de facto acting as reservoirs that modulate circulating concentrations of S1P.43
Of note, hypoxic storage of Sphk1 RBC boosted energy metabolism while preventing the accumulation of oxidative stress markers. Hypoxic storage improved PTRs of both Sphk1 and WT mice, observation in the latter confirming recent findings in mice.47 This observation is interesting in that we had hypothesized a role for S1P in stabilizing deoxyhemoglobin and promoting glycolysis. However, in the Sphk1 KO mouse the stabilizing effect of S1P on deoxyhemoglobin is limited, which indeed corresponded to slower fluxes through glycolysis compared with WT mice upon exposure to hypoxia. Alkalinization of the intracellular milieu under hypoxic storage conditions had been suggested to boost the activity of phosphofructokinase, biphosphoglycerate mutase, and G6PD, the rate-limiting enzymes of glycolysis, the Rapoport-Luebering shunt, and the PPP, respectively.65 Similar beneficial effects on all 3 pathways are indeed observed when RBCs are stored with alkaline additives.66,67 As such, this study provides further evidence that the pH effect and the oxygen-dependent metabolic modulation model proposed by multiple groups over the years31-33,68 are mutually relevant in the economy of RBC energy/redox glucose-oxidation fluxes, and that S1P does play a nonsecondary role in this system. Notably, storage-induced fragmentation of the N-terminus cytosolic domain of band 3,32,33,69 because of radical attack or caspase activity,70,71 ultimately impairs the RBC capacity to respond to oxidant stress by activating the PPP as a function of high SO2, making S1P-induced promotion of deoxyhemoglobin interaction with the very same N-terminus of band 337 less mechanistically relevant. In light of the decreased stress to band 3 under hypoxic storage conditions,26 it is interesting to hypothesize that S1P supplementation in hypoxically stored erythrocytes may still represent a viable storage strategy to further enhance the metabolic and posttransfusion benefits of these products.28 Similar considerations can be made for alkaline additives.66,67
It should be noted that this study focuses on the stored RBCs and their posttransfusion performances in heterologous, healthy murine recipients. As such, it does not take into account nonhealthy, hypoxic transfusion recipients. Because S1P is depleted in patients that are hypoxic with trauma/hemorrhagic shock72 or with sepsis,73 S1P-containing additives may boost oxygen kinetics in this recipient population and phenocopy the beneficial effects of S1P agonists like FTY720.74 In contrast, in certain categories of recipients, like patients with sickle cell disease, stabilization of deoxy-sickle hemoglobin is potentially deleterious because it would trigger polymerization and sickling.36 All these considerations will be critical if further investigations on the use of S1P as a supplement to blood products are pursued.
Acknowledgments
Research reported in this publication was supported by funds from R01HL146442, R01HL149714, and R01HL148151 (A.D. and J.C.Z.) and R21HL150032 (A.D.) by the National Heart, Lung, and Blood Institute. The REDS-IV-P CTLS project was sponsored by the National Heart, Lung, and Blood Institute contract 75N2019D00033. Samples were collected as part of the NHLBI Recipient Epidemiology and Donor Evaluation Study-III (REDS-III) RBC Omics project, which was supported by National Heart, Lung, and Blood Institute contracts NHLBI HHSN2682011-00001I, -00002I, -00003I, -00004I, -00005I, -00006I, -00007I, -00008I, and -00009I.
Authorship
Contribution: A.D., Y.X., and J.C.Z. designed the study; A.H. performed mouse work and performed mouse PTR studies, and together with J.C.Z. interpreted the results; A.H. and J.C.Z. generated the ROSA26-LCB-mCherry mouse; F.G., T.N., M.D., A.K., and A.D. performed omics analyses; M.P.B. designed and supervised the REDS-III RBC Omics study; K.B. performed bioinformatics analyses; A.D. performed data analysis and prepared figures and tables; A.D. wrote the first draft of the manuscript; and all authors contributed to manuscript revisions, editing, and finalization of the manuscript.
Conflict-of-interest disclosure: The authors declare that A.D. and T.N. are founders of Omix Technologies Inc. A.D. is also a consultant for Rubius Inc and Forma Inc. A.D. is an advisory board member of Macopharma and Hemanext Inc, a company that is developing a product for hypoxic storage of human RBCs. J.C.Z. is a consultant for Rubius Inc, and is a cofounder and the chief scientific officer for Svalinn Therapeutics, a company whose focus is unrelated to the current work. A.D., Y.X., and T.N. hold a patent on S1P supplementation on stored RBC units. The remaining authors declare no competing financial interests.
Correspondence: Angelo D’Alessandro, Department of Biochemistry and Molecular Genetics, University of Colorado Anschutz Medical Campus, 12801 East 17th Ave, Aurora, CO 80045; e-mail: angelo.dalessandro@cuanschutz.edu.
References
Author notes
∗A.H. and T.N. contributed equally to this study and are joint first authors.
Data are available on request from the corresponding author, Angelo D’Alessandro (angelo.dalessandro@cuanschutz.edu).
The full-text version of this article contains a data supplement.

![RBC S1P decreases during storage and is higher in packed RBCs from female and older donors. (A) An overview of the REDS-IV RBC Omics program is provided in panel A. (B-C) As part of the recalled donor arm of the study, 1929 units from 643 extreme hemolyzing donors were tested for RBC S1P levels (AUs, which were found to decrease during storage (B), and were lower early on during storage in AS-3 packed RBC units (AU) (C). (D-E) Higher levels of S1P were observed in blood donated by female donors (box and whisker plot; median ± ranges[D]), older donors (volcano plot of metabolic correlates to age across all blood donors tested in this study; x-axis indicates log2-fold changes per unit of age for each metabolite and the y-axis indicates the negative log10 of q-values for such correlations [E]), independent storage duration and additive. Asterisks indicate significance (ANOVA with multiple column comparisons; ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001). AU, arbitrary unit.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/7/8/10.1182_bloodadvances.2022008936/2/m_blooda_adv-2022-008936-gr1.jpeg?Expires=1765905558&Signature=1jKUM67o0654aa9Scf1OioGzo9ZMn78am7RVq8YiwD84mRXTXDppYz3AxjE~com~DEPqPihyJPM4-xn8i4y7h60~Nne5PnlbZ57S-vEN5X8HOYau8sQqWQf6G9zNldWuaKLcfhQ2d8s~t38ES4b33y7r6K~OJCsdmF7Nq-7EMyKz552upFwOG1pSTKQkMg4pDb6iE5R2EL5gqZZlW7XTAOCJHuSpydS81iGaJYd3orrngcERpwUphWXqqlB1bLlHXKQ7W8fWCHkN6WKQZzmsqLOxdn3toDblLLd4WwkAeWKK22vsy2BT58zYYj4zm-oam9YVUgwy-WVCMi3GR3CKqA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)