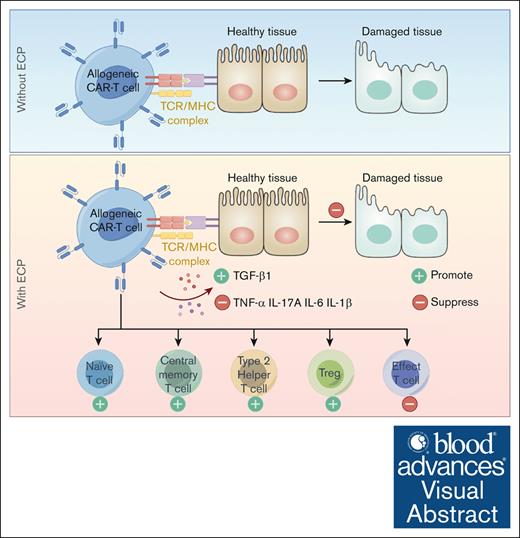
ECP constitutes a promising therapeutic approach for GVHD after CAR T-cell infusion.
ECP reduces alloreactivity without compromising the functionality of CAR-T cells.
Visual Abstract
Graft-versus-host disease (GVHD) occurs in about 10% to 33% of patients receiving “allogeneic” or “autologous” chimeric antigen receptor T (CAR-T) cells after preceding allogeneic hematopoietic stem cell transplantation (allo-HSCT) due to the substantial presence of alloreactive T cells. Extracorporeal photopheresis (ECP) shows promising clinical outcomes in the treatment of GVHD after allo-HSCT without hampering antitumor and antiviral effects. This raises an interesting question: whether ECP might constitute a new way to treat patients with GVHD after CAR T-cell therapy without compromising CAR-T cells significantly. Third-generation CD19-specific CAR-T cells were generated and an in vitro ECP protocol was established. The impact of ECP on CAR-T cells was comprehensively investigated in 2 models: the nondilution model reflects days after CAR T-cell infusion and the dilution model weeks after infusion. The therapeutic effect of ECP on GVHD was examined in an in vitro mixed lymphocyte reaction (MLR) assay. We found, ECP-treated CAR-T cells demonstrated reduced potency in inducing alloreaction compared with that of the group without ECP treatment in MLR assay. ECP could selectively induce apoptosis, thereby enriching the naive and central memory CAR-T cells with a reduced alloreactivity. The cytokine milieu of CAR-T cells could be switched from immune stimulation to immune tolerance in both models. Moreover, ECP could modulate the proliferative capacity of CAR-T cells without hampering their long-term functionality in the dilution model. In conclusion, ECP constitutes a promising treatment strategy for GVHD after allo-HSCT and CAR T-cell transfusion, as ECP reduces the alloreactivity without hampering CAR T-cell functionality.
Introduction
A paradigm shift in the management of hematological malignancies was reached by genetically engineered T cells to express chimeric antigen receptors (CARs). As of now, 6 autologous CAR T-cell products have been approved by the Food and Drug Administration and the European Medicines Agency for the treatment of relapsed/refractory large B-cell lymphoma (Yescarta, Kymriah, Breyanzi), follicular lymphoma (Yescarta, Kymriah, Breyanzi), mantle cell lymphoma (Tecartus), B-cell acute lymphoblastic leukemia (Kymriah, Tecartus), and multiple myeloma (Carvykti, Abecma). Moreover, there is growing interest in the development of “off-the-shelf” allogeneic CAR-T cells to simplify and shorten the manufacturing process and reduce production costs, making CAR-T cells more widely available.1
Although CAR T-cell therapy has shown impressive clinical responses,2 it leads to potentially serious side effects, such as cytokine release syndrome and immune-effector cell-associated neurotoxicity syndrome.3 In addition, as the use of CAR T-cell therapy increases for relapse after allogeneic hematopoietic stem cell transplantation (allo-HSCT) and with the upcoming introduction of allogeneic CAR-T cells, the graft-versus-host disease (GVHD) becomes more pronounced. This holds true regardless of whether it is in the setting of post-HSCT using donor- or recipient–derived CAR-T cells, or in non-HSCT setting involving allogeneic CAR-T cells.4 Notably, GVHD occurs in 10% to 33% of patients receiving donor-derived CAR-T cells.4-9 A recent study demonstrated that patients who developed GVHD after CAR-T treatment didn’t have a history of GVHD during their previous allo-HSCT.9 Therefore, efforts aimed to develop more effective therapies to prevent and treat GVHD in such a setting are needed.
An optional therapy could be extracorporeal photopheresis (ECP), an immunomodulatory therapy. The immunomodulatory mechanisms of ECP include the reinfusion of apoptotic cells after methoxypsoralen and ultraviolet A treatment, which are cleared by the immune system and subsequently stimulate the release of anti-inflammatory cytokines and chemokines. This process reduces the number of T helper 1 (Th1) and Th17 cells and promotes the generation of regulatory T and B cells.10,11 ECP has shown promising results in the management of steroid-resistant/refractory GVHD after allo-HSCT.12-14 Of note, ECP selectively modulates alloreactive T cells without hampering antitumoral and antiviral effects.15 These results led us to test whether ECP could be used to treat GVHD after CAR T-cell therapy without significantly impairing the function of CAR-T cells.
Methods
In vitro ECP treatment
The third-generation of CD19 CAR-T cells were successfully generated using healthy donor peripheral blood mononuclear cells (PBMCs). All donors signed the consent forms. A protocol of in vitro ECP treatment using a UV crosslinker (Bio-Link) was established in this study, which is detailed in the supplemental Information.
Dilution model
To avoid the effect of B cells on CAR-T cells, PBMCs without B cells were used to dilute the auto CAR-T cells, which is detailed in the supplemental Information.
Killing assays
To assess the killing capacity of CAR-T cells, short-term, long-term, and repetitive killing assays were performed in the study, which are explained in the supplemental Information.
MLR assay
The mismatched samples screened by HLA-A2 typing were used to perform the mixed lymphocyte reaction (MLR) experiment. The detailed experiment protocol is described in the supplemental Information.
Beads–based cytokine assay
To assess the influence of ECP on cytokine release of CAR-T cells and the cytokine milieu, supernatant from different settings were collected and quantified by using the bead-based multiplex LEGENDPlex kit (BioLegend). The details are described in the supplemental Information.
Advanced analysis of fluorescence-activated cell sorting and RNA-sequencing (RNA-seq) data
To comprehensively investigate the effect of ECP on CAR-T cells, advanced analyses were developed in this study. Further details are available in the supplemental Information.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 9 (San Diego, CA) . To examine the difference between groups, t tests or Wilcoxon signed-rank test were used for analysis. P values <.05 were regarded as significant difference. Results are shown as mean ± standard deviation, if not specifically labeled.
Results
Less CAR T-cell loss in the dilution model
Based on the dynamics of CD19–CAR T-cell expansion in our phase 1 of clinical trial, patients showed a high percentage of CAR-T cells out of leukocytes (mean, 28%; range, 6.19%-42.28%) in the first 2 months after CAR T-cell infusion, but less than 2% after 3 months (Figure 1A). Nondilution and dilution models were established accordingly to mimic the early and late stages of CAR T-cell therapy in the clinical setting, respectively (Figure 1B).
Effect of ECP therapy on viability, short-term cytotoxicity, component, and cytokine-producing capacity of CAR-T cells in 2 different in vitro models. (A) Proportion of CAR-T cells in the peripheral blood of patients after CAR T-cell therapy (n = 4). (B) Schematic diagram of in vitro dilution CAR T-cell therapy models. (C) Cell loss between the ND and the D models in different dilution ratios. Cell loss was calculated by the following formula: (the absolute number of CAR-T cells without ECP therapy cultured 24 hours) – (the absolute number of CAR-T cells with ECP therapy cultured 24 hours). (D) Representative dot plots of apoptotic CAR-T cells in different dilution ECP therapy models. Apoptotic cells were defined as Apotracker+ cells. (E) Viability of CAR-T cells shown for the ND and the D models in different dilution ratios. Nonliving cells were defined as Apotracker+cells and 7AAD+cells. (F) Representative dot plots of specific killing efficiency of CAR-T cells and unspecific killing capacity of PBMCs with or without ECP in a ratio of 1:1 to Raji tumor cells. (G) Summarized killing efficiency of CAR-T cells with or without ECP therapy in the ND and the D models. The killing efficiency was calculated by the following formula: ([initial number of tumor cells – residual number of tumor cells] × 100)/(initial number of tumor cells). (H) Absolute residual number of tumor cells after 24 hour coculture with ECP-treated CAR-T cells or ECP-treated PBMCs in the ND and the D models. (I) Contribution of unspecific killing capacity of PBMCs in the dilution model. The killing contribution of PBMCs was estimated by using the identical D model without CAR-T cells. (J) Component of CAR-T cells with respect to CD4/CD8 ratio before and after ECP treatment in the ND and the D models. (K) Influence of ECP treatment on TNF-α, IFN-γ, and multifunctional (TNF-α+IFN-γ+) cytokine production of CAR-T cells was determined after 4 hour tumor cell stimulation in an effector/tumor (E/T) ratio of 1:1 by an intracellular cytokine staining. A 2-tailed t test was performed for statistical analysis. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. ND, nondilution; D, dilution
Effect of ECP therapy on viability, short-term cytotoxicity, component, and cytokine-producing capacity of CAR-T cells in 2 different in vitro models. (A) Proportion of CAR-T cells in the peripheral blood of patients after CAR T-cell therapy (n = 4). (B) Schematic diagram of in vitro dilution CAR T-cell therapy models. (C) Cell loss between the ND and the D models in different dilution ratios. Cell loss was calculated by the following formula: (the absolute number of CAR-T cells without ECP therapy cultured 24 hours) – (the absolute number of CAR-T cells with ECP therapy cultured 24 hours). (D) Representative dot plots of apoptotic CAR-T cells in different dilution ECP therapy models. Apoptotic cells were defined as Apotracker+ cells. (E) Viability of CAR-T cells shown for the ND and the D models in different dilution ratios. Nonliving cells were defined as Apotracker+cells and 7AAD+cells. (F) Representative dot plots of specific killing efficiency of CAR-T cells and unspecific killing capacity of PBMCs with or without ECP in a ratio of 1:1 to Raji tumor cells. (G) Summarized killing efficiency of CAR-T cells with or without ECP therapy in the ND and the D models. The killing efficiency was calculated by the following formula: ([initial number of tumor cells – residual number of tumor cells] × 100)/(initial number of tumor cells). (H) Absolute residual number of tumor cells after 24 hour coculture with ECP-treated CAR-T cells or ECP-treated PBMCs in the ND and the D models. (I) Contribution of unspecific killing capacity of PBMCs in the dilution model. The killing contribution of PBMCs was estimated by using the identical D model without CAR-T cells. (J) Component of CAR-T cells with respect to CD4/CD8 ratio before and after ECP treatment in the ND and the D models. (K) Influence of ECP treatment on TNF-α, IFN-γ, and multifunctional (TNF-α+IFN-γ+) cytokine production of CAR-T cells was determined after 4 hour tumor cell stimulation in an effector/tumor (E/T) ratio of 1:1 by an intracellular cytokine staining. A 2-tailed t test was performed for statistical analysis. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. ND, nondilution; D, dilution
Short-term cytotoxicity and cytokine-producing capacity of CAR-T cells in the dilution model are not hampered by ECP therapy
To determine whether ECP treatment affect the short-term cytotoxic potential and cytokine-producing ability of CAR-T cells, ECP-treated nondiluted CAR-T cells or CAR-T cells diluted with B-cell–depleted auto-PBMCs were cocultured with CD19+Raji cells for 24 hours. Even though ECP treatment could hamper the killing efficiency of CAR-T cells in the nondilution model with an average decrease of 25% (Figure 1F-G; supplemental Figure 1), the cytotoxicity of CAR-T cells in the dilution model could be maintained when compared with untreated CAR-T cells. To exclude the possibility that NK, NKT, and γδT cells in auto-PBMCs contribute to this killing efficacy, an identical number of auto-PBMCs as the dilution model were cocultured with Raji cells, demonstrating that PBMCs barely kill tumor cells (Figure 1F,H-I). Moreover, the CD4 and CD8 ratio was not influenced by ECP therapy in both non-dilution and dilution models, as illustrated in Figure 1J.
In accordance with the cytotoxicity findings, the frequency of TNF-α+ and TNF-α+IFN-γ+ producing CAR-T cells was decreased in the nondilution model with ECP treatment, whereas comparable in the dilution model. Interestingly, the frequency of IFN-γ+CAR-T cells was not affected by ECP in both models (Figure 1K; supplemental Figures 1-3). Surprisingly, both short-term cytotoxicity and cytokine-producing capacity of CAR-T cells were unaffected by ECP treatment in the dilution model (Figure 1G,K).
Moderate proliferation of CAR-T cells with constant cytotoxicity in the dilution model
To better understand the long-term effect of ECP on CAR-T cells, the proliferative capacity with the dynamic of cell expansion, the long-term cytotoxicity and the persistence of CAR-T cells were investigated as key parameters in both dilution and nondilution models.
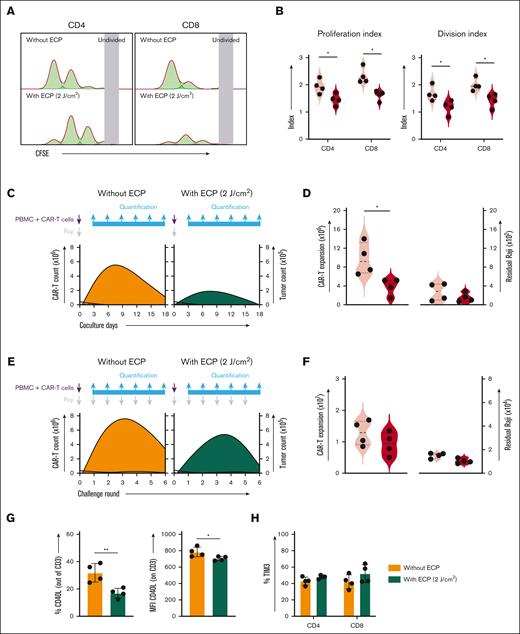
To quantify the proliferative capacity of CAR-T cells, the proliferation index representing how fast responding cells are proliferating and the division index interpreting the average number of divisions for all cells in the original culture, were calculated by a proliferation modeling tool in FlowJo. We found that ECP therapy could limit the proliferation of both CD4+ and CD8+CAR-T cells (Figure 2A-B; supplemental Figures 4,5A-B, and 6A-B), resulting in a moderate CAR T-cell expansion upon 1-time (Figure 2C-D; supplemental Figures 5C-D and 6C-D) or continuous (Figure 2E-F; supplemental Figures 5E-F and 6E-F) stimulation by tumor cells in both dilution (Figure 2; supplemental Figure 5) and nondilution models (supplemental Figure 6). Because CD40L plays an important role in the promotion of T-cell proliferation, we measured the frequency and density of CD40L expression on CD3+CAR-T cells (supplemental Figure 7). However, our results demonstrated that CD40L might only partly explain this moderate proliferative capability because a dramatic decrease of CD40L expression was only observed in the dilution model (Figure 2G) but not in the non-dilution model (supplemental Figure 6G).
Effect of ECP therapy on proliferation and long-term cytotoxicity of CAR-T cells in the D model (stimulation by Raji cells). (A) Representative histogram of proliferation of CD4+ and CD8+CAR-T cells with or without ECP therapy after 3 day stimulation by irradiated tumor cells. (B) Statistical analysis of proliferation of CD4+ and CD8+CAR-T cells with or without ECP therapy. (C) The influence of ECP on the expansion of CAR-T cells in a long-term culture assay. The dark curves display the dynamic of tumor cells and the orange and green curves indicate the dynamic of CAR-T cells. The purple arrow represents CAR-T cells and PBMCs in the coculture killing assay, whereas the gray arrow represents tumor cells, which were added once, initially. In addition, the blue arrows represent the quantification of cells in the coculture system every 3 days. (D) The expansion peak of CD3+CAR-T cells (left panel) and the residual tumor cells on the last day of coculture (right panel) in the long-term culture assay. (E) The effect of ECP on the serial killing capacity of CAR-T cells in a challenging assay. The dark curves display the dynamic of tumor cells and the orange and green curves indicate the dynamic of CAR-T cells. The purple arrow represents CAR-T cells and PBMCs in the coculture killing assay, whereas the gray arrow represents tumor cells, which were added in each round. In addition, the blue arrows represent the quantification of cells in the coculture system in every round. (F) The expansion peak of CD3+CAR-T cells (left panel) and the residual tumor cells on the last day of coculture (right panel) in the challenging assay. (G) The effect of ECP therapy on costimulatory marker CD40L expression with or without ECP treatment after 24 hour stimulation with CD19+Raji cells: the frequency of CD40L+CD3+CAR-T cells (left panel) and the density of CD40L expression on CD3+CAR-T cells (right panel). (H) The effect of ECP on expression of the exhaustion marker TIM3 in CD4+ and CD8+CAR-T cells. Samples of 4 individual donors were tested. A 2-tailed t test was used for statistical analysis. ∗P < .05; ∗∗P < .01.
Effect of ECP therapy on proliferation and long-term cytotoxicity of CAR-T cells in the D model (stimulation by Raji cells). (A) Representative histogram of proliferation of CD4+ and CD8+CAR-T cells with or without ECP therapy after 3 day stimulation by irradiated tumor cells. (B) Statistical analysis of proliferation of CD4+ and CD8+CAR-T cells with or without ECP therapy. (C) The influence of ECP on the expansion of CAR-T cells in a long-term culture assay. The dark curves display the dynamic of tumor cells and the orange and green curves indicate the dynamic of CAR-T cells. The purple arrow represents CAR-T cells and PBMCs in the coculture killing assay, whereas the gray arrow represents tumor cells, which were added once, initially. In addition, the blue arrows represent the quantification of cells in the coculture system every 3 days. (D) The expansion peak of CD3+CAR-T cells (left panel) and the residual tumor cells on the last day of coculture (right panel) in the long-term culture assay. (E) The effect of ECP on the serial killing capacity of CAR-T cells in a challenging assay. The dark curves display the dynamic of tumor cells and the orange and green curves indicate the dynamic of CAR-T cells. The purple arrow represents CAR-T cells and PBMCs in the coculture killing assay, whereas the gray arrow represents tumor cells, which were added in each round. In addition, the blue arrows represent the quantification of cells in the coculture system in every round. (F) The expansion peak of CD3+CAR-T cells (left panel) and the residual tumor cells on the last day of coculture (right panel) in the challenging assay. (G) The effect of ECP therapy on costimulatory marker CD40L expression with or without ECP treatment after 24 hour stimulation with CD19+Raji cells: the frequency of CD40L+CD3+CAR-T cells (left panel) and the density of CD40L expression on CD3+CAR-T cells (right panel). (H) The effect of ECP on expression of the exhaustion marker TIM3 in CD4+ and CD8+CAR-T cells. Samples of 4 individual donors were tested. A 2-tailed t test was used for statistical analysis. ∗P < .05; ∗∗P < .01.
Unlike the proliferation, the long-term antitumor activity of ECP-treated CAR-T cells was not substantially affected in the dilution model, which is evidenced by a similar number of residual tumor cells upon 1-time (Figure 2C-D; supplemental Figure 5C-D) or repetitive (Figure 2E-F; supplemental Figure 5E-F) tumor challenge. The analysis strategy and the representative dot plots were shown in supplemental Figures 8-10. Contrasting results were observed for the effect of ECP treatment in the nondilution model. Specifically, the findings indicated a failure of ECP-treated CAR-T cells to eliminate tumor cells after 10 days, in which tumor cells were added once at the beginning (supplemental Figure 6C-D). Additionally, there was a trend suggesting an increase in tumor cells with an early breakout when tumor cells were added in each round (supplemental Figure 6E-F).
Furthermore, the influence of ECP on the persistence of CAR-T cells was investigated by monitoring the expression of inhibitory molecule T cell immunoglobulin and mucin domain-containing protein 3 (TIM3) on CAR-T cells during the repetitive tumor challenge (supplemental Figure 8). We observed a comparable expression of TIM3 on CAR-T cells with and without ECP in both dilution (Figure 2H; supplemental Figure 5G) and nondilution (supplemental Figure 6H) models, suggesting that ECP has no negative effect on the persistence of CAR-T cells.
Favorable immunoregulatory cytokine profile by ECP therapy
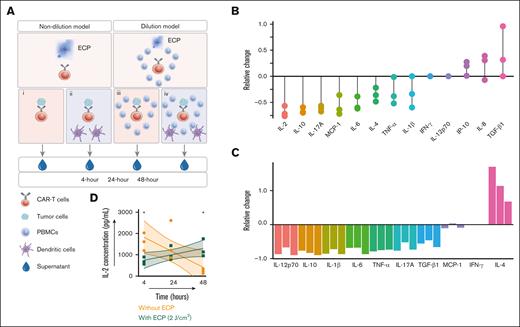
To determine the effect of ECP treatment on the cytokine profile of activated CAR-T cells, 4 coculture settings were established to monitor a broad array of cytokines in the supernatant over the time (Figure 3A).
Effect of ECP on cytokine profile of CAR-T cells. (A) Schematic diagram of beads–based cytokine analysis. After ECP treatment, CAR-T cells or CAR-T cells with auto-PBMCs were stimulated with CD19+ tumor cells in the absence or presence of APCs. The supernatants were collected after 4 hour, 24 hour, and 48 hour stimulation. Setting i: stimulation of CAR-T cells without APCs in the ND model. Setting ii: stimulation of CAR-T cells with APCs in the ND model. Setting iii: stimulation of CAR-T cells without APCs in the dilution model. Setting iv: stimulation of CAR-T cells with APCs in the dilution model. (B) The relative change of 24 hour cytokine secretion in the setting i. Every dot represents an individual donor. (C) The relative change of 24 hour cytokine secretion in the setting iv. Every bar represents an individual donor. Relative change of cytokine secretion was calculated = (cytokine concentration of ECP-treated CAR T-cell group – cytokine concentration of ECP-untreated CAR T-cell group)/(cytokine concentration of ECP-untreated CAR T-cell group). (D) Effect of ECP on the dynamics of IL-2 secretion over time. Samples of 3 individual donors were tested. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. APC, antigen presenting cell.
Effect of ECP on cytokine profile of CAR-T cells. (A) Schematic diagram of beads–based cytokine analysis. After ECP treatment, CAR-T cells or CAR-T cells with auto-PBMCs were stimulated with CD19+ tumor cells in the absence or presence of APCs. The supernatants were collected after 4 hour, 24 hour, and 48 hour stimulation. Setting i: stimulation of CAR-T cells without APCs in the ND model. Setting ii: stimulation of CAR-T cells with APCs in the ND model. Setting iii: stimulation of CAR-T cells without APCs in the dilution model. Setting iv: stimulation of CAR-T cells with APCs in the dilution model. (B) The relative change of 24 hour cytokine secretion in the setting i. Every dot represents an individual donor. (C) The relative change of 24 hour cytokine secretion in the setting iv. Every bar represents an individual donor. Relative change of cytokine secretion was calculated = (cytokine concentration of ECP-treated CAR T-cell group – cytokine concentration of ECP-untreated CAR T-cell group)/(cytokine concentration of ECP-untreated CAR T-cell group). (D) Effect of ECP on the dynamics of IL-2 secretion over time. Samples of 3 individual donors were tested. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. APC, antigen presenting cell.
The direct effect of ECP on activated CAR-T cells was evaluated in the coculture setting i in the nondilution model. Our results showed that ECP-treated CAR-T cells exerted less potency in secreting cytokine release syndrome-related cytokines such as IL-6, IL-10, IL-17A, TNF-α, and IL-1β, but were prone to release more IP-10, IL-8, and TGF-β (Figure 3B), when compared with those without ECP treatment. Consistent with the intracellular staining result (Figure 1K), the secretion of IFN-γ by activated CAR-T cells was not affected by ECP treatment in the setting i (Figure 3B).
To mimic the clinical setting, a quadripartite coculture consisting of Raji cells, CAR-T cells, auto-PBMCs, and auto-iDCs was set up as shown in Figure 3Aiv. Cytokines released by immune components in concert with activated CAR-T cells were assessed and revealed a distinctive cytokine profile, when compared with the setting without ECP treatment (Figure 3C) or without bystander cells (Figure 3B). The anti-inflammatory cytokine IL-4 was elevated in the ECP group, accompanied by a reduction of proinflammatory cytokines (Figure 3C). Moreover, the kinetics of different cytokines were also examined in the setting iv. Relative to CAR-T cells without ECP treatment, which provoking a peak of IL-2 release within 24 hours followed by a significant decrease, a steady increase of IL-2 was found in the ECP-treated CAR T-cell group (Figure 3D).
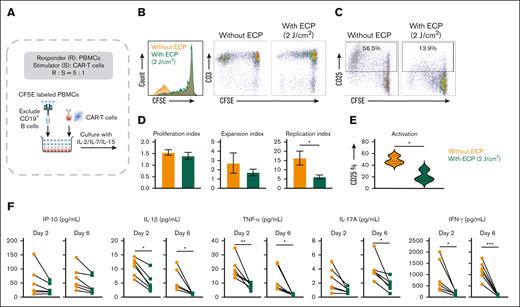
Inhibition of alloreactive T cells in terms of proliferation, activation, and cytokine release by ECP therapy
To examine the therapeutic effect of ECP on GVHD, we performed an in vitro MLR assay in which carboxyfluorescein diacetate succinimidyl ester (CFSE)-labeled PBMCs were stimulated with HLA-A2 mismatched CAR-T cells that were treated either with or without ECP (Figure 4A). Our data showed that ECP-treated CAR-T cells exhibited a lower potency to induce an alloreaction on responder PBMCs when compared with the group without ECP treatment (Figure 4B-C).
Effect of ECP therapy on alloreactive T cells. (A) Schematic diagram of the in vitro alloreaction model. (B) Representative histogram and dot plot of proliferation of responder cells in the alloreaction model. (C) Representative dot plot of activation status of responder cells in the alloreaction model. (D) Statistical analysis of proliferation of responder cells. (E) Statistical analysis of activation of responder cells. Samples of 3 individual donors were tested for proliferation and activation assays. (F) Cytokine profile in the supernatant of alloreaction model over time. CAR-T cells with and without ECP as stimulatory cells derived from 2 individual donors were used to stimulate allo-PBMCs derived from another 3 HLA-A2 mismatched donors. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001.
Effect of ECP therapy on alloreactive T cells. (A) Schematic diagram of the in vitro alloreaction model. (B) Representative histogram and dot plot of proliferation of responder cells in the alloreaction model. (C) Representative dot plot of activation status of responder cells in the alloreaction model. (D) Statistical analysis of proliferation of responder cells. (E) Statistical analysis of activation of responder cells. Samples of 3 individual donors were tested for proliferation and activation assays. (F) Cytokine profile in the supernatant of alloreaction model over time. CAR-T cells with and without ECP as stimulatory cells derived from 2 individual donors were used to stimulate allo-PBMCs derived from another 3 HLA-A2 mismatched donors. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001.
The proliferation, expansion, and replication indices, which are indicative for the proliferative capacity, were decreased by ECP, especially the replication index indicating the expansion capability of the responder PBMCs (Figure 4D). Besides the proliferation, we observed an impaired activation of alloreactive T cells, reflected by a considerable reduction of CD25 expression from 48.6 ± 7.2% to 21.6 ± 9.9% (Figure 4C,E).
Notably, the cytokine milieu of MLR with ECP was distinct from that observed when responder PBMCs were stimulated by CAR-T cells without ECP. A prominent decrease of proinflammatory cytokines was observed (Figure 4F). In the ECP treatment group, the levels of IL-1β, TNF-α, and IFN-γ in the supernatant were significantly decreased in both the initial and the end of MLR coculture, accompanied by a moderate decline of IL-17A and IP-10 in the initial phase but a remarkable reduction of IL-17A at the end of coculture (Figure 4F).
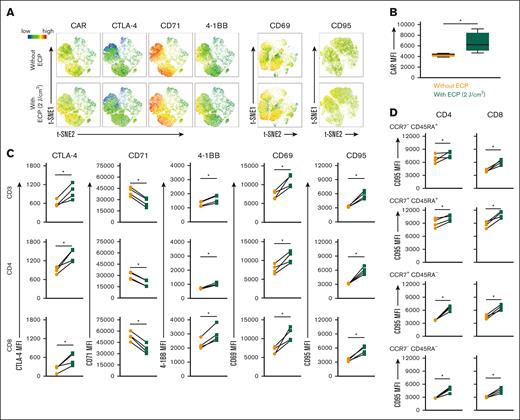
Modulation of CAR T-cell surface protein expression by ECP treatment
The direct impact of ECP on CAR-T cells was evaluated in the non-dilution model by measuring the different surface proteins on CAR-T cells. It is of note that ECP obviously affected CAR-T cells in the nondilution model, with a change of the density of some surface proteins as shown in Figure 5A.
Effect of ECP therapy on surface protein expression of CAR-T cells. (A) Surface markers expression intensity in t-SNE plot. (B) MFI of CAR expression on CAR-T cells with/without ECP treatment. (C) Effect of ECP therapy on the expression intensity of surface markers on CAR-T cells. (D) Effect of ECP therapy on the expression intensity of CD95 on effector (CCR7-CD45RA+), naive (CCR7+CD45RA+), central memory (CCR7+CD45RA-), and effector memory (CCR7-CD45RA-) of CD4+ and CD8+CAR-T cells. Samples of 4 individual donors were tested. ∗P < .05.
Effect of ECP therapy on surface protein expression of CAR-T cells. (A) Surface markers expression intensity in t-SNE plot. (B) MFI of CAR expression on CAR-T cells with/without ECP treatment. (C) Effect of ECP therapy on the expression intensity of surface markers on CAR-T cells. (D) Effect of ECP therapy on the expression intensity of CD95 on effector (CCR7-CD45RA+), naive (CCR7+CD45RA+), central memory (CCR7+CD45RA-), and effector memory (CCR7-CD45RA-) of CD4+ and CD8+CAR-T cells. Samples of 4 individual donors were tested. ∗P < .05.
ECP-treated CAR-T cells showed a significant elevation of CAR expression after 24 hours of incubation with Raji (Figure 5B). In parallel, activation markers such as 4-1BB and CD69 were markedly upregulated (Figure 5A,C). Interestingly, the coinhibitory molecule CTLA-4 was also increased, which could be an indication of the inhibition of the costimulatory signal (Figure 5A,C).
A downregulation of the proliferation indicator CD71 by ECP (Figure 5A,C) confirmed our proliferation results as shown in supplemental Figure 6A-B. Moreover, in accordance with the apoptosis effect of ECP on CAR-T cells (Figure 1D), an apparent increase of apoptotic related molecule CD95 was observed not only on the lineage (Figure 5A,C) but also on the subsets of CAR-T cells (Figure 5D).
Identification of ECP effect on diverse CAR T-cell populations by machine learning
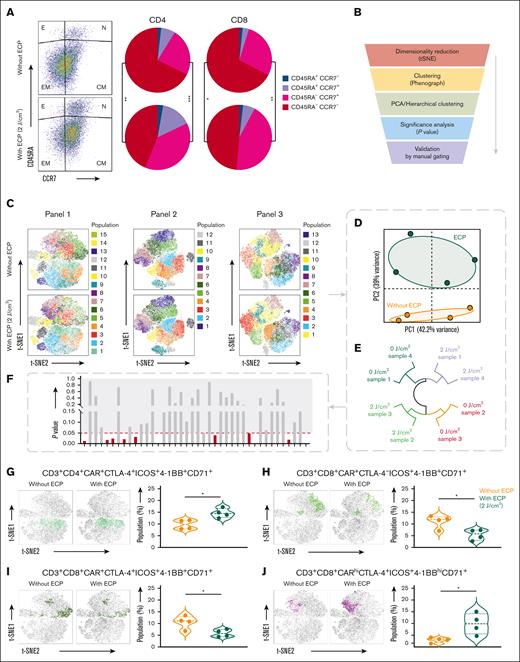
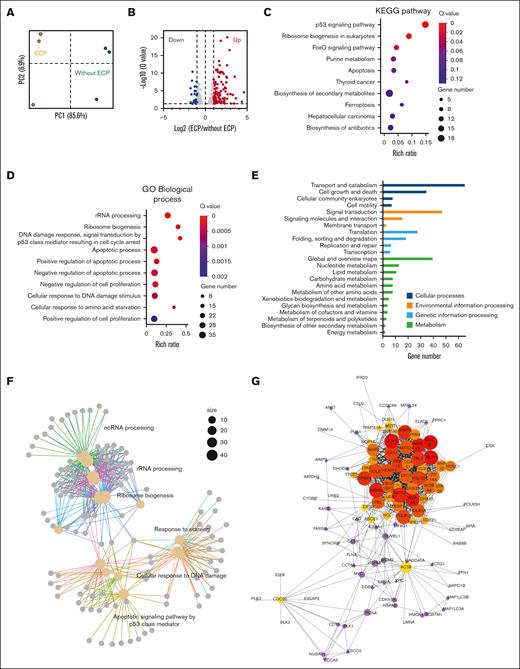
The influence of ECP on the frequency of diverse cell populations was comprehensively investigated. The components of CAR-T cells in terms of effector T cells (TE), naive T cells (TN), central memory T cells (TCM), and effector memory T cells (TEM) were modified by ECP therapy, showing an increased proportion of TN and TCM cells (Figure 6A). Additionally, an advanced data mining strategy based on machine learning was established and applied to our immunophenotyping data (Figure 6B), which allowed us to detect previously unknown cell populations in an unbiased, data-driven manner without information loss. In total, 40 different cell clusters were identified and projected in the t-SNE space (Figure 6C). ECP-treated CAR-T cells displayed distinct patterns (Figure 6D,E) with some biological variation (Figure 6E), suggesting the potency of these cell clusters to identify the effect of ECP on CAR-T cells.
Effect of ECP therapy on frequency of cell populations. (A) Representative dot plot and statistical analysis of components of CD4+ and CD8+CAR-T cells with respect to effector (E; CCR7-CD45RA+), naive (N; CCR7+CD45RA+), central memory (CM; CCR7+CD45RA–), and effector memory (EM; CCR7-CD45RA-) subsets. (B) Workflow of data mining algorithm. (C) t-SNE plot of Phenograph identified cell clusters. Evaluation of distinguishing capability of cell clusters by principal component analysis (PCA) (D) and hierarchical cluster (E). (F) Identification of cell clusters by significance analysis. (G-N) t-SNE plot and statistical analysis of cell clusters. Samples of 4 individual donors were tested. A 2-tailed t test was used for statistical analysis. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001.
Effect of ECP therapy on frequency of cell populations. (A) Representative dot plot and statistical analysis of components of CD4+ and CD8+CAR-T cells with respect to effector (E; CCR7-CD45RA+), naive (N; CCR7+CD45RA+), central memory (CM; CCR7+CD45RA–), and effector memory (EM; CCR7-CD45RA-) subsets. (B) Workflow of data mining algorithm. (C) t-SNE plot of Phenograph identified cell clusters. Evaluation of distinguishing capability of cell clusters by principal component analysis (PCA) (D) and hierarchical cluster (E). (F) Identification of cell clusters by significance analysis. (G-N) t-SNE plot and statistical analysis of cell clusters. Samples of 4 individual donors were tested. A 2-tailed t test was used for statistical analysis. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001.
The subsequent downstream analysis is focused on statistical assessment, resulting in 11 significantly different cell clusters defined as P value <.05 (Figure 6F). The retained cell clusters were further validated by manual gating to ensure the robustness. Thereafter, only 8 cell populations were considered to correlate with the ECP effect (Figure 6G-N). We observed that ECP treatment could elevate the frequency of 5 cell clusters shown in Figure 6G-N but decrease 3 cell populations shown in Figure 6G-N.
Induction of selective apoptosis of CAR-T cells by ECP therapy
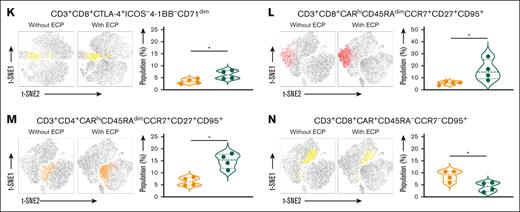
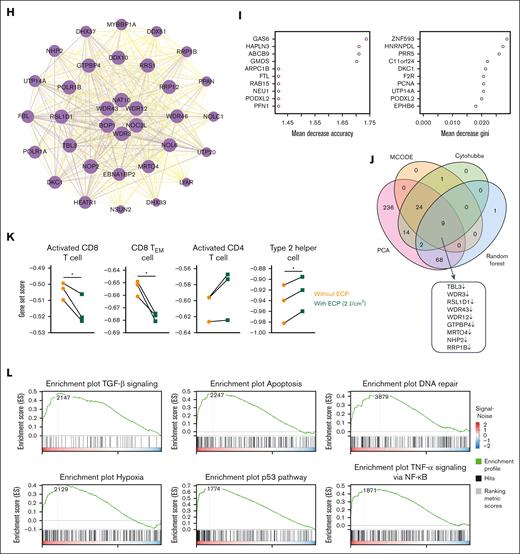
To discover the mechanism of ECP effect on CAR-T cells, we further performed RNA-seq analysis on CAR-T cells cultured for 16 hour that were treated either with or without ECP. The principal component analysis plot showed ECP treatment could cause a pronounced alteration in the transcriptional profile of CAR-T cells (Figure 7A).
Effect of ECP therapy on CAR-T cells at the transcriptional level. (A) PCA of transcriptomes of ECP-treated or untreated CAR-T cells after 16 hour culture, in which Fragments Per Kilobase Million (FPKM) value was used as the input data for each gene in different samples. (B) Volcano map of DEGs between ECP-treated and untreated groups. DEGs were defined as |Log2FC| ≥ 1 and Q value ≤0.05. (C) KEGG pathway analysis of DEGs showing the top 10 enriched pathways. The color indicates the Q value, and the size of nodes was scaled by the gene number. (D) Gene ontology enrichment analysis of DEGs showing the top 10 enriched gene ontology terms in biological process. (E) Classification of enriched KEGG pathways in cellular processes, environmental information processing, genetic information processing, and metabolism. (F) Network analysis of enriched biological process of gene ontology. The size of nodes is scaled by the gene number. (G) Protein-protein interaction network analysis of DEGs by Cytohubba. The top 50 DEGs were colored by yellow and red, whereas the neighbors were colored by purple. (H) Protein-protein interaction network analysis of DEGs by molecular complex detection. (I) Prioritization of DEGs by random forest analysis. The DEGs were ranked by mean decrease in accuracy and mean decrease in Gini. (J) Identification of hub genes by combination of 4 different algorithms. The Venn plot illustrates the number of overlap genes in all different combinations of analyses, including PCA, Cytohubba, molecular complex detection, and random forest analysis. (K) Gene signature sets for immunophenotypes assessed by single sample gene set enrichment analysis. A 2-tailed t test was used for statistical analysis. ∗P < .05. (L) Gene set enrichment analysis of ECP-treated and untreated CAR-T cells. On the x-axis, gene sets are represented by vertical black lines, whereas the enrichment score (ES) is plotted on the y-axis. Points representing genes and their corresponding ES are connected by a green line. The colored band at the bottom indicates the correlation of genes with the ECP treatment, with red indicating a positive correlation and blue indicating a negative correlation. The significance threshold is set at false discovery rate of <0.05. The color code represents the signal to noise. Samples of 3 individual donors were tested.
Effect of ECP therapy on CAR-T cells at the transcriptional level. (A) PCA of transcriptomes of ECP-treated or untreated CAR-T cells after 16 hour culture, in which Fragments Per Kilobase Million (FPKM) value was used as the input data for each gene in different samples. (B) Volcano map of DEGs between ECP-treated and untreated groups. DEGs were defined as |Log2FC| ≥ 1 and Q value ≤0.05. (C) KEGG pathway analysis of DEGs showing the top 10 enriched pathways. The color indicates the Q value, and the size of nodes was scaled by the gene number. (D) Gene ontology enrichment analysis of DEGs showing the top 10 enriched gene ontology terms in biological process. (E) Classification of enriched KEGG pathways in cellular processes, environmental information processing, genetic information processing, and metabolism. (F) Network analysis of enriched biological process of gene ontology. The size of nodes is scaled by the gene number. (G) Protein-protein interaction network analysis of DEGs by Cytohubba. The top 50 DEGs were colored by yellow and red, whereas the neighbors were colored by purple. (H) Protein-protein interaction network analysis of DEGs by molecular complex detection. (I) Prioritization of DEGs by random forest analysis. The DEGs were ranked by mean decrease in accuracy and mean decrease in Gini. (J) Identification of hub genes by combination of 4 different algorithms. The Venn plot illustrates the number of overlap genes in all different combinations of analyses, including PCA, Cytohubba, molecular complex detection, and random forest analysis. (K) Gene signature sets for immunophenotypes assessed by single sample gene set enrichment analysis. A 2-tailed t test was used for statistical analysis. ∗P < .05. (L) Gene set enrichment analysis of ECP-treated and untreated CAR-T cells. On the x-axis, gene sets are represented by vertical black lines, whereas the enrichment score (ES) is plotted on the y-axis. Points representing genes and their corresponding ES are connected by a green line. The colored band at the bottom indicates the correlation of genes with the ECP treatment, with red indicating a positive correlation and blue indicating a negative correlation. The significance threshold is set at false discovery rate of <0.05. The color code represents the signal to noise. Samples of 3 individual donors were tested.
Consequently, 372 differentially expressed genes (DEGs) were identified when comparing ECP-treated CAR-T cells with untreated CAR-T cells (Figure 7B). These DEGs were further functionally annotated by Kyoto Encyclopedia of Genes and Genomes (KEGG) (Figure 7C) and gene ontology biological process (Figure 7D) enrichment analyses, along with KEGG pathway classification analysis (Figure 7E), indicating a strong enrichment in pathways related to ribosome biogenesis and rRNA processing, DNA damage, and apoptosis, as well as proliferation and metabolism. The relationship of different pathways was also explored by a network analysis (Figure 7F), pointing out a similar result as KEGG and gene ontology enrichment analyses.
To screen the hub genes, a protein-protein interaction network was constructed based on these 372 DEGs, followed by weighing the genes in the network with the maximal clique centrality calculation (Figure 7G) and the molecular complex detection algorithm (Figure 7H). A total of 50 and 34 hub genes were identified by these 2 algorithms, respectively.
The random forest model was applied to rank the DEGs based on the potency to distinguish ECP-treated CAR-T cells from untreated CAR-T cells. Mean decrease in accuracy and mean decrease in Gini index determined the ranking of DEGs (Figure 7I). The top 10 genes for each index were shown as an example in Figure 7I. In addition, principal component analysis was also used to identify the key DEGs that dramatically contribute to the distinction of ECP-treated and untreated CAR-T cells. Incorporating these 4 different algorithms, finally, 9 downregulated hub genes by ECP were identified in our study (Figure 7J).
Single sample gene set enrichment analysis was conducted to calculate the score for the enrichment of a set of genes in the different immune cell types. It revealed that genes in CAR-T cells without ECP treatment were enriched in activated CD8+T cells and CD8+TEM cells, whereas in genes in ECP-treated CAR-T cells were enriched in activated CD4+T cells and Th2 cells (Figure 7K).
Furthermore, an unbiased comparison of ECP-treated vs untreated CAR-T cells was also conducted to identify pathways that might contribute to the ECP effect. Gene set enrichment analysis identified numerous gene sets enriched in ECP-treated CAR-T cells that are associated with apoptosis and immune regulation pathways (Figure 7L).
Discussion
Allo-HSCT represents a curative treatment for the majority of hematological malignancies. Despite advances in allo-HSCT, posttransplant relapse and GVHD continue to be major causes of treatment failure, ultimately resulting in poor outcomes for patients.16,17 CAR-T cells with a strong ability to clear tumor cells represent a promising therapeutic option for posttransplant relapse. However, donor- or recipient–derived CAR-T cells carry the risk of exacerbating preexisting GVHD or causing a de novo GVHD.4 Therefore, it is of importance to prevent or treat GVHD without compromising the desired antitumor effect of CAR-T cells.
In this study, 2 different models were established, the nondilution and the dilution model, to mimic the clinical settings based on the kinetics of CAR-T cells after infusion. The nondilution model was used to simulate the days immediately after CAR T-cell infusion, whereas the dilution model was used to simulate weeks after infusion. The impact of ECP on GVHD was assessed through an in vitro MLR assay. We found that (1) ECP-treated CAR-T cells exhibited reduced potency in inducing alloreactivity compared with the group without ECP treatment in MLR assay; (2) the selective apoptotic effect of ECP could enrich the naive and central memory CAR-T cells exhibiting less alloreactivity; (3) the cytokine profile of CAR-T cells was switched from immune stimulation to immune tolerance through ECP therapy in both models; and (4) the proliferative capacity of CAR-T cells was modulated by ECP without hampering their long-term functionality in the dilution model.
It is well known that ECP therapy induces apoptosis in response to DNA damage caused by cross-linking of pyrimidine bases.15 Subsequently, transcriptional, posttranscriptional, and translational systems react correspondingly, resulting in relevant changes in protein and metabolic levels. A total of 372 DEGs detected in ECP-treated CAR-T cells were enriched in the processes and pathways related to apoptosis such as the p53 signaling pathway, ribosome biogenesis, and forkhead box O (FoxO) signaling pathway. Of note, the identified hub genes, transducin beta-like 3 (TBL3), tryptophan-aspartic acid (WD) repeat family (WDR3, WDR12, and WDR43), ribosomal L1 domain containing 1 (RSL1D1), and ribosomal RNA processing 1B (RRP1B) genes, were also majorly involved in the regulation of apoptosis.
The signal of ECP-caused DNA damage could be directly transmitted to the p53 protein or indirectly activate p53 through an impairment of ribosome biogenesis, thereby triggering further the activation of the intrinsic apoptosis pathway.18-20 Additionally, in line with the previous study,21 an upregulation of death ligand CD95, Fas, was found in ECP-treated CAR-T cells, indicating that the extrinsic apoptosis pathway via Fas/FasL can be upregulated by ECP as well. Alterations in noncoding RNAs by ECP might be responsible for the modulation of the expression of membrane death receptors affecting the extrinsic apoptosis pathway.22
Both intrinsic and extrinsic apoptosis could give rise to the reorganization of the cytoskeleton proteins, thereby disrupting the membrane dynamics.23 This was confirmed by our finding that the TBL3 gene, which is highly involved in the organization of the cytoskeleton, cell wall, and membrane, was downregulated by ECP. Consequently, the asymmetric distribution of phosphatidylserine (PtdSer), a phospholipid of the plasma membrane, could be disrupted, leading to an exposure of PtdSer on the cell surface. This exposure could be detected by Apotracker, showing a high proportion of Apotracker+CAR-T cells after ECP therapy. Apart from PtdSer, the reorganization of cytoskeleton proteins might contribute to the elevated expression of the CAR receptor including CD19 CAR and 4-1BB after ECP treatment in our study as well.
Indeed, apoptosis could cause direct cell loss contributing to an amelioration of GVHD. It is of note that TE and TEM cells were more vulnerable to ECP treatment, leading to an enrichment of TN and TCM cells, which was confirmed by our phenotypic analysis. CD27 is upregulated during T-cell activation, which might lead to an excessive activation of lymphocytes.24 It is interesting to note that CD27+TCM cells exhibited high expression of the death ligand CD95, suggesting that ECP could selectively modulate these activated T cells and further shape the TCM cells to a less active potency. In line with these results, the selective effect of ECP is supported by our single sample gene set enrichment analysis, showing a decrease of activated and effector memory CD8+T cells but an increase of activated CD4+T cells and Th2 cells. These findings were supported by other studies that suggest ECP selectively influences alloreactive T cells in GVHD and autoreactive T cells in autoimmune diseases. Nevertheless, further research is required to identify how ECP achieves this selectivity without causing systemic immunosuppression.25
Selective apoptosis enriches cell populations with less ability to provoke alloreaction, possibly explaining why ECP-treated CAR-T cells have a lower potency to induce the activation and proliferation of allogeneic T cells in the MLR assay. Similar results were reported by other groups, demonstrating that the composition of T-cell subsets may affect the potential for GVHD.26-28
In addition to the impact of ECP on quantity and composition of CAR-T cells, ECP-induced apoptosis could alter the cytokine secretion of treated CAR-T cells and untreated bystander cells, thereby inducing immune tolerance and mitigating GVHD. When analyzing the supernatant from apoptotic CAR-T cells alone, we observed an increase of TGF-β consistent with a previous study.29 TGF-β is known to play an important role in the maintenance of peripheral tolerance by inhibition of Th1 and cytotoxic T-cell responses, as well as induction of regulatory T cells (Tregs).30 In combination with a low concentration of IL-2 that was also seen in our results, TGF-β could promote the conversion of CD4+TN cells into Tregs by triggering expression of Foxp3. This is supported by the study of Kleinclauss et al, in which intravenous infusion of apoptotic splenic cells induced Treg generation in a TGF-β dependent manner. In turn, it facilitated allogeneic bone marrow engraftment and delayed the onset of GVHD.31 Importantly, not only TGF-β signaling pathway, but also FoxO, a potent transcription factor for TGF-β induced Tregs (iTregs), was enriched in CAR-T cells after ECP treatment, which supports TGF-β to exert its beneficial anti-inflammatory effect.32
Next to iTregs induced peripherally, Tregs could be also generated centrally in the thymus, namely natural Treg cells. Both subtypes of Tregs are characterized by the expression of the high-affinity IL-2 receptor, IL-2Rα, enabling them to respond to low concentrations of IL-2. By contrast, conventional T cells express IL-2 receptors, IL-2Rβ or IL-2Rγ, with a low-intermediate affinity and require supraphysiologic concentrations of IL-2 for the activation.33 IL-2 concentration in ECP-treated cells steadily increased, reaching a peak of 1 ng/mL, reported as the optimal concentration for Treg generation.34 This might explain the observation in our previous study and also in other findings that Tregs in the circulation of patients with GVHD increased under ECP therapy.15,35
However, induction and maintenance of immune tolerance by Tregs require expression of CD69. These CD69+Tregs express high levels of suppression-associated markers, such as CTLA-4 and ICOS, secrete high amounts of TGF-β and have potent immune suppressive activity.36 The role of CD69 in the development of immune responses is highly regulated by metabolism and cytokines. Amino acid starvation together with TGF-β and IL-2 might favor the development of Tregs.37 In fact, we observed that ECP-treated CAR-T cells have an increased CD69 expression with changes in different metabolism pathways. Together, these actions provide strong evidence that ECP therapy displays an immunomodulatory effect and support the clinical use of ECP to treat patients with GVHD.
However, crucial concern was raised about whether ECP therapy impacts the antitumor activity of CAR-T cells. Although results from our previous studies showed that ECP therapy does not hamper the antiviral and antileukemic effects of immune cells,12,15 we still comprehensively investigated the short- and long-term effects of ECP on CAR-T cells. An inferior killing efficiency of ECP-treated CAR-T cells has been observed in our nondilution model. In addition, the repetitive tumor killing potential of CAR-T cells was impaired by ECP treatment in the nondilution model as well. These adverse effects of ECP might be explained by the direct induction of apoptosis and the modulation of CAR T-cell proliferation, as observed in our study.
Surprisingly, PBMCs could not only rescue CAR-T cells from apoptosis, but also maintain their functionalities under ECP treatment. The short-term killing capacity and the cytokine production of ECP-treated CAR-T cells were sustained in the dilution model. Interestingly, their functions were not hampered when compared with those in the nondilution model. An explanation for this discrepancy between the nondilution and dilution model could be the additional PBMCs in the dilution model and the different absorption abilities of immune cells for 8-MOP.
Of note, the long-term functionality of CAR-T cells in terms of multiple rounds of killing, was not compromised by ECP therapy in the dilution model, except the proliferative capacity. CD71, which negatively reflects the proliferation, was increased along with a decrease of proliferation and division indices. In addition, our transcriptional data are also suggestive for the modulatory effect of ECP on the proliferation. The genes (TBL3, GTPBP4, WDR3, NHP2, and RRP1B) as well as the pathways (p53 and FoxO) related to proliferation were modulated by ECP treatment. Apart from cell cycle arrest by ECP demonstrated by our RNA-seq data, the change of the signal 2 (costimulation) from immune activation to immune suppression, evidenced by a decrease of CD40L coupled with an increase of CTLA-4, a negative costimulatory marker, may be partly responsible for the moderate proliferation of ECP-treated CAR-T cells.
A close correlation between CAR T-cell expansion and clinical response has been reported 38 indicating an essential role of CAR T-cell expansion for their in vivo activities in patients. However, an excessive expansion of CAR-T cells could lead to severe side effects.39 Moreover, a recent study demonstrated that a decrease in cell proliferation could improve the effectiveness of engineered CAR-T cells and T-cell receptor via reducing the terminal differentiation.40 In line with this study, our data showed an increase in long-living TN and TCM CAR-T cells with a decrease of terminal differentiated TE cells after ECP treatment. The high proportion of TN and TCM cells retains the potential to proliferate and differentiate into effector cells under chronic tumor stimulation, as evidenced by our challenging assays. The long-term killing functions of CAR-T cells were not hampered by ECP therapy.
Our study has certain limitations that should be acknowledged. First, the experiments were conducted using samples from healthy donors rather than actual patient samples. This aspect may introduce potential variations in the results when extrapolating to clinical settings. To address this limitation, further investigations should be carried out using patient samples to better replicate real-world conditions. Additionally, the dilution ratio of CAR-T cells with PBMC utilized in our study was consistent, but it is important to note that clinical practice may involve different dilution ratios. Therefore, future studies should explore various dilution ratios of CAR-T cells with PBMC to provide a more accurate representation of clinical scenarios. Furthermore, to enhance our understanding of the interaction between ECP and CAR-T cells, as well as its impact on the development and progression of GVHD, it is imperative to conduct further research on the underlying mechanisms. This additional investigation will contribute to a better understanding of the complex dynamics between ECP and CAR-T cells, thereby facilitating the optimization of treatment strategies and elucidation of the pathogenesis of GVHD.
In conclusion, ECP represents a promising approach to treat GVHD in the setting of posttransplant CAR T-cell therapy and has significant potential for clinical utilization. Nevertheless, caution is warranted regarding the use of ECP within the initial 60 days following CAR T-cell infusion due to the elevated proportion of CAR-T cells present in the peripheral blood and their potential susceptibility to inhibition the by ECP therapy. Moreover, to facilitate the translation of these encouraging preclinical findings into clinical practice, it is imperative to conduct further trials.
Acknowledgment
This study was financially supported by Mallinckrodt Pharmaceuticals through an external collaborative research grant. The funding source did not play a role for the study design, collection, analysis, and interpretation.
Authorship
Contribution: L.W. and A.S. designed and coordinated the study; H.H. performed all experiments and processed the data; A.S., M.S., M.-L.S., T.S., and C.M.-T. treated the patients; A.S., B.N., and A.H.-K. provided clinical information; H.H. and Y.D. analyzed the data; L.W., A.S., M.S., H.H., B.N., M.L., H.Y., Q.C., T.S., M.-L.S., Z.G., and C.M.-T. discussed structure of the manuscript; H.H., L.W., and A.S. wrote the manuscript; A.S., M.S., and C.M.-T. edited the manuscript; and all authors critically reviewed the manuscript.
Conflict-of-interest disclosure: M.S. received funding for collaborative research from Apogenix, Hexal, and Novartis; travel grants from Hexal and Kite; and financial support for educational activities and conferences from bluebird bio, Kite, and Novartis. M.S. is a board member for Merck Sharp & Dohme (MSD) and (co-)principal investigator of clinical trials of MSD, GlaxoSmithKline (GSK), Kite, and Bristol Myers Squibb (BMS). A.S. received travel grants from Hexal and Jazz Pharmaceuticals. M.S. and A.S. are cofounders and shareholders of TolerogenixX Ltd. A.S. is a part-time employee of TolerogenixX Ltd. The remaining authors declare no competing financial interests.
Correspondence: Anita Schmitt, University Clinic Heidelberg, Im Neuenheimer Feld 410, Heidelberg 69120, Germany; email: anita.schmitt@med.uni-heidelberg.de; and Lei Wang, University Clinic Heidelberg, Heidelberg, Im Neuenheimer Feld 410, Heidelberg 69120, Germany; email: xjwl8587@gmail.com.
References
Author notes
H.H. and L.W. contributed equally to this study.
Data sets related to this study are available from the corresponding authors, Anita Schmitt (anita.schmitt@med.uni-heidelberg.de) and Lei Wang (xjwl8587@gmail.com).
The full-text version of this article contains a data supplement.

![Effect of ECP therapy on viability, short-term cytotoxicity, component, and cytokine-producing capacity of CAR-T cells in 2 different in vitro models. (A) Proportion of CAR-T cells in the peripheral blood of patients after CAR T-cell therapy (n = 4). (B) Schematic diagram of in vitro dilution CAR T-cell therapy models. (C) Cell loss between the ND and the D models in different dilution ratios. Cell loss was calculated by the following formula: (the absolute number of CAR-T cells without ECP therapy cultured 24 hours) – (the absolute number of CAR-T cells with ECP therapy cultured 24 hours). (D) Representative dot plots of apoptotic CAR-T cells in different dilution ECP therapy models. Apoptotic cells were defined as Apotracker+ cells. (E) Viability of CAR-T cells shown for the ND and the D models in different dilution ratios. Nonliving cells were defined as Apotracker+cells and 7AAD+cells. (F) Representative dot plots of specific killing efficiency of CAR-T cells and unspecific killing capacity of PBMCs with or without ECP in a ratio of 1:1 to Raji tumor cells. (G) Summarized killing efficiency of CAR-T cells with or without ECP therapy in the ND and the D models. The killing efficiency was calculated by the following formula: ([initial number of tumor cells – residual number of tumor cells] × 100)/(initial number of tumor cells). (H) Absolute residual number of tumor cells after 24 hour coculture with ECP-treated CAR-T cells or ECP-treated PBMCs in the ND and the D models. (I) Contribution of unspecific killing capacity of PBMCs in the dilution model. The killing contribution of PBMCs was estimated by using the identical D model without CAR-T cells. (J) Component of CAR-T cells with respect to CD4/CD8 ratio before and after ECP treatment in the ND and the D models. (K) Influence of ECP treatment on TNF-α, IFN-γ, and multifunctional (TNF-α+IFN-γ+) cytokine production of CAR-T cells was determined after 4 hour tumor cell stimulation in an effector/tumor (E/T) ratio of 1:1 by an intracellular cytokine staining. A 2-tailed t test was performed for statistical analysis. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. ND, nondilution; D, dilution](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/8/11/10.1182_bloodadvances.2023012463/2/m_blooda_adv-2023-012463-gr1.jpeg?Expires=1769091936&Signature=FwbfLgwdpJ~SO3A-Z1C8DIK9kVV6WY6bgnz~y98DeRa8fD-Q3knT3tN1t45m2ySsiatvYkVsQfDa7etGpY0lOJTKLzGEopXMd6v5QaH9elKjPHYVi3bS10KCosdWloqXjfaFXzSY5tqCBPeQFZPOvGs3eoC0MpWuMQMRCK13o5wxldqOmQ5irbSlx5tErUio888CEhf6LiRABtf1Qhma~BTcDiIBO-~WRqzPmJm6VFCm2k3~DqdLtySCSc7~VaNcm28qS~0X19kBmMjqRuZhzLgtKVqr5ELWMneJwi0aqqMMMfQ4s4-c0-d-QG7VfDsBiuOcxF6VPG7NpEaRrc0f~A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)