Key Points
CPX induced MRD negativity contributing to the improvement of OS.
The improved OS with CPX-351 was confirmed in the real-life setting with a long follow-up.
Visual Abstract
CPX-351 has been approved for patients with therapy-related acute myeloid leukemia (t-AML) or AML with myelodysplasia-related changes (MRC-AML). No extensive data are available on measurable residual disease (MRD) and long-term clinical outcome using CPX-351 in AML in real life. We retrospectively collected data from 168 patients in 36 centers in France and Italy who had received 1 or 2 cycles of induction with CPX-351. All patients were aged >18 years and had newly diagnosed, untreated t-AML or MRC-AML. With a median follow-up of 3 years, the median overall survival (OS) was 13.3 months. The median OS was 20.4 months vs 12.9 months for patients with MRD below or above 10–3, respectively (P = .006). In a multivariate analysis, only MRD >10–3 was associated with a poorer OS (hazard ratio, 2.6; 95% confidence interval, 1.2-5.5; P = .013). We also observed a trend toward a better median OS in patients who underwent hematopoietic stem cell transplantation with MRD <10–3 (not reached vs 26.0 months; P = .06). Achievement of MRD negativity contributed to the improvement of OS in the overall population and, maybe, in patients receiving transplant. These data provide the rationale for the 2 ongoing studies evaluating CPX-351 vs 7+3 in non–MRC-AML and non–t-AML using MRD as the primary end point for ALFA-2101 phase 2 clinical trial and event-free survival for AMLSG 30-18 phase 3 clinical trial.
Introduction
CPX-351 is a liposomal formulation of cytarabine and daunorubicin packaged at a 5:1 molar ratio. CPX-351 has been approved by the US Food and Drug Administration (FDA) and European Medicines Agency (EMEA) for patients with therapy-related acute myeloid leukemia (t-AML) or AML with myelodysplasia-related changes (MRC-AML) according to the World Health Organization (WHO) 2016 AML classification. Although WHO updated the AML classification in 2022, and t-AML and MRC-AML are no longer considered separate entities,1 the European LeukemiaNet (ELN) still recommends CPX-351 for such patients.2 Real-world experience (RWE) from several countries (France, Italy, Germany, Spain, and the United States) showed similar or better results compared with the phase 3 registrative trial, which showed the superiority of CPX-351 over conventional “3+7” chemotherapy.3-9 However, the median follow-up of RWE studies was rather short. More recently, Lancet et al published the long-term update of the phase 3 clinical trial and confirmed the higher remission and improved overall survival (OS) compared with “3+7.”10 Specifically, the overall response rate (ORR) was 47.7% with CPX-351% and 33.3% with 7+3. After 5 years of follow-up, the median OS was 9.33 months with CPX-351 and 5.95 months with 7+3. Five-year OS was 18% in the CPX-351 group and 8% in the 7+3 group. These results were significantly improved in patients undergoing allogeneic stem cell transplantation (HCT) in complete remission (CR).9,10 Assessment of measurable residual disease (MRD) identifies small numbers of AML cells surviving chemotherapy being responsible for disease relapse.11,12 The achievement of MRD-negative CR typically predicts better outcomes for patients with AML. Moreover, patients with high-risk AML benefit from HCT, especially if transplantation is performed in MRD-negative CR.13-19 No extensive data are available on MRD and long-term clinical outcome using CPX-351 in AML.
Thus, the primary objective of this study was to analyze the efficacy of CPX-351 in a real-life setting with long follow-up, evaluating the impact of MRD in responding patients.
Methods
Patients and treatment
We retrospectively collected data from patients with AML in 36 centers in France and Italy who had received 1 or 2 cycles of induction with CPX-351 as first-line therapy. All patients were aged >18 years old and had newly diagnosed, untreated t-AML or MRC-AML.
Study oversight
In France, all actions were performed according to MR004 of the Commission Nationale de l'Informatique et des Libertés for France, and all products were used after EMEA approval. Every patient received an information sheet and provided oral informed consent. CHU Nice registered this study in Institute National des Données de Santé under the reference number MR4809140819. In Italy, patients were treated in a named patient program (compassionate use); all patients signed written informed consent, and local ethic committee (EC) approved the treatment for each patient. The study was conducted in accordance with the Declaration of Helsinki.
Baseline and on-study assessments
Clinical, biological and treatment information were available for all patients (Table 1). Mutation screening was performed on 92 patients (55%) at baseline using next-generation sequencing (NGS; ≥19 genes). The prognostic factors of patients were evaluated at diagnosis using 2017 and 2022 ELN genetic risk stratification.2,20
Patient characteristics
| . | N = 170 . | % or range . |
|---|---|---|
| Age, y | ||
| Median | 66 | 20-83 |
| 18-60 | 33 | 19 |
| >60 | 137 | 81 |
| Sex | ||
| Male | 80 | 47 |
| Female | 90 | 53 |
| AML subtype | ||
| MRC-AML | 117 | 69 |
| t-AML | 48 | 28 |
| Others∗ | 5 | 3 |
| Median no. of WBC, G/L | 3 | 0-213 |
| Hyperleukocytosis | 16 | 9 |
| Karyotype | ||
| Complex | 51 | 30 |
| Monosomal | 32 | 19 |
| 2017 ELN genetic risk stratification | ||
| Favorable | 8 | 5 |
| Intermediate | 61 | 36 |
| Adverse | 98 | 58 |
| 2022 ELN genetic risk stratification | ||
| Favorable | 8 | 5 |
| Intermediate | 16 | 9 |
| Adverse | 143 | 84 |
| Lindsley classifier (N = 107) | ||
| de novo/pan-AML | 30 | 28 |
| Secondary-type mutations AML | 42 | 39 |
| TP53-mutated AML | 35 | 33 |
| . | N = 170 . | % or range . |
|---|---|---|
| Age, y | ||
| Median | 66 | 20-83 |
| 18-60 | 33 | 19 |
| >60 | 137 | 81 |
| Sex | ||
| Male | 80 | 47 |
| Female | 90 | 53 |
| AML subtype | ||
| MRC-AML | 117 | 69 |
| t-AML | 48 | 28 |
| Others∗ | 5 | 3 |
| Median no. of WBC, G/L | 3 | 0-213 |
| Hyperleukocytosis | 16 | 9 |
| Karyotype | ||
| Complex | 51 | 30 |
| Monosomal | 32 | 19 |
| 2017 ELN genetic risk stratification | ||
| Favorable | 8 | 5 |
| Intermediate | 61 | 36 |
| Adverse | 98 | 58 |
| 2022 ELN genetic risk stratification | ||
| Favorable | 8 | 5 |
| Intermediate | 16 | 9 |
| Adverse | 143 | 84 |
| Lindsley classifier (N = 107) | ||
| de novo/pan-AML | 30 | 28 |
| Secondary-type mutations AML | 42 | 39 |
| TP53-mutated AML | 35 | 33 |
WBC, white blood cell.
Lindsley classifier was used and classified patients as secondary-type mutations (defined by the presence of a mutation in SRSF2, SF3B1, U2AF1, ZRSR2, ASXL1, EZH2, BCOR, and/or STAG2), TP53 mutated, and de novo/pan AML.21
The ORR was defined by CR and CR with incomplete hematological recovery (CRi) using the international working group (IWG) 2003 criteria.22 Among the patients in CR or CRi, 62 (61%) were evaluated for MRD. In accordance with the standard MRD methodology used at site, MRD was assessed by Leukaemia-associated immunophenontypes (LAIP) flow cytometry (n = 43), NGS (n = 8), or real-time quantitative polymerase chain reaction (n = 11 [NPM1]) in patients with documentation of specific genetic alterations such as NPM1 mutation, as previously reported.11 All patients with MRD <10–3 were considered as negative. Patients were considered to be in relapse if bone marrow blasts were ≥5%, blasts reappeared in the blood, or if they developed extramedullary disease after CR/CRi.
Statistical analysis
Continuous variables are described using medians (interquartile ranges; [minimum; maximum]), and qualitative variables are described using counts and percentages. Noncontinuous variables were compared using χ2 test. Mann-Whitney and Kruskal-Wallis tests were used for continuous variables. Adverse events were evaluated according to Common Terminology Criteria for Adverse Events (CTCAE) classification. The median follow-up time was calculated as the median time from the initiation of treatment to the last follow-up. OS was calculated from the date of AML diagnosis to the date of death or last follow-up. Survival curves were estimated using the Kaplan-Meier method and were compared with the log-rank test.
Univariate and multivariate analyses were performed using Cox model. Variables significantly associated with better OS in univariate analysis were considered as covariates in multivariate analysis. Statistical tests were considered significant when the 2-tailed P value was <.05. Confidence intervals were computed with 95% coverage. All statistical analysis was performed using SPSS v.22 software (IBM SPSS Statistics).
Results
Characteristics of the study population
Between April 2018 and October 2019, a total of 168 patients treated with CPX-351 were included in this study. The male-to-female sex ratio was 80/90, and the median age was 66 years (range, 20-83). AML subtypes were MRC-AML in 121 (72%) and t-AML in 47 patients (28%). All patient’s clinical characteristics are described in Table 1.
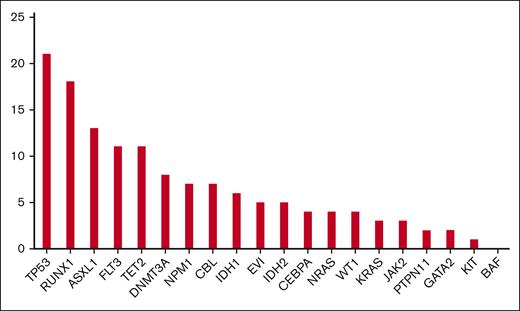
According to the ELN 2017 classification, genetic risk was favorable, intermediate, and adverse in 8 (5%), 61 (36%), and 98 patients (58%; missing for 3 patients), respectively. According to the ELN 2022 classification, genetic risk was favorable, intermediate, and adverse in 8 (5%), 16 (9%), and 143 (84%), respectively. Thirty percent and 19% of patients had complex and monosomal karyotypes, respectively. Assessed by NGS, the most frequent mutated genes were TP53 (n = 35 [21%]), RUNX1 (n = 30 [18%]), ASXL1 (n = 22 [13%]), FLT3 (n = 20 [12%]), TET2 (n = 18 [11%]), and NPM1 (n = 12 [7%]) among the 92 patients for whom NGS was available (Figure 1). According to a Lindsley classifier21 (evaluable in only 107 patients), 28 %, 39%, and 33% had de novo/pan-AML, secondary-type mutation AML, and TP53-mutated AML, respectively.
Response
The ORR was 102 of 170 (60%) after 1 (n = 91) or 2 inductions (n = 11), including 53% CR and 6% CRi. Among the 102 CR/CRi patients, 62 (61%) were evaluable for MRD after induction or first consolidation. Forty patients (65%) had MRD below the threshold of 10–3. ELN 2017 and ELN 2022 were identified as factors predicting CR/CRi rate (P = .032 and .043, respectively), but the Lindsley classifier did not predict response (P = .060). Based on ELN 2022 risk categories, favorable patients (n = 6) had a median OS of not reached vs 14.9 months (P = .45), intermediate patients (n = 6) had all negative MRD, with a median OS of 11.7 months, and adverse patients (n = 50) had a median OS of 40.9 vs 10.6 months (P = .018) in negative vs positive MRD, respectively. Based on ELN 2017 risk categories, favorable patients (n = 6) had a median OS of not reached vs 14.9 months (P = .45); intermediate patients (n = 16) had a median OS of 20.4 vs 10.5 months (P = .71); and adverse patients (n = 40) had a median OS 18.8 vs 12.9 months (P = .038) in negative vs positive MRD, respectively. In TP53-mutated patients (n = 15), we observed a median OS of 15.1 vs 10.3 months (P = .23) in negative vs positive MRD, respectively.
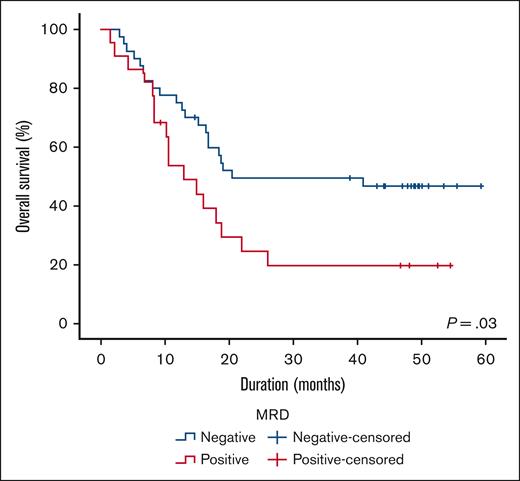
OS
With a median follow-up of 3 years, the median OS was 13.34 months for the whole population (range, 9.35-17.33). Notably, the median OS was 20.4 months vs 12.9 months for patients with MRD below or above 10–3, respectively (P = .03; Figure 2). In a univariate analysis, only MRD >10–3 (P = .031), ELN 2017 classification (P = .027), and the presence of TP53 mutation (P = .017), but not ELN 2022 or the Lindsley classifier, were associated with a significantly shorter median OS. In a multivariate analysis, only MRD >10–3 was associated with a shorter OS (hazard ratio [HR], 2.6; 95% confidence interval, 1.2-5.5; P = .013; Table 2).
Univariate and multivariate analyses to predict better OS
| . | Univariate analysis . | Multivariate analysis . |
|---|---|---|
| ELN2017 | P = .027 | ns |
| ELN2022 | ns | ∗ |
| Lindsley Classifier | ns | ∗ |
| TP53 mutation | P = .017 | ns |
| MRD status | P = .031 | P = .013 |
| . | Univariate analysis . | Multivariate analysis . |
|---|---|---|
| ELN2017 | P = .027 | ns |
| ELN2022 | ns | ∗ |
| Lindsley Classifier | ns | ∗ |
| TP53 mutation | P = .017 | ns |
| MRD status | P = .031 | P = .013 |
ns, not significant.
Allogeneic stem cell transplantation
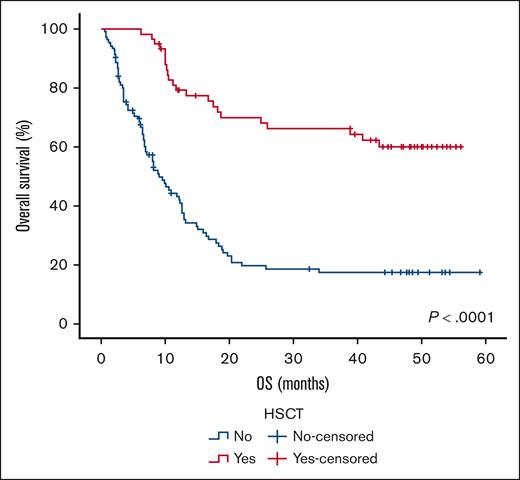
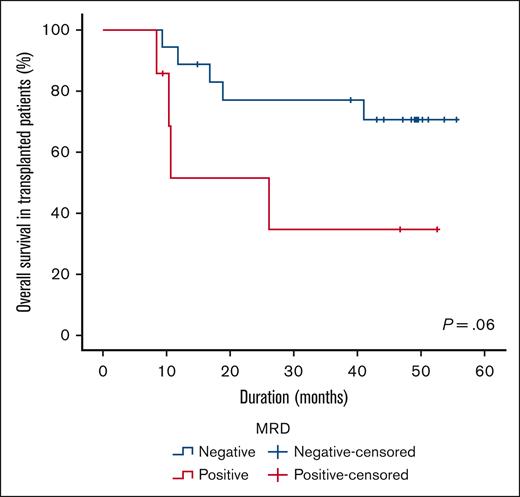
Sixty patients (35%) underwent HSCT in first CR. The demographic and clinical characteristics of the patients undergoing HSCT are listed in Table 3. With a median follow-up of 3.5 years, we confirmed an improvement of median OS between patients who received transplant compared with patients who did not (not reached vs 9.1 months; P < .0001; Figure 3). The median time between MRD evaluation (after induction) and HSCT was 3.2 months (range, 0.6-10.0). The median CPX-351 consolidation cycle received before HSCT was 1 (range, 0-2). There was no significant difference in OS based on the number of consolidation cycles received (P = .8; data not shown). Despite the low number of patients receiving transplant with positive MRD (n = 7), we also observed a trend toward a better median OS in patients receiving allograft in MRD-negative CR (not reached vs 26.0 months; P = .06; Figure 4). For patients not receiving transplant with MRD evaluation available (n = 37), we did not observe significant difference in terms of OS in negative vs positive MRD patients (15.1 vs 12.9 months; P = .38).
Characteristics of HSCT
| . | N = 60 . | % or range . |
|---|---|---|
| Age, median, y | 64 | 20-75 |
| Sex | ||
| Male | 31 | 52 |
| Female | 29 | 48 |
| AML subtype | ||
| MRC-AML | 41 | 68 |
| t-AML | 18 | 30 |
| Others | 1 | 2 |
| Disease status at time of HCT | ||
| CR | 53 | 88 |
| CRi | 1 | 2 |
| PR | 3 | 5 |
| Refractory | 3 | 5 |
| MRD status after CPX-351 induction | ||
| Negative | 18 | 30 |
| Positive | 7 | 12 |
| NA | 35 | - |
| Conditioning regimen | ||
| RIC | 41 | 68 |
| MAC | 16 | 27 |
| Donor | ||
| Matched related donor | 22 | 37 |
| Matched unrelated donor | 16 | 27 |
| Mismatched donor | 5 | 8 |
| Haploidentical donor | 17 | 28 |
| Stem cell source | ||
| Bone marrow | 6 | 10 |
| Peripheral blood | 49 | 82 |
| . | N = 60 . | % or range . |
|---|---|---|
| Age, median, y | 64 | 20-75 |
| Sex | ||
| Male | 31 | 52 |
| Female | 29 | 48 |
| AML subtype | ||
| MRC-AML | 41 | 68 |
| t-AML | 18 | 30 |
| Others | 1 | 2 |
| Disease status at time of HCT | ||
| CR | 53 | 88 |
| CRi | 1 | 2 |
| PR | 3 | 5 |
| Refractory | 3 | 5 |
| MRD status after CPX-351 induction | ||
| Negative | 18 | 30 |
| Positive | 7 | 12 |
| NA | 35 | - |
| Conditioning regimen | ||
| RIC | 41 | 68 |
| MAC | 16 | 27 |
| Donor | ||
| Matched related donor | 22 | 37 |
| Matched unrelated donor | 16 | 27 |
| Mismatched donor | 5 | 8 |
| Haploidentical donor | 17 | 28 |
| Stem cell source | ||
| Bone marrow | 6 | 10 |
| Peripheral blood | 49 | 82 |
MAC, myeloablative conditioning; NA, not available; RIC, reduced-intensity conditioning.
Discussion
New therapies were approved for the treatment of AML in recent years. Several of these may induce deeper responses, leading to an interest in assessing and using MRD as a surrogate marker for OS and improving the management of patients with AML. Indeed, several studies have since demonstrated the predictive value of MRD assessment in patients with AML.11,12,23 A meta-analysis of 81 studies reported 11 151 patients with AML with MRD-negative CR and showed an improvement of 5-year OS (68% vs 34%) and 5-year disease-free survival (64% vs 25%) compared with patients with AML with MRD-positive CR.24 Some studies also showed in MRD-positive CR after induction in adult and pediatric patients with AML worse outcomes after HCT than patients with AML with negative MRD. A meta-analysis of 19 studies in 1431 patients identified that MRD positivity before HCT was correlated with decreased leukemia-free survival (HR, 2.76), OS (HR, 2.36), and cumulative incidence of relapse (HR, 3.65).19
CPX-351 is a liposomal formulation of cytarabine and daunorubicin packaged at a 5:1 molar ratio. This drug has been approved by the FDA and EMEA for patients with t-AML or MRC-AML according to the WHO 2016 AML classification. Long-term follow-up of patients with AML included in the phase 3 registrative trial showed 18% long-term survivors after 5 years. However, in phase 3 clinical trial, MRD was not assessed. Nevertheless, some MRD data were reported in subsequent RWE retrospective studies using CPX-351, which suggested that CPX-351 could induce deeper response than classical “3+7.”
In the CPX-351 Italian compassionate use program in older adults with newly diagnosed t-AML or AML-MRC,4 MRD negativity was observed in 38% and 54% of patients using MFC (n = 40) and WT1 quantitative polymerase chain reaction (n = 38) methods, respectively. There was a trend showing that MRD negativity improved 12-month cumulative incidence of relapse (11% vs 37% for MRD-negative and MRD-positive patients, respectively; P = .151). Nevertheless, nonsignificant difference was observed for 12-month OS (71% vs 84% for MRD-negative vs MRD-positive, respectively; P = .414). In a French retrospective, multicenter analysis in patients with newly diagnosed t-AML or AML-MRC,3 16 patients (57%) achieved MRD negativity (defined as <10–3), including 8 of 14 patients (57%) who had available MRD data and proceeded to HCT; so far, OS among patients receiving transplant was not significantly different between patients with vs without MRD negativity. In a German retrospective, multicenter analysis in patients with newly diagnosed t-AML or AML-MRC,6 23 of 36 patients (64%) achieved MRD negativity (defined as <10–3); furthermore, all 23 patients proceeded to HSCT and continued to exhibit MRD negativity at the time of HSCT. The achievement of MRD negativity was associated with longer OS overall (P = .01) and among patients who proceeded to HSCT (P = .02) but not in a multivariable analysis for OS. Overall, real-world studies found no consistent difference in OS among patients with or without MRD negativity. However, it should be noted that their median follow-up times were relatively short (8.6-11 months). The data presented in this manuscript, with a longer follow-up, confirmed a high level of negative MRD after induction (64%). Negative MRD CR resulted in a median OS of 20.4 months vs 12.9 months (P = .006) in the whole cohort. The high incidence of MRD negativity may explain the benefit of CPX-351 over conventional treatment, which in the phase 3 trial was even more evident among patients who received allotransplant, because many studies confirmed the predictive role of residual MRD before transplantation.13-19 In this view, in our study, MRD negativity before transplantation showed a trend toward a longer survival (median OS, not reached vs 26 months, in patients with negative or positive pre-HSCT MRD, respectively; P = .06), albeit without reaching statistical significance, probably because of the low number of MRD-positive patients receiving HSCT. The absence of TP53 adverse prognosis in our cohort needs to be confirmed related to some of the limitations of our study: retrospective nature, small number of mutated patients, and unknown monoallelic or biallelic status.
Conclusion
After 3 years of follow-up, the improved OS with CPX-351 was confirmed in the real-life setting. Achievement of MRD negativity contributed to the improvement of OS in the overall population and, maybe, in patients who received transplant. These data provide the rationale for the 2 ongoing studies evaluating CPX-351 vs 7+3 in non–MRC-AML and non–t-AML, using MRD as the primary end point for ALFA-2101 phase 2 clinical trial (www.clinicaltrials.gov identifier NCT05260528) and event-free survival for AMLSG 30-18 phase 3 clinical trial (www.clinicaltrials.gov identifier NCT05260528).
Authorship
Contribution: T.C., E.C., F.G., and R.M.L collected data; T.C., F.G., E.C., P.M., R.R., S.B., L.F., J.-B.M., M.G., P.P., S.G., X.T., G.R., O.L., M.R., E.R., G.B., A.C., M.D., C.B., A.B., C.L., B.S., A.P., P.Z., C.R., F.G., L.A., and R.M.L. edited the manuscript; T.C. and R.M.L designed the study; and T.C., F.G., and R.M.L wrote the manuscript.
Conflict-of-interest disclosure: T.C., R.M.L., and L.A. declare consultancy and speaker bureau fees from Jazz Pharmaceuticals. The remaining authors declare no competing financial interests.
Correspondence: Thomas Cluzeau, Hematology Department, Nice University Hospital, 151 route Saint Antoine de Ginestière, 06200 Nice, France; email: cluzeau.t@chu-nice.fr.