The Case
Clinical Presentation
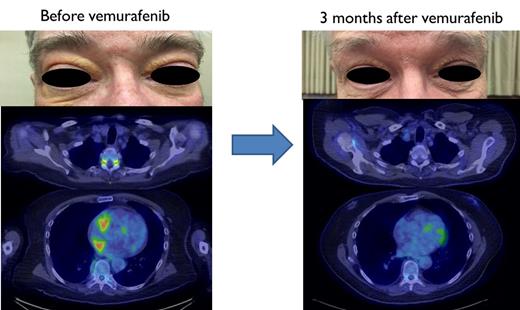
A 65-year-old man presented to his local ophthalmology clinic for one-month history of progressively worsening redness of the eyes and double vision. Physical examination revealed periorbital xathelasmas and exophthalmos, and radiographic studies demonstrated bilateral orbital masses (Figure). He underwent left anterior orbitotomy that revealed xanthogranulomatous inflammation. Due to progression of symptoms in the right eye, a right anterior orbitotomy was performed, with a histopathologic diagnosis of xanthogranuloma again. The patient was treated with prednisone to help with the inflammation, without any improvement in symptoms.
Photos showing manifestations of BRAF-V600E Erdheim-Chester disease in patient before and after treatment
Photos showing manifestations of BRAF-V600E Erdheim-Chester disease in patient before and after treatment
Diagnosis and Staging
Approximately six months after symptom onset, the patient was referred to a tertiary referral center where the ophthalmologist suspected a histiocytic disorder; in turn, the patient was referred to our histiocytosis clinic. A detailed review of systems revealed that he also had progressive upper extremity weakness, headaches, and gait imbalance. Histopathologic review of the orbitotomy specimens from the previous biopsies revealed foamy histiocytes that were CD68+ along with Touton giant cells suggestive of Erdheim-Chester disease (ECD). BRAF-V600E immunohistochemistry (IHC) analysis was negative. Upon evaluation by neurology, he was found to demonstrate cerebellar ataxia, complete ophthalmoplegia, and left-hand motor weakness. Magnetic resonance imaging (MRI) of the brain and spine revealed areas of increased enhancement in the cerebellum, pons, as well as neural foramina of the cervical and thoracic spine. A full-body 18 F-labeled fluoro-2-deoxyglucose positron emission tomography–computed tomography (FDG PET-CT) demonstrated increased uptake in multiple sites, including bilateral orbits, right atrium, abdominal aorta and its branches, cervical and thoracic spinal nerve roots, and meta-diaphyses of the femur, tibia, and fibula around the knees (Figure). We pursued next-generation sequencing (NGS) on the tissue specimen that revealed BRAF-V600E mutation, and the patient was started on oral vemurafenib for ECD treatment.
Our Approach
ECD: A Disease in Search of a Diagnosis
ECD is a rare histiocytic disorder that has diverse clinical manifestations ranging from indolent, single-organ disease to multiorgan involvement resulting in increased morbidity and mortality. Although it was previously not considered as a neoplastic disorder, the recent discovery of recurrent and clonal MAPK-ERK pathway (RAS-RAF-MEK-ERK) mutations led to its categorization as a neoplasm by the World Health Organization in 2016.1,2 ECD can virtually involve any organ system, including the osseous system (lower extremity bones, 95%), cardiovascular system (50-60%), endocrine system (50-60%), and central nervous system (CNS; 40-50%).3 The initial clinical signs and symptoms include lower extremity pain (40%) or central diabetes insipidus (30%), with the latter often preceding the diagnosis of ECD by four to 10 years.4
Owing to its nonspecific presentation mimicking other diseases and unusual tissue tropism, one of the major challenges to clinicians is the timely diagnosis of ECD. Patients often see numerous providers and undergo several biopsies before a diagnosis is made. This is exemplified by the time from onset of symptoms to ECD diagnosis that can vary from a few months to several years (median, approximately 4 years).3 Tissue biopsy of ECD specimens classically reveals foamy histiocytes that are CD68+ or CD163+. Other histopathological markers of ECD such as S100 negativity and presence of Touton giant cells are not sensitive markers for the disease, and the tissue biopsies often show fibrosis or nonspecific inflammation.5 ECD tissue specimens demonstrate the presence of MAPK-ERK and PI3K-AKT pathway alterations in 80 to 90 percent of cases, with the most common mutation being BRAF-V600E (50-60%). Other notable alterations include mutations in MAP2K1 (15-20%), KRAS/NRAS (5-8%), PI3CA (5%), and kinase fusions (3%).
The diagnosis of ECD is clinicopathologic and is made by reviewing the clinical manifestations in conjunction with histopathological features. In the case presented here, ECD diagnosis was not made until the patient was evaluated by a center with experience in these disorders, six months after initial presentation. Characteristic manifestations of ECD include bilateral, symmetric osteosclerosis of femur, tibia, and fibula around the knees as seen on FDG PET-CT or bone scintigram (Figure). However, the former modality is preferred due to the ability to concomitantly assess for other organ involvement and to aid the selection of tissue biopsy site.6 It is crucial to acquire the PET as full-body (vertex-to-toes) imaging to capture the knee osteosclerosis. Other manifestations include wispy infiltration around the kidneys (hairy kidneys) or aorta (coated aorta). Although other histiocytosis such as Langerhans cell histiocytosis and Rosai-Dorfman disease were previously considered separate entities, there have been several reports of overlap with ECD with similar MAPK-ERK mutations.7,8 Even in cases with characteristic clinical features, a tissue biopsy is recommended to rule out concomitant overlap syndromes as well as to assess for MAPK-ERK pathway mutations.9 In cases with equivocal histopathologic features, molecular findings often aid the diagnosis. All biopsy specimens should be tested for the BRAF-V600E mutation. Although IHC is a quick and cost-effective assessment method, it is less sensitive than other modalities such as droplet digital polymerase chain reaction or NGS for detection of the mutation. More exhaustive ECD testing may be guided by disease involvement of cardiac, cerebral, and orbital tissues due to its high incidence in these phenotypes.10 In the case presented here, because of high clinical suspicion we were able to uncover a BRAF-V600E mutation on NGS testing despite a negative IHC.
Evaluation and Staging of ECD
In addition to a full-body FDG PET-CT to assess organ involvement, all patients need comprehensive laboratory evaluation to assess endocrinopathies (Table). All patients with ECD should also undergo a cardiac and brain MRI because of its high sensitivity to assess heart and CNS involvement.11,12 Further CT or MRI studies may be warranted based on the organs involved. For patients with peripheral blood count abnormalities, a bone marrow biopsy is recommended to rule out concomitant myeloid neoplasms.13 Due to the widespread organ manifestations, ECD patients benefit from multidisciplinary evaluation from physicians of different subspecialties similar to the Mayo Clinic-University of Alabama at Birmingham Histiocytosis Working Group.9 The ECD Global Alliance maintains a listlist of care centers as well as knowledgeable physicians that may provide valuable consultations to the patients.
Treatment, Response Assessment, and Surveillance of ECD
There are several treatment options for patients with ECD that may be divided into targeted and nontargeted (chemotherapy/immunosuppressive) categories. For patients with the BRAF-V600E mutation, the U.S. Food and Drug Administration has now approved vemurafenib treatment based on a phase II clinical trial that resulted in metabolic response rates higher than 80 percent.14 We typically initiate treatment with 480 mg orally twice daily, and some patients may require higher or lower doses based on response and/or tolerance. Among those with CNS disease, dabrafenib may be preferred due to potentially better CNS penetration.15 For patients without the BRAF-V600E mutation, a recent phase II trial also demonstrated 89 percent overall response rates using the MEK-inhibitor, cobimetinib.16 Other treatment options that we have used include cladribine, anakinra, and pegylated interferon, although the responses may be variable.17-19 After initiating treatment, FDG PET-CT is recommended at two to three months to assess for metabolic response, and every three to six months thereafter. It is notable that a targeted therapy may take up to six to eight months to demonstrate maximum metabolic response. Other imaging modalities may be needed based on the baseline organ involvement. Despite radiographic reduction of ECD lesions, endocrinopathies may not be reversible. Since patients with ECD can develop endocrinopathies throughout their disease course, hormone evaluations should be performed annually.20
Prognosis
Factors associated with higher mortality in ECD include advanced age and disease involving the CNS, lungs, and retroperitoneum.10 Due to advances in our understanding of the disease, the prognosis of ECD has improved drastically over the past two decades, with five-year overall survival rates of 43 percent in 1996 versus 83 percent in a recent study.10,21
Clinical Course
Three months after initiating vemurafenib, the patient had a robust partial metabolic response (Figure). Upon discontinuing the drug after a year of therapy, he experienced a radiographic disease relapse, necessitating re-administration of the BRAF inhibitor that recaptured the metabolic response.
Future Directions and Challenges
Despite advances in treatments of ECD, an area of unmet need is the early diagnosis of the disease. Many patients with ECD can survive their disease due to the targeted treatments available, but have to cope with chronic debilitating effects of the disease, including and not limited to pain, neuropsychiatric symptoms, and gait ataxia. Future research is needed to identify screening methods to diagnose ECD at early stages, such as central diabetes insipidus or periorbital xanthelasmas. There is also a need for research into a “minimal residual disease” equivalent for ECD so that we can identify patients who can safely discontinue targeted treatments and avoid cumulative toxicities.
Suggested Baseline Workup for Erdheim-Chester Disease
| Laboratory . |
|---|
| Complete blood count with differential |
| Sodium, potassium, calcium, liver transaminases, bilirubin, alkaline phosphatase |
| Blood urea nitrogen, creatinine, C-reactive protein |
| Urine and serum osmolality |
| Follicular stimulating hormone/Leutinizing hormone |
| Testosterone (male patients) or estradiol (female patients) |
| Adrenocorticotropic hormone with morning cortisol |
| Thyroid stimulating hormone and free T4 |
| Prolactin and insulin-like growth factor-1 |
| Laboratory . |
|---|
| Complete blood count with differential |
| Sodium, potassium, calcium, liver transaminases, bilirubin, alkaline phosphatase |
| Blood urea nitrogen, creatinine, C-reactive protein |
| Urine and serum osmolality |
| Follicular stimulating hormone/Leutinizing hormone |
| Testosterone (male patients) or estradiol (female patients) |
| Adrenocorticotropic hormone with morning cortisol |
| Thyroid stimulating hormone and free T4 |
| Prolactin and insulin-like growth factor-1 |
| Radiographic . |
|---|
| Full body (vertex-to-toes) PET-CT scan |
| Cardiac MRI |
| Brain MRI with gadolinium contrast |
| Radiographic . |
|---|
| Full body (vertex-to-toes) PET-CT scan |
| Cardiac MRI |
| Brain MRI with gadolinium contrast |
| Molecular . |
|---|
| Next generation sequencing for MAPK-ERK and PI3K-AKT pathway mutations |
| Kinase fusion analysis |
| Molecular . |
|---|
| Next generation sequencing for MAPK-ERK and PI3K-AKT pathway mutations |
| Kinase fusion analysis |
Abbreviations: MRI, magnetic resonance imaging; PET-CT, positron emission tomography-computed tomography.
Dr. Goyal and Dr. Go indicated no relevant conflicts of interest.