One of the major challenges in cancer treatment is tumor progression due to chemotherapy-induced drug resistance that emerges as a consequence of clonal evolution. The underlying pathobiology of this process can be seen as a form of Darwinian evolution in which the selection pressure is applied by the chemotherapy. Tumor cells that have acquired resistance through somatic mutation are selected for this trait; they then become dominant and disease progression ensues. To improve clinical outcomes, it would be advantageous to be able to track the acquired mutations that confer drug resistance so that treatment could be promptly and appropriately modified. For hematologic malignancies, such as leukemias, in which the malignant cells are circulating in abundance in the peripheral blood, obtaining samples for analysis is a simple process. However, for some hematologic malignancies (e.g., lymphomas and myelomas/plasmacytomas), and for all solid tumors, tissue sampling is often problematic. To obtain tissue for mutational analysis by repeated biopsies is a cumbersome process that puts the patient at risk for procedure-related morbidity, and the results may prove uninformative if the sample is not representative of the parts of the tumor that have acquired drug resistance. Now, however, this barrier to repeat sampling of tumor DNA appears to have been circumvented by a powerful new technology, the isolation and analysis of plasma circulating tumor DNA (ctDNA) (Figure). In the current proof of concept study, Murtaza and colleagues from Cambridge University report that this futuristic approach produces results representative of the entire tumor genomic DNA, including sequence variants derived from different clones.
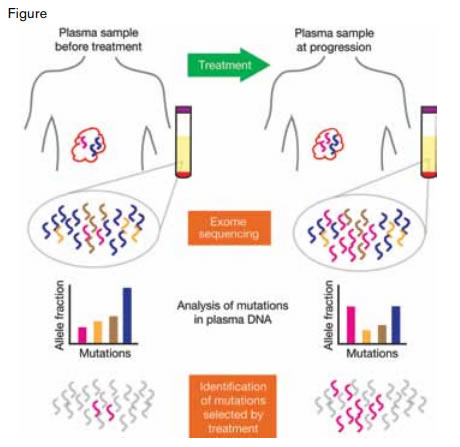
Study Design for Identification of Treatment-Associated Mutations From Exome Sequencing of Serial Plasma Samples. Plasma was collected before and at multiple time points during and after treatment of cancer patients. Mutations were identified across the plasma samples and increases in relative abundance were noted. Cataloguing of similar data across large cohorts could identify genes or pathways with recurrent mutations that arise under the selective pressure of specific treatments.
Study Design for Identification of Treatment-Associated Mutations From Exome Sequencing of Serial Plasma Samples. Plasma was collected before and at multiple time points during and after treatment of cancer patients. Mutations were identified across the plasma samples and increases in relative abundance were noted. Cataloguing of similar data across large cohorts could identify genes or pathways with recurrent mutations that arise under the selective pressure of specific treatments.
By subjecting ctDNA to deep-sequencing technology, the molecular details of chemotherapy-induced clonal selection were characterized (Figure). Murtaza et al. reported the identification of mutations associated with acquisition of drug resistance by exome sequencing of DNA isolated from serial plasma samples obtained over one to two years during chemotherapy treatment of six patient with advanced cancer (breast, ovarian, or lung). Mutations emerged during the course of treatment as represented by the following examples: 1) an activating mutation E545K in PIK3CA (phosphatidylinositol-4,5-bisphosphate 3-kinase, catalytic subunit alpha) shown to promote chemotherapy resistance in mammary epithelial cells following treatment with paclitaxel and a G56V mutation in FANCD2 (involved in DNA crosslink repair) after epirubicin treatment in the same patient; 2) a truncating mutation in RB1 (the tumor suppressor gene, retinoblastoma 1) following treatment with cisplatin; 3) a truncating mutation in MED1 (mediator complex subunit 1, an estrogen receptor co-activator) that confers tamoxifen resistance following treatment with tamoxifen and trastuzumab; and following subsequent treatment of the same patient with lapatinib and capecitabine, a splicing mutation in growth arrest-specific 6 (GAS6), a ligand for the AXL tyrosine kinase receptor implicated in chemotherapy resistance of non-small cell lung cancer and breast cancer cell lines; and 4) a resistance-conferring mutation (T790M) in epidermal growth factor receptor (EGFR) as well as a Y163C mutation in p53 following treatment with gefitinib. Changes in the allele frequencies of these mutations were noted over time, suggesting that the mutant clone had expanded as a result of an acquired proliferative/survival advantage. Simultaneous samples of tissue biopsy of metastatic disease and plasma DNA were available for analysis in two of the patients. One case of breast cancer exhibited a total of 151 mutations, 93 were present in both the tissue and plasma, with a higher allele frequency of the mutations seen in the plasma, and a positive correlation coefficient of 0.71 for mutations in the ctDNA and the tissue biopsy DNA. The other case (ovarian cancer), in which simultaneous parallel samples were available, exhibited a total of 895 mutations, of which 172 mutations were found in both tissue and plasma, with a correlation coefficient of 0.72.
In Brief
This remarkable technical advance of plasma ctDNA mutation analysis will allow real-time detection of evolving cancer clones that possess the genetic changes that confer drug resistance. As these mutations are catalogued and subjected to sophisticated informatics analysis, it will be possible to derive treatment algorithms that can identify chemotherapy combinations that can be used to eradicate emerging drug resistant mutant clones before significant tumor progression has occurred.
Competing Interests
Dr. Becker indicated no relevant conflicts of interest.