Ischemic stroke has previously been associated with sickle cell trait, though evidence for this linkage has primarily been limited to case reports1-3 and a single, prospective, population-based study4 that provided some evidence of the association. Specifically, in the Atherosclerosis Risk in Communities Study, a population-based secondary analysis, 3,497 African American participants (mean age, 54 years; 62% female) were observed for a total of 65,371 patient years. The study found that sickle cell trait was associated with an ischemic stroke with a hazard ratio of 1.4 (95% CI, 1.0-2.0).
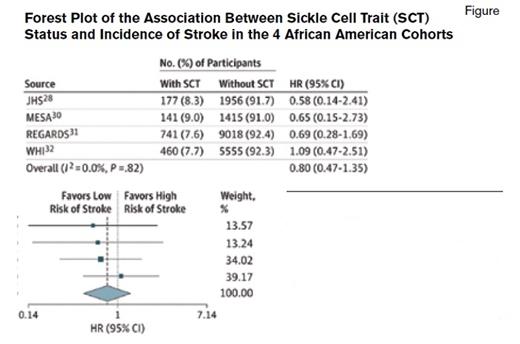
The fully adjusted Cox proportional hazards regression model (adjusted model 3) is shown. Weights are from random-effects analysis. Boxes indicate hazard ratios (HRs); error bars, 95% Cls; and diamond, overall results. HR indicates hazard ratio; JHS, Jackson Heart Study; MESA, Multi-Ethnic Study of Atherosclerosis; REGARDS, Reasons for Geographic and Racial Differences in Stroke; and WHI, Women's Health Initiative.
The fully adjusted Cox proportional hazards regression model (adjusted model 3) is shown. Weights are from random-effects analysis. Boxes indicate hazard ratios (HRs); error bars, 95% Cls; and diamond, overall results. HR indicates hazard ratio; JHS, Jackson Heart Study; MESA, Multi-Ethnic Study of Atherosclerosis; REGARDS, Reasons for Geographic and Racial Differences in Stroke; and WHI, Women's Health Initiative.
It was in this context that Dr. Hyacinth I. Hyacinth and colleagues conducted a meta-analysis of four very large population cohorts with a high proportion of African Americans: the Jackson Heart Study (September 1, 2005 - December 31, 2012); the Multi-Ethnic Study of Atherosclerosis (July 1, 2002 - December 31, 2012); Reasons for Geographic and Racial Differences in Stroke (January 1, 2003 - December 31, 2014), and the Women’s Health Initiative (October 1, 1998 - December 31, 2012). The mean age of the cohorts ranged from 50.4 to 63.2 years. Within each cohort study, the major risk factors for stroke were evaluated; these included, but were not limited to, systolic blood pressure, diabetes mellitus, hypertension, cigarette-smoking status, atrial fibrillation, left ventricular hypertrophy, and history of cardiovascular disease. Importantly, a panel of neurologists using the available medical and imaging records adjudicated each stroke. Incident ischemic stroke was defined as the first adjudicated ischemic stroke after enrollment in the prospective cohort study. In three of four cohorts, the incidence of acute ischemic stroke was lower than in the general population. After adjusting for established risk factors for ischemic stroke, the pooled hazard ratio for sickle cell trait was 0.80 (95% CI, 0.47-1.35; P = .82) (Figure). Counter to the Atherosclerosis Risk in Communities Study, these new data do not provide evidence that sickle cell trait is associated with an increased risk of ischemic stroke.
As with any meta-analysis, inherent limitations attenuate strong conclusions for subgroup analyses. Approximately 50 percent of the cohort was not directly genotyped for their sickle cell trait status; instead genetic imputation — the practice of inferring variants based on statistical inference — was used. Imputation is an acceptable strategy for genotyping, and this method was unlikely to lead to a misclassification of sickle cell trait status. Quite possibly, other modifying genes, environmental risk factors, or both, may increase the risk of ischemic stroke in individuals with sickle cell trait; however, these analyses would be considered hypotheses-generating and not hypothesis-testing. A priori: We have neither strong evidence nor demonstrated biological plausibility for how sickle cell trait in combination with other modifying genes (for instance α globin gene deletion) or environmental factors, may influence risk of ischemic stroke.
In Brief
In summary, in adults, we now have strong evidence that sickle cell trait is not associated with ischemic stroke. We await more systematic data analyses and preclinical studies to elucidate the mechanisms for the well-established adverse events associated with sickle cell trait, which include, but are not limited to, renal medullary carcinoma,5 heat-induced death without universal precautions to prevent dehydration during rigorous training,6 and splenic infarct associated with travel to high altitudes or exposure to less oxygen.7
References
Competing Interests
Dr. DeBaun indicated no relevant conflicts of interest.