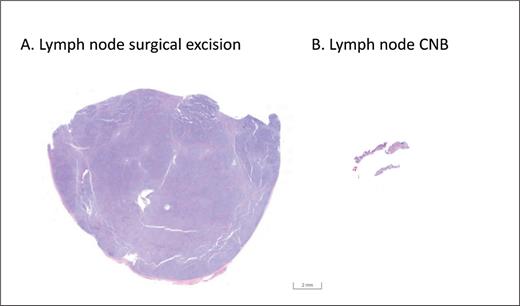
Pathologists have a perennial reputation for craving more tissue in making any type of diagnosis, and lymphoma is no exception. Speaking as a pathologist, this is completely understandable. Although we are assisted by ancillary studies such as flow cytometry, fluorescence in situ hybridization, and molecular clonality studies,1 current lymphoma diagnosis and classification continue to rely heavily on morphologic features.2,3 Tumor cytology can be affected by procedural and tissue processing artifacts such as crush, hemorrhage, and nuclear staining artifacts, and these tend to be more commonly seen in limited biopsies4,5 (Figure). Moreover, distinguishing malignant lymphomas from reactive conditions depends on analyzing the tissue architecture, which may be difficult to appreciate in a small tissue sample. While a larger excision of lesional tissue can be performed if the initial biopsy is deemed inadequate, the pathologist may perceive pressure to render a definitive diagnosis on the first biopsy in order to spare the patient an additional procedure. Despite these caveats, core needle biopsy (CNB) is becoming an increasingly frequent approach in the initial workup of suspected lymphoma, largely due to lower cost and fewer complications compared to surgical lymph node excision.6 A key question remains as to whether these advantages come at the expense of a less accurate diagnosis.
Low-power microscopic slide images of: A) a section of an excisional lymph node biopsy and B) a core needle biopsy (CNB), taken at the same magnification. The excisional biopsy contains a much larger sample of tissue, affording the pathologist an opportunity to more effectively evaluate tissue architecture and possible tumor heterogeneity.
Low-power microscopic slide images of: A) a section of an excisional lymph node biopsy and B) a core needle biopsy (CNB), taken at the same magnification. The excisional biopsy contains a much larger sample of tissue, affording the pathologist an opportunity to more effectively evaluate tissue architecture and possible tumor heterogeneity.
Dr. Charlotte Syrykh and colleagues addressed this question by analyzing the diagnostic performance of lymph node CNB compared to surgical excision in 32,285 patients with clinical suspicion of lymphoma in France. These samples were diagnosed at local institutions (a mix of university, public, and private hospitals and comprehensive cancer centers) and were all reviewed by expert pathologists through the French Lymphopath network.7 As expected, the proportion of CNB versus surgical excision increased throughout the study period, from 25 percent of cases in 2010 to 40 percent in 2018. The rate of definitive diagnosis on central expert review was significantly lower with CNB (92.3%) compared to surgical excision (98.1%). A lack of definitive diagnosis was usually due to uncertainty as to the diagnosis of lymphoma (vs. a reactive condition) or the specific lymphoma subtype rather than inadequate material. The concordance rate between local diagnoses and the central expert panel diagnoses was higher on surgical excision (78.8%) compared to CNB (76.9%). When material was referred to pathology experts owing to an initial nondefinitive diagnosis at the local hospital, the rate of the expert review rendering a definitive diagnosis was higher for surgical excisions (93.3%) compared to CNB material (81.4%), mostly due to an increase in the number of cases that could be classified into a specific lymphoma subtype. In particular, peripheral T-cell lymphomas (notably, angioimmunoblastic T-cell lymphoma) and Hodgkin lymphomas presented challenges when encountered on CNB, likely reflecting the importance of tissue architecture in rendering these specific diagnoses. In fact, nodular lymphocyte predominant Hodgkin lymphoma was diagnosed less than half as frequently on CNB compared to surgical excision.
In Brief
Overall, the study by Dr. Syrykh and colleagues confirms that a diagnosis and subtyping of lymphoma can be made by CNB in most cases. Nevertheless, the authors demonstrate that when compared with CNB, a surgical excisional biopsy does provide a definitive diagnosis (that is reproducible upon expert review) in a higher proportion of cases. Flow cytometry, which can greatly assist the classification of some lymphomas, is not routinely performed in France; thus, it is possible that the diagnostic performance of CNB may be higher in areas where flow cytometry is used more frequently. Another limitation is that the study did not evaluate the relative performance of CNB versus surgical biopsy in diagnosing lymphomas in extranodal sites. In the end, the authors conclude that “pathologists who feel uncertain about a diagnosis of lymphoma on CNB should recommend a lymph node surgical excision,” which is sage advice. Above all, it is critical to get the diagnosis correct prior to initiating treatment; if the original diagnosis was made on shaky ground due to limited biopsy material, it may be impossible to ever determine a lymphoma diagnosis with certainty.
Competing Interests
Dr. Hasserjian indicated no relevant conflicts of interest.