The Case
A 23-year-old presented to the emergency room with a headache and a fever of 101.5 degrees Fahrenheit. Physical examination revealed a fatigued patient with cervical lymphadenopathy and skin rashes/hives. The patient reported staying in a mountain house, but denied any tick bites. The patient’s COVID test was negative, while a complete blood count (CBC) revealed a white blood cell (WBC) count of 14,500/mcL; a red blood cell (RBC) count of 5.11 million/mcL; hemoglobin levels of 13.8 g/dL; hematocrit levels of 42%; a mean corpuscular volume of 89 fl; and a platelet count of 187,000/mcL. A 200-cell manual WBC differential revealed 12.9% neutrophils, 42.2% lymphocytes, 6.9% monocytes, 0.9% eosinophils, and 37.1% “other cells.” The smear was subsequently forwarded for pathologist review, with the “other cells” described as atypical lymphocytes, consistent with reactive lymphocytes of predominantly Downey type II cells. Further review of the patient’s chart showed mild transaminitis (alanine transaminase of 175 U/L, aspartate aminotransferase of 146 U/L, and alkaline phosphatase of 170 U/L). The patient’s hepatitis panel was negative. An abdominal ultrasound was notable for an enlarged spleen (7.2 cm x 7.5 cm x 15.1 cm), and a monospot test was positive, confirming the pathologist’s impression of reactive lymphocytosis in the setting of infectious mononucleosis.
The Question
What is your approach to peripheral smear review for atypical lymphocytosis?
The Response
Unlike the presence of circulating blasts or immature granulocytes, peripheral blood lymphocyte atypia is hard to define due to its variability and significant overlap between reactive and neoplastic conditions. This makes review of peripheral blood smears for identification of morphologically abnormal lymphocytes a challenging smear review indication. In the College of American Pathologists’ proficiency testing challenges, “lymphocyte, reactive” and “malignant lymphoid cell” are the top two poorly performing cell identifications, with median percent correct answers of 78% and 62%, respectively (unpublished data). Both reactive and malignant lymphocytosis can present with a range of CBC abnormalities, such as elevated WBC count due to lymphocytosis or association with thrombocytopenia and/or anemia. There are two major consequences of the incorrect interpretation of atypical lymphocytosis: delays in correct diagnosis (or even misdiagnosis) and reflex to unnecessary testing. We present our approach to atypical lymphocytosis, which we hope helps avoid these two unacceptable outcomes.
A pathologist review of peripheral blood smear is the interpretation of blood smear findings together with CBC and other available laboratory data in the clinical context.1 Microscopic examination (by conventional or digital microscopy) is the cornerstone of this review, with evaluation of the microscopic appearance of WBCs, RBCs, and platelets. Evaluation and interpretation of an atypical lymphocytosis requires examination of a representative population of lymphocytes, as the distinction between reactive versus malignant lymphocytosis is often made on population characteristics rather than individual lymphocyte characteristics.
Atypical Lymphocytosis, Reactive
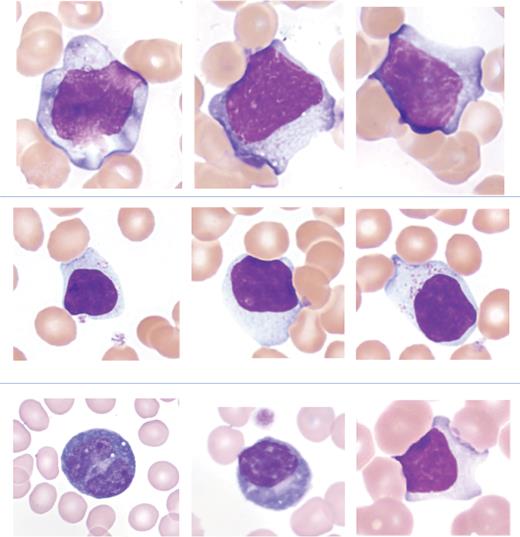
Reactive lymphocytes are usually present in infectious conditions, with Epstein-Barr virus-driven infectious mononucleosis being one of the most common, especially in young adults. Other viral infections associated with reactive lymphocytes include HIV, human T-lymphotropic virus type I, cytomegalovirus, measles, mumps, rubella, influenza, hepatitis, adenovirus, coxsackievirus, and poliovirus.2,3 Transient stress lymphocytosis is characterized by an abrupt increase in lymphocytes in patients recently hospitalized for trauma or medical event. The key distinguishing feature of reactive lymphocytosis is cell heterogeneity, including a range of cell and nuclear sizes and shapes, as well as chromatin patterns. All of these changes are present in the same smear, with careful examination of many fields essential to recognizing this important feature. While subclassification of reactive lymphocytes is not routine practice, reactive lymphocytes may be subcategorized as Downey type I, II, or III cells, with Downey type II cells representing the most common type of reactive lymphocyte.4 Downey type II cells have round to oval nuclei and moderately condensed chromatin with abundant pale gray-blue cytoplasm. The cytoplasm often partially surrounds adjacent RBCs, with peripheral basophilia and occasionally basophilia radiating perpendicularly out from the nucleus. Plasmacytoid lymphocytes (named for their resemblance to plasma cells) and large granular lymphocytes are descriptors of other reactive lymphocyte morphologies. In addition to viral infection, expansion of large granular lymphocytes may occur following autologous or allogeneic stem cell transplant, following solid organ transplant, or in the setting of dasatinib therapy for Philadelphia-positive B-lymphoblastic leukemia or chronic myeloid leukemia.5-7 Examples of reactive lymphocytes are shown in Figure 1.
Examples of reactive lymphocytes
The top row is from a patient with infectious mononucleosis and represents Downey type II cells. The middle row shows examples of large granular lymphocytes. The bottom left is a reactive lymphocyte with immunoblastic features (Downey type III cell), the bottom middle shows a plasmacytoid lymphocyte, and the bottom right is an example of a Downey type I cell. All images: Giemsa stain, 100X.
Examples of reactive lymphocytes
The top row is from a patient with infectious mononucleosis and represents Downey type II cells. The middle row shows examples of large granular lymphocytes. The bottom left is a reactive lymphocyte with immunoblastic features (Downey type III cell), the bottom middle shows a plasmacytoid lymphocyte, and the bottom right is an example of a Downey type I cell. All images: Giemsa stain, 100X.
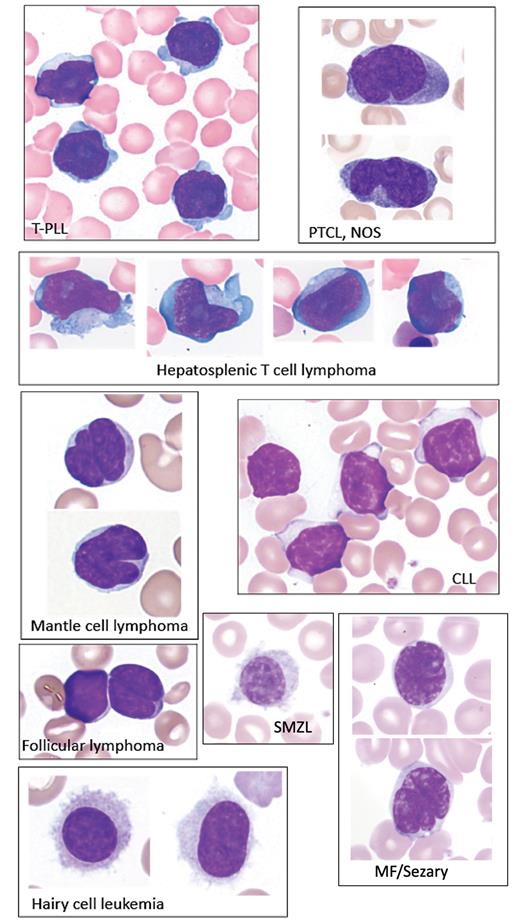
Atypical Lymphocytosis, Malignant
The most common lymphomas involving peripheral blood are chronic lymphocytic leukemia (CLL), large granular lymphocytic leukemia, splenic marginal zone lymphoma, cutaneous T-cell lymphoma (CTCL)/mycosis fungoides, and adult T-cell leukemia/lymphoma. However, any lymphoma can present with peripheral blood involvement, termed “leukemic phase,” with cell morphology usually resembling the originating site (i.e., lymph node, spleen, skin, etc.). Table 1, despite its simplicity, represents a very helpful approach to malignant lymphomas based on cell size and nuclear shape. Although not definitive, some nuclear and cytoplasmic morphologic features are associated with certain lymphomas and may be noted during review. For example, CLL can be identified by small cells with round nuclei with unevenly condensed chromatin and scant cytoplasm, while CTCL/Sézary syndrome often appears as medium-sized cells with convoluted cerebriform nuclei and condensed chromatin with inconspicuous nucleoli and a moderate amount of cytoplasm. Examples of circulating lymphoma cells are shown in Figure 2.
Categorization of malignant lymphomas by cell size and nuclear shape
| Nuclear shape . | Cell size . | ||
|---|---|---|---|
| Small . | Medium . | Large . | |
| Round | CLL, LPL | PLL, SMZL | BL |
| Slightly irregular | FL, MCL | HCL | LGLL |
| Convoluted | ATLL, CTCL | DLBCL | |
| Nuclear shape . | Cell size . | ||
|---|---|---|---|
| Small . | Medium . | Large . | |
| Round | CLL, LPL | PLL, SMZL | BL |
| Slightly irregular | FL, MCL | HCL | LGLL |
| Convoluted | ATLL, CTCL | DLBCL | |
Abbreviations: ATLL, adult T-cell leukemia/lymphoma; BL, Burkitt lymphoma; CLL, chronic lymphocytic leukemia; CTCL, cutaneous T-cell leukemia; DLBCL, diffuse large B-cell lymphoma; FL, follicular lymphoma; HCL, hairy cell leukemia; LGLL, large granular lymphocytic leukemia; LPL, lymphoplasmacytic lymphoma; MCL, mantle cell lymphoma; PLL, prolymphocytic leukemia; SMZL, splenic marginal zone lymphoma.
Examples of circulating lymphoma cells
All images: Giemsa stain, 100X. Abbreviations: CLL, chronic lymphocytic leukemia; MF, mycosis fungoides; PTCL, NOS, peripheral T-cell lymphoma, not otherwise specified; SMZL, splenic marginal zone lymphoma; T-PLL, T-prolymphocytic leukemia.
Examples of circulating lymphoma cells
All images: Giemsa stain, 100X. Abbreviations: CLL, chronic lymphocytic leukemia; MF, mycosis fungoides; PTCL, NOS, peripheral T-cell lymphoma, not otherwise specified; SMZL, splenic marginal zone lymphoma; T-PLL, T-prolymphocytic leukemia.
While in-depth knowledge of malignant cell morphology associated with various lymphomas is helpful, it is not necessary during peripheral blood smear review. Malignant lymphocytes share common features that allow for distinction from reactive lymphocytes in most cases (Table 2). We find that several features are especially helpful in suggesting lymphocytes’ malignant nature, including absence of morphologic heterogeneity, marked nuclear irregularities, presence of nucleoli, and cytoplasmic projections. Detailed review of a clinical chart can also help guide morphologic assessment.
Most common features of reactive and malignant lymphocytosis
| Feature . | Reactive . | Malignant . |
|---|---|---|
| Patient’s age | <30 | >50 |
| Lymphadenopathy | Typically absent | May be present |
| Absolute lymphocyte count | Usually increased | Increased, normal, or decreased |
| Percent lymphocytes | Usually increased | Increased, normal, or decreased |
| Platelets | Normal | Normal or decreased |
| Anemia | Absent or mild | Usually present |
| Cell heterogeneity | Present | Absent |
| Cell size | Variable but usually large | Small to medium to large |
| Nucleus | Irregular | Round, indented, folded, irregular |
| Nucleolus | Absent or inconspicuous | Absent, prominent |
| Cytoplasm | Abundant, radiating basophilia | Scant to moderate |
| Cytoplasmic projections | Absent | May be present * |
| Red blood cell molding | Present | Usually absent |
| Smudge cells | Absent | May be present ** |
| Feature . | Reactive . | Malignant . |
|---|---|---|
| Patient’s age | <30 | >50 |
| Lymphadenopathy | Typically absent | May be present |
| Absolute lymphocyte count | Usually increased | Increased, normal, or decreased |
| Percent lymphocytes | Usually increased | Increased, normal, or decreased |
| Platelets | Normal | Normal or decreased |
| Anemia | Absent or mild | Usually present |
| Cell heterogeneity | Present | Absent |
| Cell size | Variable but usually large | Small to medium to large |
| Nucleus | Irregular | Round, indented, folded, irregular |
| Nucleolus | Absent or inconspicuous | Absent, prominent |
| Cytoplasm | Abundant, radiating basophilia | Scant to moderate |
| Cytoplasmic projections | Absent | May be present * |
| Red blood cell molding | Present | Usually absent |
| Smudge cells | Absent | May be present ** |
*Cytoplasmic projections are usually seen in hairy cell leukemia and splenic marginal zone lymphoma.
**Although nonspecific, smudge cells are usually associated with chronic lymphocytic leukemia; however, they may be seen in any lymphoma where malignant cells have a high nuclear-to-cytoplasmic ratio.
Ancillary Studies
Recognition of lymphoid cell morphology as either reactive or malignant can not only expedite a patient’s workup but also help avoid unnecessary testing and associated costs. The two most common tests following atypical cell identification on a blood smear are flow cytometry and B-cell/T-cell clonality by molecular methods. Other assessments include reflex tests used based on the results of flow cytometry and clonality, such as conventional cytogenetics, fluorescence in situ hybridization, and next-generation sequencing. Flow cytometry is fast, capable of providing valuable immunophenotyping data within hours. However, depending on the criteria for flow cytometry screening, the positive test rate may be low, even in tertiary medical centers. Appropriate screening criteria will depend on the patient population.8
Conclusion
Atypical lymphocytosis is a nonspecific descriptor with poor concordance among laboratory professionals categorizing lymphocytes. Our approach as hematopathologists to a peripheral blood smear review for atypical lymphocytes includes microscopic evaluation along with review of CBC and other available laboratory data in the clinical context. Morphologic features of lymphocyte populations can help favor a reactive versus a malignant process. Peripheral smear review by an experienced pathologist can help expedite further diagnostic workup or avoid unnecessary ancillary testing.
Disclosure Statement
Drs. Courville and Pozdnyakova indicated no relevant conflicts of interest.