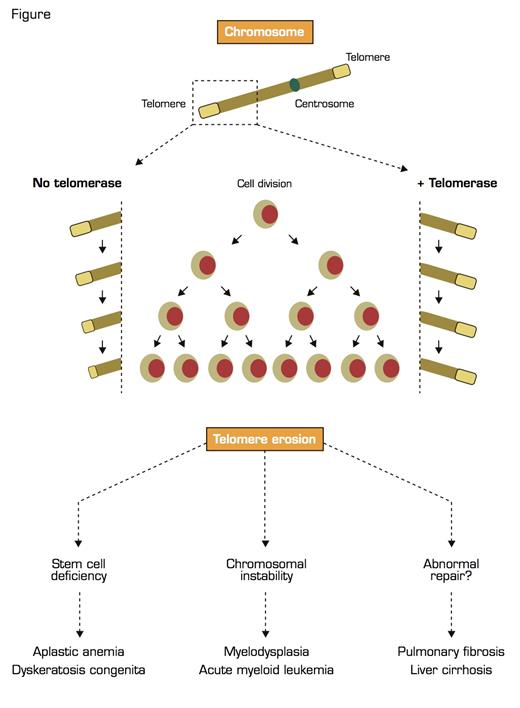
The discoveries of telomere structure and maintenance won Blackburn, Greider, and Szostak the Nobel Prize in Physiology or Medicine in 2009. Telomeres cap and protect the ends of chromosomes, and abnormal telomere erosion has marked clinical implications ranging from bone marrow failure and acute myeloid leukemia (AML) to pulmonary and hepatic fibrosis (Figure).
Telomeres are Located at the Ends of Linear Chromosomes and are Composed of Hundreds to Thousands of TTAGGG Repeats Coated by Specialized Proteins Collectively Termed Shelterin. As the cell divides, telomeres shorten due to DNA polymerase’s inability to fully replicate the telomeres. If the cell expresses telomerase (right side of the Figure), telomere lengths are maintained, preserving cellular proliferative capacity. If telomerase is absent or impaired (left side of the Figure), telomeres progressively shorten, eventually reaching critical length, inducing cell senescence, apoptosis, and chromosomal instability. These processes may be clinically translated into disease.
Telomeres are Located at the Ends of Linear Chromosomes and are Composed of Hundreds to Thousands of TTAGGG Repeats Coated by Specialized Proteins Collectively Termed Shelterin. As the cell divides, telomeres shorten due to DNA polymerase’s inability to fully replicate the telomeres. If the cell expresses telomerase (right side of the Figure), telomere lengths are maintained, preserving cellular proliferative capacity. If telomerase is absent or impaired (left side of the Figure), telomeres progressively shorten, eventually reaching critical length, inducing cell senescence, apoptosis, and chromosomal instability. These processes may be clinically translated into disease.
Due to DNA polymerase’s inability to fully replicate the ends of chromosomes, at each mitosis the newly synthesized DNA strand becomes shorter than the template strand, a fundamental phenomenon in biology termed the “end-under-replication problem.” With subsequent cell divisions, the ends of the chromosomes — telomeres — are eroded, and, when critically short, they signal proliferation arrest and apoptosis, preventing loss of important genetic material or chromosomal instability. To counter telomere loss, highly proliferative cells, including hematopoietic stem cells, express telomerase, an enzyme that adds DNA repeats to the end of telomeres, elongating them. Telomerase is composed of an RNA component that serves as a template, a reverse transcriptase enzyme, the protein dyskerin, and several other proteins, which provide stability to the complex.
Most patients with dyskeratosis congenita, an inherited pediatric bone marrow failure syndrome that is associated with mucocutaneous abnormalities (nail dystrophy, skin reticular hyperpigmentation, and leukoplakia), and some patients with acquired aplastic anemia carry mutations in genes encoding components of the telomerase complex. These mutations impair telomerase activity, causing excessive telomere shortening and eventually inducing cellular senescence and apoptosis, which clinically translates into marrow failure.
Mutations in the dyskerin encoding gene DKC1 are the cause of X-linked dyskeratosis congenita, while autosomal cases are caused by mutations in the genes for the RNA component (TERC) or, less frequently, the telomerase enzyme itself (TERT); bi-allelic mutations in other associated proteins (NOP10, NHP2) also are found in autosomal recessive dyskeratosis congenita. Mutations in TINF2, which encodes the protein TIN2 that binds and protects telomeric DNA, cause deficient telomere capping, resulting in extremely short telomeres even in the presence of normal telomerase, ultimately leading to bone marrow failure. In summary, mutations in either of the components of the telomerase complex or in telomere-binding proteins, all resulting in pathologic telomere attrition, are associated with marrow failure. This concept parallels Fanconi anemia, in which lesions in multiple genes that encode components of a single molecular pathway result in a similar clinical phenotype.
Mutations in the TERT or TERC genes also are genetic risk factors for the development of acquired aplastic anemia, a disorder without the physical stigmata typical of dyskeratosis congenita and not restricted to childhood. Patients with mutations are otherwise clinically indistinguishable from other acquired aplastic anemia patients, but they have very short telomeres in leukocytes; they usually do not respond to immunosuppressive therapy with antithymocyte globulin; and several of them have a family history positive for a hematologic disease (unexplained cytopenia, leukemia), pulmonary fibrosis, or liver cirrhosis. Telomere-length measurement may be a useful clinical tool in recognizing these patients, who are unlikely to respond to immunosuppression, as it is important to predict clinical outcome.
Telomerase mutations do not necessarily lead to bone marrow failure. Family members of patients with telomerase mutations have a telomere defect but are clinically healthy, although they usually have a hypoplastic bone marrow, reduced numbers of CD34+ cells, and increased serum levels for growth factors (G-CSF, erythropoietin). Therefore, selection of suitable sibling donors for stem cell transplantation must take into account the mutation status and telomere length of potential candidates. Additionally, other diseases have been convincingly associated with the same molecular defect, especially pulmonary fibrosis and hepatic cirrhosis.
Patients with aplastic anemia carrying telomerase mutations have an increased risk of developing myelodysplasia. Telomerase deficiency may cause variable degrees of telomere shortening in hematopoietic stem cells; due to short telomeres, these cells become prone to chromosomal instability (aneuploidy, breakage-fusion bridges, translocations) and eventually, in the presence of other genetic and/or environmental factors, are also more vulnerable to “second hits” and malignant transformation. A strong family history of myelodysplasia and myelodysplasia evolving to AML also is observed, and constitutional telomerase mutations are found in up to 8 percent of AML cases; telomerase mutations correlate with chromosomal abnormalities, especially trisomy 8 and inv(16). The TERT gene locus is also an important risk factor for many cancers, such as lung cancer, bladder cancer, and glioma.
The treatment of patients with telomerase mutations and marrow failure is mainly restricted to hematopoietic stem cell transplantation, provided a suitable non-carrier sibling donor is available, and high-dose androgen therapy. Androgens have been used for many years to treat constitutional marrow failure syndromes; only recently have we learned that sex hormones up-regulate telomerase expression and function in hematopoietic cells, including hematopoietic progenitors, perhaps providing a molecular explanation for their efficacy.
The relevance of Blackburn and her colleagues’ work in the 1980s cannot be overemphasized, given the relevance of their findings to the pathophysiology and treatment of hematologic diseases. The discoveries of telomeres and telomerase have changed treatment: Androgens are a good therapeutic option for patients with mutations, telomere length predicts outcome after immunosuppressive therapy, and short telomeres may be a contraindication for immunosuppression. In patients eligible for transplantation, careful screening of telomere length and telomerase mutations in sibling donors is advised to prevent potentially fatal graft failure.