Cord blood transplantation has been limited for adults in part because engraftment is significantly delayed compared to bone marrow or peripheral blood stem cells (PBSCs). Times to reach an absolute neutrophil count (ANC) of 500/μL and to become independent of platelet transfusions with a platelet count of at least 20,000/μL generally are within 10 to 14 days when PBSCs are transplanted, but times increase to 27 days for ANC and 60 days for platelets in adults receiving transplantation with a single cord blood unit (with the minimum nucleated cell dose of 1x107/kg recipient weight).1 When two cord blood units are administered, the times to engraftment are 23 and 62 days, on average.2
This paper reports the results of a clinical trial from Irwin Bernstein’s group at the Fred Hutchinson Cancer Research Center in which patients received two cord blood units, one unmanipulated and the other expanded in vitro prior to transplantation. For the ex vivo expansion of hematopoietic progenitor cells, they used an approach previously developed in the Bernstein laboratory3 in which thawed cord blood cells were stimulated for 16 days with delta-like 1, a ligand for notch receptors. Previous studies showed that stimulation of the notch signaling pathway promotes expansion of hematopoietic stem/progenitor cells. Ex vivo stimulation led to a 160-fold increase in the number of CD34+ cells derived from the thawed cord blood unit, and these human CD34+ cells were able to engraft the hematopoietic system of immunodeficient mice for months.
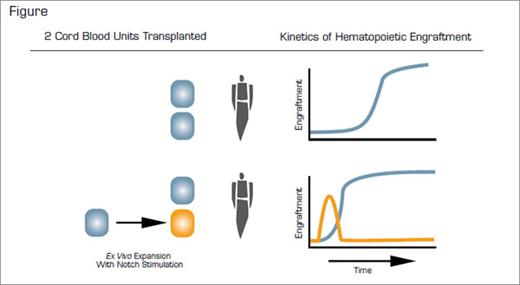
The paper describes the preclinical validations as well as preliminary results from 10 patients (ranging from 3-43 years old and 16-79 kg in weight) in an ongoing phase I clinical trial. All patients had high-risk leukemias that were in morphologic remission at the time of transplant. Cord blood units were at least a four of six HLA match with the recipient and three of six match with one another. The average infused CD34-cell dose from the expanded cord blood unit was 6 x 106 CD34+ cells/kg, while that from the unmanipulated unit was 0.24 x 106/kg. Safety was the primary objective of the trial, and there were no apparent adverse events reported. One of the 10 patients experienced primary graft rejection. The nine other patients on the trial showed a median time to ANC engraftment of 16 (range 7-34) days. There are no data yet available on the time to platelet engraftment. As depicted in the figure, the investigators found that nearly all of the early ANC engraftment was derived from the expanded unit, while in all but one patient the longer-term engraftment (beyond 20 days) was predominantly from the unmanipulated cord blood unit. Even though engraftment from the expanded unit was transient, engraftment overall and from the non-expanded unit was accelerated compared to patients who received two unexpanded units. Those patients with later engraftment (20-30 days) showed no engraftment from the expanded unit.
Ex vivo expansion of hematopoietic stem cells, which by definition are cells that are capable of long-term multi-lineage hematopoietic reconstitution in a myeloablated host, remains a Holy Grail of hematology research. However, in this study, Delaney and colleagues have successfully expanded hematopoietic progenitor cells to provide short-term multi-lineage reconstitution of myeloablated individuals. This provided a clinically important function in patients undergoing cord blood transplantation by producing much needed leukocytes prior to engraftment of long-term hematopoietic stem cells.
References
Competing Interests
Drs. Krause and Laughlin indicated no relevant conflicts of interest.