Abstract
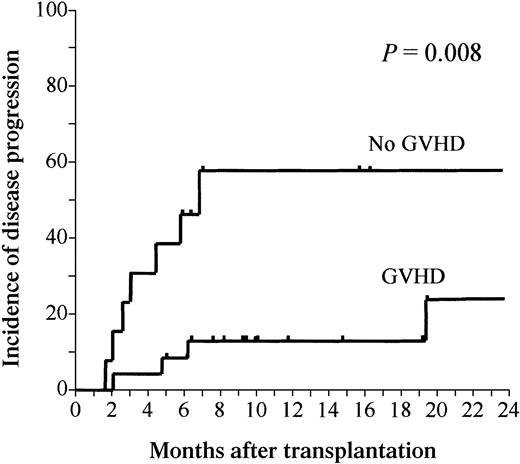
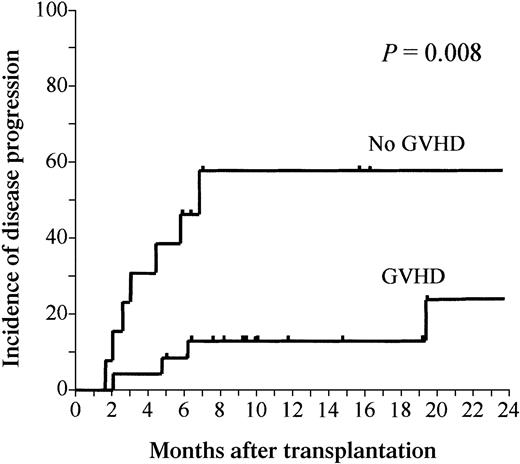
We report the results of a prospective study of a reduced-intensity conditioning (RIC) regimen followed by allogeneic peripheral blood stem cell transplantation (PBSCT) from an HLA-identical sibling in 37 patients with acute myeloid leukemia (AML; n = 17) or myelodysplastic syndrome (MDS; n = 20). The median age was 57 years, and 22 (59%) were beyond the early phase of their disease. The incidence of grade II to IV acute graft-versus-host disease (GVHD) was 19% (5% grade III-IV), and the 1-year incidence of chronic extensive GVHD was 46%. With a median follow-up of 297 days (355 days in 24 survivors), the 1-year probability of transplant-related mortality was 5%, and the 1-year progression-free survival was 66%. The 1-year incidence of disease progression in patients with and without GVHD was 13% (95% CI, 4%-34%) and 58% (95% CI, 36%-96%), respectively (P = .008). These results suggest that a graft-versus-leukemia effect plays a crucial role in reducing the risk of relapse after a RIC allograft in AML and MDS.
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) with myeloablative conditioning is a valid treatment option for adults with high-risk myelodysplastic syndrome (MDS) and acute myelogenous leukemia (AML).1,2 Several groups of investigators have developed reduced-intensity conditioning (RIC) regimens, which led to engraftment of donor lymphoid and hematopoietic stem cells without the extrahematologic toxicities of traditional myeloablative transplants.3-10 However, experience with RIC HSCT in AML and MDS is limited. We herein report results of a prospective multicenter study of a RIC regimen followed by allogeneic peripheral blood stem cell transplantation (PBSCT), which is being conducted in several institutions in Spain.
Study design
Patient selection
Eligibility criteria for entry into this RIC allogeneic PBSCT program included patients with AML or high-risk MDS who were at least 50 years old or had undergone a prior autologous HSCT. Patients gave written informed consent for inclusion in the protocol, which was approved by all local ethical review boards and the Spanish Drug Agency (protocol 99-0151). Between December 1998 and September 2001, 37 patients underwent an RIC PBSCT from an HLA-identical sibling in 9 transplantation centers in Spain.
Patient characteristics are shown in Table1. Disease phase at transplantation was categorized as early in 15 cases (AML or MDS in first complete remission [CR] after chemotherapy and hypoplastic MDS) and nonearly in 22 cases.
Conditioning regimen and supportive care
The RIC regimen consisted of fludarabine 30 mg /m2intravenously on days −9 to −5 and busulfan 1 mg/kg times 10 doses (days −6 to −4, total 10 mg/kg), as previously reported in detail.10 Graft-versus-host disease (GVHD) prophylaxis included cyclosporine A (CsA) plus short-course methotrexate (MTX), with CsA tapering starting on day +90 if no GVHD appeared. Infection prophylaxis, grading, and treatment of acute and chronic GVHD were done by standard methods.10
Chimerism analysis
After transplantation, serial samples of unfractionated peripheral blood (PB) and bone marrow (BM) mononuclear cells were analyzed for degrees of donor-recipient chimerism using polymerase chain reaction (PCR) of informative minisatellite regions, as previously described in detail.10
Statistical analysis
This interim analysis was done on March 15, 2002. The probability of progression-free survival (PFS) was estimated from the time of transplantation using Kaplan-Meier product-limit estimates. The probabilities of transplant-related mortality (TRM), disease progression, and acute and chronic GVHD were calculated using cumulative incidence estimates.11 Univariate Cox regression was used to analyze the association of various variables with disease progression, with GVHD included as a time-dependent covariate. A multivariate Cox regression analysis was done to confirm whether GVHD was an independent protective factor for disease progression, with inclusion of variables that showed a trend in univariate testing.
Results and discussion
Early procedure-related toxicities were mild in all cases, and there were no early deaths.
Hematologic recovery and infections
Hematologic recovery was prompt in all cases. Neutrophils decreased to less than 0.5 × 109/L in all cases and recovered at a median of 16 days after transplantation (range, 11-27 days). The median times to reach a stable platelet count more than 20 × 109/L and more than 50 × 109/L were day +11 (range, days 0-36) and day +14 (range, days 11-51), respectively. Twenty patients (54%) developed uncomplicated febrile neutropenia. Thus far 7 patients have reactivated cytomegalovirus (CMV), which represents a 180-day probability of developing CMV infection of 20%.
Acute and chronic GVHD
Acute GVHD occurred in 14 patients (38%), which reached grade I in 7 cases, grade II in 5, and grade III in 2 cases. The 100-day incidence of grade II to IV acute GVHD was 19% (95% CI, 10%-37%). Twenty-one of 32 evaluable patients developed chronic GVHD, which was extensive in 11 cases, for a 1-year probability of chronic extensive GVHD of 43% (95% CI, 29%-65%).
Chimerism
On days +21 to +28, 24 (65%) patients were in complete donor chimerism (CDC) in PB and 21 of 28 (75%) in the BM, and on days +90 to +100 the rates of CDC were 25 of 31 (81%) and 17 of 20 (85%), respectively. On days +180 to +200 (n = 14) and beyond 1 year after transplantation (n = 10) all patients showed a pattern of CDC.
Responses and outcome
The median overall follow-up is 297 days (range, 61-1156 days). Currently 24 patients are alive, with a median follow-up of 355 days (range, 170-1156 days). Thirteen patients died, 10 from their underlying disease and 3 from TRM. The 1-year incidence of TRM is 5% (95% CI, 1%-21%), and the 1-year PFS is 66% (95% CI, 50%-81%). The 1-year incidence of disease progression is 28% (95% CI, 16%-47). In univariate analysis only the development of GVHD (defined as acute GVHD grade II-IV or chronic GVHD or both) conferred protection against disease progression, whereas disease phase (P = .1) and achieving CDC in PB within the first 100 days after transplantation (P = .15) showed a nonsignificant trend. The 1-year cumulative incidences of disease progression in patients with (n = 24) and without (n = 13) GVHD were 13% (95% CI, 4%-34%) and 58% (95% CI, 36%-96%), respectively (hazard rate [HR] for progression 6.3; 95% CI, 1.6-24.7; P = .008; Figure1). In multivariate Cox regression analysis including GVHD, achievement of CDC within 100 days (both as time-dependent covariates) and disease phase, only GVHD showed a protective effect on disease progression (HR for progression 7.5; 95% CI, 1.8-31.3; P = .006).
Disease progression after PBSCT.
Cumulative incidence of disease progression after allogeneic PBSCT with RIC in patients with (n = 24) and without (n = 13) GVHD (acute grade II-IV or chronic GVHD). The 1-year incidence of disease progression in patients with and without GVHD was 13% (95% CI, 4%-34%) and 58% (95% CI, 36%-96%), respectively (P = .008).
Disease progression after PBSCT.
Cumulative incidence of disease progression after allogeneic PBSCT with RIC in patients with (n = 24) and without (n = 13) GVHD (acute grade II-IV or chronic GVHD). The 1-year incidence of disease progression in patients with and without GVHD was 13% (95% CI, 4%-34%) and 58% (95% CI, 36%-96%), respectively (P = .008).
Our results indicate that this fludarabine-busulfan RIC regimen is well tolerated and highly immunosuppressive, with no graft failures and a TRM of only 5%. TRM and disease progression are both high after an allogeneic HSCT in adult patients with AML and high-risk MDS.1,2,12 In these diseases the intensity of the conditioning regimens has been shown to have an influence on the risk of relapse, and thus RIC regimens may have a deleterious impact on PFS.13 On the other hand, several studies have shown that a graft-versus-leukemia effect may lead to a reduction of relapse in AML.14-16
Few data are currently available regarding the results of RIC allografts in AML and MDS. Recently, the European Group for Blood and Marrow Transplantation Acute Leukemia Working Party described the results from a retrospective study that showed a 1-year TRM of 47% in 64 patients with AML and 48% in 53 patients with MDS; the relapse rates were 30% and 33%, respectively.17 A phase II study from Houston using fludarabine plus melphalan among 31 patients showed a 1-year TRM of 34% and an overall survival and PFS of 36% and 34%, respectively.4,18 Another study reported in abstract form described 47 patients with AML who underwent related (n = 26) or unrelated donor (n = 21) HSCT after a minimal conditioning regimen.19 After a median follow-up of 218 days, 12 related (46%) and 12 unrelated (60%) transplant recipients were alive in CR, with a TRM of 18%. These results agree with our prospective series of patients who received a homogeneous conditioning regimen and standard GVHD prophylaxis and supportive care. The most important observation in our study is that the risk of disease progression after transplantation was much lower in patients who developed acute or chronic GVHD than in those who did not. These differences cannot be easily explained by other relevant prognostic factors between the groups. As seen in Table 2, patients who developed GVHD had a trend for less early phases and had a longer follow-up, variables that intuitively should increase the risk of having a relapse. Additionally, in univariate and multivariate analysis, the only variable that decreased the HR of progressing was GVHD. This observation suggests that a graft-versus-leukemia effect does exist in AML and MDS after an RIC allograft. These results, however, should be interpreted with caution due to the small sample size, the relatively short follow-up, the few relapses observed, and the potential existence of undetected confounding factors.
These results argue in favor of continuing the efforts to establish the role of RIC allografts in the long-term control of myeloid malignancies. However, for the meantime, young patients with AML or MDS should receive standard myeloablative conditioning prior to undergoing an allogeneic HSCT, whereas patients at high risk for TRM may be offered an RIC allograft within a clinical trial.
Prepublished online as
Blood First Edition Paper, April 30, 2002; DOI 10.1182/blood-2002-02-0400.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Rodrigo Martino, Servei d'Hematologia Clı́nica, Hospital de la Santa Creu i Sant Pau, Av Sant Antoni Ma. Claret, 167 08025 Barcelona, Spain; e-mail:rmartino@hsp.santpau.es.