Mesenchymal stem cells (MSCs) have been recently shown to inhibit T-cell proliferation to polyclonal stimuli. We characterized the effect of MSCs of bone marrow origin on the T-cell response of naive and memory T cells to their cognate antigenic epitopes. The immune response to murine male transplantation antigens, HY, was selected because the peptide identity and major histocompatibility complex (MHC) restriction of the immunodominant epitopes are known. C57BL/6 female mice immunized with male cells were the source of memory T cells, whereas C6 mice transgenic for HY-specific T-cell receptor provided naive T cells. Responder cells were stimulated in vitro with male spleen cells or HY peptides in the presence or absence of MSCs. MSCs inhibited HY-specific naive and memory T cells in a dose-dependent fashion and affected cell proliferation, cytotoxicity, and the number of interferon γ (IFN-γ)–producing HY peptide-specific T cells. However, the MSC inhibitory effect did not selectively target antigen-reactive T cells. When MSCs were added to the T-cell cultures in a Transwell system or MSCs were replaced by MSC culture supernatant, the inhibitory activity was abrogated. T-cell reactivity was also restored if MSCs were removed from the cultures. The expression of MHC molecules and the presence in culture of antigen-presenting cells (APCs) or of CD4+/CD25+ regulatory T cells were not required for MSCs to inhibit. We conclude that MSCs inhibit naive and memory T-cell responses to their cognate antigens. Overall our data suggest that MSCs physically hinder T cells from the contact with APCs in a noncognate fashion.
Introduction
Bone marrow (BM) stroma contains multipotential nonhematopoietic progenitor cells capable of differentiating into various tissues of mesenchymal origin. First identified for their ability to differentiate into bone and adipocytes,1further studies have demonstrated that mesenchymal stem cells (MSCs) can also differentiate, under appropriate in vitro conditions, to form chondrocytes, tenocytes, skeletal myocytes, neurons, and cells of visceral mesoderm.2-5 MSCs have been isolated in different species and are present at a low frequency (1/105) in adult BM, but they appear to constitute approximately one third of the initial adherent BM-derived stromal colonies in vitro. They are characterized by the absence of hematopoietic markers (CD45−/CD34−/CD14−) and the expression of a specific pattern of adhesion molecules (CD106+/CD54+/SH2+/SH3+). Through these molecules, MSCs interact with hematopoietic stem cells and influence their homing and differentiation. Evidence for a definite role of BM stroma in T-cell development comes from the observation that the BM microenvironment provides appropriate support for T cells to develop in the absence of the thymus6 and that the majority of T cells adhering to BM stroma display an immature phenotype.7 Furthermore, after BM transplantation, BM stromal cells appear to migrate to the thymus where they participate in the positive selection of thymocytes.8,9 In addition to providing critical cell-cell contact, MSCs produce growth factors for hematopoiesis and may attract infused hematopoietic stem cells to the marrow by inducing homing receptors. In a nonobese diabetic/severe combined immunodeficiency (NOD/SCID) system Peled et al showed that stromal-derived factor 1 (SDF-1) and its receptor CXCR4 enhance CD34+ cell migration and engraftment in BM.10Therefore, the BM microenvironment greatly influences the developmental potential of hematopoietic stem cells. These characteristics have generated substantial interest in the transplantation setting where MSCs may be a promising cell type for tissue engineering, cellular therapy, and somatic gene therapy applications. Studies already conducted in both humans and animal models have demonstrated that MSCs are capable of long-term engraftment and in vivo differentiation.11 12
Great potential for MSCs would be derived from the observation that they can exert an immunoregulatory activity. Their effects, especially on mature T lymphocytes, have not yet been defined. It has recently been reported that MSCs can inhibit T-cell proliferation induced in a mixed lymphocyte reaction (MLR) or by nonspecific mitogens.13 Of particular interest is the observation that in vivo administration of MSCs in baboons significantly prolongs the survival of major histocompatibility complex (MHC)–mismatched skin grafts.14 Because these properties might open attractive possibilities in the field of hematopoietic as well as solid organ transplantation, better characterization of MSC immunoregulatory activity and the elucidation of its mechanism are crucial. In view of the lack of MHC class I and II molecules on MSCs, it is difficult to ascribe specific T-cell receptor (TCR)/MHC/peptide interactions to their mechanism of immunoregulation. However, MSCs might selectively inhibit T cells that have encountered antigen, sparing those that have not been activated by TCR engagement. The susceptibility of naive and memory T cells to immunoregulatory stimuli15 could have profound implications when considering potential clinical applications of MSCs. We addressed these questions using an animal model in which the effect of MSCs of BM origin on the immune responses to various peptide epitopes of the transplantation antigen HY was evaluated. In this system the peptide identity and the MHC restriction of the immunodominant epitopes are known.16 17 We found that inhibition requires the presence of MSCs in culture and MSC–T-cell contact. Both naive and memory cells are subjected to MSC-mediated suppression but MSCs do not appear to selectively target antigen-reactive T cells. The MSC inhibitory effect does not require the presence of antigen-presenting cells (APCs) and is not mediated through CD4+/CD25+ regulatory T cells. The implications of these results are discussed.
Materials and methods
Mice
C57BL/6 (H2b), BALB.B (H2b), and CBA (H2k) mice were purchased from Olac Harlen (Bicester, United Kingdom). CBA/Ca, C57BL/6-Thy1.1, and C3H.SW (H2b) mice were bred by Clinical Biomedical Services at the Hammersmith Hospital. Mice were used between age 7 and 10 weeks of age.
C6 TCRhigh mice (C6) are transgenic for the Vα8 and Vβ11 TCR chains from the HY-specific CD8+ T-cell clone, C6, specific for the HY antigen-derived peptide TENSGKDI presented by H2Kk (HY Kk).17 18 The strain is on a CBA/Ca background. Spleen cells from these mice were used as a source of HY-specific naive T cells. HY-specific memory T cells were obtained by immunizing C57BL/6 female mice by intraperitoneal injection of 5 × 106 syngeneic male splenocytes.
Generation of MSCs
MSCs were generated from BALB.B (H2b), C3H.SW (H2b), or CBA (H2k) mice. BM cells, collected by flushing femurs and tibias with medium, were cultivated in 6-well plates or 25-cm2 flasks (Costar, Cambridge, MA) at a concentration of 106/mL nucleated cells in Dulbecco modified Eagle medium (DMEM), with high glucose concentration, GLUTAMAX I (Gibco BRL, Paisley, United Kingdom), 10% heat-inactivated adult bovine serum (Labtech International, Sussex, United Kingdom), 100 U/mL penicillin, and 100 μg/mL streptomycin (Gibco BRL). No cytokines were added at any stage. Cultures were incubated at 37°C in a 5% CO2 atmosphere. After 72 hours, nonadherent cells were removed. When 70% to 80% confluent, adherent cells were trypsinized (0.05% trypsin at 37°C for 5 minutes), harvested, and expanded in larger flasks. A homogenous cell population was obtained after 3 to 5 weeks of culture. Before further expansion and experimental use, MSCs were tested for their ability to differentiate into adipocytes and osteoblasts.19 Adipocytic differentiation was induced by 10−8 M dexamethasone, whereas 10−8 M dexamethasone, 50 μg/mL ascorbic acid, and 10 mM β-glycerophosphate were used for osteoblastic differentiation. Oil red O and von Kossa dyes were used to identify adipocytes and osteoblasts, respectively. More than 90% of the cells differentiated depending on the time left in culture with the differentiating agent. The identity of MSCs was also confirmed by immunophenotypic criteria, based on the expression of CD106 and the absence of hematopoietic (with anti-CD45, -CD14, -CD11c antibodies) or endothelial cell (with anti-CD31 antibodies) markers. All antibodies were purchased from Pharmingen (Oxford, United Kingdom). MSCs were maintained in culture for no more than 15 in vitro passages. The proportion of CD45+ cell in the MSC preparations used in the various experiments never exceeded 3% CD45+cells.
In selected experiments the 3T3-F442A MSC line (from a H2dmouse), a kind gift of Dr H. Green (Harvard Medical School, Boston, MA), was used. The cells were cultivated in DMEM containing 10% heat-inactivated adult bovine serum (Gibco BRL) according to the conditions originally described.20
T-cell cultures
All cultures were carried out in RPMI 1640 supplemented with 5 × 10−5 M 2-mercaptoethanol (2-ME), 10% fetal calf serum (FCS), GLUTAMAX I (Gibco BRL, Life Technologies, United Kingdom), 100 U/mL penicillin, and 100 μg/mL streptomycin. In some experiments an anti–transforming growth factor β (TGF-β1-β2-β3) monoclonal blocking antibody (Genzyme, Cambridge, MA) was added to the cultures at a concentration of 1 and 10 μg/mL.21
Depletion of CD25+cells
Depletion of CD25+ cells was performed using MiniMacs system (Miltenyi Biotec, Camberley, United Kingdom). Biotinylated anti-CD25 antibodies (7D4 clone; BD Pharmingen, Germany) were added to spleen cell suspensions at a concentration of 1 μl/30 × 106 cells/mL and incubated at 4°C for 20 minutes. After extensive washing with phosphate-buffered saline (PBS), cells were incubated with Mini-MACS streptavidin MicroBeads (Miltenyi Biotech) for 15 minutes and subjected to passage through selection columns in a magnetic field. Fluorescence-activated cell sorting (FACS) analysis of the eluted fraction (CD25−) stained with a phycoerythrin (PE)–labeled anti-CD25 (PC61 clone) showed CD25+ cells to be less than 1%.
Antigenic peptides
Stimulator cells were pulsed with 1000 ng/mL Kk-restricted (TENSGKDI) HY peptide17 (encoded by the Smcy gene) or with the Db-restrictedSmcy (KCSRNRQYL),22 the Uty(WMHHNMDLI)23 encoded, and the Ab-restrictedDby encoded (NAGFNSNRANSSRSS)24 HY peptides at 37°C for 2 hours. Unpulsed irradiated CBA or C57BL/6 female splenocytes were used as negative controls.
T-cell proliferation assay
T-cell proliferation assays were performed in round-bottom 96-well plates (Costar) in a total volume of 0.2 mL RPMI 1640. A total of 0.5 μCi (0.0185 MBq) [3H]-thymidine (ICN, Costa Mesa, CA) was added into each well 2 (naive transgenic T cells) or 3 (memory T cells) days later as required, and cells were harvested onto glass fiber filters using an LKB 96 well-harvester (Wallac Oy, Turku, Finland) after an additional 24 hours. Uptake of [3H]-thymidine was measured on an LKB Betaplate counter (Wallac Oy). The results are expressed as mean counts per minute (cpm) for triplicate cultures (SEs were routinely < 10%).
CD3/CD28 stimulation
CD28/CD3-coated Dynabeads (Dynal, Bromborough, United Kingdom) were prepared by conjugating 5 μg CD28 and CD3 antibodies (both from Pharmingen) to 107 beads, according to the manufacturer's instructions. For proliferation, 1 to 5 × 105 responder T cells were incubated with 1 to 5 × 104 CD3/CD28-coated Dynabeads/well. The cells were cultivated in a total volume of 200 μL in flat-bottomed 96-well plates and assessed for proliferation 3 days later.
T-cell cytotoxicity
Effector cells were incubated in 96-well plates with51Cr-labeled peptide-pulsed RMA-S target cells at effect-to-target (E/T) ratios of 50:1, 17:1, 5:1, and 1.5:1. After 4 hours, 100 μL supernatant was collected and 51Cr release was measured using a γ counter. Results were calculated from a 12-point regression curve resolved at an E/T ratio of 10:1. The percentage of lysis was calculated from the formula 100 × (E − M)/(T − M), where E is the experimental release, M is the spontaneous release in the presence of medium alone, and T is the maximum release in the presence of 5% Triton X-100.
Flow cytometric analysis
In addition to the monoclonal antibodies listed in “Generation of MSCs,” MSCs were also stained with CD80 (B7-1), CD86 (B7-2), class I (H2), and class II (H2A) MHC molecules, all purchased from Pharmingen. For immunophenotype analysis, MSCs were detached using trypsin/EDTA (ethylenediaminetetraacetic acid), washed and resuspended at 106/mL. The 100 μL cell suspension was incubated at 4°C for 15 minutes with mouse unconjugated immunoglobulins (Sigma Immunochemicals, Poole, United Kingdom), followed by incubation with the specific antibody at 4°C for 30 minutes. Cells were washed with PBS containing 1% bovine serum albumin and 0.1% sodium azide (PBSAS). At least 10 000 events were analyzed by flow cytometry (FACScan; Becton Dickinson, Heidelberg, Germany) using Cell Quest software.
Antigen-specific T-cell responses were measured by enumerating interferon γ (IFN-γ)–producing T cells in response to HY peptides. Irradiated syngeneic splenocytes, pulsed with 10 nM HY peptides at 37°C for 2 hours, and then washed, were added to responder T cells at a 1:1 ratio. Prior to peptide pulsing, stimulator cells were depleted of T cells with antimouse pan-T Dynabeads (Dynal, Bromborough, United Kingdom). Nonpeptide-pulsed, irradiated syngeneic splenocytes were used as the negative control. During the last 4 hours of stimulation, Brefeldin A (Sigma) was added at a concentration of 10 μg/mL to block cytokine secretion. At the end of the cultures, the cells were stained with anti-CD4 and anti-CD8 (Pharmingen). Subsequently, the cells were washed with PBS and fixed/permeabilized with a commercial solution (permeabilizing solution, Becton Dickinson) for 10 minutes. After further washing, the cells were stained with anti-IFN-γ antibody (Pharmingen) for 30 minutes at room temperature. At least 100 000 events in the lymphocyte gate were analyzed at FACScan.
CD8+ T cells expressing H2b restricted HY-specific T-cell receptors were analyzed by using soluble/MHC peptide tetramers. Tetramers were produced by refolding H2-Db heavy chain with β2-microglobulin and HY peptides WMHHNMDLI (encoded by the Uty gene) or KCSRNRQYL (encoded by theSmcy gene),22,23 as previously described.16 Tetramers were conjugated with PE-labeled ExtrAvidin-R-PE complex (Sigma). Before staining, cells were depleted of the B-cell fraction by negative selection with antimouse pan-B Dynabeads (Dynal).
Transwell cultures
Splenocytes (15 × 106/mL) from HY-immunized C57BL/6 female mice were cultivated with irradiated syngeneic male splenocytes (15 × 106/mL) in the lower chamber of a 24-mm diameter Transwell plate with a 0.3-μm pore size membrane (Costar). Autologous or allogeneic MSCs (2 × 105) were seeded onto the Transwell membrane of the inner chamber 1 to 2 hours before the beginning of the culture. Control cultures did not contain MSCs or MSCs were added directly to the secondary MLR. After 7 days, viable cells were evaluated for antigen-specific intracellular IFN-γ and frequency of peptide/MHC tetramer-positive/CD8+ T cells.
In selected experiments, MSCs were replaced with supernatant from MSC cell cultures. A day before being split, MSC culture supernatant was harvested, centrifuged, and filtered through a 0.2-μm Millipore filter.
Results
MSCs fail to stimulate T cells in secondary H2-mismatched MLR
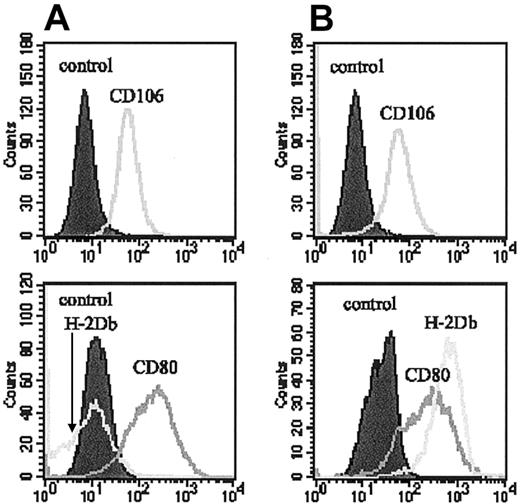
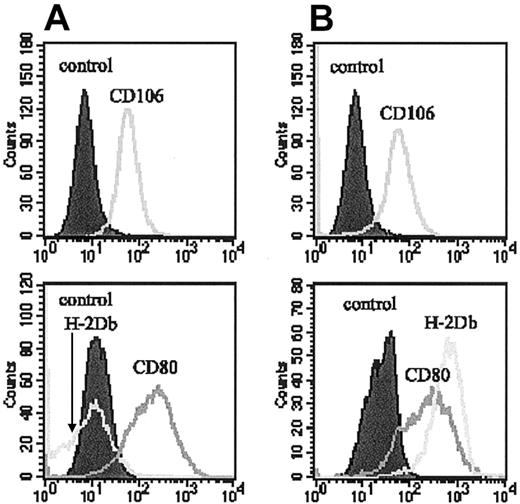
Initial experiments showed MSCs to be poor stimulators of secondary MLRs. Their ability to function as APCs was tested by using MSCs as stimulators of secondary allogeneic MLR. Spleen cells (2 × 105/well) from CBA (H-2k) mice were used as responder cells in primary cultures stimulated with irradiated BALB.B spleen cells (5 × 105/well). Cells harvested at day 7 from these primary cultures were then seeded at 2 × 105/well and restimulated with graded numbers (102, 103, 104/well) of irradiated (60 cGy) MSCs of BALB.B origin. BALB.B splenocytes (2 × 105/well) were used as stimulators in the control cultures. The limit of the maximum number of MSCs (104/well) was chosen because at this concentration MSCs occupy on a 96-well plate the approximately same surface as 2 × 105 splenocytes, the number producing the best stimulation of secondary MLR (not shown). No proliferation was detected at any of the MSCs doses used (Figure 1). No difference was seen whether the MSCs were irradiated or not. This lack of stimulator cell activity was consistent with their phenotype: MSCs expressed neither MHC class I nor class II molecules. The analysis for costimulatory molecules showed that they did not express CD86, although they were positive for CD80 (Figure2). To assess whether the lack of MHC class I expression was the major factor for the inability of MSCs to present alloantigens, MSCs were pretreated with IFN-γ prior to their use as stimulators of secondary MLRs. Despite the induction of MHC class I expression (Figure 2), no proliferation was observed (Figure1). MHC class II was not expressed following IFN-γ pretreatment.
MSCs do not stimulate allogeneic T cells.
The ability of MSCs to function as APCs was tested by using MSCs as stimulators of secondary allogeneic MLRs. Spleen cells from CBA (H2k) mice, stimulated in primary cultures with BALB.B (H2b) spleen cells (2 × 105/well), were restimulated with (A) BALB.B or (B) autologous CBA splenocytes as stimulators in the control cultures and with (C) graded numbers (102, 103, 104/well) of irradiated (60 cGy; black bars) or nonirradiated (white bars) MSCs of BALB.B origin. (D) In a separate experiment, BALB.B MSCs were pretreated with IFN-γ (100 U/mL for 48 hours) before being used in the cultures. (E) Proliferation of MSCs alone not irradiated. Cultures were performed in triplicate and the results reported are the average of 3 experiments of identical design. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures (stimulation with syngeneic spleen cells) in all experiments.
MSCs do not stimulate allogeneic T cells.
The ability of MSCs to function as APCs was tested by using MSCs as stimulators of secondary allogeneic MLRs. Spleen cells from CBA (H2k) mice, stimulated in primary cultures with BALB.B (H2b) spleen cells (2 × 105/well), were restimulated with (A) BALB.B or (B) autologous CBA splenocytes as stimulators in the control cultures and with (C) graded numbers (102, 103, 104/well) of irradiated (60 cGy; black bars) or nonirradiated (white bars) MSCs of BALB.B origin. (D) In a separate experiment, BALB.B MSCs were pretreated with IFN-γ (100 U/mL for 48 hours) before being used in the cultures. (E) Proliferation of MSCs alone not irradiated. Cultures were performed in triplicate and the results reported are the average of 3 experiments of identical design. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures (stimulation with syngeneic spleen cells) in all experiments.
Immunophenotype of BM MSCs.
MSCs were analyzed for the expression of CD106, CD80, and MHC class I molecules in standard conditions (A) or after 48 hours of culture with 100 U/mL IFN- γ (B).
Immunophenotype of BM MSCs.
MSCs were analyzed for the expression of CD106, CD80, and MHC class I molecules in standard conditions (A) or after 48 hours of culture with 100 U/mL IFN- γ (B).
MSC inhibit naive and memory antigen-specific T cells
Because, despite the expression of MHC class I and some costimulatory molecules, MSCs failed to induce T-cell stimulation, we tested whether this could be attributed to an inhibitory effect on T-cell activation. The effect of addition of MSCs to cultures of both naive and memory HY-specific T cells in the presence of their cognate peptides was tested. Splenocytes from C6 mice transgenic for a H2-Kk-restricted HY-specific T-cell receptor were used as a source of naive T cells and cultivated in the presence of irradiated syngeneic (CBA, H2k) spleen cells pulsed with the cognate Kk-restricted HY peptide (HY KkSmcy) as APCs. Graded doses of MSCs were added as third-party cells for the duration of the in vitro stimulation. After 24 hours CD8+cells were analyzed for IFN-γ by intracellular staining (Figure3B). Parallel cultures were assessed for T-cell proliferation after 48 hours (Figure 3A). Both HY peptide-specific IFN-γ production and T-cell proliferation were inhibited. Inhibition was dependent on the number of MSCs in culture. The proliferative activity was significantly inhibited at an MSC/responder (M/R) ratio as low as 1:104. At the highest ratio (1:101), T-cell proliferation and the percentage of IFN-γ–producing CD8+ T cells were reduced by 85% and 53%, respectively.
MSCs inhibit the response of naive antigen-specific T cells in a dose-dependent fashion.
Splenocytes from C6 mice transgenic for a Kk-restricted HY-specific TCR were stimulated with irradiated syngeneic (CBA, H-2k) spleen cells pulsed with the cognate HY KkSmcy (TENSGKDI) peptide. Graded doses of MSCs were added as third-party cells for the duration of the in vitro stimulation. After 24 hours CD8+ cells were analyzed for IFN-γ by intracellular staining (B). T-cell proliferation was assessed after 48 hours (A). Results are shown for cells cultured in the presence (▪) or absence ( ) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
MSCs inhibit the response of naive antigen-specific T cells in a dose-dependent fashion.
Splenocytes from C6 mice transgenic for a Kk-restricted HY-specific TCR were stimulated with irradiated syngeneic (CBA, H-2k) spleen cells pulsed with the cognate HY KkSmcy (TENSGKDI) peptide. Graded doses of MSCs were added as third-party cells for the duration of the in vitro stimulation. After 24 hours CD8+ cells were analyzed for IFN-γ by intracellular staining (B). T-cell proliferation was assessed after 48 hours (A). Results are shown for cells cultured in the presence (▪) or absence ( ) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
Splenocytes from wild-type female C57BL/6 (H2b) mice immunized with syngeneic male spleen cells were used as a source of HY-specific memory T cells. They were restimulated in vitro with syngeneic male spleen cells. Graded doses of MSCs were added as a third party to the MLR. After 7 days, the cells were harvested and restimulated with H2b-restricted HY peptide-pulsed (HY DbSmcy, HY DbUty, HY AbDby) female spleen cells and assessed for T-cell proliferation (Figure 4A), number of HY peptide-specific IFN-γ+ (Figure 4B), and HY DbSmcy and HY DbUtytetramer-positive CD8+ T cells (Figure 4C). To measure HY-specific cytotoxic activity, cells were harvested after 5 days and tested against HY peptide-pulsed (DbSmcy and DbUty) RMA-S cell line in a51Cr-release assay (Figure 4D). Proliferation, number of IFN-γ–producing and tetramer-positive CD8+ cells, and the cytotoxic activity of these HY-specific memory T cells were inhibited by MSCs in a dose-dependent fashion. It is interesting to note that the effector functions (IFN-γ production and cytotoxicity) of memory T cells appeared to be more susceptible to inhibition than antigen-specific T-cell expansion (proliferation and expansion of tetramer-positive T cells). Furthermore, the percentage of inhibition observed on IFN-γ production is greater than that observed on cytotoxic activity, thus suggesting that MSCs could selectively interfere with certain pathways of T-cell activation/function.
MSCs inhibit the response of antigen-specific memory T cells in a dose-dependent fashion.
Splenocytes from normal, nontransgenic female C57BL/6 (H-2b) mice immunized with syngeneic male spleen cells were restimulated in vitro with syngeneic male spleen cells. Graded doses of MSCs were added as a third party to the MLRs. After 7 days, the cells were harvested and restimulated with female spleen cells pulsed with the HY peptides HY DbSmcy (KCSRNRQYL), HY DbUty (WMHHNMDLI), and HY AbDby (NAGFNSNRANSSRSS) and then assessed for T-cell proliferation (A), numbers of HY-specific IFN-γ+cells (B), and HY DbSmcy and HY DbUty tetramer-positive CD8+ T cells (C). HY-specific cytotoxic activity was tested against HY peptide-pulsed (HY DbSmcy and HY DbUty) RMA-S cell line in a51Cr-release assay (D). The results refer to the cultures in the presence (▪) or absence ( ) of the HY peptide. The results reported are the average of 5 experiments of identical design. T-cell proliferations (2 experiments) were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates the MSC-to-responder T cells ratio. * signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
) of the HY peptide. The results reported are the average of 5 experiments of identical design. T-cell proliferations (2 experiments) were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates the MSC-to-responder T cells ratio. * signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
MSCs inhibit the response of antigen-specific memory T cells in a dose-dependent fashion.
Splenocytes from normal, nontransgenic female C57BL/6 (H-2b) mice immunized with syngeneic male spleen cells were restimulated in vitro with syngeneic male spleen cells. Graded doses of MSCs were added as a third party to the MLRs. After 7 days, the cells were harvested and restimulated with female spleen cells pulsed with the HY peptides HY DbSmcy (KCSRNRQYL), HY DbUty (WMHHNMDLI), and HY AbDby (NAGFNSNRANSSRSS) and then assessed for T-cell proliferation (A), numbers of HY-specific IFN-γ+cells (B), and HY DbSmcy and HY DbUty tetramer-positive CD8+ T cells (C). HY-specific cytotoxic activity was tested against HY peptide-pulsed (HY DbSmcy and HY DbUty) RMA-S cell line in a51Cr-release assay (D). The results refer to the cultures in the presence (▪) or absence ( ) of the HY peptide. The results reported are the average of 5 experiments of identical design. T-cell proliferations (2 experiments) were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates the MSC-to-responder T cells ratio. * signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
) of the HY peptide. The results reported are the average of 5 experiments of identical design. T-cell proliferations (2 experiments) were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates the MSC-to-responder T cells ratio. * signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
MSCs do not specifically target antigen-reactive T cells
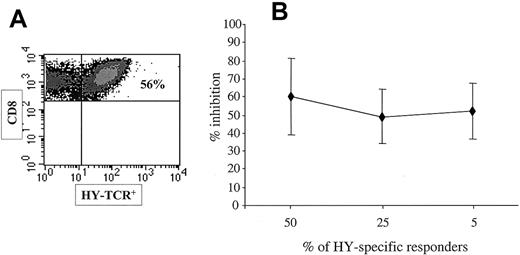
Although MSCs can inhibit antigen-specific immune responses, it is unlikely that this results from the recognition of the cognate peptide presented by MSCs because they lack expression of MHC molecules. Nevertheless, MSCs might specifically interact with and inhibit only the T cells that become activated after encountering antigen. To address this question we used as responder cells a population containing different proportions of HY-specific T cells but we kept the number of MSCs fixed. Memory spleen cells from HY-immune female C57BL/6 mice were stimulated in vitro with male cells. After 7 days, the cultures, which contained an average of 50% of DbUty tetramer-positive CD8+ T cells (Figure 5A) were used for restimulation either directly or diluted 1:2 or 1:10 with splenocytes from naive female mice to reduce the concentration of HY-specific T cells to 25% or 5%, respectively. Naive and memory cells were from mice polymorphic for the Thy1 allele (Thy1.1+ and Thy1.2+, respectively) to be able to confine the analysis to the memory T-cell population. Responder cells were restimulated with H2b-restricted HY peptide-pulsed (HY DbSmcy, HY DbUty, HY AbDby) female spleen cells and assessed for number of HY peptide-specific IFN-γ+ Thy1.2+cells generated in the presence or absence of a fixed number of MSCs. In this system the ratio between MSCs and T cells remained the same, but the ratio between MSCs and HY-specific T cells varied. The inhibitory effect of MSCs on HY-specific memory T cells after in vitro expansion is significant but not complete. By reducing the ratio between antigen-specific and non–antigen-specific T cells up to 10-fold, we would expect a higher inhibition if MSCs exclusively targeted antigen-specific T cells. However, no difference in the magnitude of inhibition was observed at different ratios between MSCs and HY-specific T cells (Figure 5B).
MSCs do not specifically target antigen-reactive T cells.
Spleen cells from normal Thy1.2 C57BL/6 HY-immune female mice were stimulated with syngeneic male cells. After 7 days the proportion of HY-TCR+ T cells was 50% (A). These responder cells were used as such or mixed with splenocytes from Thy1.1 C57BL/6 naive female mice at a 1:2 or 1:10 ratio. Then 5 × 106 cells of the different mixtures were stimulated with equal number of HY peptide-pulsed (DbSmcy, DbUty, AbDby) syngeneic female cells in the presence or absence of a fixed number (105) of MSCs. After 24 hours the Thy1.2+ cell population was assessed for numbers of peptide-specific IFN-γ+ cells. The graph in panel B reports the percentages of inhibition exerted by MSC on the different mixtures of responder cells. The bars show SDs.
MSCs do not specifically target antigen-reactive T cells.
Spleen cells from normal Thy1.2 C57BL/6 HY-immune female mice were stimulated with syngeneic male cells. After 7 days the proportion of HY-TCR+ T cells was 50% (A). These responder cells were used as such or mixed with splenocytes from Thy1.1 C57BL/6 naive female mice at a 1:2 or 1:10 ratio. Then 5 × 106 cells of the different mixtures were stimulated with equal number of HY peptide-pulsed (DbSmcy, DbUty, AbDby) syngeneic female cells in the presence or absence of a fixed number (105) of MSCs. After 24 hours the Thy1.2+ cell population was assessed for numbers of peptide-specific IFN-γ+ cells. The graph in panel B reports the percentages of inhibition exerted by MSC on the different mixtures of responder cells. The bars show SDs.
MSC inhibitory effect is not MHC-dependent
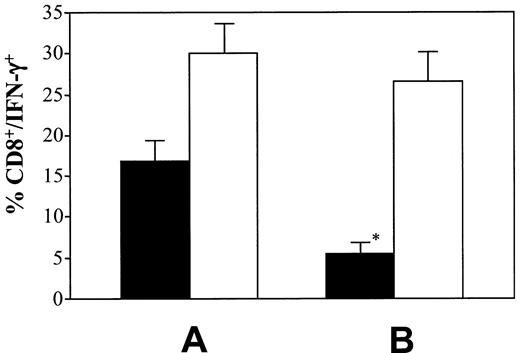
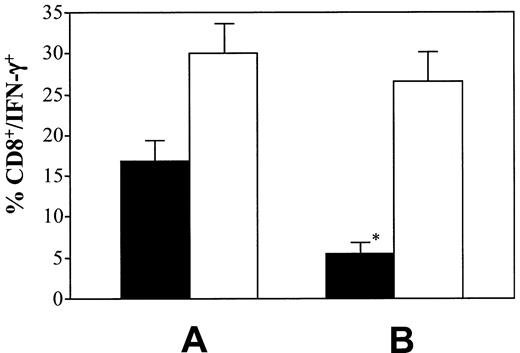
MSCs do not constitutively express MHC molecules, but they can do so after treatment with IFN-γ. In the cultures in which MSCs were added to the MLR as third party, we observed that after 7 days they expressed MHC class I molecules, probably as a result of IFN-γ production in the culture (data not shown). Although the presence of MHC class I molecules on MSCs does not appear to induce the proliferation of allogeneic T cells in MHC-mismatched cultures (Figure1), we tested whether MHC class I molecule expression was required for the inhibitory effects on naive and memory HY-specific T cells to be exerted. For these experiments, we used the 3T3-F442A MSC line of BALB/c origin, which does not express MHC molecules even after IFN-γ treatment (data not shown). No difference in the inhibitory activity was detected in comparison with H2b-matched BALB.B MSCs in terms of proliferation and IFN-γ production by naive (Figure6A) or memory (Figure 6B) responder cells. These findings were consistent with the observation that C6 splenocytes (H2k) can be inhibited by H2b MSCs (Figure 3).
The MSC inhibitory effect is MHC-independent.
Spleen cells from C6 transgenic (naive) (A) or normal C57BL/6 HY-immune (memory) (B) mice were stimulated with HY KkSmcy peptide or syngeneic male cells, respectively, as described previously, in the presence or absence of the 3T3-F442A MSC line, which does not express MHC class I molecules even after IFN-γ treatment. T-cell proliferation (cpm) and percentage of IFN-γ–producing CD8+ T cells were evaluated. The results refer to the cultures in the presence (■) or absence (▪) of HY antigen. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures without MSC in all experiments.
The MSC inhibitory effect is MHC-independent.
Spleen cells from C6 transgenic (naive) (A) or normal C57BL/6 HY-immune (memory) (B) mice were stimulated with HY KkSmcy peptide or syngeneic male cells, respectively, as described previously, in the presence or absence of the 3T3-F442A MSC line, which does not express MHC class I molecules even after IFN-γ treatment. T-cell proliferation (cpm) and percentage of IFN-γ–producing CD8+ T cells were evaluated. The results refer to the cultures in the presence (■) or absence (▪) of HY antigen. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures without MSC in all experiments.
MSC inhibitory effect is transient
The fact that MHC expression on MSCs does not influence the MSC-mediated inhibition suggests that it also does not require the T cells to recognize antigen on MSCs. Moreover, our data show that MSCs do not exclusively target antigen-reactive T cells. It remained to be determined whether the MSCs induced persistent nonresponsiveness or whether the inhibitory effect was transient. To address this question, splenocytes from C6 mice were stimulated with the Kk-restricted HY peptide in the presence or absence of MSCs as a third party. Twenty-four hours later, nonadherent cells were harvested and depleted of CD106+ cells to exclude the interference of any residual MSCs. The CD106−/nonadherent C6 cells were restimulated with the HY peptide without MSCs. IFN-γ–producing CD8+ T cells were enumerated 24 hours later. The results are shown in Figure 7. Although the presence of MSCs in the first 24-hour culture inhibited the first antigenic stimulation, when MSCs were removed the response to the HY peptide was restored. These findings demonstrate that MSCs inhibit T cells only when they are present in culture, but the effect is reversed when MSCs are removed.
The MSC inhibitory effect is transient.
(A) Spleen cells from C6 transgenic (naive) mice were stimulated for 24 hours with HY KkSmcy(TENSGKDI) peptide-pulsed APCs (▪). Cells were then harvested, washed, and restimulated with the same peptide for an additional 24 hours (■). (B) The same responder cells (C6 transgenic) were stimulated for 24 hours with HY KkSmcypeptide-pulsed APCs in the presence of MSCs (MSC/R ratio = 1:10; ▪). Cells were then harvested, depleted of MSCs by CD106 antibodies and Dynabeads before restimulation with the same peptide (■). The y-axis reports the percentage of IFN-γ–producing CD8+ T cells. The results reported are the average of 3 experiments of identical design. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures containing MSCs (panel A, ▪) in all experiments. The comparison between the restimulation of C6 cells with HY KkSmcy peptide (■) previously stimulated with the same peptide in the presence (B) or absence (A) of MSCs was not statistically significant. The bars show the SD.
The MSC inhibitory effect is transient.
(A) Spleen cells from C6 transgenic (naive) mice were stimulated for 24 hours with HY KkSmcy(TENSGKDI) peptide-pulsed APCs (▪). Cells were then harvested, washed, and restimulated with the same peptide for an additional 24 hours (■). (B) The same responder cells (C6 transgenic) were stimulated for 24 hours with HY KkSmcypeptide-pulsed APCs in the presence of MSCs (MSC/R ratio = 1:10; ▪). Cells were then harvested, depleted of MSCs by CD106 antibodies and Dynabeads before restimulation with the same peptide (■). The y-axis reports the percentage of IFN-γ–producing CD8+ T cells. The results reported are the average of 3 experiments of identical design. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures containing MSCs (panel A, ▪) in all experiments. The comparison between the restimulation of C6 cells with HY KkSmcy peptide (■) previously stimulated with the same peptide in the presence (B) or absence (A) of MSCs was not statistically significant. The bars show the SD.
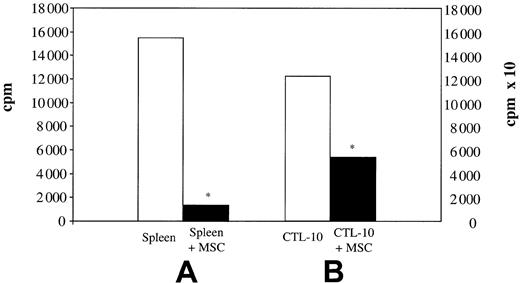
MSC inhibitory effect requires cell contact
The MSC inhibitory effect could be mediated by soluble factors or could require cell contact to be exerted. The fact that the inhibitory activity was dose-dependent and transient (ie, entirely dependent on the presence of MSCs) was in support of the latter hypothesis. MSC culture supernatant was added (1:1 dilution) to the cultures in which memory HY-specific T cells were stimulated with syngeneic male spleen cells. After 7 days the numbers of HY DbSmcytetramer-positive CD8+ T cells were evaluated. In parallel, cells were stimulated with HY peptide–pulsed APCs for 6 hours to assess the numbers of IFN-γ+/CD8+ T cells. The results are reported in Figure 8. No difference in the number of tetramer-positive T cells was detected (Figure 8A) and the number of IFN-γ+/CD8+ T cells was not reduced in the presence of MSC supernatant (Figure 8B). The necessity of cell contact for the inhibitory effect was confirmed by experiments in a Transwell system. MSCs were added to the inner chamber and the MLR was cultivated separately in the lower chamber. When the MSCs were not in contact with the MLR, the inhibition of antigen-specific T cells was much reduced (Figure 8A-B). Consistent with a need for cell-cell contact and the absence of an effect of soluble factors, we did not find any interleukin 10 (IL-10) in the MSC culture supernatant as evaluated by enzyme-linked immunosorbent assay (ELISA); further, addition of anti-TGFβ–blocking antibody had no influence on inhibitory activity even when used at concentrations 10-fold higher (10 μg/mL) than those described by others13 (data not shown).
The inhibitory effect of MSCs requires cell contact.
HY-specific memory T cells from immunized B6 females were stimulated in vitro with syngeneic male spleen cells (B6) in the presence of MSCs (B6 + MSC) or supernatant from MSC cultures (B6 + MSC-SN). In parallel, responder T cells were also stimulated with syngeneic male spleen cells in the presence of MSCs in a Transwell system (B6 + MSC-T/W). The percentage of HYDbSmcy and HYDbUty tetramer-positive CD8+ T cells (A) and HY-specific IFN-γ+ CD8+ T cells (B) are shown for each culture. The results reported are the average of 4 identical experiments. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures (B6).
The inhibitory effect of MSCs requires cell contact.
HY-specific memory T cells from immunized B6 females were stimulated in vitro with syngeneic male spleen cells (B6) in the presence of MSCs (B6 + MSC) or supernatant from MSC cultures (B6 + MSC-SN). In parallel, responder T cells were also stimulated with syngeneic male spleen cells in the presence of MSCs in a Transwell system (B6 + MSC-T/W). The percentage of HYDbSmcy and HYDbUty tetramer-positive CD8+ T cells (A) and HY-specific IFN-γ+ CD8+ T cells (B) are shown for each culture. The results reported are the average of 4 identical experiments. The bars show the SD. * indicates statistically significant (at least P < .01) versus control cultures (B6).
MSC inhibitory effect is neither dependent on APCs nor on CD4+/CD25+ regulatory T cells
The MSC inhibitory effect could be exerted directly on effector T cells or mediated via different splenocyte types present in culture. To address this question, we asked whether APCs were required for the inhibitory effect to be exerted. We stimulated T-cell proliferation with CD3/CD28-coated beads. This type of stimulation circumvents the need for APCs because antibodies interact directly with T cells to activate them. When MSCs were added to the cultures they potently inhibited spleen cell proliferation in response to the antibody-coated beads (Figure 9A). The results were confirmed using an HY DbUty-specific CD8+ T-cell clone (CTL-10)25 as responder cells (Figure 9B).
MSC inhibitory effect does not require APCs.
Proliferative response of B6 splenocytes (A) or HY-specific T-cell clone CTL-1025 (B) to CD3/CD28-coated beads in the presence or absence of MSCs. One representative experiment is shown of 3 performed. The background counts for unstimulated spleen and T-cell clone were less than 1% and less than 5%, respectively. The scale of the y-axis on the left and on the right is different. Asterisk indicates statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
MSC inhibitory effect does not require APCs.
Proliferative response of B6 splenocytes (A) or HY-specific T-cell clone CTL-1025 (B) to CD3/CD28-coated beads in the presence or absence of MSCs. One representative experiment is shown of 3 performed. The background counts for unstimulated spleen and T-cell clone were less than 1% and less than 5%, respectively. The scale of the y-axis on the left and on the right is different. Asterisk indicates statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
Alternatively, MSCs might exert their inhibitory effect via regulatory T cells. Much attention has recently been paid to a distinct CD4+ T-cell subset expressing the CD25 molecule, which appears to actively suppress T-cell activation.26 To ascertain whether CD4+/CD25+ regulatory T cells are required for the MSC-mediated inhibition, spleen cells from C6 mice were depleted of CD25+ cells and stimulated with H2k-restricted HY peptide-pulsed (HY KkSmcy) female spleen cells in the presence or absence of MSCs and 24 hours later assessed for the number of HY peptide–specific IFN-γ+ CD8+ cells. CD25-depleted and CD25-replete C6 T cells were equally inhibited by MSC (50% versus 44%, not statistically significant; Figure10).
MSC inhibitory effect does not require CD4+/CD25+ regulatory T cells.
CD25-depleted or CD25-replete C6 splenocytes (5 × 106) were stimulated in vitro with HY KkSmcy peptide pulsed female cells in the presence or absence of MSC (105). After 24 hours HY-specific IFN-γ+CD8+ T cells were enumerated. MSC inhibition on CD25− responders was 50% as compared to 44% in the control CD25-replete cultures (not statistically significant). The bars show the SD.
MSC inhibitory effect does not require CD4+/CD25+ regulatory T cells.
CD25-depleted or CD25-replete C6 splenocytes (5 × 106) were stimulated in vitro with HY KkSmcy peptide pulsed female cells in the presence or absence of MSC (105). After 24 hours HY-specific IFN-γ+CD8+ T cells were enumerated. MSC inhibition on CD25− responders was 50% as compared to 44% in the control CD25-replete cultures (not statistically significant). The bars show the SD.
Discussion
Transplantation has been one of the major advances in medicine during the last few decades. BM transplantation, in particular, can cure a variety of malignancies by exploiting the graft-versus-tumor effect exerted by the lymphocytes contained in the donor BM preparation. Major problems remain with the lack of suitable BM donors. The option of increasing donor-recipient histoincompatibility is associated with a high risk of both graft rejection or graft-versus-host disease (GVHD), a situation in which more powerful and selective strategies to diminish immune responses following transplantation would be desirable. There has recently been enormous interest in the stem cells contained in the BM because it appears that they can differentiate into lineages other than hematopoietic.27-32 BM also contains rare stem cells that differentiate into mesenchymal lineage cells that not only have multipotential differentiation ability33 but also appear to modulate immune responses in vitro. This property could have a substantial impact in transplantation because infusion of MSCs in conjunction with the donor organ or BM might favor engraftment. Administration of MSCs has been reported to prolong donor skin graft survival in nonhuman primates.14 The ability of MSCs to suppress immune responses could also be harnessed to reduce GVHD, the idea underlying a multicentric clinical trial in which patients with advanced hematologic malignancies receive donor MSCs at the time of hemopoietic stem cell infusion as a prophylaxis for GVHD. So far, the reported overall incidence of acute and chronic GVHD appears to be significantly lower in the group infused with MSCs as compared to the controls (P = .002 and P = .02, respectively).34 However, the characteristics and the mechanisms of this inhibition are entirely unknown.
Here we show that BM-derived MSCs have a profound inhibitory effect on activation of T cells by their cognate peptides in vitro. This inhibition, which affects both naive and memory T cells, is manifest in antigen-specific proliferation, IFN-γ production, and cytotoxic activity. Physiologic inhibition of T cells is considered to occur by deletion, anergy, or suppression.35 Whereas in the first case T cells die, in the other situations T cells remain alive but are unable to respond to antigen. Here we show that the inhibitory effect exerted by MSCs on naive T cells is already detectable at 24 hours, but it is relieved once MSCs are removed from the culture, so they are not deleted (Figure 7). However, in the cultures in which MSCs are incubated with memory T cells for 7 days, which are then harvested and restimulated with antigen, T cells remain unable to respond (Figure 4). In the case of naive antigen-reactive T cells, which recover responsiveness when separated after 24 hours with MSCs, it seems unlikely that their nonresponsiveness in the continued presence of MSCs is due to anergy, because 24 hours is a reasonable time frame for anergy induction.36 The alternative hypotheses are that MSCs induce T-cell suppression either directly by soluble factors or indirectly by preventing T-cell activation. The requirement of cell contact for MSCs to display their inhibition suggests they may operate by preventing T-cell activation. The absence of IL-10 in MSC culture supernatants and the inability of anti-TGFβ–blocking antibodies to inhibit the MSC effect (data not shown) are in accord with such a hypothesis. It is not yet clear whether naive are more difficult to anergize than memory T cells.15 Although the inhibition of IFN-γ production seems more pronounced on memory T cells than in naive T cells, the precursor frequency of responder T cells differs in the 2 populations. At the time of culture with MSCs the numbers of antigen-specific T cells were higher in the naive transgenic splenocytes than in the memory HY-primed splenocytes. The proportion of HY-specific T cells in spleens of immunized female mice is 10%16 compared with more than 90% in naive C6 transgenic mice.18
A crucial question is whether the inhibitory effect depends on the presence of cognate antigen. The evidence that MSCs do not require MHC molecules to inhibit T-cell responses (Figure 6) strongly argues against a cognate mechanism but does not rule out the possibility that MSCs inhibit specifically the cells that are activated by interaction with antigen. However, it is the ratio between MSCs and total T cells rather than with antigen-specific T cells that influences the inhibition (Figure 5). These results favor the notion that MSCs do not specifically target T cells that encounter antigen. Because neither APCs (Figure 9) nor CD4+/CD25+ regulatory T cells (Figure 10) are required for the inhibition to occur, overall our data suggest that MSCs physically hinder T cells from the contact with APCs in a noncognate fashion.
Two papers have recently reported that MSCs inhibit T-cell proliferation induced by nonspecific mitogens or in polyclonal, polyepitope MLRs.13,14 Ours is the first demonstration of the inhibitory effect of MSCs on T-cell response to cognate peptide. It is noteworthy that our findings differ from those reported by Di Nicola et al13 because in their work the effect of MSCs appears to be mediated by soluble factors, and in particular by TGF-β or hematopoietic growth factor (HGF) or both, and does not require cell contact. Although this discrepancy might merely be explained by the fact that experiments were carried out in different species, our MSCs have been generated in a different way. It is possible that BM stromal cells are different from MSCs in this respect. These differences may also explain the much higher inhibitory efficiency of our MSCs, an effect is clearly visible when the ratio between MSCs and responder T cells is as low as 1:103 as compared to ratio of 1:1 required to see an effect with stromal cells of Di Nicola et al. However, it is possible that soluble factors may have a small role also in our system (Figure 8).
Regardless of the mechanisms underlying the MSC inhibitory effect, the physiologic role of this is unclear. It is well known that mesenchymal elements play a major role in T-cell ontogeny in the thymus. Because we observed that cell contact is required, MSCs might provide a niche in the BM in which lymphocytes are suppressed or deleted. However, the effect of MSCs may not be specific to the immune system but have a more general “inhibitory” activity on protein synthesis or the cell cycle in a variety of cell types.
Our findings clearly have possible therapeutic implications. Because of their differentiation ability and susceptibility to stable gene transduction, MSCs represent an attractive target to develop gene therapy. The evidence that MSCs do not present alloantigen and that they do not require MHC expression to exert their inhibitory effect suggests that they can be derived from a donor irrespective of their MHC haplotype and prepared as an “off-the-shelf” reagent for any patient. Here we show that MSCs have a profound inhibitory effect on T-cell responses to transplantation antigens and may thus be used to control host-versus-graft (HvG) and GVHD, especially in those situations in which BM transplantation is performed following reduced intensity conditioning. More importantly, we have demonstrated that not only naive but also antigen-experienced (memory) T cells can be inhibited. The current ongoing clinical trials involve the infusion of MSCs at the time of BM transplantation.34 When this procedure is used for patients with leukemia, it is possible that the inhibitory effect may also jeopardize the graft-versus-leukemia effect, which is crucial for a successful outcome. This potential complication needs to be considered against the probability that, according to our data, MSCs have the potential ability to inhibit even ongoing GVHD.
Prepublished online as Blood First Edition Paper, December 27, 2002; DOI 10.1182/blood-2002-07-2104.
Supported by the Leukaemia Research Fund. M.K. was recipient of an AIRC-FIRC (Associazione Italiana Ricerca Cancro-Federazione Italiana Ricerca Cancro) Fellowship (“L Fontana e M Lionello”).
M.K. and S.G. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Francesco Dazzi, Department of Immunology, Imperial College Faculty of Medicine, Hammersmith Hospital, Du Cane Rd, London W12 0NN, United Kingdom; e-mail:f.dazzi@ic.ac.uk.


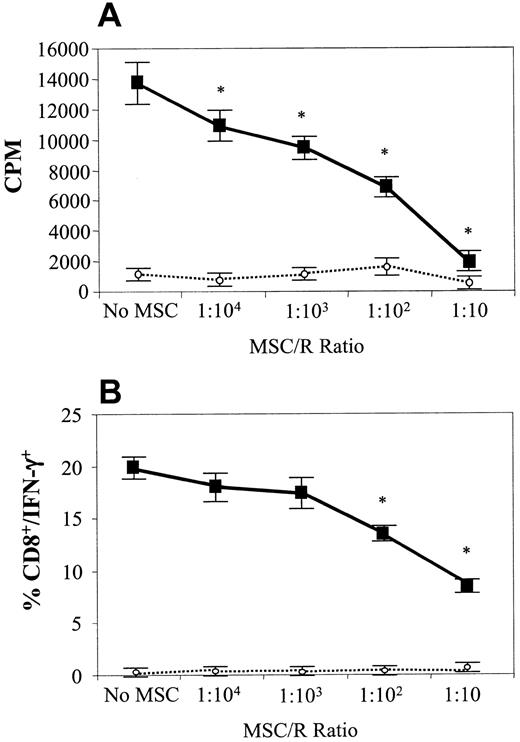








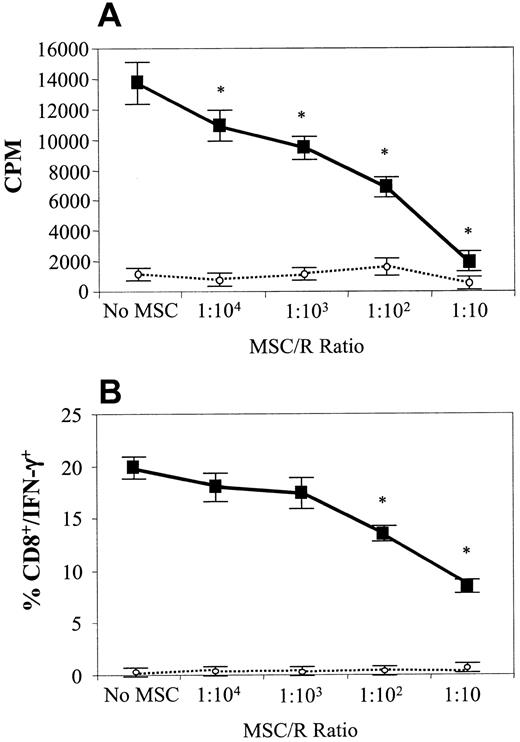
 ) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.
) of the HY peptide. The results reported are the average of 3 experiments of identical design. T-cell proliferation cultures were performed in triplicate and results averaged. The bars show the SD. MSC/R indicates MSC-to-responder T cells ratio. Asterisk signifies statistically significant (at least P < .01) versus control cultures without MSCs in all experiments.