Given their abundance and importance in thrombosis and hemostasis, platelets have been the target of intense scientific inquisition for decades. While the study of physiologic platelet functions such as aggregation and granule secretion have been well characterized, platelets remain a difficult target of study from the perspective of signal transduction. Nucleated cells can be genetically manipulated via a variety of rapid techniques to map out detailed signaling pathways, whereas the study of platelet signaling has largely been limited to the use of soluble agonists or inhibitors, knockout mice, or platelet precursor cells such as megakaryocytes. Although these techniques have provided invaluable insights into platelet signaling pathways, they are hindered by issues of specificity and/or time.
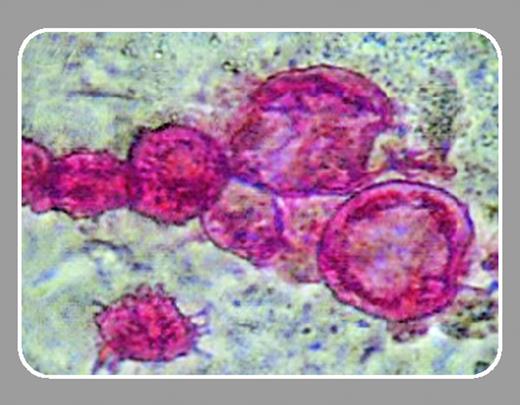
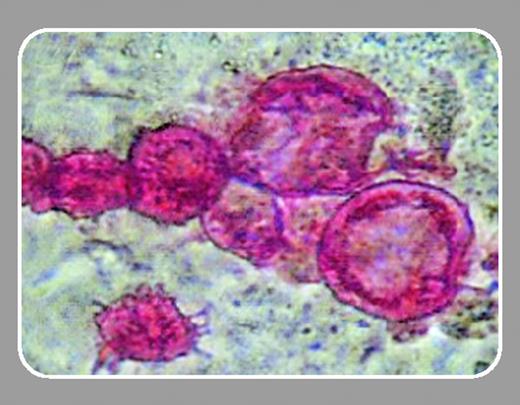
In this issue of Blood, Fujimoto and colleagues (page 4044) describe a detailed and efficient technique by which functional platelets derived from embryonic stem (ES) cells can be genetically transfected. Recent studies have shown that the nucleated megakaryocytes can be manipulated by viral infection1 or by RNA interference.2 Additionally, physiologically active platelets can be produced from megakaryocytes in vitro.3 However, Fujimoto and colleagues bring together the concepts of exogenous gene expression in megakaryocytes and platelet differentiation. The authors first confirmed the presence of functional platelets from their differentiated megakaryocyte cultures through both subcellular imaging and agonist-induced fluorescent fibrinogen binding. Next, they transfected the differentiated megakaryocytes with either green fluorescent protein (GFP) or a β3 integrin construct (Tac-β3) that has been shown in nonplatelet systems to inhibit agonist-induced αIIbβ3 activation. The transfections were demonstrated to carry over from the megakaryocytes to the platelets, since GFP-transfected megakaryocytes produced GFP-positive platelets, and Tac-β3–transfected megakaryocytes produced platelets that were significantly impaired in their ability to bind fibrinogen in response to protease-activated receptor 4 (PAR4)–activating peptide.
Along with demonstrating the ability to “transfect” platelets, another important feature of this study is the utility it provides for other platelet researchers. In addition to employing a system using cultured and renewable ES cells, the authors show that this system can generate levels of platelets that are comparable to platelet numbers obtained from murine blood (1 × 104 ES cells yielding up to 1.8 × 108 platelets). The article also goes into great detail to document the processes of megakaryocyte differentiation and platelet production, demonstrating the transition of ES cells to undefined colonies of cells to individual megakaryocytes positive for αIIb, and finally the presence of proplatelet structures leading to platelet release. This flow chart of cellular maturation is a useful tool for interpreting the results from a culture that contains a heterogeneous mix of cells types that are constantly changing. Studies such as these should pave the way for further exploration of intracellular platelet processes by allowing for rapid platelet production and manipulation. As the authors also point out, platelets produced similarly with human ES cells may provide a therapeutic benefit for patients with platelet disorders.