HEMOSTASIS, THROMBOSIS, AND VASCULAR BIOLOGY
Current beliefs are that familial thrombotic thrombocytopenic purpura (TTP) is caused by mutations of the ADAMTS13 gene and that acquired TTP is caused by autoantibodies that inhibit ADAMTS13 activity. These concepts are consistent with observations on treatment: familial TTP can be effectively treated by plasma infusion to replace ADAMTS13, whereas plasma exchange, presumably performed to remove inhibitory autoantibodies in addition to replacement of ADAMTS13, is more effective treatment for acquired TTP. These observations provide a logical explanation for (1) how TTP occurs in relation to accumulation of unusually large multimers of von Willebrand factor (VWF), and (2) how the treatment works. This is a wonderful example of translational research. However, translation inevitably becomes less clear as more carefully designed clinical observations are reported. Nature speaks many languages with many nuances, subtleties, and surprises.
For example, our assumption about familial TTP is adjusted by the stunning case reports of identical twin sisters who developed TTP at ages 23 years and 24 years by Studt and colleagues (page 4195). Although both sisters had absent ADAMTS13 activity, the presence of immunoglobulin G (IgG) antibodies that inactivated ADAMTS13 and the eventual recovery of normal ADAMTS13 levels demonstrated that the TTP was acquired rather than due to an abnormality of the ADAMTS13 gene. However, ADAMTS13 levels remained undetectable with persistent inhibitors 5 to 17 months after complete hematologic recovery, demonstrating that severe ADAMTS13 deficiency is not always sufficient to cause TTP.
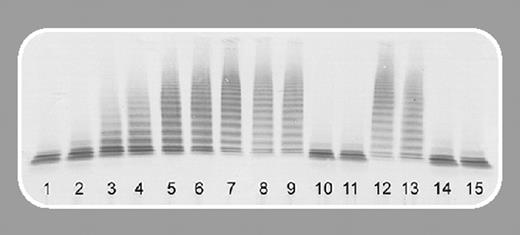
Another report in this issue by Zheng and colleagues (page 4043) describes 37 consecutive patients with clinically diagnosed TTP. Of 20 patients who had idiopathic TTP, 16 (80%) had severe ADAMTS13 deficiency, 7 had a demonstrable inhibitor of ADAMTS13 activity, and in 4 patients a high titer of inhibitor predicted a prolonged and severe clinical course. Zheng and colleagues also observed that clinical remissions may occur in spite of continued severe ADAMTS13 deficiency and persistent inhibitor activity.
How can clinicians use this information? Several issues prevent immediate integration of ADAMTS13 assays into routine patient care. Patients with typical TTP may not have severe ADAMTS13 deficiency; therefore, the diagnostic sensitivity of ADAMTS13 deficiency is uncertain. TTP, similar to other thrombotic disorders, may result from multiple risk factors, such as pregnancy, factor V Leiden,1 obesity, and African American background,2 in addition to ADAMTS13 deficiency. Furthermore, ADAMTS13 assays are not readily available and their interpretation may often be affected by previous transfusions.
If we learn that one of our patients has severe ADAMTS13 deficiency with a high titer of inhibitory activity, should this influence our management? Zheng and colleagues' observations can support decisions to add immunosuppressive agents to plasma exchange treatment for these patients and escalate immunosuppressive intensity if they do not recover promptly. However, the relation between inhibitor titers and response to plasma exchange is imperfect: patients with strong inhibitors may respond promptly and completely to plasma exchange; others without a demonstrable inhibitor may have a prolonged course.2
If we learn that one of our patients has persistent severe ADAMTS13 deficiency while in clinical remission, what should we do? An ominous observation is the description of patients who have recovered from TTP and later had stroke symptoms without thrombocytopenia or anemia.3,4 In these reports, the documentation of severe ADAMTS13 deficiency and inhibitor activity suggested that TTP was the etiology of the stroke symptoms and the patients responded to rituximab or plasma exchange. However, there is no current role for “maintenance” or “prophylactic” treatment. These observations make the clinical diagnosis of TTP, already often uncertain, even more difficult.
And if we learn that one of our patients with a clinical diagnosis of TTP does not have severe ADAMTS13 deficiency, should this influence our management? Can plasma exchange, with its high risk of complications,5 be avoided? Not now. Plasma exchange appears to be effective in some patients without severe ADAMTS13 deficiency.2 Although the rationale for plasma exchange in patients with ADAMTS13 may be clear, the observations of recovery even while severe ADAMTS13 deficiency persists suggest that there are additional reasons why plasma exchange works.
The story of ADAMTS13 is a great milestone in our understanding of TTP. There will be more milestones.