Atherosclerosis is an inflammatory disease of the arterial wall that carries an important socioeconomic burden. The severe clinical manifestations of atherosclerosis (myocardial infarction, stroke) are mainly due to the abrupt obstruction of the vessel lumen by a thrombus formed on the contact of a ruptured or eroded atherosclerotic plaque. The available data strongly suggest that immunoinflammatory–related mechanisms are the major determinants of plaque complications. Therefore, most of the important advances in the comprehension of the mechanisms of atherosclerosis have come from studies aimed at elucidating the critical components involved in the modulation of the immunoinflammatory balance within the plaque. However, despite the increasing knowledge regarding the role of inflammation in atherogenesis, the precise intracellular transduction pathways involved in this process remain largely unexplored.
Recent studies have pointed to the transcription factor nuclear factor κB (NF-κB) as potentially one of the most important proinflammatory pathways in atherogenesis. Various risk factors for atherosclerosis, including hypercholesterolemia, diabetes and its associated advanced glycation end products, hypertension, elevated plasma homocysteine levels, and increased oxidative stress, which is common to all the preceding conditions, are important activators of NF-κB. Activated NF-κB has been identified in smooth muscle cells, macrophages, and endothelial cells of human atherosclerotic lesions,1 and enhanced activation of this transcription factor has been shown to occur very early following a high-fat, cholatefree diet in low-density lipoprotein receptor (LDLR)–deficient mice.2 However, apart from significant positive correlations between activated NF-κB and proatherogenic activity, the direct role of NF-κB in the development and composition of atherosclerotic plaques had not yet been assessed.
In a recent study, Kanters et al, using LDLR-deficient mice with a macrophage-restricted deletion of IκB kinase 2 (IKK2) leading to specific inhibition of NF-κB activation in macrophages, reported the unexpected finding of increased atherosclerotic lesion formation and inflammation.3 This result was associated with a significant reduction in the anti-inflammatory and antiatherogenic cytokine interleukin-10 (IL-10), suggesting that a certain level of NF-κB activation was required for the control of the inflammatory reaction and the protection against unabated inflammatory and proatherogenic responses. This is in agreement with studies showing a central role for NF-κB in the induction of “protective” anti-apoptotic and anti-inflammatory genes, critical to the resolution of the inflammatory process.4
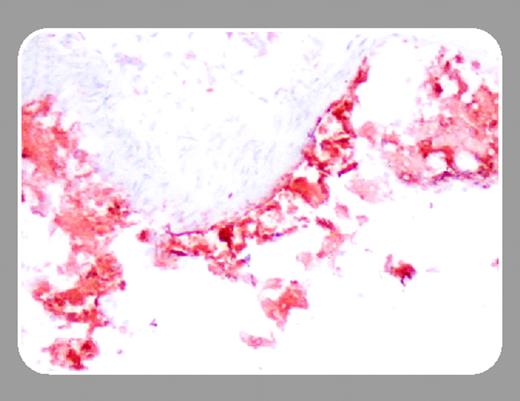
However, according to the study by Kanters and colleagues in this issue of Blood (page 934), the detrimental effect of NF-κB inhibition in atherogenesis depends on how NF-κB activity is inhibited. In this study, Kanters et al examined the effects of hematopoietic NF-κB1 (p50) deficiency in the development of atherosclerotic lesions in LDLR knockout mice. Instead of promoting the formation of larger inflammatory lesions, as was the case with IKK2 deficiency, a significant decrease in lesion size in mice with NF-κB1 deficiency, despite enhanced accumulation of T and B lymphocytes within the lesions, was observed. This could be explained, at least in part, by the observation that, in contrast to IKK2 deficiency, NF-κB1 deficiency did not lead to an alteration of the inflammatory balance in favor of a proatherogenic phenotype. Despite increased tumor necrosis factor (TNF) expression by NF-κB1–/– macrophages, other major proatherogenic molecules such as monocyte chemoattractant protein-1 (MCP-1) were down-regulated, whereas critical antiatherogenic factors such as IL-10 were significantly up-regulated. Decreased MCP-1 production and increased IL-10 expression may have contributed to limitation of plaque size despite enhanced accumulation of T cells. Another plausible mechanism leading to inhibition of lesion development in NF-κB1–deficient animals could be attributed to a potential defect in the uptake of oxidized low-density lipoprotein (oxLDL) by macrophages, as characteristic foam cells were absent in NF-κB1–/– lesions and both scavenger receptor class A (SR-A) expression and uptake of oxLDL were significantly reduced in NF-κB1–/– macrophages upon ex vivo stimulation with lipopolysaccharide (LPS). Whether this in vitro effect, observed following LPS stimulation, is relevant to the in vivo situation remains to be determined.
NF-κB appears to be at the crossroads of the inflammatory response in atherosclerosis, fine-tuning the response of the vessel wall to injury. Kanters et al should be commended for these provocative studies on the role of NF-κB, one of the most important proinflammatory transcription factors, in atherosclerosis.