Abstract
While studying the unique Nramp1 (Slc11a1)–independent susceptibility to Mycobacterium bovis (BCG) infection of BXH-2 mice, we noted that these mice develop important splenomegaly and enlargement of lymph nodes. Segregation analyses in several F2 crosses showed that splenomegaly segregates as a single recessive trait caused by a novel mutation in BXH-2, independent of the infection. Histologic and fluorescence-activated cell sorter (FACS) analyses indicated that splenomegaly is associated with a large increase in Mac1+/GR1+ (macrophage antigen-1+/granulocyte differentiation antigen 1+) granulocyte precursors in spleen, lymph nodes, and bone marrow, resembling a myeloproliferative syndrome. This is concomitant to extramedullary erythropoiesis in the spleen, as measured by proportion of Ter119+ erythroid cells. The locus controlling this myeloproliferative syndrome and splenomegaly was designated Myls and maps to an 18 centimorgan (cM) region of chromosome 8, which also contains an integrated copy of an N-ecotropic murine leukemia virus (MuLV) provirus (Emv2). The relationship between Myls, expansion of Mac1+/GR1+ cells, and Emv2 was investigated. Homozygosity at Myls is necessary but not sufficient for B-ecotropic virus replication in splenocytes, the extent of which appears to be under separate genetic control. Our results suggest a model in which Myls-dependent myeloproliferation in BXH-2 acts as a predisposing factor for the subsequent development of virally induced myeloid leukemia characteristic of this strain.
Introduction
Natural resistance of mice to Mycobacterium bovis, Salmonella typhimurium, and Leishmania donovani is regulated by Nramp1/Slc11a1 gene on chromosome 1.1-5 Nramp1 is a membrane phosphoglycoprotein formed of 12 transmembrane domains expressed exclusively in mononuclear phagocytes and in neutrophils6,7 and functions as a pH-dependent divalent cation (Mn2+, Fe2+) efflux pump at the phagosomal membrane.8 Studies in vitro and ex vivo showed that Nramp1 protein affects the ability of the macrophage and neutrophils to restrict intracellular replication of phylogenically unrelated intracellular parasites9 by restricting the availability of nutritional metals to bacteria and parasites contained in lysosomes and tertiary granules.8 This activity antagonizes the ability of intracellular parasites to express key survival determinants such as modulation of phagosome maturation.10,11 In inbred mouse strains, susceptibility to infection is caused by a Gly-to-Asp substitution (G169D) in predicted transmembrane domain 4 (TM4),12 which prevents proper maturation or membrane integration of the protein.13
BXH-2 is a recombinant inbred strain derived from an F2 cross of C57BL/6J (Nramp1D169) and C3H/HeJ (Nramp1G169) parental strains.1,3,14 Despite being homozygous for the resistance allele (Nramp1G169), BXH-2 mice are susceptible to M bovis (BCG; Bacille Calmette-Guérin) infection in vivo (log10BCG = 5.90 ± 0.5), although they appear resistant to infection with S typhimurium and L donovani.3 In addition, crossing BXH-2 mice (Nramp1G169) to C57BL/6J (Nramp1D169) mice produces F1 animals that are uniformly resistant to M bovis (BCG) infection (Nramp1D169/G169; log10BCG = 3.55 ± 0.24), thus clearly indicating that phenotypic susceptibility to infection in BXH-2 is caused by a factor that overrides the resistance conveyed by their functional Nramp1G169 allele. BXH-2 mice are also known to express high levels of a B-ecotropic murine leukemia virus throughout life and show a high incidence of virally induced myeloid leukemia.15-17 Leukemia in these mice is caused by retroviral insertional mutagenesis whereby the virus expressed in these mice infects hematopoietic cells and occasionally deregulates the expression of a cellular protooncogene or inactivates the expression of a tumor suppressor gene and thereby induces a tumor.18
During an investigation of the seemingly Nramp1-independent susceptibility to M bovis (BCG) infection in BXH-2, we failed to identify modifier genes of Nramp1. However, we noted that approximately 25% of the F2 mice develop important splenomegaly and enlargement of lymph nodes, even in control experiments without M bovis (BCG) infection. Here, we present evidence that the splenomegaly phenotype is under the control of a single locus on chromosome 8–designated Myls. This locus appears to control the appearance of a myeloproliferative syndrome characterized by expansion of the Mac1+/GR1+ (macrophage antigen-1+/granulocyte differentiation antigen 1+) myeloid compartment in spleen, lymph nodes, and bone marrow. The presence of this myeloproliferative syndrome appeared to have no effect on susceptibility to M bovis (BCG) infection. The relationship between Myls, the expansion of the myeloid compartment, and the expression of the B-ecotropic murine leukemia virus (MuLV) was further investigated.
Materials and methods
Animals
Inbred C57BL/6J, BALB/cJ, C3H/HeJ, and A/J mice were purchased from The Jackson Laboratory (Bar Harbor, ME). Recombinant inbred BXH-2 male mice were originally obtained from the Jackson Laboratory (as single male animals in the mid-1990s) and were used to generate F2 crosses to BALB/cJ, C57BL/6J, and A/J that were phenotyped for susceptibility to Mycobacterium bovis (BCG) infection. F2 progeny were produced by systemic brother-sister mating and were used between 2 and 6 months of age. A second BXH-2 stock from the National Cancer Institute (NCI; Frederick, MD) was used to generate additional F2 crosses for linkage mapping studies in 2001.
Infection with Mycobacterium bovis (BCG)
Mycobacterium bovis (BCG, strain Montreal) was prepared for in vivo infections, as previously described,2 and 2 × 104 colony-forming units (CFUs) were used to inoculate mice (2 to 3 months of age) by the intravenous route. Twenty-one days after infection, mice were killed, weighed, and the degree of infection was assessed by the determination of spleen CFUs. The index of BCG infection was defined as the logarithm of the mean number of viable BCG recovered from spleens. The spleen index (SI) was determined as the root square of spleen weight (× 100) divided by the body weight.19
Genotyping
Genomic DNA was prepared from tail biopsies as previously described.20 Microsatellite markers (total of 193, approximate 10 centimorgan [cM] genome coverage) informative for BALB/cJ and either C57BL/6J or C3H/HeJ parents of BXH-2 (www.genome.wi.mit.edu/cgi-bin/mouse/index) were purchased from Research Genetics (Huntsville, AL). Genotyping was performed by standard polymerase chain reaction (PCR)–based method using trace amount of [32P]α–deoxy adenosine triphosphate (dATP), followed by separation on denaturing polyacrylamide gels. Some markers were genotyped using primer pairs fluorescently labeled by Applied Biosystems (Foster City, CA). Products were analyzed by capillary separation using an ABI prism 3700 automated DNA sequencer (Applied Biosystems). Data were collected and analyzed using the GeneScan 3.5 software package and were visualized using Genotyper 3.6 software (Applied Biosystems).
Statistical analysis
Linkage between genotypes at individual markers and SI was tested, and identification of21 quantitative trait loci (QTLs) was performed using Map Manager QT. This is an interval mapping method for the identification of loci affecting a quantitative trait based on multiple regression.22,23 Logarithm of odds (LODs) scores were calculated as χ2/2ln(10) with χ2 values computed using the expectation/maximization algorithm in Map Manager QT (Roswell Park Cancer Institute; http://www.mapmanager.org).
Histology
Spleen, lymph nodes (mesenteric, axillary), liver, thymus, lung, kidney, and femur were harvested from (A/J × BXH-2)F2 mice and from BXH-2, B6, and A/J parental controls of at least 3 months of age. Tissues were fixed in Bouin solution (picric acid 9 g/L, acetic acid 4%, and formaldehyde 4%, methanol 4%). Five-micrometer paraffin-embedded sections were stained with hematoxylin and eosin and photographed at × 40, × 400, and × 1000 original magnification (Figure 5). Blood smears were fixed and stained with Diff-Quik Stain Set (Dade Behring, Düdingen, Switzerland). A complete analysis of hematologic parameters in peripheral blood (erythrocyte count, white blood cell count, hemoglobin, hematocrit, platelets, MCV [mean corpuscular volume], MCH [mean concentration of hematocrit], MCHC [mean cellular hemoglobin concentration]) was also conducted (Diagnostic and Research Support Service, Animal Resources Centre, McGill University, Montreal, QC, Canada).
Histologic analysis of target tissues from mice segregating the splenomegaly phenotype. Spleen (S) (R indicates red pulp; W, white pulp), bone marrow (BM) and lymph nodes (LN) from (BALB/cJ × BXH-2)F2 mice showing presence (high SI) or absence (low SI) of splenomegaly were harvested, fixed, sectioned, and stained with hematoxylin and eosin. Original magnification was × 40 (M,O), × 400 (A,C,E,G,I,K), and × 1000 (B,D,F,H,J,L,N,P). Important infiltration of cells with neutrophil-like appearance with “ring” nuclei is seen in red pulp of the spleen, bone marrow, and in enlarged lymph nodes of F2 mice showing splenomegaly.
Histologic analysis of target tissues from mice segregating the splenomegaly phenotype. Spleen (S) (R indicates red pulp; W, white pulp), bone marrow (BM) and lymph nodes (LN) from (BALB/cJ × BXH-2)F2 mice showing presence (high SI) or absence (low SI) of splenomegaly were harvested, fixed, sectioned, and stained with hematoxylin and eosin. Original magnification was × 40 (M,O), × 400 (A,C,E,G,I,K), and × 1000 (B,D,F,H,J,L,N,P). Important infiltration of cells with neutrophil-like appearance with “ring” nuclei is seen in red pulp of the spleen, bone marrow, and in enlarged lymph nodes of F2 mice showing splenomegaly.
Flow cytometry
The preparation of single cell suspensions from spleen, lymph nodes, and bone marrow as well as their analysis by flow cytometry was as previously described.24 Briefly, splenocytes as well as single cell suspensions from lymph nodes and bone marrow were washed with phosphate-buffered saline (PBS) containing 1% heat inactivated fetal bovine serum (FBS). Nonspecific binding was blocked using a blocking buffer containing 20% heat-inactivated FBS and 1 × PBS. Flow cytometry was performed using antibodies against various mouse cell surface markers: CD4, CD8, Thy1.2, and T-cell–receptor αβ (TcRαβ; T lymphocytes), B220 (B lymphocytes), Mac1 (macrophages, natural killer [NK] cells, granulocytes), GR1 (granulocytes), Ter 119 (erythroid cells), and CD11c (dendritic cells). CD4, CD8, Thy1.2, TcRαβ, B220, Mac1, GR1, and Ter 119 were all coupled to specific fluorophors and were purchased from Cedarlane (Hornby, ON, Canada). CD11c was from Pharmingen (San Diego, CA). Immunostaining was performed on ice using saturating amounts of monoclonal antibodies. Propidium iodide (Sigma, St Louis, MO) was used at a concentration of 0.625 μg/mL. Data were collected and analyzed using the FACScan flow cytometer and Cellquest software (Becton Dickinson, San Jose, CA).
XC plaque assay
To assess the presence of a B-ecotropic virus in spleens from A/J, BXH-2, F1, and F2 progenies, an XC plaque assay was used.16,25 Single cell suspensions were resuspended in Dulbecco modified Eagle minimal essential medium (DMEM) containing 10% calf serum and then treated with mitomycin C (25 μg/3 mL cell suspension; Sigma-Aldrich, Oakville, ON, Canada) for 30 minutes at 37°C. Cells were recovered by centrifugation and resuspended in DMEM 10% calf serum containing 8 μg/mL polybrene (Aldrich Chemical, St Louis, MO) followed by serial dilutions and overlay of a monolayer of BALB 3T3 (clone A31). Cells were incubated for an hour and then 5 mL of DMEM 10% calf serum was added. Dishes were incubated until the cells reached confluency and then they were irradiated with UV and overlaid with 106 XC cells in DMEM containing 5% FBS. Medium was changed after 24 hours, and 24 hours later the cells were fixed and stained (0.2% methylene blue, 50% methanol). The number of plaques was determined macroscopically.
Results
Segregation analyses
BXH-2 mice are susceptible to infection with Mycobacterium bovis (BCG),3 despite harboring a resistant allele at the Nramp1 locus (Nramp1G169). BXH-2 mice also have splenomegaly at the time that they are killed following BCG infection. This splenomegaly is unique to BXH-2 (SI 0.927 ± 0.066) mice and is not seen in either infected C57BL/6J (SI 0.693 ± 0.047) or C3H/HeJ (SI 0.530 ± 0.027) mice analyzed in a similar fashion (Figure 1; data not shown). To investigate the genetic heritability of both phenotypes, BXH-2 males were crossed to multiple females to generate informative F1 and F2 mice of different strain combinations, which were infected with Mycobacterium bovis (BCG), and their susceptibility to infection was initially assessed by CFU counts in the spleen 3 weeks later (data not shown). The analysis of F2 crosses involving BXH-2 and 3 independent inbred strains of either Nramp1D169 (susceptible) or Nramp1G169 (resistant) genotypes failed to detect segregation of novel BXH-2–derived susceptibility loci, with most if not all variance determined by Nramp1 alleles (data not shown).
Replication of Mycobacterium bovis (BCG) and splenomegaly response in different crosses. Informative F1 and F2 crosses were derived from mouse strains BXH-2, C57BL/6J (B6, panel B), C3H/HeJ (C3, panel C), BALB/cJ (BA, panel D), and A/J (A, panel E), in the combinations indicated at the top of each graph. (BALB/cJ × BXH-2) F2 animals were genotyped with a total of 193 polymorphic dinucleotide repeat markers providing an average coverage of 10 cM along each chromosome. For individual F2 crosses, mice were further separated according to homozygosity or heterozygosity for either mutant (Nramp1D169, D) or wild-type (Nramp1G169, G) alleles at Nramp1. At the time they were killed, spleen weight was determined and used to calculate the spleen index, as described in “Materials and methods.” Dots represent individual mice, and means for each group are shown as lines on the graphs.
Replication of Mycobacterium bovis (BCG) and splenomegaly response in different crosses. Informative F1 and F2 crosses were derived from mouse strains BXH-2, C57BL/6J (B6, panel B), C3H/HeJ (C3, panel C), BALB/cJ (BA, panel D), and A/J (A, panel E), in the combinations indicated at the top of each graph. (BALB/cJ × BXH-2) F2 animals were genotyped with a total of 193 polymorphic dinucleotide repeat markers providing an average coverage of 10 cM along each chromosome. For individual F2 crosses, mice were further separated according to homozygosity or heterozygosity for either mutant (Nramp1D169, D) or wild-type (Nramp1G169, G) alleles at Nramp1. At the time they were killed, spleen weight was determined and used to calculate the spleen index, as described in “Materials and methods.” Dots represent individual mice, and means for each group are shown as lines on the graphs.
A different picture emerged from the analysis of the splenomegaly phenotype. Indeed, in the (B6 × BXH-2) cross (Figure 1B), (B6 × BXH-2)F1 mice showed a spleen index (SI ∼0.6), which was in the range of B6 (SI ∼0.7) and C3H (SI ∼0.5) controls but which was clearly inferior to that of BXH-2 (SI ∼0.9; Figure 1A). This suggests that splenomegaly of BXH-2 behaves as a recessive trait. Analysis of SI values of (B6 × BXH-2)F2 mice showed that splenomegaly was indeed segregating in this cross, with approximately 25% F2 animals (47/184) showing SI values in the range of BXH-2 (SI ≥ 0.8) and the rest showing values in the range of B6 and C3H parental controls (0.45 < SI < 0.8; Figure 1B). Grouping of (B6 × BXH-2)F2 mice according to their Nramp1 genotype (G/D, D/D, G/G) showed that there was no effect of Nramp1 on the presence/absence of splenomegaly, as the latter segregated in animals of all 3 Nramp1 genotypes. The high splenomegaly trait segregating in (B6 × BXH-2)F2 mice is unique to BXH-2 and was not detected in (B6 × C3H)F2 mice derived from the same progenitor strains and similarly infected with M bovis (BCG) (Figure 1C). This strongly suggests that splenomegaly in BXH-2 mice is associated with a novel mutation that appeared during the breeding of this strain. BXH-2–associated splenomegaly also appeared to segregate as a recessive monogenic trait in (BALB/cJ [Nramp1D169] × BXH-2)F2 and (A/J [Nramp1G169] × BXH-2)F2 mice (Figure 1D-E). These results suggested that splenomegaly is unrelated to and segregates independently from the presence/absence of M bovis (BCG) replication.
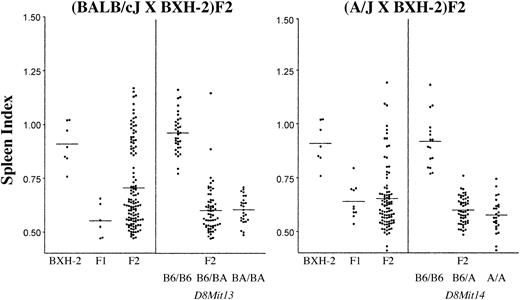
To test this hypothesis, 118 (BALB/cJ × BXH-2)F2 mice and 91 (A/J × BXH-2)F2 mice were produced, killed at 3 to 4 months of age, and the SI values determined in the absence of M bovis (BCG) infection (Figure 2). The results were identical in both crosses and showed that BXH-2–associated splenomegaly segregates as a single recessive trait as 33 of 118 uninfected (BALB/cJ × BXH-2)F2 and 14 of 91 uninfected (A/J × BXH-2)F2 animals had SI values of at least 0.8. Thus, the unique splenomegaly of BXH-2 initially detected in response to M bovis (BCG) infection appears to be an autonomous trait that segregates as a single trait even in the absence of infectious stimulus.
Segregation of splenomegaly in F2 mice derived from BXH-2. F1 and F2 animals derived from (BALB/cJ × BXH-2) and from (A/J × BXH-2) crosses were killed and spleen index was calculated as described in “Materials and methods.” For individual F2 crosses, mice were further separated according to homozygosity or heterozygosity for C57BL/6J (B6), BALB/cJ (BA), or A/J (A) alleles at D8Mit13 (polymorphic with BALB/cJ) or D8Mit14 (polymorphic with A/J). BXH-2 is fixed for B6 alleles at D8Mit13 and D8Mit14. Dots represent individual mice, and means for each group are shown as lines on the graphs.
Segregation of splenomegaly in F2 mice derived from BXH-2. F1 and F2 animals derived from (BALB/cJ × BXH-2) and from (A/J × BXH-2) crosses were killed and spleen index was calculated as described in “Materials and methods.” For individual F2 crosses, mice were further separated according to homozygosity or heterozygosity for C57BL/6J (B6), BALB/cJ (BA), or A/J (A) alleles at D8Mit13 (polymorphic with BALB/cJ) or D8Mit14 (polymorphic with A/J). BXH-2 is fixed for B6 alleles at D8Mit13 and D8Mit14. Dots represent individual mice, and means for each group are shown as lines on the graphs.
Linkage mapping of splenomegaly
To map the BXH-2 locus controlling splenomegaly, a whole genome scan was conducted in 187 informative (BALB/cJ × BXH-2)F2 mice infected with M bovis (BCG) (Figure 1D). Genotyping data were compiled and analyzed by a standard analysis of variance (ANOVA) test, using spleen index as a phenotypic marker. A single highly significant linkage was identified on the distal portion of chromosome 8, with a maximum LOD score of 44.1 for marker D8Mit13 (χ2 = 202.9; Table 1). Linkage analysis of the splenomegaly trait was also carried out in a second group of 118 uninfected (BALB/cJ × BXH-2)F2 mice, using a subset of markers from distal chromosome 8 (Table 2), and also revealed very strong linkage to D8Mit13 (χ2 = 158.8; LOD = 34.5), confirming that M bovis (BCG) infection has no effect on expressivity or penetrance of splenomegaly. Further linkage studies in 2 additional (A/J × BXH-2)F2 populations infected (n = 187) or not infected (n = 91) with M bovis (BCG) verified very strong linkage of splenomegaly to distal chromosome 8 markers, including D8Mit14 (χ2 = 113.1, LOD = 24.6; and χ2 = 114.5, LOD = 24.9, respectively; Table 2). The effect of parental allele combinations for distal chromosome 8 markers on splenomegaly is shown for the (BALB/cJ × BXH-2)F2 (D8Mit13) and (A/J × BXH-2)F2 (D8Mit14) crosses (Tables 1, 2; Figure 2). These results show that in both crosses, splenomegaly is transmitted by BXH-2 alleles as a fully recessive trait, with chromosome 8 alleles explaining 100% of the phenotypic variance. This locus has been given the temporary designation Myls.
Figure 3 shows the distribution of chromosomal haplotypes for 4 informative chromosome 8 markers in relation to splenomegaly (Myls) in 305 (BALB/cJ × BXH-2)F2 mice. Minimizing the number of double crossovers produced the locus order telomere-D8Mit86-D8Mit200-D8Mit13-D8Mit326, with the Myls locus mapping within an 18-cM interval bounded by D8Mit200 and D8Mit13 (Figure 4). The exact distance of Myls to the flanking markers within this interval cannot be established with certainty, as mice homozygotes for BALB/cJ alleles and heterozygotes for BA/B6 alleles have the same wild-type phenotype.
Haplotype map of (BALB/cJ × BXH-2)F2 mice for the central portion of chromosome 8. Each column represents a chromosomal haplotype in (BALB/cJ × BXH-2)F2 mice, with the total number of animals bearing this haplotype indicated at the bottom (n). For genetic markers D8Mit86, 200, 13, and 326, homozygosity for either C57BL/6J (▪; BXH-2 derived), or BALB/cJ (□), or heterozygosity (◥) is identified. The presence (▪) or absence (semi-hatched boxes) of splenomegaly (Myls) is shown. Haplotypes showing one recombination or 2 recombination events in the D8Mit86 to D8Mit326 are shown to the left and to the right, respectively.
Haplotype map of (BALB/cJ × BXH-2)F2 mice for the central portion of chromosome 8. Each column represents a chromosomal haplotype in (BALB/cJ × BXH-2)F2 mice, with the total number of animals bearing this haplotype indicated at the bottom (n). For genetic markers D8Mit86, 200, 13, and 326, homozygosity for either C57BL/6J (▪; BXH-2 derived), or BALB/cJ (□), or heterozygosity (◥) is identified. The presence (▪) or absence (semi-hatched boxes) of splenomegaly (Myls) is shown. Haplotypes showing one recombination or 2 recombination events in the D8Mit86 to D8Mit326 are shown to the left and to the right, respectively.
Schematic representation of chromosome 8. Markers shown were used to genotype mice of the F2 crosses. Intermarker distances (right; in cM) are based on the frequency of recombination in the crosses: 305(BALB/cJ × BXH-2)F2 and 278(A/J × BXH-2)F2. However, their absolute positions in megabase (Mb; left) along the chromosome are based on National Center for Biotechnology Information (NCBI; www.ncbi.nlm.nih.gov/genome/guide/mouse/) and Ensembl project (www.ensembl.org) databases. The centromere is identified by a large dot.
Schematic representation of chromosome 8. Markers shown were used to genotype mice of the F2 crosses. Intermarker distances (right; in cM) are based on the frequency of recombination in the crosses: 305(BALB/cJ × BXH-2)F2 and 278(A/J × BXH-2)F2. However, their absolute positions in megabase (Mb; left) along the chromosome are based on National Center for Biotechnology Information (NCBI; www.ncbi.nlm.nih.gov/genome/guide/mouse/) and Ensembl project (www.ensembl.org) databases. The centromere is identified by a large dot.
Histopathology of splenomegaly
To better define the pathologic basis of splenomegaly observed in BXH-2 mice and segregating in F2 mice derived from it, spleen, lymph nodes, liver, thymus, lung, kidney, and femur bone marrow were harvested from BXH-2, B6, and A/J parental controls as well as from (A/J × BXH-2)F2 mice displaying splenomegaly (high SI) or not (low SI). F2 mice with splenomegaly showed abnormalities in spleen, bone marrow, and lymph nodes, whereas liver, thymus, lungs, and kidney were normal. In addition, analysis of hematologic cellularity and biochemical parameters failed to detect major changes between the 2 groups of mice. Spleens from F2 mice with high SI were on average 2 to 3 times the size of that seen in other F2 mice or in normal controls (data not shown). Microscopic examination of spleen sections showed that the structure and cellular composition of the white pulp was very similar in both groups of mice, consisting mostly of lymphocyte-like cells (compare Figure 5E,F with G,H). In control and low-SI mice, the red pulp showed a plurality of identifiable cell types, with large numbers of reticuloid macrophages and erythrocytes, with additional lymphocytes and polymorphonuclear leukocytes (Figure 5A-B). The cellular composition of the red pulp from F2 mice with high SI was strikingly different from low-SI mice: it was characterized by the presence of a very large number of cells with ring nuclei resembling immature polymorphonuclear leukocytes (Figure 5C-D). In bone marrow, the normal cellularity seen in low-SI F2 mice (Figure 5I-J) was largely replaced by an abundant number of cells with polymorphonuclear precursor appearance (Figure 5K-L). Finally, lymph nodes from F2 mice with high SI were enlarged compared with controls (compare Figure 5M,O) and also showed abundant infiltration of cells with polymorphonuclear precursor appearance. A number of large cells containing elongated inclusions were also noted in lymph nodes and marrow (compare Figure 5N,P and J,L). These results suggest a dramatic expansion of the myeloid compartment (neutrophil, PMN) in F2 mice with splenomegaly, possibly associated with an inflammatory response or with a myeloproliferative disorder.
Cell types affected by splenomegaly
Single cell suspensions were prepared from spleen, bone marrow, and lymph nodes and analyzed by fluorescence-activated cell sorter (FACS) for surface markers. In these experiments, we compared C57BL/6J, BXH-2, and (BALB/cJ × BXH-2)F2 mice that displayed or did not display splenomegaly (Figure 6A-B). In the spleen of BXH-2 mice and F2 animals with splenomegaly, a dramatic 13-fold increase (2.2% to 27.9%) of a cell population doubly positive for Mac1 (monocyte, macrophage, granulocyte) and GR1 (granulocyte) cells was observed (Figure 6A). This expansion of Mac1+/GR1+ cells is in agreement with the presence of a large number of cells with ring nuclei morphologically resembling polymorphonuclear leukocyte precursors (Figure 5). In addition, a 14-fold increase (0.6% to 8.7%) in the proportion of Ter119+ cells (erythroid cells) was noted in the spleen of BXH-2 and of F2 mice with splenomegaly, when compared with control B6 and F2 mice without splenomegaly (Figure 6A). A similar increase in the proportion of Mac1+/GR1+ cells was noted in the lymph nodes of BXH-2 mice and F2 animals with splenomegaly (data not shown). Finally, a parallel analysis of bone marrow cells from these same mice (Figure 6B) showed a 3-fold increase (25.5% to 82.5%) in the proportion of Mac1+/GR1+ cells, which was concomitant with a 15.5-fold decrease (31.0% to 2.0%) in the number of Ter119+ cells. These results confirm that the distinct phenotype of BXH-2 includes expansion of Mac1+/GR1+ cells. The reduction of Ter119+ cells in bone marrow, which was paralleled by an increase of these cells in the spleen, is indicative of extramedullary erythropoiesis in mice with splenomegaly. This extramedullary erythropoiesis is probably secondary to the expansion of Mac1+/GR1+ cells in bone marrow and other hematopoietic organs, possibly associated with a myeloproliferative syndrome (Myls).
Cellular composition of spleen and bone marrow in mice segregating the splenomegaly phenotype. Monocellular suspensions from spleen (A) and bone marrow (B) from C57BL/6J and BXH-2 parental controls as well as from (BALB/cJ × BXH-2)F2 mice showing presence (high SI) or absence (low SI) of splenomegaly were used. Cells were analyzed by flow cytometry for the expression of various cell surface markers, the most informative ones being Thy1.2 (T lymphocytes), Mac1 (macrophage/granulocyte), GR1 (granulocyte), Ter119 (erythroid lineage), and CD11c (dendritic cells), as indicated at the top of each panel. Cells were prepared and stained with either one marker or with 2 markers in combination using different fluorophors (fluorescein isothiocyanate [FITC], phycoerythrin [PE]) and as described in “Materials and methods.” The fraction (percentage) of singly or doubly positive cells found in each quadrant is indicated. BXH-2 mice and F2 animals with splenomegaly (high SI) show important increase in the proportion of Mac1/GR1 doubly positive cells in bone marrow and spleen. In these mice, Ter119+ cells are increased in the spleen (extramedullary erythropoiesis) and reduced in bone marrow when compared with C57BL/6J controls or with F2 mice lacking splenomegaly.
Cellular composition of spleen and bone marrow in mice segregating the splenomegaly phenotype. Monocellular suspensions from spleen (A) and bone marrow (B) from C57BL/6J and BXH-2 parental controls as well as from (BALB/cJ × BXH-2)F2 mice showing presence (high SI) or absence (low SI) of splenomegaly were used. Cells were analyzed by flow cytometry for the expression of various cell surface markers, the most informative ones being Thy1.2 (T lymphocytes), Mac1 (macrophage/granulocyte), GR1 (granulocyte), Ter119 (erythroid lineage), and CD11c (dendritic cells), as indicated at the top of each panel. Cells were prepared and stained with either one marker or with 2 markers in combination using different fluorophors (fluorescein isothiocyanate [FITC], phycoerythrin [PE]) and as described in “Materials and methods.” The fraction (percentage) of singly or doubly positive cells found in each quadrant is indicated. BXH-2 mice and F2 animals with splenomegaly (high SI) show important increase in the proportion of Mac1/GR1 doubly positive cells in bone marrow and spleen. In these mice, Ter119+ cells are increased in the spleen (extramedullary erythropoiesis) and reduced in bone marrow when compared with C57BL/6J controls or with F2 mice lacking splenomegaly.
B-ecotropic MuLV virus replication
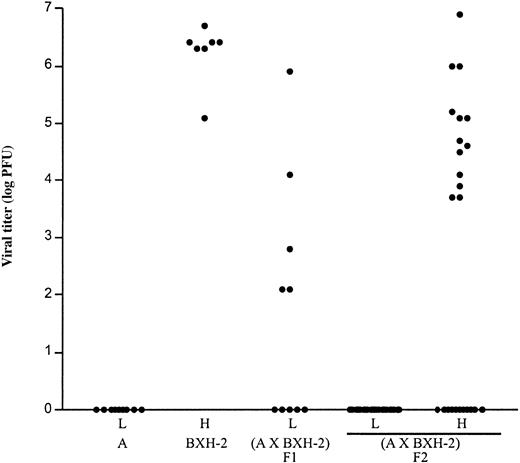
BXH-2 mice develop B-ecotropic murine leukemia virus (MuLV)–induced myeloid leukemia at high frequency.16 One of the phenotypic features of this leukemia is the presence of splenomegaly and hepatomegaly.17 Although it is difficult to see how the fully recessive nature of splenomegaly controlled by Myls could be caused by the transmission of a replication-competent MuLV, the fact that 1 of the 2 endogenous ecotropic MuLVs carried by BXH-2 mice (Emv2) regionally maps to the 18-cM Myls interval prompted further experimentation. Possible cosegregation of splenomegaly and the presence of replication-competent ecotropic virus was investigated in spleens of A/J and BXH-2 controls and in (A/J × BXH-2)F1 and F2 spleens, using an XC plaque assay (Figure 7). While none of the A/J mice (0/9) had virus in their spleens, all BXH-2 (7/7) spleens were virus positive with titers ranging from 105 to 107 plaque-forming units (PFUs)/spleen. In contrast, while (A/J × BXH-2)F2 animals with low SI were uniformly negative for virus (0/26), approximately half of the F2 animals (13/24) with splenomegaly (Myls homozygotes) showed the presence of viral replication in the spleen (Figure 7). These results suggest partial cosegregation, but not tight linkage, of the splenomegaly phenotype with virus replication, indicating that they are not caused by the same genetic event.
Detection of B-ecotropic murine leukemia virus (MuLV) in the spleen of mice segregating the splenomegaly phenotype. Spleen cells from control A/J (5- to 13-week-old) and BXH-2 (5- to 16-week-old) parents and from (A/J × BXH-2) F1 (20- to 36-week-old) and F2 (5- to 16-week-old) mice showing either presence (high SI; H) or absence (low SI; L) of splenomegaly were harvested and used to detect the presence of B-ecotropic virus by an XC plaque assay, as described in “Materials and methods.” BALB 3T3 mouse cells were exposed to serial dilutions of mitomycin C–treated splenocytes. After reaching confluence, the infected cultures were UV irradiated and overlaid with XC cells. Forty-eight hours later, cells were fixed and stained for syncytial plaques count (plaque-forming units, PFU), and a viral titer was calculated (log PFU).
Detection of B-ecotropic murine leukemia virus (MuLV) in the spleen of mice segregating the splenomegaly phenotype. Spleen cells from control A/J (5- to 13-week-old) and BXH-2 (5- to 16-week-old) parents and from (A/J × BXH-2) F1 (20- to 36-week-old) and F2 (5- to 16-week-old) mice showing either presence (high SI; H) or absence (low SI; L) of splenomegaly were harvested and used to detect the presence of B-ecotropic virus by an XC plaque assay, as described in “Materials and methods.” BALB 3T3 mouse cells were exposed to serial dilutions of mitomycin C–treated splenocytes. After reaching confluence, the infected cultures were UV irradiated and overlaid with XC cells. Forty-eight hours later, cells were fixed and stained for syncytial plaques count (plaque-forming units, PFU), and a viral titer was calculated (log PFU).
Discussion
BXH-2 mice were derived from an F2 cross between C57BL/6J and C3H/HeJ parents. Interestingly, although carrying resistance alleles at Nramp1 (Nramp1G169),3 BXH-2 mice are highly permissive for replication of Mycobacterium bovis (BCG). By examining F1 mice generated from crosses between BXH-2 and several inbred strains that are either Nramp1G169 (A/J) or Nramp1D169 (C57BL/6J, BALB/cJ), we observed that BXH-2 susceptibility to M bovis (BCG) infection is completely recessive. In F2 mice, susceptibility to M bovis (BCG) was completely controlled by Nramp1 alleles, and we were unable to identify a suitable cross where BXH-2 susceptibility to M bovis (BCG) infection would segregate and could be mapped (data not shown). This suggests that BXH-2 susceptibility to M bovis (BCG) is either complex, only expressed in the context of the rest of the BXH-2 genome, and/or can be actively suppressed by multiple loci segregating in the inbred strains used to generate the F2 crosses.
During the process of phenotyping F1 and F2 mice, we noted that BXH-2 animals at the peak of infection had splenomegaly. Although splenomegaly is a normal response to M bovis (BCG) infection,26 splenomegaly in BXH-2 mice was far superior to that seen in any other inbred strains tested, including B6 and C3H, the parents of BXH-2. When analyzed in informative F2 crosses, splenomegaly was inherited in a completely recessive fashion that segregated as a monogenic trait but independently of Nramp1 alleles. In fact, splenomegaly was found to segregate in independent F2 crosses even in the absence of M bovis (BCG) infection, suggesting that splenomegaly was not caused by infection. A single locus Myls controlling splenomegaly was mapped to the central portion of chromosome 8. Histologic studies in F2 mice indicated that splenomegaly was associated with the presence of a very large number of cells with ring nuclei resembling immature polymorphonuclear leukocytes in the red pulp, whereas the white pulp appeared normal. These cells were also found in large numbers in lymph nodes and in bone marrow and were identified by FACS analysis as Mac1+/GR1+ granulocytes. Expansion of the Mac1+/GR1+ compartment in these organs was associated with extramedullary erythropoiesis in the spleen, as noted by the relative distribution of Ter119+ erythroid precursors in these organs. Examination of blood smears from F2 mice (8- to 16-weeks old) with splenomegaly failed to detect these granulocyte precursors in circulating blood, suggesting that expansion of these cells may occur primarily in situ in spleen, lymph nodes, and bone marrow. Expansion of the Mac1+/GR1+ compartment in these organs may result from either an inflammatory response to an as yet unidentified stimulus or may happen constitutively through loss of a negative control of proliferation in this cell compartment (myeloproliferative syndrome). The former appears unlikely since our mouse colony has been basically pathogen free for many years (albeit not strictly specific pathogen free [SPF]), the experiments used for this study span approximately 5 years, and splenomegaly is not only fully recessive but also 100% penetrant in the 5 F2 crosses analyzed, an observation not compatible with a possible effect of an environmental pathogen. Therefore, our results suggest that the Myls locus on chromosome 8 corresponds to a novel mutation that appeared during the breeding of BXH-2 mice, which is inherited in a fully recessive and fully penetrant fashion and that regulates the size of the Mac1+/GR1+ cellular compartment.
BXH-2 mice spontaneously develop myeloid leukemia with a pathophysiology that includes splenomegaly, lymph node enlargement, and neurologic damage following infiltration of leukemic cells into the brain.16 This leukemia is caused by a B-ecotropic MuLV via insertional mutagenesis. BXH-2 mice also express a low level of a dual tropic mink cell focus-forming virus, which is not tumorigenic.17 Replication of this B-ecotropic virus is under control of the Fv-1 gene, and BXH-2 has the Fv1b permissive allele at this locus.27 The ecotropic MuLV expressed in BXH-2 mice has previously been proposed to arise by recombination between the 2 endogenous ecotropic proviruses carried in BXH-2 mice, Emv1 and Emv2. Neither endogenous provirus is highly expressed, suggesting that each may carry a mutation, perhaps selected, that prevents it from being expressed. If the mutations are in different locations in the 2 proviruses, then recombination between the 2 proviruses could regenerate a nondefective virus that is then transmitted in BXH-2 mice. The virus expressed in BXH-2 mice is not integrated in the germ line and is transmitted by females to their offspring via transplacental infection and/or through the mother's milk. The 2 endogenous BXH-2 ecotropic proviruses do not appear to contribute to the development of tumors in BXH-2 mice since the virus expressed in BXH-2 mice can induce tumors in other BXH strains that lack both endogenous proviruses, whereas other BXH strains that have both proviruses do not develop leukemia.17,28
Several lines of evidence suggest that Myls-controlled splenomegaly is not caused by the virus horizontally transmitted in BXH-2 mice. First, splenomegaly induced by this expressed virus would be expected to behave as a dominant trait in F1 and F2 crosses,29 as opposed to the recessive mode of inheritance for Myls seen here. Second, the BXH-2 virus is not integrated in the genome and is transmitted by females to their offspring.28 In the BXH-2 F1 and F2 crosses generated with A/J, B6, and BALB/c (Figure 1) and used to study the segregation of Myls, only BXH-2 male animals were used for breeding. Third, Southern blots with pECO probe on tail DNA digested with PvuII failed to detect new viral integrations in our BXH-2 stock (data not shown). However, it is still possible that a third provirus is present. Indeed, such a provirus may display restriction fragments identical to those of Emv1 and Emv2 and thus may have gone undetected by Southern blotting. Fourth, only about half of the spleens of (A/J × BXH-2)F2 animals with splenomegaly (Myls/Myls) scored positive for virus by XC plaque assays. The fact that not all F2 spleens with splenomegaly expressed virus further supports the hypothesis that virus expression does not cause splenomegaly. Finally, splenomegaly segregating in the (BXH-2 [Fv-1b] × C3H [Fv-1n])F2 cross was found to appear even in F2 mice homozygote for Fv-1n (as determined by genotyping with D4Mit42) that are not permissive to replication of B-ecotropic virus.
In contrast to (A/J × BXH-2)F2 animals with splenomegaly, virus was never detected in the spleens of (A/J × BXH-2)F2 animals without splenomegaly. Thus, splenomegaly appears to be required for virus expression. However, only about 50% of (A/J × BXH-2)F2 animals with splenomegaly express virus. Therefore, although we cannot exclude the possibility that some B-ecotropic virus replication may have escaped detection by the XC plaque assay used, the association between virus expression and splenomegaly appears incomplete. What is the source of the virus detected in the spleens of (A/J × BXH-2)F2 animals with splenomegaly? We favor the hypothesis that this virus is again generated by recombination between Emv1 and Emv2. These 2 proviruses are the only endogenous ecotropic proviruses segregating in these animals, as detected by Southern blotting (data not shown), and therefore one or both of these proviruses must be the source of the virus expressed in (A/J × BXH-2)F2 mice. BXH-2 mice are homozygous for Emv1 and Emv2, whereas A/J mice are homozygous for Emv1 but lack Emv2. All (A/J × BXH-2)F2 animals will therefore carry 2 copies of Emv1, whereas 75% will carry at least one copy of Emv2 (the other 25% will carry no copies of Emv2). In support of this model, all (A/J × BXH-2)F2 animals with splenomegaly (Myls/Myls) that express virus carry at least one copy of Emv2. Viremia in F2 animals is therefore linked to Emv2. Why don't F2 animals without splenomegaly express virus? After all, 75% of these animals also carry Emv1 and at least one copy of Emv2. While there are many possible explanations, one explanation we favor is that the myeloproliferation and ensuing splenomegaly (specific for Myls/Myls homozygotes and absent in +/+ or Myls/+ F2s) drives the recombination between Emv1 and Emv2, which is necessary to generate this virus. Recombination is not 100% efficient, however, possibly explaining why only 50% of the Myls/Myls F2 animals with splenomegaly have detectable virus in their spleen. Other possible explanations for the significant fraction of Myls/Myls homozygotes in which we do not detect viremia in the spleen by our assay (Figure 7) include the following: (1) Not all Myls/Myls F2 mice develop viremia due to incomplete penetrance and/or reduced expressivity of the trait, possibly caused by intrinsic or environmental factors. (2) All Myls/Myls animals may have virus in their spleen, but the viral titer in some animals may be too low to be detected by our assay. (3) The production of virus on the Myls/Myls background may be further influenced by other genetic factors that are yet to be identified. These different possibilities need to be distinguished experimentally.
Our results also help to explain a long-standing paradox: why do BXH-2 mice develop leukemia while the 11 other BXH strains do not (even though some of these strains are homozygous for Emv1 and Emv2), and why are BXH-2 mice uniquely susceptible to myeloid leukemia as opposed to other hematopoietic diseases such as T- and B-cell lymphoma? Our results suggest that the unique features of BXH-2 are due to the Myls mutation, which is fixed in and unique to BXH-2 and the BXH-2 endogenous proviruses Emv1 and Emv2, which were inherited from their C3H/HeJ and C57BL/6J parents. Myls causes the splenomegaly seen in preleukemic BXH-2 mice and also drives the recombination between Emv1 and Emv2, which is needed to generate an infectious MuLV. Once the infectious MuLV is generated it causes leukemia in BXH-2 mice via insertional mutagenesis. Myeloid leukemia is the preferred disease type because it is this population of cells that is expanded due to the Myls mutation. Expansion of the myeloid cell compartment provides more myeloid cells for virus infection and eventual insertional mutagenesis.
What causes Myls-associated splenomegaly and myelodysplasia? As discussed previously, splenomegaly does not appear to be caused by virus replication. Splenomegaly is also not associated with Emv1 since splenomegaly was present in (BXH-2 × B6)F2 animals lacking Emv1. While we cannot completely rule out the possibility that splenomegaly is caused by Emv2, we favor the hypothesis that splenomegaly is due to the loss of a negative growth regulation signal, perhaps due to a mutation in a tumor suppressor gene and/or a block of maturation of Mac1+/GR1+ granulocyte precursors associated with a secondary expansion of that compartment. If our hypothesis is true, positional cloning of Myls may provide important insights into genes that specifically regulate the growth and/or maturation of myeloid cells.
Prepublished online as Blood First Edition Paper, November 20, 2003; DOI 10.1182/blood-2003-06-1852.
Supported by research grants to P.G. from the Canadian Genetic Diseases Network (CGDN). K.T. was supported by studentships from the Fonds de la Recherche en Santé du Québec (FRSQ) and the Canadian Institutes of Health Research (CIHR). N.G.C. and N.A.J. were supported by the National Cancer Institute, Department of Health and Human Services (DHHS). P.G. is a Distinguished Scientist of the Canadian Institutes of Health Research.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank François Canonne-Hergaux, Nada Jabado, and Anny Fortin for helpful advice and Caroline Lagassé, Vladimir Marquez Azalgara, and Ginette Massé for their technical help.





![Figure 6. Cellular composition of spleen and bone marrow in mice segregating the splenomegaly phenotype. Monocellular suspensions from spleen (A) and bone marrow (B) from C57BL/6J and BXH-2 parental controls as well as from (BALB/cJ × BXH-2)F2 mice showing presence (high SI) or absence (low SI) of splenomegaly were used. Cells were analyzed by flow cytometry for the expression of various cell surface markers, the most informative ones being Thy1.2 (T lymphocytes), Mac1 (macrophage/granulocyte), GR1 (granulocyte), Ter119 (erythroid lineage), and CD11c (dendritic cells), as indicated at the top of each panel. Cells were prepared and stained with either one marker or with 2 markers in combination using different fluorophors (fluorescein isothiocyanate [FITC], phycoerythrin [PE]) and as described in “Materials and methods.” The fraction (percentage) of singly or doubly positive cells found in each quadrant is indicated. BXH-2 mice and F2 animals with splenomegaly (high SI) show important increase in the proportion of Mac1/GR1 doubly positive cells in bone marrow and spleen. In these mice, Ter119+ cells are increased in the spleen (extramedullary erythropoiesis) and reduced in bone marrow when compared with C57BL/6J controls or with F2 mice lacking splenomegaly.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/103/6/10.1182_blood-2003-06-1852/6/m_zh80060458550006.jpeg?Expires=1767732205&Signature=xeIdH0Z4FIfIHP~Yn5iIHQAE2zVt4Ad6-AC~tm1CXE66L4XI6xbOXkiKQiaZ-0rhSMRhjlUG59juWPXPoy7hcxlYxQLC6Q2KaR2jYzeDSZrr0iJB7haHNKUBDDkYsFZ8KKo428Y3P8F~P15oRPDGPt3eDTgLqKqMrhCv53zccgrcZH8qU2b9Zaz9CAdD~HxWptJFsdd6vqoccOYhCtM-W5uk4IpuM6Yosi0qxF4yv41ghNPI4v3zW2YFqSf8cVKt66-6bQoe3Vf5971QtBTXfHihWi097A6dhIPgkFrRCPmMEWidsEQXGnSumKcuFh~HcqNgC1up7vQxqICj-pMqYQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)