GENE THERAPY
Several congenital deficiencies such as hemophilia B and anemia are currently treated by administration of recombinant proteins. However, repeated clinical administration of therapeutic proteins is cumbersome, and such genetic disorders could be cured via gene transfer vectors, allowing sustained and/or controlled expression of these proteins. In this respect, the intramuscular inoculation of adeno-associated viral (AAV) vectors expressing human blood coagulation factor IX seems extremely promising for treatment of patients with hemophilia B, and clinical trials have now progressed into phase 1/2.1 Likewise, biologically active erythropoietin (EPO) can be secreted from skeletal muscle and was shown to improve erythropoiesis in beta-thalassemic mice.2 So far, protein replacement therapy with recombinant human EPO (rhuEPO) produced from mammalian cells, biologically equivalent to the natural hormone, has been extremely effective to remedy several forms of anemia. Although approximately 3 million people throughout the world have now been treated, very few patients have developed pure red cell aplasia following rhuEPO therapy.3 It is only in the last few years that a significant increase in the # of cases of absolute resistance to rhuEPO therapy due to anti-EPO antibodies was reported, most likely as a result of slight modifications in the production and formulation of the clinical grade rhuEPO. As for gene therapy, there is clear evidence for humoral and cellular immune responses against transgenic proteins—as well as absence of such responses, depending on vector design, gene dosage, or the underlying mutation in the dysfunctional gene.
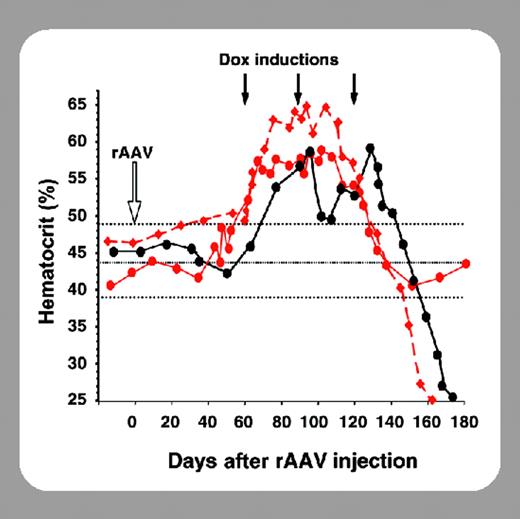
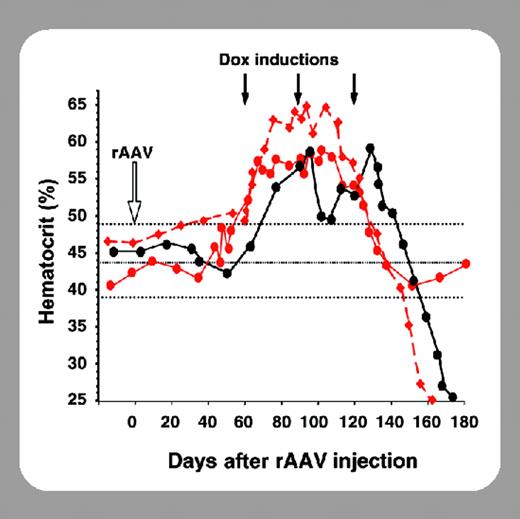
In this issue of Blood, 2 independent studies from Chenuaud and colleagues (page 3303) and Gao and colleagues (page 3300) describe for the first time an inadvertent autoimmune response in nonhuman primates resulting from transfer of a gene encoding a self-antigen. Their approach was to deliver the homologous EPO cDNA driven by ubiquitous and/or regulatable promoters via AAV vectors injected in muscle or aerosolized in lung, resulting in supra-physiologic serum levels of EPO, from 10- to 100 000- fold over the baseline. However, this genetic intervention broke the immune tolerance, and, within a few weeks, some macaques suffered from severe autoimmune anemia, possibly induced by T/B lymphocytes and monocyte infiltrates in inoculated muscles as well as by neutralizing antibodies against both the transgenic and endogenous EPO. The reasons for the autoimmunity induced by homologous EPO gene transfer are not clear. Trivial mechanisms such as sequence differences between transgenic and endogenous EPO cDNAs as well as vector particle-induced inflammation could be ruled out a priori. Furthermore, the fact that anemia sporadically arose in 2 different macaque species upon gene transfer using several rAAV serotypes in 2 ectopic expression sites (muscle or lung versus kidney) rather suggests an EPO-specific effect. Thus, the autoimmune anemia might be due to the ectopic expression site of the transgene or to supraphysiologic expression levels that could induce posttranslational modifications; yet it may also be contributed by vector spreading in the draining lymph nodes and subsequent EPO expression in professional APCs. In addition, there was no clear correlation between elevated EPO levels and anemia, suggesting that the events occur in a haplotype-dependent manner.
These results are extremely important, not only because they teach us that in vivo gene delivery is effective, but also because they stress that the direct translation to the clinic of preclinical data obtained in inbred rodent models is not straightforward. Although the laboratory mouse has been invaluable in the preclinical gene therapy era, it shows limitations. Autoimmune responses to gene transfer have never been reported in these small animal models, possibly because they have not been identified or exhaustively assessed. In contrast, more relevant information in safety, efficiency, and immunologic consequences of gene transfer can be expected from wild and large animals. Thus, as vectors have now become efficient enough to allow effective gene delivery, experiments in nonhuman primates are more practical than before, and their more extensive implementation in preclinical studies may be a prerequisite before going to the clinic.