Abstract
Administration of exogenous interleukin-18 (IL-18) regulates experimental acute graft-versus-host disease (GVHD) in a Fas-dependent manner when donor CD4+ T cells are required for mortality after experimental allogeneic bone marrow transplantation (BMT). However, CD4+ and CD8+ T cells can induce acute GVHD after clinical allogeneic BMT, and the role of IL-18 in CD8+-mediated acute GVHD is unknown. We, therefore, determined the role of IL-18 in GVHD mediated by CD4+ or CD8+ T cells across major histocompatibility complex (MHC) class II- and class I-disparate allogeneic BMT, respectively. Administering IL-18 significantly increased survival in CD4+-mediated GVHD but reduced survival in CD8+-mediated GVHD. This increase in deaths was associated with significantly greater clinical, biochemical, and histopathologic parameters of GVHD damage and was independent of Fas expression on donor T cells. Administering IL-18 significantly enhanced allospecific cytotoxic function and expansion of CD8+ cells. Endogenous IL-18 was critical to GVHD mediated by CD8+ donor T cells because IL-18 receptor-deficient donors caused significantly less GVHD but exacerbated CD4+-mediated, GVHD-related death. Furthermore, administering anti-IL-18 monoclonal antibody significantly reduced CD8+-mediated, GVHD-related death. Together these findings demonstrate that IL-18 has paradoxical effects on CD4+ and CD8+ cell-mediated GVHD. (Blood. 2004;104:3393-3399)
Introduction
Acute graft-versus-host disease (GVHD), the major toxicity of allogeneic bone marrow transplantation (BMT), is a complex process involving dysregulated inflammatory cytokine cascades and distorted responses of donor cellular effectors to host alloantigens.1 Proinflammatory cytokines such as tumor necrosis factor alpha (TNF-α) and interleukin-1 (IL-1), released by host tissues during conditioning treatment, and interferon (IFN)-γ, released from donor T cells, play major roles in enhancing acute GVHD.2 Alloreactive donor T cells are important effector cells in the development of GVHD, and proinflammatory cytokines enhance the generation of donor antihost cytotoxic function.3 Thus, cytokine manipulation strategies have the potential to affect GVHD by altering the proinflammatory environment and the cellular effectors that are critical in acute GVHD.
Interleukin 18 (IL-18) is produced by a wide variety of cells such as macrophages, microglia, human peripheral blood mononuclear cells, dendritic cells, T cells, keratinocytes, intestinal and airway epithelia, osteoblasts, and adrenal corticocytes.4 IL-18 stimulates a T helper 1 (TH1) response by inducing IFN-γ, particularly in concert with IL-12.5 IL-18 is also a stimulator of potent proinflammatory cytokines, such as TNF-α, IL-1, and granulocyte macrophage-colony-stimulating factor (GM-CSF).6 IL-18 has been implicated in various disease processes such as autoimmune disorders.4,6 Under certain circumstances, however, IL-18 alone can promote TH2 polarization and allergic inflammation.4
Serum levels of IL-18 are elevated in clinical and experimental acute GVHD.7,8 IL-18 prevents murine chronic GVHD,9 but its effect on the induction of acute GVHD is unclear. In nonirradiated BMT recipients, neutralizing IL-18 did not alter any acute GVHD parameter analyzed.8 Recently, however, Reddy et al10 have demonstrated that administering IL-18 reduces the mortality rate in a lethally irradiated murine BMT model of B6 (H-2b) → B6D2F1 (H-2b/d) acute GVHD induced primarily by CD4+ cells in response to multiple major histocompatibility complex (MHC) and minor histocompatibility antigens.11 Protection against GVHD in that model depended on the expression of Fas and on enhanced donor T-cell apoptosis. However, CD4+ and CD8+ T cells can induce GVHD after clinical allogeneic BMT, and the CD4+ and CD8+ T-cell subsets have differential susceptibility to apoptosis.12 Therefore, we compared the role of IL-18 in mediating acute GVHD in MHC class II (CD4+ mediated) and MHC class I (CD8+ mediated) disparate BMT systems. We found that IL-18 had dramatically opposite effects on the severity of acute GVHD in these different models.
Materials and methods
Mice
Female C57BL/6 (B6, H-2b, CD45.2+), B6.Ly-5a (CD45.1+), B6.C-H2bm12 (bm12, KbDbI-Abm12I-Eb, CD45.2+), B6.C-H2bm1 (bm1, Kbm1DbI-AbI-Eb, CD45.2+), C3H.SW (H-2b, CD45.2+), B6.MRL-TNF-rs6lpr (lpr, H-2b), B6D2F1 (H-2b/d, CD45.2+), and B6.129P2-Il1rrptm1Aki (IL-18r1-/-, H-2b) mice were purchased from the Jackson Laboratories (Bar Harbor, ME). The age range of mice used for experiments was 8 to 12 weeks. Mice were housed in sterilized microisolator cages and received filtered water and normal chow or autoclaved hyperchlorinated drinking water for the first 3 weeks after BMT.
BMT and assessment of acute GVHD
Mice underwent transplantation according to a standard protocol described previously.11 Briefly, recipients received 1300 cGy total body irradiation (TBI; cesium Cs 137 [137Cs] source), split into 2 doses separated by 3 hours to minimize gastrointestinal (GI) toxicity. T cell-depleted (TCD) bone marrow (BM) cells (5 × 106) plus either 2 × 106 enriched CD8+ (into bm1 recipients) or CD4+ (into bm12 recipients) T cells from respective allogeneic or syngeneic donors were resuspended and injected intravenously into recipient animals on day 0. In some experiments, 3 × 106 CD8+ cells were used. Depletion of BM T cells or positive selection of CD4+ and CD8+ cells from spleens was performed using relevant MicroBeads and the AutoMACS system (Miltenyi Biotec, Bergisch Gladbach, Germany) according to the manufacturer's protocol. B6 recipients underwent transplantation in the same manner with CD8+ cells selected from C3H.SW mice. B6D2F1 recipients received (5 × 106) TCD BM from wild-type B6 and 2 × 106 nylon wool-purified CD3+ from IL-18r1-/- donor spleens. For donor cell engraftment experiments, CD45.1+ B6.Ly-5a mice were used as donors. Survival was monitored daily, and body weights and GVHD clinical scores of recipients were measured weekly. The degree of systemic acute GVHD was assessed by a scoring system that incorporates 5 clinical parameters—weight loss, posture (hunching), activity, fur texture, and skin integrity—and that is more accurate than weight loss alone, as described previously.13 At the time of analysis, mice from coded cages were evaluated and graded from 0 to 2 for each criterion. A clinical index was subsequently generated by summation of the 5 criteria scores (maximum index, 10).
Histology
Formalin-preserved small bowel and large bowel were embedded in paraffin, cut into 5-μm-thick sections, and stained with hematoxylin and eosin for histologic examination. Slides were coded without reference to previous treatment and were examined by a pathologist. A semiquantitative scoring system was used to assess GVHD abnormalities.14 The small intestine was scored for villous blunting, crypt regeneration, loss of enterocyte brush border, luminal sloughing of cellular debris, crypt cell apoptosis, crypt destruction, and lamina propria lymphocytic infiltrate. The colon was scored for crypt regeneration, vacuolization and attenuation of surface colonocytes, crypt cell apoptosis, crypt destruction, and lamina propria lymphocytic infiltrate. The scoring system denoted 0 as normal, 0.5 as focal and rare, 1.0 as focal and mild, 2.0 as diffuse and mild, 3.0 as diffuse and moderate, and 4.0 as diffuse and severe. Scores were added to provide a total score for each specimen. After scoring, the codes were broken and data were compiled.
Administration of IL-18 and anti-IL-18 monoclonal antibody
Recombinant murine IL-18 (rmIL-18) was purchased from MBL (Nagoya, Japan) and was reconstituted in phosphate-buffered saline (PBS; Gibco, Grand Island, NY). Mice were injected intraperitoneally with IL-18 (1 μg/d per mouse) on days -2, -1, 0, 1, and 2 (5 injections total) because this dose has been shown to be sufficient for regulating GVHD.10 Mice from the control groups received only PBS according to a similar schedule. In the IL-18 blockade experiments, rat anti-mouse IL-18 monoclonal antibody (mAb) of IgG2a (anti-IL-18 mAb; MBL) was administered intraperitoneally (10 μg/d per mouse), after reconstitution in PBS, on days -1, 0, and every 3 days until 3 weeks after BMT. The control groups received rat immunoglobulin G2a (IgG2a; R&D, Flanders, NJ) reconstituted and injected in a similar fashion.
Fluorescence-activated cell sorter analysis
Fluorescein isothiocyanate (FITC)-conjugated mAbs to mouse CD45.1 and phycoerythrin (PE)-conjugated mAbs to CD8+ were purchased from BD PharMingen (San Diego, CA). The procedure was performed as described previously.10 Briefly, cells were first incubated with mAb 2.4G2 for 15 minutes at 4°C and then with the relevant FITC- or PE-conjugated mAb for 30 minutes at 4°C. Finally, cells were washed twice with PBS/0.2% bovine serum albumin and fixed with PBS/1% paraformaldehyde. Flow cytometry was performed by using FACSVantage SE cell sorter (Becton Dickinson Immunocytometry Systems, San Jose, CA).
Analysis of donor cell apoptosis
Spleens from recipient mice in some of the experiments were harvested 5 days after transplantation and stained with allophycocyanin (APC)-conjugated CD8+ and PE-conjugated CD45.1 and then were washed with 1 × PBS and stained with FITC-conjugated annexin (R&D) in the dark for 15 minutes at room temperature in labeling buffer. Donor cell apoptosis was identified on the basis of annexin staining from double staining for CD45.1 and CD8+.
Cytokine enzyme-linked immunosorbent assay
Antibodies were purchased from BD PharMingen, and assays were performed according to the manufacturer's protocol. Briefly, samples were diluted 1:2 to 1:5, and TNF-α or IFN-γ was captured by the specific primary mAb and detected by horseradish peroxidase (TNF-α) or biotin-labeled (IFN-γ) secondary mAbs. Plates were read at 450 nm using a microplate reader (model 3550; Bio-Rad Labs, Hercules, CA). Recombinant mTNF-α and mIFN-γ (BD PharMingen) were used as standards for enzyme-linked immunosorbent assay (ELISA). Samples and standards were run in duplicate, and the sensitivity of the assays was 16 to 20 pg/mL for each cytokine, depending on the sample dilution. Serum IL-18 was measured by using the mouse IL-18 ELISA kit from R&D Systems (Minneapolis, MN). Samples were diluted 1:2 and were run in duplicate with the standards. The sensitivity of the assay was 25 pg/mL.
Serum LPS estimation
The limulus amebocyte lysate (LAL) assay (BioWhittaker, Walkerville, MD) was performed according to the manufacturer's protocol to determine the lipopolysaccharide (LPS) concentration in serum. Briefly, serum samples were collected and analyzed using pyrogen-free materials, diluted 10% (vol/vol) in LAL reagent water, and heated to 70°C for 5 minutes to minimize nonspecific inhibition. Samples were then incubated with equal volumes of LAL for 10 minutes at 37°C and were developed with equal volumes of substrate solution for 6 minutes. The absorbance of the assay plate was read at 405 nm using the same microplate reader as in cytokine assays. Samples and standards were run in duplicate, and the lower limit of detection was 0.15 U/mL. All units expressed are relative to the US reference standard EC-6.
51Cr release assays
The cytotoxic function of CD8+ T cells was analyzed by the chromium (Cr) release assay, as described previously.15 Briefly, purified B6 CD8+ cells (5 × 106/mL) were cultured with irradiated bm1 splenocytes (5 × 106/mL) in flat-bottom, 24-well plates in a total volume of 2 mL in the presence or absence of IL-18 (20 ng/mL) or anti-IL-18 mAb (0.5 μg/mL) for 96 hours. All the groups were normalized for CD8+ cells. They were added at varying effector-target ratios and were incubated for 3 hours with allogeneic bm1 or syngeneic B6 concanavalin A-stimulated lymphoblast target cells (2 × 106 cells), labeled with 100 μCi (3.7 MBq) 51Cr. 51Cr activity in supernatants was determined in an autogamma counter (Packard Instrument, Meriden, CT). The percentage of specific lysis was calculated as follows: 100 × (sample count - background count)/(maximal count - background count).
Statistical analysis
The Mann-Whitney U test was used for the statistical analysis of cytokine data, LPS levels, clinical GVHD scores, weight loss, and histology, whereas the Wilcoxon rank test was used to analyze survival data.
Results
Effect of IL-18 administration on acute GVHD-related deaths after MHC class I and class II disparate allogeneic BMT
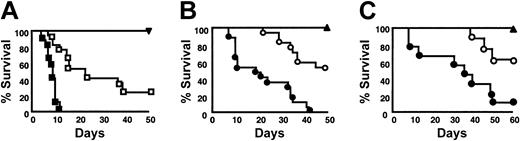
Because CD4+ and CD8+ cells can cause GVHD and have distinct requirements for apoptosis,12 we first compared the effect of exogenous IL-18 injection on acute GVHD-related death in a CD4+-dependent, single MHC class II-disparate (B6, H-2b → bm12, KbDbI-Abm12I-Eb) and in a CD8+-dependent, MHC class I-mismatched (B6, H-2b → bm1, Kbm1DbI-AbI-Eb) BMT model.16 Recipient bm12 mice underwent transplantation with TCD BM, together with CD4+ T cells from allogeneic B6 or syngeneic donors, respectively, as described in “Materials and methods.” Similarly, bm1 mice received TCD BM and CD8+ T cells from allogeneic B6 or syngeneic bm1 donors. Recombinant murine IL-18 was injected into BMT recipients intraperitoneally for 5 days from day -2 to day +2, whereas control mice received identical injections of the diluent. This dose of rmIL-18 was chosen for its ability to modulate acute GVHD in another model.10 As shown in Figure 1A, consistent with the previous data, administering rmIL-18 significantly delayed CD4+-mediated GVHD deaths after MHC class II-disparate BMT (B6 → bm12) (▪ vs □; P < .0001).10 In stark contrast, injection of IL-18 after B6 → bm1 BMT accelerated the GVHD mediated by CD8+ T cells and caused a 100% mortality rate by day 45 (Figure 1B, • vs ○; P < .0001). Animals that underwent syngeneic BMT and received rmIL-18 showed 100% survival (▴), ruling out any nonspecific toxicity of the conditioning and administration of IL-18. All BMT recipients displayed complete donor hematopoietic chimerism, as determined by fluorescence-activated cell sorter (FACS) analysis (data not shown).
Effect of IL-18 on GVHD-related mortality. (A) Recipient bm12 mice were irradiated with 13 Gy TBI and injected with 5 × 106 TCD BM and 2 × 106 purified CD4+ T cells from either allogeneic B6 (□ and ▪) or syngeneic bm12 (▾; n = 9) donors, as described in “Materials and methods.” Allogeneic bm12 recipients were injected intraperitoneally with 1 μg/d rmIL-18 per mouse (▪, n = 17) or diluent (□, n = 17) from days -2 to +2. Syngeneic recipients also received the same dose and schedule of IL-18. Data from 3 similar experiments are combined. Percentage survival after BMT. Percentage survival, ▪ vs □; P < .0001 by Wilcoxon rank test. (B) bm1 mice underwent irradiation and transplantation with 5 × 106 TCD BM and 2 × 106 purified CD8+ T cells from allogeneic B6 or syngeneic bm1 donors. Allogeneic recipients were injected with rmIL-18 (•, n = 17) or diluent (○, n = 17), as described. Syngeneic animals (▴, n = 9) were treated with IL-18 in a similar manner. Data from 3 similar experiments are combined. Percentage survival, • vs ○; P < .0001 by Wilcoxon rank test. (C) B6 recipients were injected with IL-18 or the diluent and underwent transplantation with TCD BM and 2 × 106 CD8+ T cells from allogeneic C3H.SW (•, n = 8; ○, n = 9) or syngeneic B6 donors (▴, n = 4) as described. Percentage survival after BMT, • vs ○; P = .01 by Wilcoxon rank test.
Effect of IL-18 on GVHD-related mortality. (A) Recipient bm12 mice were irradiated with 13 Gy TBI and injected with 5 × 106 TCD BM and 2 × 106 purified CD4+ T cells from either allogeneic B6 (□ and ▪) or syngeneic bm12 (▾; n = 9) donors, as described in “Materials and methods.” Allogeneic bm12 recipients were injected intraperitoneally with 1 μg/d rmIL-18 per mouse (▪, n = 17) or diluent (□, n = 17) from days -2 to +2. Syngeneic recipients also received the same dose and schedule of IL-18. Data from 3 similar experiments are combined. Percentage survival after BMT. Percentage survival, ▪ vs □; P < .0001 by Wilcoxon rank test. (B) bm1 mice underwent irradiation and transplantation with 5 × 106 TCD BM and 2 × 106 purified CD8+ T cells from allogeneic B6 or syngeneic bm1 donors. Allogeneic recipients were injected with rmIL-18 (•, n = 17) or diluent (○, n = 17), as described. Syngeneic animals (▴, n = 9) were treated with IL-18 in a similar manner. Data from 3 similar experiments are combined. Percentage survival, • vs ○; P < .0001 by Wilcoxon rank test. (C) B6 recipients were injected with IL-18 or the diluent and underwent transplantation with TCD BM and 2 × 106 CD8+ T cells from allogeneic C3H.SW (•, n = 8; ○, n = 9) or syngeneic B6 donors (▴, n = 4) as described. Percentage survival after BMT, • vs ○; P = .01 by Wilcoxon rank test.
To rule out the strain-dependent artifact, we tested the effect of IL-18 in a second model of acute GVHD mediated by CD8+ T cells induced by minor histocompatibility antigens (C3H.SW → B6).17 In this model also, IL-18 aggravated GVHD-related death (Figure 1C, • vs ○; P = .01). Thus, IL-18 reduced GVHD in a CD4+-dependent model, and it paradoxically intensified GVHD-related death in 2 different CD8+-dependent experimental models.
IL-18 increases GVHD-specific morbidity and target organ damage after MHC class I disparate BMT
We further evaluated the impact of IL-18 on several GVHD parameters in the CD8+-dependent B6 → bm1 model. Acute GVHD-specific morbidity was quantified according to the clinical scoring system described in “Materials and methods.” Figure 2A shows that clinical GVHD in animals receiving rmIL-18 was more severe than in control treated animals (P < .05 by Mann-Whitney U test from weeks 1 to 3). As expected, scores for syngeneic BMT recipients gradually returned to baseline by week 2. We next measured the serum levels of LPS, which correlated with the severity of intestinal acute GVHD.1,18 Consistent with the increased acute GVHD-related mortality and clinical severity, IL-18 injection caused significantly higher serum levels of LPS (8.3 ± 2.7 U/mL vs 2.5 ± 0.57 U/mL; P < .001; Figure 2B) compared with the controls. We also examined the small intestine and colon for histologic changes of acute GVHD using a semiquantitative pathology index, as described in “Materials and methods.” Figure 2C shows that rmIL-18 caused significantly more histopathologic GI tract damage on day +7 compared with controls (P = .002). Thus, injection of IL-18 in this CD8+-dependent acute GVHD model was associated with increased GVHD, as determined by survival, clinical, biochemical, and histopathologic parameters, dramatically opposed to its effect in CD4+-dependent systems.10
IL-18 increases GVHD-specific morbidity and target organ damage after MHC class I disparate BMT. (A) bm1 animals underwent irradiation and transplantation with 5 × 106 TCD BM cells and 2 × 106 CD8+ T cells from allogeneic B6 or syngeneic bm1 donors, as described in “Materials and methods.” IL-18 was injected into syngeneic (▴) and allogeneic recipients (•), and allogeneic control mice (○) were injected with the diluent. The animals were assessed weekly for clinical severity of acute GVHD. Data from 1 of 2 similar experiments are shown. Clinical severity was increased with the injection of IL-18. ○ vs •; ★P < .01 or ★★P < .05 by Mann-Whitney U test. (B) Serum from the recipient animals that underwent transplantation, as described (n = 4 per group), was obtained on day 7 after BMT and was analyzed. Allogeneic recipients treated with IL-18 (▤) or diluent (▪) and IL-18-injected syngeneic (□) animals are shown. Serum LPS levels are elevated after IL-18 treatment. ▤ vs ▪; ★P < .001. Results from 1 of 2 similar experiments are shown. (C) Animals that underwent transplantation (n = 4/group) were killed; small and large bowels were obtained for analysis on day 7 after BMT. Coded slides were scored semiquantitatively to assess pathologic damage, as described in “Materials and methods.” Total GVHD score; mean ± SE of the sum of scores for small bowel and colon from individual animals in each group. Allogeneic recipients treated with IL-18 (▤) or diluent (▪) and IL-18-injected syngeneic (□) animals are shown. ▤ vs ▪; ★P = .002. ▪ vs □; P = .01.
IL-18 increases GVHD-specific morbidity and target organ damage after MHC class I disparate BMT. (A) bm1 animals underwent irradiation and transplantation with 5 × 106 TCD BM cells and 2 × 106 CD8+ T cells from allogeneic B6 or syngeneic bm1 donors, as described in “Materials and methods.” IL-18 was injected into syngeneic (▴) and allogeneic recipients (•), and allogeneic control mice (○) were injected with the diluent. The animals were assessed weekly for clinical severity of acute GVHD. Data from 1 of 2 similar experiments are shown. Clinical severity was increased with the injection of IL-18. ○ vs •; ★P < .01 or ★★P < .05 by Mann-Whitney U test. (B) Serum from the recipient animals that underwent transplantation, as described (n = 4 per group), was obtained on day 7 after BMT and was analyzed. Allogeneic recipients treated with IL-18 (▤) or diluent (▪) and IL-18-injected syngeneic (□) animals are shown. Serum LPS levels are elevated after IL-18 treatment. ▤ vs ▪; ★P < .001. Results from 1 of 2 similar experiments are shown. (C) Animals that underwent transplantation (n = 4/group) were killed; small and large bowels were obtained for analysis on day 7 after BMT. Coded slides were scored semiquantitatively to assess pathologic damage, as described in “Materials and methods.” Total GVHD score; mean ± SE of the sum of scores for small bowel and colon from individual animals in each group. Allogeneic recipients treated with IL-18 (▤) or diluent (▪) and IL-18-injected syngeneic (□) animals are shown. ▤ vs ▪; ★P = .002. ▪ vs □; P = .01.
IL-18 and donor T-cell apoptosis
Fas-FasL interaction is critical for apoptosis of T cells,19 and expression of Fas by donor T cells is required for IL-18-mediated protection against GVHD dependent on donor CD4+ T cells.10 Our surprising finding of enhanced GVHD after IL-18 injections in CD8+-dependent GVHD led us to investigate the relevance of Fas-mediated apoptosis in that model. Splenocytes from bm1 recipients of B6.Ly-5a donor cells were harvested on day +5 after BMT and donor (CD45.1+) CD8+ cells were analyzed for annexin V staining to determine apoptosis. As shown in Table 1, there was no significant difference in the percentage of apoptotic donor cells between IL-18 and the control treated allogeneic recipients (P = .84). We also determined the functional relevance of Fas expression on CD4+ and CD8+ donor T cells with respect to the effects of IL-18 in these GVHD models by using Fas-deficient (lpr, H-2b) mice as BMT donors. As expected,10 the beneficial effect of IL-18 on CD4+-mediated acute GVHD was lost when Fas- deficient donors were used (Figure 3A, ▪ vs □; P = .69). Furthermore, consistent with the hypothesis that IL-18 increased Fas expression and induced greater apoptosis of donor CD4+ T cells, injection of IL-18 did not significantly increase the apoptosis of CD4+ T cells in the bm12 mice that received transplanted T cells from lpr donors (41 ± 7 vs 37 ± 9; P = NS).
Fas expression on donor T cells is required for IL-18-mediated GVHD protection in MCH class II-disparate BMT, but it does not have a role in MHC class I-dependent GVHD induced by IL-18. (A) bm12 animals underwent irradiation and transplantation with TCD BM from B6 and CD4+ T cells from allogeneic Fas-deficient lpr (H-2b) donors and were injected with IL-18 (▪, n = 6) or the diluent (□, n = 5) as in Figure 1. IL-18 had no effect on the mortality (▪ vs □, P = .69). (B) bm1 (B; •, n = 11; ○, n = 11) recipients were given 13 Gy TBI and underwent transplantation as in Figure 1, with TCD BM from B6 donor plus CD8+ T cells from Fas-deficient lpr donors. For syngeneic BMT, bm1 (▴, n = 6) recipients received TCD BM plus CD8+ cells from bm1 donors. Mice that underwent transplantation received rmIL-18 (• and ▴) or the diluent (○) from day -2 to +2, as in “Materials and methods.” Percentage survival after BMT. • vs ○; P = .0005.
Fas expression on donor T cells is required for IL-18-mediated GVHD protection in MCH class II-disparate BMT, but it does not have a role in MHC class I-dependent GVHD induced by IL-18. (A) bm12 animals underwent irradiation and transplantation with TCD BM from B6 and CD4+ T cells from allogeneic Fas-deficient lpr (H-2b) donors and were injected with IL-18 (▪, n = 6) or the diluent (□, n = 5) as in Figure 1. IL-18 had no effect on the mortality (▪ vs □, P = .69). (B) bm1 (B; •, n = 11; ○, n = 11) recipients were given 13 Gy TBI and underwent transplantation as in Figure 1, with TCD BM from B6 donor plus CD8+ T cells from Fas-deficient lpr donors. For syngeneic BMT, bm1 (▴, n = 6) recipients received TCD BM plus CD8+ cells from bm1 donors. Mice that underwent transplantation received rmIL-18 (• and ▴) or the diluent (○) from day -2 to +2, as in “Materials and methods.” Percentage survival after BMT. • vs ○; P = .0005.
Endogenous IL-18 might reduce the severity of acute GVHD by enhancing Fas-mediated apoptosis of CD4+ T cells. Therefore, the absence of Fas on CD4+ T cells from lpr donors might be expected to cause more deaths in bm12 recipients than from wild type (WT) donors. The rapidity of acute GVHD-related mortality (in less than 2 weeks) after MHC class II disparate B6 → bm12 allogeneic BMT, makes it difficult to demonstrate a statistically significant greater rate of mortality or clinical GVHD in the recipients of CD4+ T cells from lpr mice than from WT donors.
In contrast, rmIL-18 increased the severity of acute GVHD-related mortality mediated by donor CD8+ T cells even when they did not express Fas (Figure 3B, • vs ○; P = .0005). Taken together, these data demonstrate that protection from CD4+ T cell-mediated acute GVHD by IL-18 is dependent on Fas expression but that its amplification of CD8+-mediated GVHD is independent on Fas expression.
IL-18 increases proinflammatory cytokines and enhances the expansion and cytotoxic activity of donor CD8+ T cells
We next evaluated the potential mechanisms for IL-18-mediated aggravation of acute GVHD mediated by CD8+ T cells. IL-18 can induce proinflammatory cytokines and enhance cytotoxic T lymphocyte (CTL) activity.4,6 The production of cytokines such as IFN-γ and TNF-α and the expansion and cytotoxic function of donor T cells have been implicated in GVHD-related mortality.1-3,20 Therefore, we measured serum levels of IFN-γ and TNF-α on day +7 after MHC class I disparate BMT. As shown in Figure 4A, IFN-γ was markedly elevated in recipients of rmIL-18 than in the controls (P = .002). IL-18 administration significantly increased serum levels of TNF-α (P < .001; Figure 4B). IL-18 administration also significantly enhanced donor CD8+ T-cell expansion in the recipient spleens after MHC class I disparate BMT on days +7 and +14 (Figure 4C; P = .0001 and P < .0001, respectively), in contrast to its effect of reducing early donor T-cell expansion in the CD4+-mediated B6 → F1 system.10
Effect of IL-18 on serum proinflammatory cytokines, donor CD8+ T-cell expansion, and CTL activity after BMT. bm1 mice were injected with IL-18 or diluent and underwent transplantation with TCD BM and CD8+ T cells from syngeneic or allogeneic donors, as in Figure 1B. Sera from the recipient animals (n = 3/group) were obtained on day +7 after BMT and were analyzed as described in “Materials and methods.” Syngeneic plus IL-18 (□), allogeneic plus diluent (▪), and allogeneic plus IL-18 (▤). Serum levels of (A) IFN-γ and (B) TNF-α were significantly elevated in the IL-18-injected allogeneic recipients compared with allogeneic control animals (▤ vs ▪; ★P < .01). (C) Splenocytes were harvested from the recipients (n = 4/group) and labeled with anti-CD8+ PE and anti-CD45.1+ FITC. The number of donor T cells (CD45.1+CD8+) was determined by flow cytometry. IL-18 significantly increased donor CD8+ expansion (▪, allogeneic controls vs ▤, allogeneic plus rmL-18) on days 7 and 14 after BMT (★P = .01). (D) IL-18 augments allospecific CD8+ T-cell activity. B6 CD8+ T cells were cultured with bm1 stimulators in a primary mixed lymphocyte culture (MLC) with IL-18 (20 ng/mL) (▪) or the diluent (□), as described in “Materials and methods.” After 4 days of culture, CD8+ cells were assessed for cytotoxicity against bm1 concanavalin A-stimulated lymphoblasts in a 51Cr release assay at the indicated effector-target ratios. CTL activity was significantly enhanced by IL-18 (▪ vs □; ★P < .01; ★★P < .05). Error bars represent means ± SE.
Effect of IL-18 on serum proinflammatory cytokines, donor CD8+ T-cell expansion, and CTL activity after BMT. bm1 mice were injected with IL-18 or diluent and underwent transplantation with TCD BM and CD8+ T cells from syngeneic or allogeneic donors, as in Figure 1B. Sera from the recipient animals (n = 3/group) were obtained on day +7 after BMT and were analyzed as described in “Materials and methods.” Syngeneic plus IL-18 (□), allogeneic plus diluent (▪), and allogeneic plus IL-18 (▤). Serum levels of (A) IFN-γ and (B) TNF-α were significantly elevated in the IL-18-injected allogeneic recipients compared with allogeneic control animals (▤ vs ▪; ★P < .01). (C) Splenocytes were harvested from the recipients (n = 4/group) and labeled with anti-CD8+ PE and anti-CD45.1+ FITC. The number of donor T cells (CD45.1+CD8+) was determined by flow cytometry. IL-18 significantly increased donor CD8+ expansion (▪, allogeneic controls vs ▤, allogeneic plus rmL-18) on days 7 and 14 after BMT (★P = .01). (D) IL-18 augments allospecific CD8+ T-cell activity. B6 CD8+ T cells were cultured with bm1 stimulators in a primary mixed lymphocyte culture (MLC) with IL-18 (20 ng/mL) (▪) or the diluent (□), as described in “Materials and methods.” After 4 days of culture, CD8+ cells were assessed for cytotoxicity against bm1 concanavalin A-stimulated lymphoblasts in a 51Cr release assay at the indicated effector-target ratios. CTL activity was significantly enhanced by IL-18 (▪ vs □; ★P < .01; ★★P < .05). Error bars represent means ± SE.
We next evaluated the effect of IL-18 on the cytotoxic activity of CD8+ T cells. CD8+ cells from B6 mice were cultured with irradiated bm1 splenocyte stimulators for 4 days in the presence or absence of IL-18 and were then used as effector cells against 51Cr-labeled concanavalin A-stimulated splenocytes from bm1 mice. As shown in Figure 4D, IL-18 significantly augmented allospecific CD8+ CTL activity against bm1 splenic lymphoblasts (P < .05). Together, these data suggest that IL-18 aggravated GVHD in MHC class I-disparate recipients by increasing proinflammatory cytokines and enhancing allospecific donor CD8+ T-cell expansion and cytotoxic function. To further confirm the effect of enhanced allospecific cytotoxicity by IL-18, CD8+ T cells from B6 mice were incubated with irradiated bm1 splenocytes in the presence or absence of anti-IL-18 mAb, as described in “Materials and methods.” Anti-IL-18 mAb significantly reduced allospecific CD8+ CTL activity against bm1 splenic lymphoblasts at a 50:1 effector-target ratio (44.1% vs 54.4%; P < .05). These data demonstrate that IL-18 enhances the allospecific CTL of CD8+ cells and that IL-18 blockade reduces the CTL activity of these cells.
Blockade of IL-18 attenuates CD8+-mediated acute GVHD
We further evaluated the role of endogenous IL-18 on the severity of acute GVHD mediated by CD4+ and CD8+ T cells. We measured serum levels of IL-18 on day +7 after MHC class II- and class I-disparate BMT. As shown in Figure 5A, IL-18 was markedly elevated in the allogeneic bm12 and bm1 recipients compared with the syngeneic controls (P < .01). Because the results of the previous experiments suggested that IL-18 can enhance CD8+-mediated CTL, we hypothesized that endogenous IL-18 might potentiate CD8+-dependent acute GVHD-related mortality. Therefore, we neutralized IL-18 in vivo after allogeneic BMT in the MHC class I-disparate model. BMT recipients were injected with anti-IL-18 mAb (10 μg/d per mouse) or the control isotype IgG2a from day -1, 0, and every 3 days thereafter until day +21. Figure 5B shows that allogeneic BMT mice injected with anti-IL-18 mAb exhibited significantly better survival than control treated animals (▪ vs □; P = .01). Consistent with the improved survival, the clinical severity of GVHD was significantly less in anti-IL-18 mAb-treated recipients than in controls (P < .05; Figure 5C). Syngeneic BMT mice injected with the control antibody showed 100% survival, ruling out any nonspecific effects of the treatment, and all the surviving animals showed complete donor engraftment. Taken together, these data suggest that IL-18 enhances acute GVHD on MHC class I disparate BMT by enhancing the allospecific cytotoxic activity of donor CD8+ cells.
Treatment with anti-IL-18 mAb attenuates acute GVHD-related mortality and morbidity. (A) bm1 and bm12 animals underwent irradiation and transplantation with 5 × 106 TCD BM cells and 2 × 106 CD8+ and CD4+ T cells, respectively, from allogeneic B6 or syngeneic bm1 and bm12 donors, as described in “Materials and methods.” Serum from these recipient animals (n = 4/group), was obtained on day 7 after BMT and was analyzed as described in “Materials and methods.” Allogeneic bm12 (▪) and bm1 recipients (▤) and syngeneic (□) animals are shown. Serum IL-18 levels are elevated after allogeneic BMT. (B) bm1 recipients were given 13 Gy TBI and underwent transplantation with 5 × 106 TCD BM and 3 × 106 CD8+ cells from B6 donors, as in Figure 1B. Allogeneic recipient animals were injected intraperitoneally with 10 μg/d anti-IL-18 mAb (▪, n = 14) or the isotype IgG2a (□, n = 14) from day -1, 0, and every 3 days thereafter until the third week (total, 9 doses). Syngeneic recipients (▵, n = 6) underwent transplantation with cells from bm1 donors and were injected with the isotype IgG2a following the same schedule. Data of 2 individual experiments are combined. (B) Percentage survival after BMT. ▪ vs □; P = .01 by Wilcoxon rank test. (C) Animals were scored for clinical GVHD, as described in “Materials and methods.” ▪ vs □; ★P < .01 or ★★P < .05 by Mann-Whitney U test. Error bars represent ± SE.
Treatment with anti-IL-18 mAb attenuates acute GVHD-related mortality and morbidity. (A) bm1 and bm12 animals underwent irradiation and transplantation with 5 × 106 TCD BM cells and 2 × 106 CD8+ and CD4+ T cells, respectively, from allogeneic B6 or syngeneic bm1 and bm12 donors, as described in “Materials and methods.” Serum from these recipient animals (n = 4/group), was obtained on day 7 after BMT and was analyzed as described in “Materials and methods.” Allogeneic bm12 (▪) and bm1 recipients (▤) and syngeneic (□) animals are shown. Serum IL-18 levels are elevated after allogeneic BMT. (B) bm1 recipients were given 13 Gy TBI and underwent transplantation with 5 × 106 TCD BM and 3 × 106 CD8+ cells from B6 donors, as in Figure 1B. Allogeneic recipient animals were injected intraperitoneally with 10 μg/d anti-IL-18 mAb (▪, n = 14) or the isotype IgG2a (□, n = 14) from day -1, 0, and every 3 days thereafter until the third week (total, 9 doses). Syngeneic recipients (▵, n = 6) underwent transplantation with cells from bm1 donors and were injected with the isotype IgG2a following the same schedule. Data of 2 individual experiments are combined. (B) Percentage survival after BMT. ▪ vs □; P = .01 by Wilcoxon rank test. (C) Animals were scored for clinical GVHD, as described in “Materials and methods.” ▪ vs □; ★P < .01 or ★★P < .05 by Mann-Whitney U test. Error bars represent ± SE.
IL-18 receptor 1-deficient (IL-18r1-/-) donor T cells have differential effects on CD4+- and CD8+-mediated GVHD
We next used a genetic approach to evaluate and confirm the paradoxical effect of IL-18 in acute GVHD mediated by CD4+ and CD8+ T cells. Our previous data led us to hypothesize that IL-18 would affect donor T cells and that, therefore, any regulatory effects of IL-18 would be lost when CD4+ T cells did not express the IL-18 receptor (resulting in more deaths), whereas the opposite would occur in a CD8+-mediated system. Because of the rapid GVHD-related mortality in the bm12 recipients after allogeneic BMT, to better evaluate the impact of endogenous IL-18 on CD4+ mediated GVHD-related mortality, we used the B6 into B6D2F1 model in which GVHD-related mortality occurs at a slower rate but is critically dependent on CD4+ T cells.11
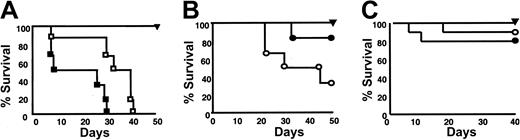
Figure 6A shows exacerbation of mortality in CD4+-mediated GVHD (B6 → B6D2F1) when 2 × 106 spleen T cells from IL-18 receptor-1-deficient (IL-18r1-/-) mice and 5 × 106 TCD BM from wild-type B6 mice were used as donors (P = .01). Conversely, the mortality rate was attenuated in the CD8+-dependent B6 → bm1 system using IL-18r1-/- donors (Figure 6B; P = .05). Although CD4+ T cells are critical for mortality after B6 into F1 transplantation, we further determined whether administering IL-18 would exacerbate GVHD when F1 mice undergo transplantation with purified B6 CD8+ T cells.11 IL-18 administration had no significant effect on GVHD-related mortality at the end of the 40-day observation period, when the F1 recipients underwent transplantation with B6 CD8+ T cells and TCD BM compared with controls (Figure 6C; 80% vs 90%; P = NS). Together these data demonstrate that different subsets of donor T cells respond differentially to IL-18 production in vivo and that the predominance of one subset or another can cause diametrically opposite results in the outcome of acute GVHD severity.
IL-18 receptor 1-deficient donor T cells have differential effects on CD4+- and CD8+-mediated acute GVHD-related mortality. (A) B6D2F1 mice underwent irradiation with 13 Gy TBI and transplantation with 5 × 106 TCD BM from allogeneic wild-type B6 donors plus 2 × 106 CD3+ T cells from wild-type B6 or IL-18r1-/-mice, respectively (□, n = 6; ▪, n = 6). Syngeneic recipients (▴, n = 5) underwent transplantation with cells from F1 donors. Data from 1 of 2 similar experiments are shown. Percentage survival after BMT in allogeneic recipients □ vs ▪; P = .01. (B) bm1 underwent irradiation and transplantation with TCD BM from allogeneic wild-type B6 and 2 × 106 CD8+ T cells from wild-type B6 (○, n = 6) or IL-18r1-/-mice (•, n = 6). Syngeneic recipients (▴, n = 3) underwent transplantation, as described in “Materials and methods.” Data from 1 of 2 experiments are shown. Percentage survival of allogeneic recipients after BMT, ○ vs •; P = .05. (C) B6D2F1 mice underwent irradiation with 11 Gy TBI and transplantation with 5 × 106 TCD BM and were purified with 2 × 106 CD8+ T cells from allogeneic B6 donors and were injected with IL-18 (•, n = 10) or the diluent (○, n = 10), as described in “Materials and methods.” Syngeneic recipients (▾, n = 4) underwent transplantation with cells from F1 donors. Percentage survival after BMT in allogeneic recipients ○ vs •; P = NS.
IL-18 receptor 1-deficient donor T cells have differential effects on CD4+- and CD8+-mediated acute GVHD-related mortality. (A) B6D2F1 mice underwent irradiation with 13 Gy TBI and transplantation with 5 × 106 TCD BM from allogeneic wild-type B6 donors plus 2 × 106 CD3+ T cells from wild-type B6 or IL-18r1-/-mice, respectively (□, n = 6; ▪, n = 6). Syngeneic recipients (▴, n = 5) underwent transplantation with cells from F1 donors. Data from 1 of 2 similar experiments are shown. Percentage survival after BMT in allogeneic recipients □ vs ▪; P = .01. (B) bm1 underwent irradiation and transplantation with TCD BM from allogeneic wild-type B6 and 2 × 106 CD8+ T cells from wild-type B6 (○, n = 6) or IL-18r1-/-mice (•, n = 6). Syngeneic recipients (▴, n = 3) underwent transplantation, as described in “Materials and methods.” Data from 1 of 2 experiments are shown. Percentage survival of allogeneic recipients after BMT, ○ vs •; P = .05. (C) B6D2F1 mice underwent irradiation with 11 Gy TBI and transplantation with 5 × 106 TCD BM and were purified with 2 × 106 CD8+ T cells from allogeneic B6 donors and were injected with IL-18 (•, n = 10) or the diluent (○, n = 10), as described in “Materials and methods.” Syngeneic recipients (▾, n = 4) underwent transplantation with cells from F1 donors. Percentage survival after BMT in allogeneic recipients ○ vs •; P = NS.
Discussion
IL-18 is known to induce TH1 differentiation and to enhance CTL function,4,6 each of which has been implicated in the pathogenesis of GVHD. IL-18 is elevated during acute GVHD,7,8 but paradoxically it can regulate acute GVHD in a donor/recipient strain combination in which mortality is critically dependent on donor CD4+ T cells (B6 → B6D2F1).10,11 We confirm that IL-18 regulates acute GVHD in a CD4+-dependent, MHC class II-disparate (B6 → bm12) model, but, in stark contrast, it aggravates acute GVHD in a CD8+-dependent, MHC class I-disparate (B6 → bm1) model. Amplification of acute GVHD-related mortality by IL-18 was confirmed by biochemical and histopathologic markers and was observed in a second CD8+-dependent model of GVHD induced by minor histocompatibility antigens (C3H.SW → B6).17 This difference is attributed to the fact that IL-18 causes Fas-dependent apoptosis of donor CD4+ T cells but not donor CD8+ T cells. In fact, IL-18 administration increased the serum levels of proinflammatory cytokines and enhanced the expansion and CTL function of donor CD8+ T cells, thus amplifying clinical GVHD. Furthermore, neutralizing IL-18 by administering anti-IL-18 mAbs decreased mortality in the CD8+-dependent system, a result that contrasts to CD4+-mediated acute GVHD.10 Finally, this differential effect of IL-18 on CD8+- and CD4+-mediated GVHD was also confirmed by using T cells from IL-18 receptor 1-/- donor mice. These results explain previous observations that IL-18 can reduce GVHD, but only when CD4+ T cells are the primary mediators of GVHD, and can enhance only CD8+-mediated graft-versus-leukemia (GVL). Thus, IL-18 therapy might reduce CD4+-mediated clinical GVHD and still preserve CD8+-mediated GVL responses. However, in a recent study, Arnold et al8 used IL-18-binding protein, a soluble IL-18 decoy receptor, to neutralize IL-18 in a nonirradiated model of acute GVHD and observed no change in GVHD severity. Thus, it is possible that significantly different results might be obtained in sublethal or nonirradiation conditions. The impact of conditioning on Fas/FasL-deficient donor T cell-mediated GVHD also remains to be determined. Therefore, because clinical GVHD is mediated by CD4+ and CD8+ T cells and the conditions for predominantly CD4+- or CD8+-mediated GVHD and GVL are yet to be determined in humans, caution must be exercised in clinical application of IL-18 after allogeneic BMT.
Surface expression of CD4+ or CD8+ is commonly used to identify T-cell subsets that recognize antigen presented by MHC class II or class I, respectively.21,22 Rather than simply defining cells with different functions, it is now known that these CD4+ and CD8+ T-cell subsets have differential properties for induction of apoptosis, cell survival, and cytokine responsiveness.23 Indeed, acute GVHD mediated by CD4+ T cells can be inhibited by the early administration of TH1 cytokines such as IFN-γ,24 IL-2,25 IL-12,26 and IL-18.10 After hematopoietic stem cell transplantation, alloreactive antihost T cells expand but then undergo Fas-dependent apoptosis after a brisk proliferating phase.27 TH1-inducing cytokines such as IL-1228 and IL-1810 increase Fas expression and accelerate apoptosis, thus appearing to impart some of their beneficial effects by perturbation of early donor T-cell expansion. Of great interest is the fact that these TH1-inducing cytokines have been shown to inhibit CD4+-dependent GVHD while preserving the CD8+-mediated GVL effect after allogeneic BMT in these models.25,26,29 Together, these data suggest that an in vivo alloreaction of CD4+ cells was more affected than that of CD8+ cells by the administration of exogenous TH1 cytokines. However, CD4+ and CD8+ T cells are critical for GVHD after clinical allogeneic BMT. Therefore, whether treatment with TH1-inducing cytokines results in the reduction of GVHD in a predominantly CD8+-dependent BMT model has not been evaluated. Our data show that IL-18 regulated the in vivo alloreactivity of CD4+ cells but amplified the effect on CD8+ T cells, resulting in more severe GVHD.
Fas signaling plays an important role in apoptosis of host-reactive T cells after BMT,27 but it does not play a similar role in modulating the apoptosis of CD4+ and CD8+ T-cell subsets. Analyses of T-cell responses to various antigens have shown that Fas usually plays a dominant role in apoptosis of CD4+ T cells.12,30,31 In contrast, the role of Fas in the apoptosis of CD8+ cells has been shown to be negligible.12,32-34 Because Fas signaling is less important for CD8+ cell apoptosis, and given that enhanced Fas-mediated apoptosis of donor T cells induced by IL-18 is critical for regulating CD4+-mediated GVHD, it is likely that this protective mechanism was absent in the MHC class I-disparate BMT model. It is intriguing that IL-18 administration did not cause a significant increase in CD8+ T-cell apoptosis despite increasing serum levels of TNF-α. IL-18 can increase the levels of Akt and GADD45, which promote cell survival, and therefore might regulate the TNF-α-mediated apoptosis of donor CD8+ T cells.35,36 However, the exact mechanism(s) remains to be determined.
IL-18 induces proinflammatory cytokines, such as IFN-γ, TNF-α, and IL-1,5,37-40 that have been implicated in GVHD pathophysiology,1,2 and our data suggest that the amplification of acute GVHD by CD8+ T cells after the administration of IL-18 might in part be caused by the increased production of proinflammatory cytokines. In addition, IL-18 significantly enhanced donor CD8+ cell expansion after transplantation and up-regulated the antihost cytotoxic activity of donor CD8+ T cells, which could also intensify the severity of acute GVHD.1,2 These data are consistent with other reports that demonstrate increased CTL activity induced by IL-18.9,15 Furthermore, anti-IL-18 mAb reduced the in vitro CTL activity and contributed to attenuated GVHD-related mortality, suggesting that IL-18 aggravates GVHD by enhancing the CTL activity of donor CD8+ T cells. To determine the role of IL-18-induced cytotoxic mechanisms in mediating CD8 GVHD, B6 perforin-deficient CD8+ T cells were used as donors and bm1 mice as recipients. Bm1 animals injected with IL-18, though, showed a greater trend toward mortality, but it did not reach statistical significance compared with controls (60% v 80%; P = NS). These results suggest that IL-18 might increase GVHD-related mortality at least in part by enhancing the CTL function of donor CD8 T cells. Experiments are in progress to determine the relative contributions of the enhanced proinflammatory cytokine secretion and the CD8+ cytotoxic function in IL-18 aggravation of GVHD.
Recent experimental data demonstrate that naive but not memory donor T cells cause GVHD.41,42 However, the effect of IL-18 on naive, effector, and memory alloreactive CD4+ and CD8+ T cells is not known. Future studies will determine the effect of IL-18 on these T-cell subsets to further define the role of IL-18 in the immunobiology of acute GVHD.
In summary, we demonstrate a paradoxical role for IL-18 in CD4+ and CD8+ T cell-mediated GVHD by the injection of exogenous IL-18, the blockade of endogenous IL-18, and the absence of IL-18 receptor 1 on donor T cells. These findings underscore the importance of the diverse effects a single cytokine, IL-18, can have in the complex biology of GVHD that is regulated by variable cytokine patterns at different time points. Therefore, caution must be exercised before applying cytokine manipulation in general to the clinical situation in which both T-cell subsets play an important role in mediating GVHD.
Prepublished online as Blood First Edition Paper, July 27, 2004; DOI 10.1182/blood-2004-02-0763.
Supported by National Institutes of Health grants K08 AI052863-01 (P.R.) and PO1 CA 49542 (J.L.M.F.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.