Abstract
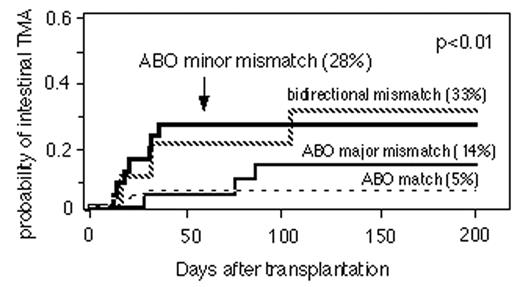
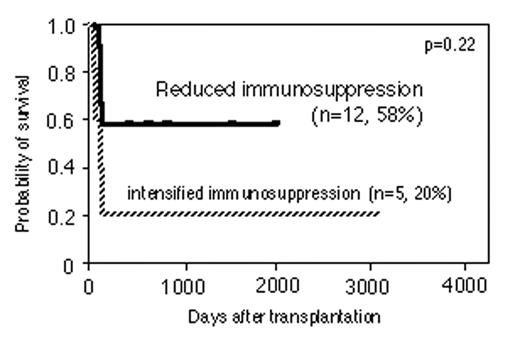
Intestinal thrombotic microangiopathy (TMA) after allogeneic stem cell transplantation is emerging as a major clinical issue, which is different from aGVHD in pathogenesis and clinical management. We performed a retrospective analysis of 140 pediatric patients with acute leukemia (82 ALL and 58 AML) who underwent allogeneic stem cell transplantation in Japanese Red Cross Nagoya First Hospital from 1991 to 2003 (69 from HLA matched sibling, 13 from HLA mismatched family donors and 58 from unrelated volunteer donors). Blood type was matched in 78 patients and mismatched in 62 patients (25 in minor , 26 in major and 11 in bidirectional). Seventeen patients developed intestinal TMA with a cumulative incidence of 13%. The median time to onset was 28 days (range, 10–104 days). Intestinal TMA was defined histopathologically by colonoscopic biopsies in 7 patients and bloody diarrhea and laboratory findings. Intestinal TMA occured in 28% of ABO minor mismatched transplantation, 32.5% of bidirectional, 14.4% of major mismatched and 5.8% in matched transplantation (p<0.01)(Fig1)p. In multivariate analysis, ABO minor mismatched transplants (HR=5.3, 95%CI 1.4–19.7, p=0.01), HLA mismatched related donors (HR=16.6, 95%CI 1.6–173.3, p=0.02 ) and unrelated donors (HR=16.4, 95%CI 2.0–130.6, p<0.01 ) were significantly associsted with the risk of intestinal TMA. The estimated 5-year overall survival (OS) was 47.1% in intestinal TMA patients compared with 56.7% in patients with no intestinal TMA (p=0.18). Intensified immunosuppressants for the treatment of intestinal TMA (n=5) lead to poor OS (20%). Seven out of 12patients (58%) who had reduced immunosuppressant were still alive with a median follow-up of 24 months (p=0.29). Our findings suggest that ABO mismatched transplantation, especially ABO minor mismatch, is a risk factor for developing intestinal TMA. Successful treatment for intestinal TMA by diminishing immunosuppressive drugs is warranted.
Author notes
Corresponding author