Abstract
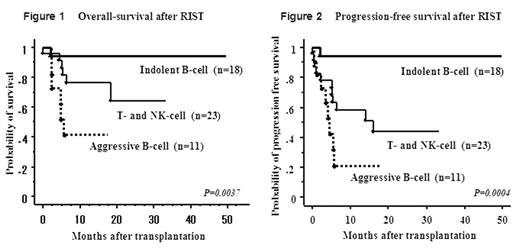
Since allogeneic hematopoietic stem cell transplantation (HSCT) is reported to have a high mortality rate for advanced lymphoma patients, less toxic technique has been expected. We evaluated the safety and preliminary efficacy of RIST in patients with advanced NHL on the basis of the WHO classification. We retrospectively reviewed the medical records of 52 patients with NHL who underwent RIST from February 2000 to April 2004 at National Cancer Center Hospital. The median age of the patients at the time of RIST was 50 years (range, 26 to 67 years). Eighteen patients had indolent B-cell lymphoma (follicular 16, lymphoplasmacytic 1, chronic lymphocytic leukemia 1), 11 had aggressive B-cell lymphoma (diffuse large B cell 8, mediastinal large B cell 2, mantle cell 1), and 23 had T-cell and NK-cell lymphoma (adult T-cell leukemia/lymphoma 12, peripheral T-cell, unspecified 8, extranodal NK/T-cell 1, enteropathy-type T-cell 1, anaplastic large cell 1). The median number of prior chemotherapy regimens was 3 (range, 1–8), and 17 (33%) patients had experienced autologous HSCT before RIST. Thirty (58%) patients had progressive/refractory disease at the time of transplantation. The RIST regimens were fludarabine- (n=47) and cladribine-based (n=5), of whom 9 patients received additional anti-thymocyte globulin. Stem cell sources were related peripheral blood (n=36), unrelated bone marrow (n=8), and unrelated cord blood (n=8). GVHD prophylaxis was cyclosporin alone (n=36) or cyclosporin and short-term methotrexate (n=16). The median duration of follow-up after transplantation was 309 days (range, 2 to 1492 days). Except for one patient who died early on day 2, all patients showed sustained engraftment. Acute GVHD gradeII–IV developed in 32 patients (62%), gradeIII–IV developed in 12 (23%) and chronic GVHD developed in 29 (56%). The day-100 TRM rate was 6%, including sepsis (n=2) and liver failure (n=1). The estimated one-year overall-survival and estimated progression-free survival rates were 75% and 63%, respectively, for all patients; 94% and 94% for indolent B cell, 76% and 58% for T or NK cell and 42% and 21% for aggressive B cell, as shown in Figures 1 and 2. (P = 0.0037 and, 0.0004 by log-rank test). In our analysis, GVHD did not clearly affect the clinical response or survival. Sustained engraftment and the low TRM rate indicate that RIST is feasible in patients with relapsed or refractory NHL. Although this is a preliminary study with a heterogeneous population and a short follow-up, the results suggest that RIST might be a promising procedure in relapsed or refractory NHL, especially in indolent B-, T- and NK-NHL. Further large-scale prospective studies are warranted.
Author notes
Corresponding author