Comment on Lacayo et al, page 2646
In this issue, Lacayo and colleagues describe a successful approach to identify clinically useful gene expression signatures for high-risk cancer patients, using acute myeloid leukemias with mutated FLT3 tyrosine receptor genes as a model.
As we move forward into the postgenome era, the analysis of gene expression profiles of tumor cells promises to pinpoint, at diagnosis, cancer patients with the highest risk of relapse. Once identified, such patients might benefit from trials of novel but often more toxic therapies, with the recognition that alternative treatments initiated at diagnosis have the greatest possibility of success. This progress is welcome because it addresses a major dilemma faced by all cancer therapists: how can one be certain that all patients selected by a particular gene expression profile are high-risk so that treatment can be changed from the very beginning? While major advances will accrue by improving therapy for patients predicted to have resistant disease, it is very important not to jeopardize the outcomes of lower-risk patients, who would benefit from standard regimens that are relatively safe and likely to be effective for them.
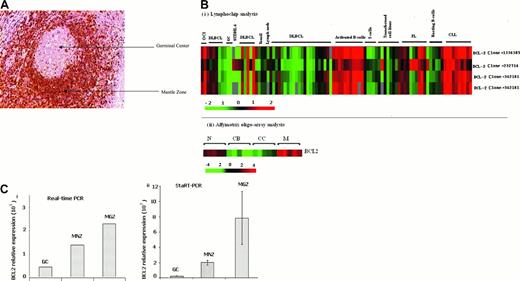
In the best of worlds, defects in a single gene or signal transduction pathway would predict the treatment responsiveness of a large number of leukemia patients with a high level of statistical certainty, but that has hardly been the case. Instead, we are finding that the discrimination of truly high-risk leukemias and other tumors can be a daunting task. This challenge is well illustrated by recent findings in acute myeloid leukemias (AMLs) with mutated FLT3 tyrosine kinase receptor genes.1-4 FIG1
Hierarchic clustering FLT3-MU samples supervised by clinical outcome. See the complete figure in the article beginning on page 2646.
Hierarchic clustering FLT3-MU samples supervised by clinical outcome. See the complete figure in the article beginning on page 2646.
In the current issue of Blood, Lacayo and colleagues provide an elegant demonstration of how microarrays are being used to identify clinically useful high-risk gene expression signatures. They chose a subgroup of childhood AML patients whose leukemic blast cells harbored activating mutations of the FLT3 gene. It is already known that the large subgroup of AML patients whose blast cells harbor FLT3 mutations includes an over-representation of high-risk cases, but it is also appreciated that a FLT3 mutational status alone is not sufficient to predict the early emergence of resistant disease.1,2 Thus, the authors picked an ideal circumstance in which to test the clinical utility of gene profiling to reliably identify high-risk patients. By relying on a multifaceted biostatistical analysis of microarray data from 36 patients with FLT3 mutations (among the 81 patients from a single Pediatric Oncology Group trial), Lacayo and colleagues were able to identify a robust signature for high-risk patients, characterized by increased expression of the RUNX3 gene (also known as AML2) and decreased expression of ATRX, which encodes an SWI/SNF protein involved in regulating patterns of gene expression and DNA methylation. This signature, which includes cases with each of the 2 types of FLT3 mutations (internal tandem duplications [ITDs] and activating loop point mutations), did not identify every patient destined to fail therapy but, it is important to note, did pinpoint a subgroup whose long-term rate of continuous complete remission was only about 5% (see Figure 3 of the Lacayo et al article). The authors show that this signature can be accurately detected by widely available quantitative reverse transcriptase-polymerase chain reaction (RT-PCR) approaches, as well as by the Stanford microarray platform, which should greatly simplify the reproducible detection of this high-risk signature by investigators treating AML patients. Once these results are independently confirmed and, ideally, extended to adult patients with AML, patients with this signature can be considered for alternative therapies, which may include newly developed drugs or antibodies that inhibit the activity of the FLT3 kinase.1-5
Virtually nothing is known about the mechanisms by which high levels of RUNX3 combined with low levels of ATRX could influence the chemosensitivity of leukemias with activating FLT3 mutations. Certainly, these genes encode intriguing transcriptional regulatory proteins that may well be involved in the pathogenesis and treatment responsiveness of AML. Approaches that could be used to investigate these mechanisms include RNAi knockdown (in the case of RUNX3) or vector-induced overexpression (ATRX) followed by microarray and phenotypic analysis. In-depth analysis following up on intriguing microarray studies, such as the one by Lacayo and colleagues and other recently published reports,6,7 should provide insight into the molecular pathways that sustain the growth and survival of leukemic cells and eventually lead to new agents for challenging diseases like AML.