Abstract
The stromal compartments of hematopoietic organs (eg, spleen) are known to influence the viability and growth of diseased hematopoietic progenitors. Here we have used Friend murine leukemia virus (F-MuLV)–induced erythroleukemia to investigate factors of the splenic microenvironment that may make it fertile for the expansion and survival of malignant erythroblasts. We found that splenectomized, erythroleukemic mice exhibited extended survival compared with age-matched sham controls. In vitro, the proliferation of primary erythroleukemic cells cocultured with leukemic-derived splenic adherent cells or their conditioned media was found to be significantly higher than that observed in cocultures with healthy-derived adherent splenic cells. Cytokine protein arrays revealed that F-MuLV–infected splenocytes secreted elevated levels of interleukin-6 (IL-6), vascular endothelial growth factor-A (VEGF-A), macrophage chemoattractant protein-5 (MCP-5), soluble tumor necrosis factor receptor-1 (sTNFR1), IL-12p70, tumor necrosis factor-α (TNF-α), and IL-2 over normal splenocytes. Medium supplemented with both VEGF-A and MCP-5 could sustain proliferation of primary erythroleukemic cells in vitro, and significant proliferative suppression was observed upon addition of neutralizing antibodies to either of these factors. Furthermore, in vivo administration of a neutralizing antibody to VEGF-A extended survival times of erythroleukemic mice in comparison with controls. These findings suggest that VEGF-A and MCP-5 are potentially pivotal paracrine mediators occurring within the diseased splenic microenvironment capable of promoting disease acceleration and expansion of erythroleukemic blasts.
Introduction
Solid tumors can be viewed as abnormal organs composed of 3 general cell types: tumor cells, tumor-associated endothelium, and the stroma (reviewed by Liotta and Kohn1 and Wernert2 ). The latter serves to nourish and support the growing tumor cell mass, respectively. Similarly, the stroma of hematopoietic organs is known to support the processes of normal and malignant hematopoiesis (ie, “liquid” tumors or leukemias).3,4 In both cases, support cells are essential for tumor growth and metastasis. However, the changes occurring in their associated endothelial and stromal cells that accelerate the disease process are poorly characterized.
A number of hematologic malignancies including chronic lymphocytic leukemia (CLL), marginal zone non-Hodgkin lymphoma (NHL), hairy cell leukemia (HCL), and chronic myelogenous leukemia (CML) display varying propensities for pathological enlargement of the spleen (splenomegaly).5-7 Thus, splenic involvement appears to be stage specific for each type of disease and is generally considered to take place during the mid to late stages. Particularly for CML, splenomegaly is evident during accelerated disease and blast crisis.8 Surgical intervention (splenectomy) is typically reserved for patients who are experiencing extreme discomfort or who may benefit from a laparotomy if such a procedure is thought to be useful in governing the therapeutic strategy.8 These clinical observations suggest mechanistic growth response elements contributed by the spleen, which remain rather enigmatic.
Friend murine leukemia virus (F-MuLV)–induced erythroleukemia has been used for decades as a model for analyzing neoplastic transformation, leukemia progression, genetic susceptibility to cancer, and, more recently, erythroid differentiation.9,10 It is well established that following inoculation of neonates of susceptible murine strains with F-MuLV, infected erythroblasts depart the bone marrow and sequester within the spleen,11 followed by the development of foci over the following 2 weeks.12 It has been previously reported that the spleen plays a role in the susceptibility and resistance of the host to Friend virus infection from the polycythemia variant of Friend virus (FVP).13
Recent studies have shown that several factors are important for leukemic proliferation, some of which are produced by the bone marrow stroma.14-16 For example, leukemic cells usually differentiate in the presence of erythropoietin (EPO). However, if such cells are cocultured with bone marrow stroma in the presence of EPO, they are prevented from undergoing terminal differentiation.14 These results suggest that factors in the bone marrow stroma can block EPO-induced terminal differentiation of erythroblasts. Therefore, because splenic involvement is prevalent in several hematologic disorders of mice and humans, we decided in the current study to investigate whether the splenic stroma affects the erythroleukemic overgrowth modeled by Friend disease.
Here we have studied the changes occurring in the microenvironment of the spleen that could potentially accelerate the pathological course of Friend disease, a model known to exhibit considerable splenic involvement. We report here that among several pertinent angiogenesis/inflammatory cytokines assayed in an in vitro system obtained from F-MuLV–infected splenocytes, vascular endothelial growth factor-A (VEGF-A) and macrophage chemoattractant protein-5 (MCP-5) appear to be key players contributing to the accelerated overgrowth of erythroleukemic cells. We also show that erythroleukemic mice treated with a neutralizing antibody against VEGF-A survive longer than controls. Hence, the splenic stroma of erythroleukemic mice produces proangiogenic/inflammatory factors that contribute to the progression of the disease.
Materials and methods
Murine splenectomy
Viral lysates of the replication-competent NB-tropic F-MuLV were prepared through repeated culturing of the fibroblastic, clone-B cell line in minimum essential medium-alpha (αMEM) (Gibco, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS) (Gibco) and penicillin/streptomycin at 1000 U/mL (Gibco). Four-week-old BALB/c mice infected at birth with F-MuLV were divided into 2 groups: a splenectomized group and sham controls. All procedures were conducted according to institutional guidelines. Briefly, mice were anesthetized and injected with the analgesic buprenorphine. A 1 cm midline incision through the skin and musculature was made just below the sternum, followed by exposure of the spleen. The spleen was then gently retracted, freed, and removed by cauterization. Musculature and subcutaneous tissues were closed by absorbable sutures and metal wound clips, respectively. Similarly, sham control mice underwent this operative procedure, only with spleens remaining intact.
Tumor isolation and in vitro expansion of healthy- and leukemic-derived splenic adherent cells and primary erythroleukemic cells
Briefly, BALB/c neonates (n = 3) were infected with the replication-competent helper virus F-MuLV 1 day after birth to induce erythroleukemia (Friend disease) (reviewed by Lee et al10 ). Age-matched noninfected littermates (n = 3) served as controls. After 9 weeks, leukemic mice with palpable spleens and decreased hematocrit values, both measured to ascertain leukemic burden (volume expansion), were sampled. At this point the spleen is highly enriched (more than 90%) for leukemic erythroblasts. Mice were anesthetized with 4% isoflurane, and spleens were excised and placed in sterile 1 × phosphate-buffered saline (PBS), followed by mechanical homogenization using a mortar and pestle and 2 washes in 1 × PBS. Cells were plated in αMEM containing 10% FBS, 10 ng/mL stem cell factor (SCF), 1 U/mL EPO, and 10 ng/mL epidermal growth factor (EGF) and allowed to expand for 3 to 4 days until adherent and suspension cells were easily discernible. At this time, 50% of the media was exchanged with fresh media every 3 days. After 3 to 5 such cycles, suspension cells were then considered as primary erythroleukemic cells. Such procedures were carried out according to a previously described method so as to obtain splenic adherent cells in culture.17 Following separation of suspension from adherent cells, erythroleukemic cells were centrifuged at 200g for 5 minutes. These cells were then plated and cultured in fresh medium, medium derived from adherent cell line cultures, or similarly with the addition of various cytokines and neutralizing antibodies as described in “Recombinant mouse proteins and antibodies.”
Detection of viral integration into erythroleukemic splenocytes
Genomic DNA was extracted from cultured cells using DNA Mini Kit (Qiagen, Mississauga, Ontario, Canada). Polymerase chain reaction (PCR) was performed with 2 μL DNA, 2 units of Taq DNA polymerase (Invitrogen, Burlington, Ontario, Canada), 10 mM deoxyribonucleoside triphosphate (dNTP), 100 pg of each primer, and the provided PCR reaction buffer. The primers were designed from the Friend virus envelope (env) that provides a product of about 500 base pairs (bp). Sense: 5′-CCTTGGCTATCCGGTTTACA-3′. Antisense: 5′-GGACAGGGTCAGCTTGTGTT-3′. The reaction was allowed to proceed at 94°C for 1 minute, at 55°C for 45 seconds, and at 72°C for 1 minute in each cycle. The amplification was carried on for 30 cycles in a Peltier Thermal Cycler (MJ Research, Watertown, MA).
Recombinant mouse proteins and antibodies
For in vitro experiments, concentrations of recombinant mouse cytokines were 4 ng/mL interleukin-6 (IL-6) (BD Pharmingen, San Diego, CA), 10 ng/mL MCP-5 (R&D Systems, Minneapolis, MN), 10 ng/mL tumor necrosis factor-α (TNF-α) (R&D Systems), and 4 ng/mL VEGF164 (R&D Systems), as recommended by the manufacturer. Neutralizing antibodies against mouse MCP-5, TNF-α, and VEGF164 (R&D Systems) were used at concentrations of 5 μg/mL, 0.5 μg/mL, and 5 μg/mL, respectively, according to manufacturer's recommendations or following established dose response analyses. For in vivo experiments, a neutralizing antibody against mouse VEGF-A or goat immunoglobulin G (IgG) as a control (R&D Systems) was administered intraperitoneally twice weekly over a 2-week period at a concentration of 50 μg per 200 μL PBS per mouse as described elsewhere.18
Proliferation assays
Unless indicated otherwise, primary erythroleukemic cell lines were cultured at a starting density of 1 × 104 cells per milliliter in conditioned αMEM (10% FBS, 10 ng/mL SCF, 1 U/mL EPO, and 10 ng/mL EGF). Cells were allowed to grow over a period of 72 hours, during which time cell counts and viability were assessed every 24 hours by the method of trypan blue exclusion (Gibco) using a hemocytometer. Similarly, these experiments were repeated and results confirmed using the method of AlamarBlue reduction assay (BioSource International, Camarillo, CA).19 In some experiments erythroleukemic (suspension) cells were cocultured with adherent cells to ascertain that stimulatory factors secreted by the adherent cell population were partly responsible for the leukemic overgrowth evident in the Friend disease model of erythroleukemia. In other experiments, cytokines or neutralizing antibodies to known angiogenesis-promoting growth factors or cytokines—namely, those determined to be differentially regulated by cytokine profiling—were added to the medium of primary cells, and growth kinetics were then measured.
Protein cytokine antibody array
Starvation medium (2% FBS, 100 ng/mL SCF, 1 U/mL EPO, and 10 ng/mL EGF) was precultured for 24 hours with murine leukemic-derived splenic adherent cells (LDSACs) or from healthy-derived splenic adherent cells (HDSACs) and then assayed for cytokines using TransSignal RayBio Mouse Cytokine Antibody Array Kit (Panomics, Redwood City, CA) according to manufacturer's instructions. Briefly, starvation conditioned medium was overlaid onto stromal cells and incubated for 24 hours, followed by collection of the medium, into which the array membrane was submerged. After 24 hours, the membrane was washed with wash buffer and incubated for 2 hours with a secondary sandwich-labeled anticytokine mix of antibodies. Streptavidin–horseradish peroxidase (streptavidin-HRP) conjugate was then incubated for 30 minutes followed by several washes with Tris (tris(hydroxymethyl)aminomethane)/Tween-buffered saline (TTBS). A chemiluminescent reaction was detected on film by autoradiography. Differential signals correspond to differences between the samples in cytokine activities, and the results of densitometry (Bio-Rad, Mississauga, Ontario, Canada) were plotted for all groups following normalization.
Quantification of splenic-associated endothelial cells
Either LDSAC or HDSAC populations were twice washed carefully with PBS to discard suspension cells. Cells were then collected by scraping, pelleted at 200g for 5 minutes, and then resuspended in fluorescence-activated cell sorting (FACS) buffer (0.5% bovine serum albumin [BSA] and 10 mM EDTA [ethylenediaminetetraacetic acid] in PBS). Monoclonal antibodies, anti-CD45 conjugated to peridinin chlorophyll protein (PerCP), anti–flk-1 conjugated to phycoerythrin (PE), and anti-CD13 conjugated to fluorescein isothiocyanate (FITC) (BD Pharmingen), were then added to cell suspensions and incubated for 30 minutes. Cells were then washed twice with FACS buffer and evaluated by a FACSCalibur (Becton Dickinson, San Jose, CA) with acquisition of at least 10 000 cells per sample. Endothelial cells were defined as negative for hematopoietic marker CD45 and positive for endothelial markers flk-1 and CD13.20
Qualitative and quantitative assessment of the splenic microvasculature
Spleens from healthy and erythroleukemic mice were harvested and fixed in 10% buffered formalin, and paraffin sections were prepared, followed by immunostaining as in a previously described protocol21 with the following modifications. Purified rat antimouse CD144 (vascular endothelial [VE]-cadherin) (Santa Cruz Biotechnology, Santa Cruz, CA) was incubated with 1:200 dilution in antibody-diluting buffer (Dako, Carpinteria, CA) for 2 hours at room temperature. After several washes with PBS, a secondary antibody, antirat IgG (Jackson ImmunoResearch Laboratories, Bar Harbor, ME), was incubated for 30 minutes at room temperature, followed by streptavidin/biotin labeling using HistoStain SP Kit (Zymed, South San Francisco, CA). Samples were then examined by light microscopy (Carl Zeiss Vision, Toronto, Ontario, Canada) using a 20 × objective lens to provide magnification of 200 ×. Images were acquired using an AxioCam camera and Axiocision 4 software (Carl Zeiss Vision). For quantification purposes the immunostained sections of both healthy and leukemic spleens were scanned and assessed for vessel area using Adobe Photoshop 6 software (Adobe Systems, San Jose, CA). The vessel areas were calculated as the percentage of pixel numbers representing vessels to the total pixel numbers within the entire field.
Microvascular corrosion casting
Microvascular casting was conducted as previously described.22 Briefly, mice were anesthetized and injected intravenously with 10 000 U/kg heparin via the tail vein following vascular rinsing with lactated Ringer solution plus 1 U/mL heparin until clear of red blood cells. Mice were then perfused with Baston no. 17 casting polymer, a mixture of 6.5 mL monomer base, 1.5 mL catalyst, and 0.2 mL promoter solution (Polysciences, Warrington, PA). After polymerization, the animal was digested with a 30% potassium hydroxide solution. Spleen vessels casts were removed, rinsed in distilled water, and dried. For scanning electron microscopy, samples were mounted on specimen holders and sputter-coated with gold in an argon atmosphere. Casts were examined with an Hitachi S-570 scanning electron microscope (Hitachi Science Systems, Mississauga, Ontario, Canada) at an acceleration voltage of 15 kV and working distance of 15 mm.
Statistical analysis
Comparison of growth kinetics within a given experiment was conducted using repeated Student t tests for 1 and 2 populations with significance values of P < .05. One-way analyses of variance (ANOVAs) were conducted in similar fashion with significance values of P < .05.
Results
Splenectomy extends survival of erythroleukemic mice
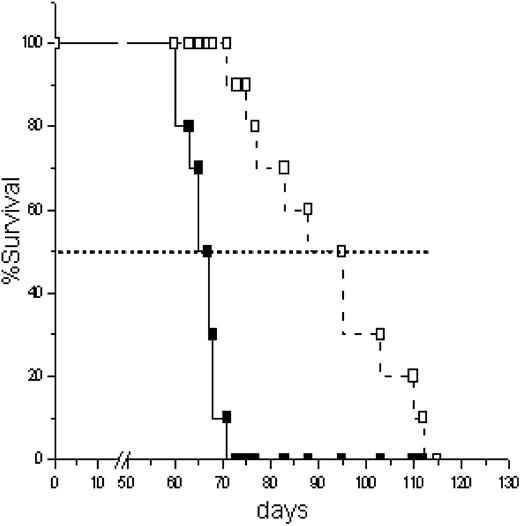
To test whether removal of the spleen during early disease offered mice with Friend disease a survival benefit, 4-week-old erythroleukemic mice were either splenectomized (n = 10) or underwent a sham procedure (n = 10) and monitored weekly. Moribund mice were monitored closely and killed according to institutional guidelines over the following weeks. Mice were killed when either exhibiting severe anemia or considerable abdominal swelling due to severe splenomegaly. As depicted in Figure 1, a significant difference was observed between the survival of splenectomized versus nonsplenectomized erythroleukemic mice, the former experiencing a delay of approximately 30 days in median survival time (P < .05). The overall survival for splenectomized erythroleukemic mice is approximately 95 days whereas that of sham controls is 67 days. Notably, 100% of splenectomized diseased mice eventually died from severe anemia in addition to the development of hepatomegaly. These results may therefore have indicated a potential role of the spleen in the acceleration of Friend disease.
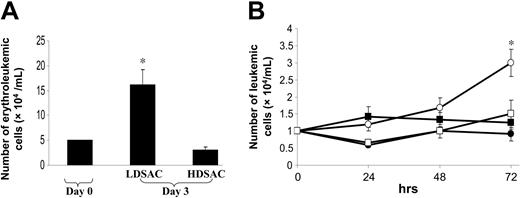
LDSACs, but not HDSACs, drive the expansion of erythroleukemic blasts in vitro
Because stromal cell compartments are known to support and promote the growth of cancers in general, both in solid and liquid tumors,2,4 we asked whether they also contribute, at least in part, to the ability of the spleen to drive the overgrowth of a hematologic neoplasm. To this end, we investigated what attributes of the leukemic spleen could induce a hyperproliferative response of erythroleukemic cells. Thus, primary splenic tissues obtained from healthy and diseased mice were cultured in vitro for 9 days. Suspension cells were then discarded, and the plates were washed with PBS followed by enumeration of adherent cells to equalize for cell number according to “Materials and methods.” Primary erythroleukemic cells were then seeded and cocultured with LDSACs and HDSACs for 4 days. As shown in Figure 2A, only when primary erythroleukemic cells were cocultured with LDSACs was an increase (3-fold) in the number of erythroleukemic cells observed (P < .05). In the presence of HDSACs there actually appears to be a decrease in the number of cells in comparison with their initial seeding density. Whereas viability of erythroleukemic cells was high in LDSAC cocultures, at least 30% of those in HDSAC cocultures were dead as confirmed by positive trypan blue staining. Notably, in all cases, when either LDSACs or HDSACs were cultured in the absence of erythroleukemic cells, they did not survive (data not shown). These results further suggest that the spleen of diseased mice provides a supportive microenvironment.
Survival analysis of splenectomized and sham erythroleukemic mice. Age-matched BALB/c neonates were infected with F-MuLV according to “Materials and methods.” Splenectomy (□) and sham (▪) procedures were performed 4 weeks later followed by daily observations over the duration of the study. All deceased mice and those required to be killed according to institutional guidelines were documented according to date of death and plotted according to the method of Kaplan-Meier. Significance between splenectomy and sham groups was calculated using a Mann-Whitney U test with 2-sided P values and significant differences reflecting P < .05. Dotted horizontal line represents median survival.
Survival analysis of splenectomized and sham erythroleukemic mice. Age-matched BALB/c neonates were infected with F-MuLV according to “Materials and methods.” Splenectomy (□) and sham (▪) procedures were performed 4 weeks later followed by daily observations over the duration of the study. All deceased mice and those required to be killed according to institutional guidelines were documented according to date of death and plotted according to the method of Kaplan-Meier. Significance between splenectomy and sham groups was calculated using a Mann-Whitney U test with 2-sided P values and significant differences reflecting P < .05. Dotted horizontal line represents median survival.
Analysis of primary erythroleukemic cell growth cocultured with LDSACs, HDSACs, or their conditioned media. (A) Primary erythroleukemic (suspension) cells, seeded at a density of 5 × 104/mL, were cocultured with adherent cells derived in vitro either from healthy controls or mice infected with F-MuLV and presenting with Friend disease. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between LDSAC and HDSAC cocultures to reflect P < .05. (B) Primary erythroleukemic cells, seeded at a density of 1 × 104/mL, were cultured in conditioned medium previously used to grow LDSACs (○) versus HDSACs (□), hence LDSAC- and HDSAC-derived media, respectively. Their respective controls (•, ▪) represent similar experiments conducted in control media. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between different growth conditions to reflect P < .05 (*). Error bars indicate ± standard deviation.
Analysis of primary erythroleukemic cell growth cocultured with LDSACs, HDSACs, or their conditioned media. (A) Primary erythroleukemic (suspension) cells, seeded at a density of 5 × 104/mL, were cocultured with adherent cells derived in vitro either from healthy controls or mice infected with F-MuLV and presenting with Friend disease. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between LDSAC and HDSAC cocultures to reflect P < .05. (B) Primary erythroleukemic cells, seeded at a density of 1 × 104/mL, were cultured in conditioned medium previously used to grow LDSACs (○) versus HDSACs (□), hence LDSAC- and HDSAC-derived media, respectively. Their respective controls (•, ▪) represent similar experiments conducted in control media. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between different growth conditions to reflect P < .05 (*). Error bars indicate ± standard deviation.
LDSAC-conditioned medium potentiates expansion of erythroleukemic blasts in vitro
Several studies have shown that malignant hematopoiesis is regulated by both autocrine and paracrine signaling loops.23,24 To delineate the mode by which splenic stroma promotes F-MuLV–induced erythroleukemia, we collected media from cultures equal in number for LDSACs, HDSACs, bone marrow stroma, or NIH-3T3 cells and tested their effects on the growth of primary erythroleukemic cells. The results in Figure 2B indicate that only when primary erythroleukemic cells were grown with LDSAC-conditioned medium did they show an increased proliferation rate in vitro (P < .05). These results suggest that an intricate role of paracrine signaling in erythroleukemic cell expansion is present within the spleen.
F-MuLV–infected mice exhibit integration into the genome of LDSACs
A recent study has reported that in addition to the infection of erythroblasts, B and T cells are also susceptible target cells of Friend virus during late-stage disease. These virus-positive cells are highly populated in the bone marrow and spleen.25 Prior to conducting further experiments, we set out to ascertain whether the stromal compartment of the spleen was genetically altered due to retroviral insertional mutagenesis by F-MuLV, hence conceivably contributing to phenotypic alterations. Similar processes have also been described in systems to obtain immortalized fibroblasts.26 As seen in Figure 3, viral env sequence PCR product was observed in LDSACs but not in HDSACs. Comparisons were made using HB60 erythroleukemic cells27 as a positive control and NIH-3T3 fibroblasts as a negative control. Our results therefore indicate that the nature of Friend virus integration is not only into erythroblasts, although the primary cause of death is consistently erythroleukemia.
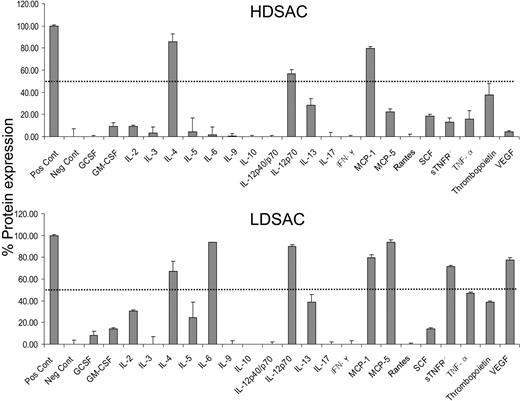
LDSACs produce factors with proangiogenic and inflammatory activities
To ascertain that the composition of the LDSAC-derived medium was indeed responsible for the differences observed in the proliferative capacity of erythroleukemic cells, 22 different cytokines and growth factors were assayed by antibody arrays. HDSACs and LDSACs were cultured in starvation medium for 24 hours. The medium was then collected and screened for the presence of cytokines according to “Materials and methods.” The array signals along with a graphical interpretation of the normalized values are depicted in Figure 4. In the HDSAC-conditioned medium, only IL-4, MCP-1, and IL-12 cytokines were overexpressed (more than 50% normalization) whereas several additional cytokines— namely, IL-6, VEGF-A, MCP-5, and soluble tumor necrosis factor receptor-1 (sTNFR1)—were expressed overabundantly in LDSAC-conditioned medium. In addition, there was a presence of elevated expression of IL-12p70, TNF-α, and IL-2 (P < .05). These observations indicate that the splenic stroma of erythroleukemic mice secretes proangiogenic and inflammatory cytokines, some of which may be essential for the leukomogenic process.
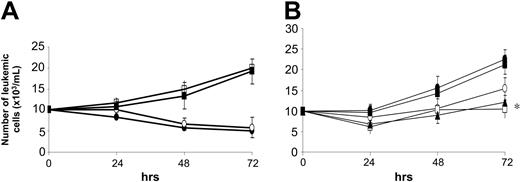
Combination of VEGF-A/MCP-5 induces erythroleukemic expansion in vitro without further potentiation in the presence of IL-6 or TNF-α
Next we sought to determine which of the cytokines that were overexpressed by LDSACs could potentiate erythroleukemic cell proliferation—hence, those factors that could be implicated as mediators of paracrine induction within the spleen. For this approach, primary erythroleukemic cells were seeded in standard medium supplemented with exogenous VEGF-A, MCP-5, IL-6, TNF-α, or all possible combinations thereof. As shown in Figure 5A, combinations of VEGF-A/MCP-5 and VEGF-A/MCP-5/IL-6 significantly increase proliferation rates of erythroleukemic cells. The addition of either IL-6 or TNF-α does not appear to further potentiate this response (data not shown for TNF-α). In all other possible combinations no such proliferative responses were evident (data not shown). These results suggest that VEGF-A and MCP-5 are mandatory for the induction of erythroleukemic cell overgrowth in vitro and that combination of the 2 produced the greatest growth kinetics.
To verify these conclusions, neutralizing antibodies against VEGF-A and MCP-5 were added to primary erythroleukemic cells cultured with LDSAC-conditioned media. Both MCP-5 and VEGF-A neutralizing antibodies alone or in combination inhibit growth of erythroleukemic cells when compared with LDSAC-conditioned medium alone (P < .05). However, the most effective suppression is observed using αVEGF-A as a single agent or in combination with MCP-5, although not reaching significance (Figure 5B). The addition of a neutralizing antibody against TNF-α was also tested to rule out other potential mediators that seemed to be deregulated when comparing LDSAC and HDSAC cultures. However, the growth kinetics of primary cells was not altered in its presence. Thus, our results suggest that both VEGF-A– and MCP-5–mediated paracrine signaling are the most biologically relevant mediators of diseased potentiation within the spleens of erythroleukemic mice.
Analysis of F-MuLV integration within the host genome. Genomic DNA from LDSACs (1), leukemic suspension cells (2), HDSACs (3), normal suspension cells (4), NIH-3T3 cells as negative control (5), HB60 leukemic cells as positive control (6), and 1 kbp ladder (7) was extracted. Friend virus env primers were used to amplify the integration site of the virus's env as described in “Materials and methods.”
Analysis of F-MuLV integration within the host genome. Genomic DNA from LDSACs (1), leukemic suspension cells (2), HDSACs (3), normal suspension cells (4), NIH-3T3 cells as negative control (5), HB60 leukemic cells as positive control (6), and 1 kbp ladder (7) was extracted. Friend virus env primers were used to amplify the integration site of the virus's env as described in “Materials and methods.”
Cytokine profiling of LDSAC- and HDSAC-conditioned growth medium. Mouse cytokine antibody arrays were performed using TransSignal RayBio Mouse Cytokine Antibody Array Kit (MA6050) according to the manufacturer's instructions. Membranes were incubated with LDSAC- or HDSAC-derived medium for 24 hours. Blots were developed and subsequently treated according to “Materials and methods.” Autoradiography was then performed, and intensities were measured by densitometric analysis. Following normalization of the data, with positive controls set at 100% and negative controls at 0, data were plotted and significance considered among the tested cytokines to reflect P < .05. GCSF indicates granulocyte colony stimulating factor; GM-CSF, granulocyte macrophage colony stimulating factor; INF, interferon; and IL, interleukin. Error bars indicate ± standard deviation.
Cytokine profiling of LDSAC- and HDSAC-conditioned growth medium. Mouse cytokine antibody arrays were performed using TransSignal RayBio Mouse Cytokine Antibody Array Kit (MA6050) according to the manufacturer's instructions. Membranes were incubated with LDSAC- or HDSAC-derived medium for 24 hours. Blots were developed and subsequently treated according to “Materials and methods.” Autoradiography was then performed, and intensities were measured by densitometric analysis. Following normalization of the data, with positive controls set at 100% and negative controls at 0, data were plotted and significance considered among the tested cytokines to reflect P < .05. GCSF indicates granulocyte colony stimulating factor; GM-CSF, granulocyte macrophage colony stimulating factor; INF, interferon; and IL, interleukin. Error bars indicate ± standard deviation.
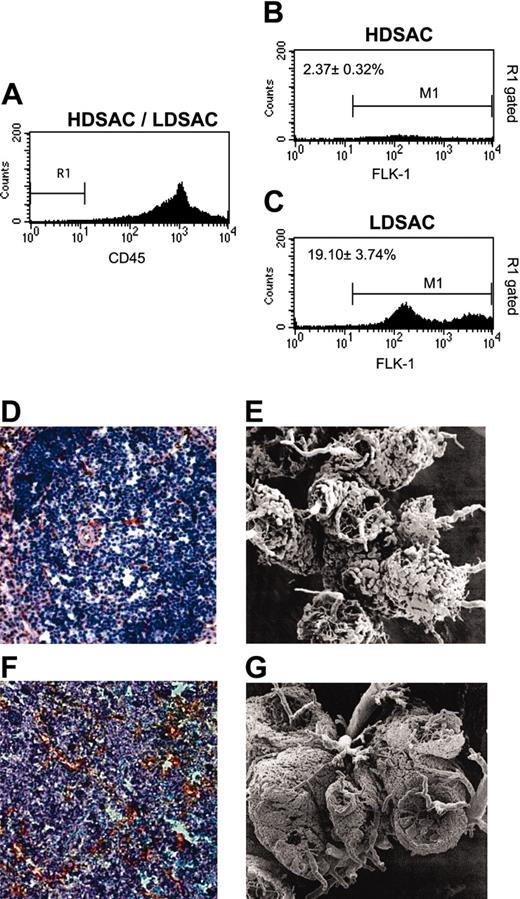
LDSACs have elevated numbers of endothelial cells over HDSACs
Because LDSACs secrete a 15-fold higher concentration of VEGF-A than HDSACs, and given the knowledge of their potent angiogenic properties, we compared the percentage of endothelial cells between HDSACs and LDSACs. For this approach, LDSAC and HDSAC populations from both early and late stages of erythroleukemia were tested for the presence of endothelial markers flk-1 and CD13 and the hematopoietic marker CD45 according to “Materials and methods” and previously described methodologies.20,28 The results in Figure 6 show that in the later stage (9 weeks after tumor induction) the HDSAC population contains approximately 2% of flk-1+/CD45- cells. However, the proportion of such cells in LDSACs is approximately 20% when gating on flk-1+/CD45-. More than 97% of the gated cells, which are not hematopoietic in origin (flk-1+/CD45-), were also found to be CD13+ (data not shown). In contrast, in the early stage of disease (3 weeks after tumor induction), no significant increase in the percentage of endothelial cells in LDSACs was observed when compared with HDSACs (2.75% ± 0.76% and 2.32% ± 0.47%, respectively). In addition, immunohistochemistry of VE-cadherin and intravascular casting were performed on both healthy and erythroleukemic splenic sections to assess for vascular density and patterning. As evidenced in Figure 6D, a central artery is surrounded by conspicuous white pulp and mantle regions, both of which are separated from the marginal sinusoids. This morphology is easily discernable by casting (Figure 6E). The erythroleukemic spleen, however, appears to exhibit vascular patterning in disarray with diffuse positive staining (Figure 6F). As well, an engorgement of erythroleukemic blasts surrounding the central arteriole has apparently replaced the white pulp (Figure 6G). In addition, the vessel areas examined in the immunostained sections revealed increased percentages of positively stained blood vessels (VE-cadherin positive) in leukemic spleens over those of healthy controls (1.8% and 0.3%, respectively). Taken together, an activated endothelium and the overall increase in vessel areas of erythroleukemic mice can be attributed to the convert pathology within the spleen, as represented by the increased endothelial cell population.
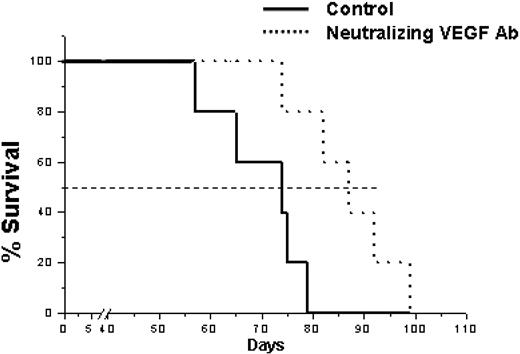
In vivo administration of a neutralizing antibody against VEGF-A extends the survival time of erythroleukemic mice
To test whether our in vitro findings can still be carried out in erythroleukemic mice in vivo, we tested whether treating diseased mice with a neutralizing antibody against VEGF-A can decelerate tumor growth kinetics, hence extending survival. For this approach, 5-week-old erythroleukemic mice were divided into 3 groups: (1) a group treated with 50 μg per mouse of a neutralizing antibody against VEGF-A, twice weekly for 2 weeks according to a previous study18 ; (2) a group treated with goat IgG (control) antibody administered at the same concentration schedule as that of the first group; and (3) a control group similarly administered with PBS (5 per group). The results in Figure 7 show that mice treated with VEGF-A neutralizing antibody exhibit a moderately extended median survival time of 15 days over control mice (88 versus 74 days, respectively). Mice treated with goat IgG exhibit no significant difference from the untreated control group (data not shown). These results suggest that, indeed, erythroleukemic mice treated with a VEGF-A neutralizing antibody exhibit a prolonged survival despite a short-term administration of this antiangiogenic agent.
In vitro analysis of angiogenesis-potentiated overgrowth of primary erythroleukemic cells. (A) Using the cytokine array findings as a reference, primary erythroleukemic cells, seeded at a density of 1 × 104/mL, were cultured in standard medium with the addition of exogenous VEGF-A, MCP-5, IL-6 (□); VEGF-A and MCP-5 (▪); IL-6 and VEGF-A (○); or media alone (•) as per “Materials and methods.” (B) In separate experiments, erythroleukemic cells were cultured in LDSAC-conditioned media (•) with the addition of neutralizing antibodies to VEGF-A (□), MCP-5 (○), and TNF-α (▪), or in various combinations; only combined inhibition of VEGF-A and MCP-5 (▴) is shown for simplicity. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between all tested groups to reflect P < .05 (*). Error bars represent ± standard deviation.
In vitro analysis of angiogenesis-potentiated overgrowth of primary erythroleukemic cells. (A) Using the cytokine array findings as a reference, primary erythroleukemic cells, seeded at a density of 1 × 104/mL, were cultured in standard medium with the addition of exogenous VEGF-A, MCP-5, IL-6 (□); VEGF-A and MCP-5 (▪); IL-6 and VEGF-A (○); or media alone (•) as per “Materials and methods.” (B) In separate experiments, erythroleukemic cells were cultured in LDSAC-conditioned media (•) with the addition of neutralizing antibodies to VEGF-A (□), MCP-5 (○), and TNF-α (▪), or in various combinations; only combined inhibition of VEGF-A and MCP-5 (▴) is shown for simplicity. Scoring of live cells occurred every 24 hours by trypan blue exclusion over a 72-hour time course with significance considered between all tested groups to reflect P < .05 (*). Error bars represent ± standard deviation.
Flow cytometry, immunohistochemistry, and casting analyses of the endothelial cell composition in LDSAC and HDSAC populations. Representative flow cytometry evaluation of endothelial cells either from LDSAC or HDSAC cultures in the late stage of Friend disease. (A) The chosen region (R1) from the total cell population, negative for CD45, either from HDSAC or LDSAC adherent cell populations. (B) The percentage of gated R1 cells that are positive for flk-1 (M1) in the HDSAC population. (C) The percentage of gated R1 cells that are positive for fetal liver kinase-1 (flk-1) (M1) in the LDSAC population. Immunohistochemistry of VE-cadherin stained with 3′3-diaminobenzidine DAB (red) and counterstained with hematoxylin for blood vessel detection was performed on healthy and erythroleukemic spleen sections as described in “Materials and methods” (D,F, respectively). Casting images were performed according to “Materials and methods” on healthy and erythroleukemic spleens in late-stage disease (E,G, respectively).
Flow cytometry, immunohistochemistry, and casting analyses of the endothelial cell composition in LDSAC and HDSAC populations. Representative flow cytometry evaluation of endothelial cells either from LDSAC or HDSAC cultures in the late stage of Friend disease. (A) The chosen region (R1) from the total cell population, negative for CD45, either from HDSAC or LDSAC adherent cell populations. (B) The percentage of gated R1 cells that are positive for flk-1 (M1) in the HDSAC population. (C) The percentage of gated R1 cells that are positive for fetal liver kinase-1 (flk-1) (M1) in the LDSAC population. Immunohistochemistry of VE-cadherin stained with 3′3-diaminobenzidine DAB (red) and counterstained with hematoxylin for blood vessel detection was performed on healthy and erythroleukemic spleen sections as described in “Materials and methods” (D,F, respectively). Casting images were performed according to “Materials and methods” on healthy and erythroleukemic spleens in late-stage disease (E,G, respectively).
Discussion
In the present study we demonstrate a role of the splenic microenvironment in sustaining and promoting a hematologic malignancy, modeled by Friend disease. Adherent cells generated from spleens of diseased, but not healthy, mice were found to sustain the proliferation of erythroleukemic blasts in vitro. This observation indicated that the physiology of splenic cells in erythroleukemic mice was conditioned to provide a supporting microenvironment for the progression of the disease. Indeed, in assessing the profile of cytokines inherent to the pathological spleen, an up-regulation of several cytokines in cultures of erythroleukemic adherent cells was demonstrated. Further analyses revealed that 2 of these cytokines, VEGF-A and MCP-5, were mandatory for the proliferation of erythroleukemic blasts in vitro. This conclusion is based on 2 experimental outcomes. First, medium supplemented with both VEGF-A and MCP-5 was sufficient to provide growth of erythroleukemic blasts, similar to that observed with LDSACs or their conditioned medium. Second, neutralizing antibodies to either VEGF-A or MCP-5 blocked the ability of LDSAC-conditioned media to promote erythroleukemia blast overgrowth. We suggest that during the development of erythroleukemia the spleen becomes a preferential site for propagation of malignant blasts because its stromal compartments provide an essential paracrine-potentiated overgrowth via the secretion of primarily VEGF-A and MCP-5. Indeed, when we administered a neutralizing antibody against VEGF-A to erythroleukemic mice, we found that they exhibited prolonged survival.
In retrospect, it is not surprising that VEGF-A constitutes a major microenvironmental factor promoting leukemogenesis. The role of proangiogenesis-related factors in the progression of several solid tumors is well established. Only recently, however, has the angiogenic response in leukemia been uncovered. Following the discovery of increased microvessel density within the bone marrow of pediatric and adult cancer patients with distinct types of leukemia,29,30 there has been increasing evidence to suggest that angiogenesis and leukemia progress in a synchronized manner, primarily by the production of several key angiogenic mediators (reviewed by Moehler et al31 ). Indeed, of these several proangiogenic mediators currently known, VEGF-A continues to be extensively investigated because it has been associated with several hematologic malignancies.31 Recent evidence suggests that both autocrine and paracrine signaling loops exist among malignant blasts and endothelial cells (both cell autonomous and nonautonomous); these involve primarily VEGF signaling following the binding of its receptor, flk-1, to facilitate aggressive expansion of the disease.24,32 As such, this information suggests that a conducive organ microenvironment is an essential component for the survival and expansion of the tumors (leukemia), albeit in a stage- and subtype-dependent manner. Our work reinforces recent findings by showing that VEGF-A is a mediator of leukemic cell expansion, at least in a paracrine manner.24 However, in addition to this we have observed that the expansion of erythroleukemic cells is also dependant on the presence of the inflammatory mediator, MCP-5.
We have observed that MCP-5 is one of the primary contributors to the proliferation of erythroleukemic blasts and is highly overexpressed in LDSAC culture. In this work, we demonstrated that anti–MCP-5 and anti–VEGF-A neutralizing antibodies as single agents or in combination suppressed the proliferation of erythroleukemic cells. However, the VEGF-A neutralizing antibody exhibited the greatest impact overall. Intriguingly, a study by Ueno et al33 has shown the partial requirement of MCP-5 for tumor growth. In their study, MCP-1, which is a human homolog of the mouse MCP-5,34 was up-regulated in the microenvironment of a human breast cancer. The authors showed that MCP-1 and VEGF were significant indicators for early relapse. They concluded that these factors could play an important role in the regulation of angiogenesis and the immune system. Our findings are not only in accordance with theirs, but they provide evidence of a ubiquitous angiogenic/inflammatory response element in solid and liquid tumors alike. Thus, erythroleukemic cells homing and expanding within the spleens of mice with Friend disease may occur, at least in part, due to the presence of an enriched microenvironment. This would therefore be suggestive of a potential benefit for employing an antiangiogenic treatment strategy to drive down the production of key angiogenic/inflammatory mediators.
Survival analysis of erythroleukemic mice treated with neutralizing antibody against VEGF-A. Erythroleukemic mice were randomized and divided into 3 groups: (1) control untreated group (solid line); (2) group treated with goat IgG as a control (data not shown); or (3) a group treated with a neutralizing antibody against VEGF-A (dotted line) for 2 weeks. Mice were monitored on a daily basis and killed according to institutional guidelines, and survival was assessed by the method of Kaplan-Meier. Dotted horizontal lines represent median survival.
Survival analysis of erythroleukemic mice treated with neutralizing antibody against VEGF-A. Erythroleukemic mice were randomized and divided into 3 groups: (1) control untreated group (solid line); (2) group treated with goat IgG as a control (data not shown); or (3) a group treated with a neutralizing antibody against VEGF-A (dotted line) for 2 weeks. Mice were monitored on a daily basis and killed according to institutional guidelines, and survival was assessed by the method of Kaplan-Meier. Dotted horizontal lines represent median survival.
Moreover, the histologic evidence of loss of splenic architecture caused by infiltrating blasts is further supported by the patterns observed with vascular casting. In particular, the pathological angiogenesis induced by the leukemic spleen can be appreciated in the inner aspect of the germinal center, normally filled with organized centripetal sinusoids in the healthy organ. It is disordered in the pathological specimen, suggesting tumor-induced changes in the vasculature. Taken together with the increased number of endothelial cells in erythroleukemic spleen, these results suggest a proangiogenic response mechanism within the spleen that not only leads to the up-regulation of pivotal angiogenic factors such as VEGF-A but also the activation and proliferation of endothelial cells, which leads to disorganized vessel structure of leukemic spleen. Conceivably, both may facilitate the rapid expansion of malignant blasts within the spleen.
Although we do not provide a complete analysis of the cellular composition of the LDSAC and HDSAC cultures, we have observed a 10-fold increase in the percentage of endothelial cells in the LDSACs over HDSACs in vitro as well as an increase in blood vessels and loss of spleen architecture in diseased spleens in vivo. These results suggest that in this erythroleukemia model it is reasonable to expect similar angiogenesis-dependent responses by the leukemic erythroblasts as have been demonstrated in xenograft models of common human hematologic malignancies.4,35,36 Furthermore, the spleen as a favorable microenvironment for expanding cells was found to contribute to the tumor progression via paracrine loops, although autocrine loops cannot be ruled out during this process. Indeed, we observed flk-1 RNA expression (VEGF receptor-2 [VEGFR-2]) in some in-house–derived erythroleukemic cell lines (Y.S. and D.C., unpublished observations August, 2003), which supports the possibility of an autocrine loop mediated by VEGF as previously reported.24 This brings into question the effect(s) of VEGF-A neutralizing antibody in vivo because it may suggest that overexpression of other VEGF types (eg, VEGF-C and VEGF-D) may still activate VEGFR-2 (reviewed by Carmeliet37 ), which can induce proliferation of such cells. However, we are aware only of the up-regulation of the flk-1 receptor on the erythroleukemic blasts in our model system, which is supported by previous studies,24,36 but not of IL-6 or MCP receptors. Yet, our findings suggest that these receptors play a pivotal role in altering growth-signaling pathways of these blasts.
Overall, our findings of prolonged survival with the administration of a VEGF-A neutralizing antibody in vivo and the contribution of both MCP-5 and VEGF-A to leukemogenesis in vitro not only provide a contributory mechanistic role for the spleen in the development and progression of murine erythroleukemia but also suggest that early surgical intervention (ie, splenectomy) might be considered as an adjunct to targeted antiangiogenic treatment modalities for human hematologic neoplasms that are similarly aggressive.
Prepublished online as Blood First Edition Paper, February 8, 2005; DOI 10.1182/blood-2004-08-3210.
Supported by grants from the Canadian Institutes of Health Research (CIHR) (Y.B.D., R.S.K.), the Ontario Cancer Research Network (OCRN) (Y.B.D.), the National Institutes of Health (NIH; CA-41233) (R.S.K.), and National Cancer Institute of Canada (NCIC) (R.S.K). Y.S. is a recipient of a postdoctoral fellowship award from the CIHR. D.C. is supported by a studentship award from the CIHR.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr Eitan Yefenof, Dr David Spaner, and Dr Urban Emmenegger for their input and the critical assessment of this manuscript.