Abstract
Angiogenesis and inflammation are closely related biologic processes in wound healing and the responses to vascular injury as well as in cardiovascular diseases; however, the molecular connections are poorly defined. In particular, it is yet unclear whether endogenous factors can regulate both angiogenesis and inflammation. Here, we show that the endogenous angiogenesis inhibitor, angiostatin (containing kringle domains 1-4 of plasminogen), serves an anti-inflammatory role, since the kringles 1-3 and its kringle 4 directly interact with leukocyte β1- and β2-integrins, respectively. In particular, a specific interaction between kringle 4 and αMβ2-integrin (Mac-1) but not leukocyte function antigen 1 (LFA-1) was identified. Angiostatin thereby inhibited β1- and β2-integrin–mediated adhesion of leukocytes to extracellular matrix proteins and the endothelium as well as their transmigration through the endothelium in vitro. Moreover, angiostatin blocked the peritonitis-induced neutrophil emigration in vivo. In addition, through its interaction with Mac-1, angiostatin reduced activation of the proinflammatory transcription factor nuclear factor κB (NFκB), as well as the NFκB-related expression of tissue factor, a potent initiator of hemostasis following vascular injury. Finally, angiostatin forms were generated in vivo following skin injury/inflammation and were detectable during the following entire period of wound healing peaking at the terminal phase of the healing process. Taken together, over and above inhibition of neovascularization, angiostatin was identified as an antiadhesive/anti-inflammatory substance. These observations could provide the basis for new therapeutic applications of angiostatin to target chronic inflammatory processes in different pathologic situations.
Introduction
The recruitment of leukocytes is an integral part of both chronic inflammatory processes or vascular remodeling and of the immediate response toward bacterial infection or tissue injury. Leukocyte recruitment requires a coordinated sequence of multistep adhesive and signaling events including selectin-mediated rolling, leukocyte activation, and integrin-mediated firm adhesion and diapedesis.1 During firm adhesion of leukocytes to the endothelium, members of the β2-integrin family, leukocyte function antigen 1 (LFA-1; αLβ2, CD11a/CD18), Mac-1 (αMβ2, CD11b/CD18), and p150,95 (αXβ2, CD11c/CD18), as well as β1-integrins on the leukocyte surface interact with endothelial counterligands such as intercellular adhesion molecule-1 (ICAM-1), surface-associated fibrinogen, or vascular cell adhesion molecule-1 (VCAM-1). Whereas very late antigen-4 (VLA-4; α4β1-integrin) mediates leukocyte adhesion to fibronectin in the extracellular matrix, Mac-1 regulates leukocyte adhesion to provisional matrix substrates including fibrinogen (FBG), which becomes deposited at sites of inflammation and injury during the phase of increased vascular permeability or damage.2-4 Ligation and activation of Mac-1 results in modulation of gene expression mediated at least in part by the activation of the transcription factor nuclear factor κB (NF-κB),5-7 which has been proposed as a critical molecular bridge between oxidant stress and gene expression as a result of cell exposure to inflammatory, infectious, or other stressful stimuli.8-10
Angiogenesis and inflammation are closely related in biologic processes such as wound healing and response to vascular injury. Moreover, neovascularization accompanies chronic inflammatory conditions including psoriasis, rheumatoid arthritis, and granulomatous diseases; in such cases, neovascularization may function to sustain inflammation, since new capillaries facilitate leukocyte entry into inflammatory lesions.11 The crosstalk between integrins and proteolytic systems, such as matrix metalloproteinases and the fibrinolytic system, plays a central role during vascular remodelling.12 We and others have recently demonstrated the molecular convergence of adhesive forces/contacts and the plasminogen system on the surface of leukocytes, necessary for their recruitment. Both urokinase plasminogen activator and its receptor were shown to interact with β2-integrins, in particular Mac-1, to engage this multifunctional integrin for adhesion and migration.13-15
Angiostatin, a proteolytic fragment of plasminogen, entailing either the first 3 or first 4 kringle domains (K1-3, K1-4) of plasminogen is a potent inhibitor of angiogenesis in vivo.16-18 After urokinase-dependent conversion of plasminogen into the 2-chain serine protease, plasmin serves as both the substrate and enzyme for the generation of angiostatin,19 however several other mechanisms have been proposed for the generation of angiostatin from plasminogen.20 Inhibition of endothelial cell proliferation and migration by angiostatin is mediated by different kringles of the molecule.21-23 Furthermore, angiostatin interacts with the integrins α4β1 and α9β1, as well as with αvβ3,24 which has an important function during pathologic angiogenesis due to its expression on angiogenic endothelium and its function in a spatio-temporal manner.25 Moreover, biologically active angiostatin (K1-3) can be generated by neutrophil-derived elastase,26 and a recent report demonstrated that angiostatin interferes with neutrophil migration and thereby chemokine-induced angiogenesis,27 whereby the underlying mechanisms remained undefined.
These diverse observations prompted us to investigate the exact role of angiostatin in leukocyte recruitment. We demonstrate here the existence of a direct interaction between angiostatin and the β2-integrin Mac-1 and have confirmed the interaction between angiostatin and β1-integrins. These interactions define the anti-inflammatory role of angiostatin, thereby introducing possible novel therapeutic applications for angiostatin in chronic inflammatory disorders.
Materials and methods
Materials
The following reagents were provided from these sources: isolated Mac-1, LFA-1, and ICAM-1 (Dr S. Bodary, Genentech, San Francisco, CA); purified I-domain of Mac-1 (Dr D. Tuckwell, Manchester, United Kingdom); blocking monoclonal antibody (mAb) 60.3 against human CD18 (Dr J. Harlan, Seattle, WA); mAb against tissue factor (Dr W. Ruf, Scripps, La Jolla, CA); β2-integrin activating mAb Kim185 (Dr. M. Robinson, Slough Berkshire, United Kingdom); mAb L15 against LFA-1 (Dr Y. van Kooyk, Amsterdam, the Netherlands); mAb LPM19c against Mac-1 (Acris, Hiddenhausen, Germany); mAb 3.9 against p150,95 (Ancell, Bayport, MN); mAb TDM29 and 6S6 against β1-chain (CD29; Chemicon, Hofheim, Germany); mAb HP2.1 against integrin α4-chain (Immunotech, Hamburg, Germany); mAb against ICAM-1 (DAKO, Hamburg, Germany); and respective isotype-matched control antibodies (DAKO). The blocking mAb against mouse Mac-1 (M1/70), mouse LFA-1 (M17/4), and mouse ICAM-1 (3E2), as well as respective isotype-matched control antibodies, which were used for in vivo inhibition studies, were from Pharmingen (Hamburg, Germany). MnCl2, fibrinogen (FBG), fibronectin (FN), ϵ-aminocaproic acid (EACA), and monocyte chemoattractant protein-1 (MCP-1) were from Sigma (Munich, Germany). Vitronectin (VN) was purified from human plasma and converted into the multimeric form as previously described.28 Vitamin D3 was from Biomol (Hamburg, Germany), transforming growth factor-β was from R&D Systems (Boston, MA), and recombinant soluble VCAM-1 was purchased from Chemicon. Recombinant human angiostatin entailing kringles 1-3 of plasminogen (amino acids 97-357), with a single amino acid mutation (N308 to E308) preventing N-glycolysation, was expressed and purified from Pischia pastoris (methylatropic yeast).29,30 Angiostatin forms (K1-4, K1-3, and K4) were generated and purified as previously described.18,31 Briefly, plasminogen was purified from human plasma and proteolysed with 0.75 μg elastase/100 mg plasminogen for 5 hours at 37°C. Cleavage products were then isolated by affinity chromatography using lysine-sepharose and subsequently separated dependent on their molecular weight using a S300-gel filtration column. In sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) at reducing conditions, K1-4, K1-3, and K4 each appeared at 42, 38, and 14 kDa, respectively. The identity of the different angiostatin forms was also verified by aminoterminal protein sequencing.
Cell culture
Myelomonocytic THP-1 cells, K562 cells, and K562 cells transfected with different β2-integrin forms, as well as human umbilical vein endothelial cells (HUVECs), were cultivated as previously described.32-35 K562 cells (nontransfected, stable LFA-1, or p150.95 transfectants) were kindly provided by Dr Y. van Kooyk (Amsterdam, the Netherlands). K562 cells transfected with Mac-1 were kindly provided by Dr M. Smith (Celltech, Slough, United Kingdom). Human neutrophils were isolated from peripheral blood as previously described.33
Cell adhesion assay
Adhesion assays were performed as previously described.33-35 As shown in Figure 1, adhesion assays of THP-1 cells or neutrophils to immobilized FBG, FN, VN, ICAM-1, or VCAM-1 (each 10 μg/mL), or to bovine serum albumin (BSA) as control, were performed, both in the absence or presence of inhibitory antibodies or angiostatin forms in the soluble phase. Moreover, adhesion of THP-1 cells or neutrophils to immobilized angiostatin forms (K1-4, K1-3, and K4; 400 nM) was carried out as shown in Figure 2. Briefly, microtiter plates were coated with the respective substrates in bicarbonate buffer, pH 9.6, and blocked with 3% BSA-solution. Isolated human neutrophils, or THP-1 cells, which had been differentiated for 24 hours in the presence of vitamin D3 (100 nM) and transforming growth factor-β (2 ng/mL), were washed in serum-free RPMI medium and plated onto the precoated wells (105/well) at 37°C for 60 minutes in the absence or presence of inhibitors. Following the incubation period, the wells were washed and adherent cells were fixed with methanol-acetone (1:1) at 4°C for 30 minutes. Adherent cells were then stained with crystal violet and quantified by measuring absorbance at 590 nm.
Angiostatin interferes with leukocyte adhesion. The adhesion of PMA-stimulated THP-1 cells to immobilized vitronectin (A), fibrinogen (B), ICAM-1 (C), fibronectin (D), or VCAM-1 (E) in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○) in the soluble phase is shown. (F) The adhesion of PMA-stimulated human neutrophils to immobilized fibrinogen (▪) or immobilized fibronectin (▦]) is shown in the absence (–) or presence of inhibitory mAb (anti-Mac-1 or anti-β1, respectively, each 20 μg/mL), K1-4, K1-3, K4 (each 1000 nM), or a combination of K1-3 and K4, as indicated. Cell adhesion is represented as absorbance at 590 nm. All data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.
Angiostatin interferes with leukocyte adhesion. The adhesion of PMA-stimulated THP-1 cells to immobilized vitronectin (A), fibrinogen (B), ICAM-1 (C), fibronectin (D), or VCAM-1 (E) in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○) in the soluble phase is shown. (F) The adhesion of PMA-stimulated human neutrophils to immobilized fibrinogen (▪) or immobilized fibronectin (▦]) is shown in the absence (–) or presence of inhibitory mAb (anti-Mac-1 or anti-β1, respectively, each 20 μg/mL), K1-4, K1-3, K4 (each 1000 nM), or a combination of K1-3 and K4, as indicated. Cell adhesion is represented as absorbance at 590 nm. All data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.
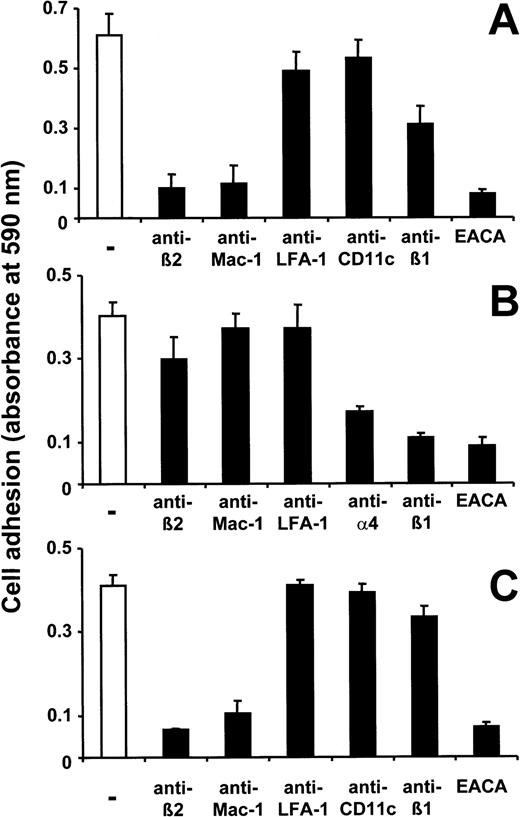
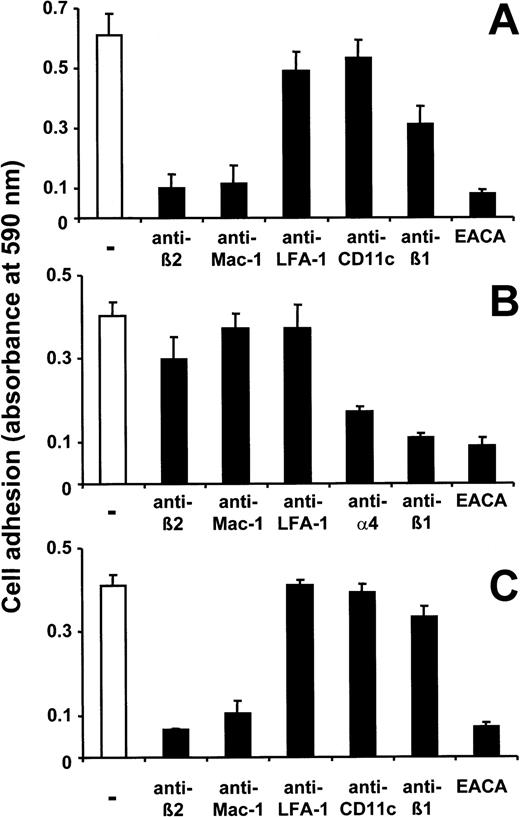
Interaction of angiostatin with leukocyte integrins. Adhesion of PMA-stimulated THP-1 cells to immobilized K1-4 (A), K1-3 (B), or K4 (C) is shown in the absence (–) or presence of inhibitory mAb (each 20 μg/mL) as well as EACA (10 mM) as indicated. Cell adhesion is represented as absorbance at 590 nm. Data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.
Interaction of angiostatin with leukocyte integrins. Adhesion of PMA-stimulated THP-1 cells to immobilized K1-4 (A), K1-3 (B), or K4 (C) is shown in the absence (–) or presence of inhibitory mAb (each 20 μg/mL) as well as EACA (10 mM) as indicated. Cell adhesion is represented as absorbance at 590 nm. Data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.
Adhesion of THP-1 cells or neutrophils to cultured monolayers of HUVECs was tested as previously described.34,35 Briefly, HUVECs were grown to confluency onto 96-well plates. Fluorescence-labeled neutrophils (105/well), or differentiated THP-1 cells, were washed twice followed by no pretreatment or by stimulation with phorbol myristate acetate (PMA; 50 ng/mL). Cells were washed and added to HUVECs at 37°C for 60 minutes in the absence or presence of inhibitors. After washing, adhesion of neutrophils, or THP-1 cells, was quantified as the percentage of total cells added using a fluorescence microplate reader (Bio-Tek, Neufahrn, Germany).34,35
Transendothelial migration
Transendothelial migration was performed as previously described.36 Briefly, transmigration assays were performed using 6.5-mm transwell filters with a 5-μm pore size (Costar, Bodenheim, Germany). After inserts were coated with gelatin (Sigma), HUVECs were seeded on transwell filters 2 days prior to the assay and grown without medium in the lower compartment for 48 hours in a humidified atmosphere (37°C, 5% CO2). At the beginning of the transmigration assay, 600 μL migration assay medium (serum-free RPMI in the absence or presence of 50 ng/mL MCP-1) was added to the lower compartment of the Transwell system. Neutrophils (3 × 105 in 100 μL) were added to the upper compartment on top of the endothelial monolayer. After incubation for 4 hours at 37°C, the number of transmigrated cells in the lower compartment was estimated with a cell counter (CASY-Counter; Schärfe-System, Reutlingen, Germany). The inserts were washed twice in phosphate-buffered saline (PBS) and fixed with methanol-acetone (1:1), stained with crystal violet, and mounted on glass slides in order to confirm the confluency of the endothelial monolayer of the filters after the assay.
In vitro ligand-receptor interactions
Binding of biotinylated FBG or ICAM-1 to immobilized Mac-1 or LFA-1 was performed as previously described.33-35,37 Alternatively, binding of biotinylated I-domain (1 μg/mL) to immobilized K1-4, K1-3, or K4 (each 400 nM) was performed in tris(hydroxymethyl)aminomethane (Tris)–buffered saline (TBS) containing 0.3% BSA, 0.05% Tween-20, 1 mM Mn2+. Following incubation for 2 hours at 22°C in each case, peroxidasecoupled streptavidin was added, followed by addition of the substrate ABTS (2,2′-azino-bis[3-ethylbenzthiazoline-6-sulfonic acid]), and binding was quantitated at 405 nm. Nonspecific binding to BSA-coated wells was used as blank and was subtracted to calculate specific binding.
Generation of cutaneous wounds and detection of angiostatin
Mice were anesthetized using 13 μL of 2.5% avertin per gram body weight. There were 2 round cutaneous wounds generated at both sides of the lower dorsal trunk after shaving the hair and disinfecting the skin with Softasept N (Braun Melsungen AG, Melsungen, Germany). The area of circular skin removed was 8 mm in diameter. Curved scissors and surgical techniques were used. The wounds were well separated by more than 1 cm skin. This protocol was approved by the veterinarians of the animal facilities of the University of Heidelberg and the Governmental Office Karlsruhe (experimental protocols 35-9185.81-2 and 35-9185.81/G-37/03).
At days 0, 1, 3, 7, and 11 after generation, wounds were extracted. For the preparation of total wound extract, wounds were homogenized using a pestle and liquid nitrogen and were then lysed in a buffer containing 50 mM Tris-HCl [pH 8.0], 150 mM NaCl, 0.02% sodium azide, 1% Triton X-100, 2 mM benzamidin, 20 μg/mL soybean inhibitor, 1 mM leupeptin, 1 μg/mL aprotinin, 0.5 mM phenylmethylsulfonyl fluoride (PMSF). After centrifugation (1500 g, 2 minutes, 4°C), lysates were cleared from insoluble material, followed by 4 freeze (–80°C)/thaw (37°C) cycles. Lysates were then centrifuged (15 000 rpm, 5 minutes, 4°C), and the supernatant was collected and centrifuged again (20 000 g, 1 minute, 4°C). The supernatant was then used for Western blot analysis after determining and adjusting protein concentration.
Western blot analysis
Western blot analysis for the detection of tissue factor on THP-1 cells or angiostatin forms in wound lysates was performed as previously described.38 Following overnight preincubation with tumor necrosis factor-α (5 nM) in the absence or presence of competitors, THP-1 cells were centrifuged and the pellet was lysed by adding sample buffer (125 mM Tris-HCl, pH 6.8; 4% SDS; 2% mercaptoethanol; 20% glycerol; 1 mg bromphenol blue). After a 5-minute incubation at 95 °C, 30 μL of the THP-1 lysates or 20 μL of the wound extracts was analyzed by SDS-PAGE and subsequently transferred to a polyvinylidene difluoride membrane. The membranes were blocked with Tris-buffered saline supplemented with 0.1% Tween-20 (wash buffer) and 2% low-fat milk powder and incubated with mAb TF9-6B4 against tissue factor or rabbit antiangiostatin (Acris) overnight at 4°C, diluted 1:500 in wash buffer containing 2.5% BSA. Following incubation with the appropriate peroxidase-conjugated secondary antibody (DAKO), blots were developed using an enhanced chemiluminescence (ECL)–based system (Amersham, Freiburg, Germany).
Electrophoretic mobility shift assay (EMSA)
Nuclear proteins were harvested as described elsewhere39,40 and assayed for transcription factor binding activity using the NFκB consensus sequence 5-GTTGAGGGGACTTTCCCAGGC-3. Specificity of binding was ascertained by competition with a 160-fold molar excess of unlabeled consensus oligonucleotides and by supershift experiments.39,40
In vivo peritonitis model
Thioglycollate-induced peritonitis in mice was performed as previously described.34,35,37 For inhibition studies, 30 minutes prior to the injection of thioglycollate, the following compounds were administered intraperitoneally: various concentrations of K1-4, K1-3, and K4; and mAbs against mouse Mac-1, against mouse LFA-1, or against mouse ICAM-1 in PBS (each mAb 100 μg). Control mice were treated with the same volume of PBS or the respective isotype-matched control antibody (100 μg). Each compound was administered in a total volume of 0.4 mL. In order to evaluate neutrophil recruitment, mice were killed at 4 hours following injection of thioglycollate. Thereafter, the peritoneal lavage was collected and the number of emigrated neutrophils was quantitated as previously described.34,35,37
Statistical analysis
Data were compared using the Student t test and analysis of variance (ANOVA) as appropriate; P values of less than .05 were regarded as significant.
Results
Angiostatin interferes with integrin-mediated leukocyte adhesion
As previously established, adhesion of leukocytic cells such as myelomonocytic THP-1 or neutrophils to immobilized FBG is predominantly mediated by the β2-integrin Mac-1, while Mac-1 and LFA-1 control cell adhesion to ICAM-1. In contrast, adhesion to FN and VCAM-1 is mediated by the β1-integrin VLA-4 (α4β1), and to immobilized VN by the urokinase-receptor (uPAR).14,34,37 In order to characterize the role of angiostatin in these adhesion processes, we tested adhesion of THP-1 and human peripheral blood neutrophils to different immobilized substrates (VN, FBG, ICAM-1, FN, VCAM-1) in the absence or presence of 3 angiostatin forms, consisting either of the first 4 kringles (K1-4), the first 3 kringles (K1-3), or the isolated kringle 4 (K4) of plasminogen in the soluble phase. Whereas uPAR-dependent adhesion to VN was not affected by any form of angiostatin, Mac-1–dependent adhesion to FBG and ICAM-1 was inhibited by K1-4 in a dose-dependent manner (Figure 1). Strikingly, isolated K4 inhibited Mac-1–dependent adhesion comparable with K1-4, whereas K1-3 exhibited no significant inhibitory function (Figure 1B-C). In addition, VLA-4–dependent THP-1 cell adhesion to FN and VCAM-1 was also blocked by K1-4, somehow to a lesser extent. However, in this case the isolated K4 was not inhibitory, whereas K1-3 and K1-4 blocked adhesion to a similar degree (Figure 1D-E). Coincubation of K1-3 with K4 did not enhance the inhibitory function of K1-3 and of K4 on VLA-4–dependent and Mac-1–dependent adhesion, respectively (Figure 1F). Together, K1-4 prevents both VLA-4– and Mac-1–dependent neutrophil and THP-1 adhesion, whereby K1-3 primarily interfered with VLA-4–dependent and K4 with Mac-1–dependent adhesive events.
These observations indicated a direct interaction of different kringles in the angiostatin molecule with leukocyte integrins. Therefore, we studied whether leukocytes could directly bind to immobilized angiostatin forms. THP-1 cells not only adhered to K1-4, but adhesion to K1-4 was inhibited by a blocking monoclonal antibody (mAb) against β2-integrins and to a lesser extent by a blocking mAb against β1-integrin (Figure 2A). Moreover, myelomonocytic cell adhesion to immobilized K1-4 was inhibited by a blocking mAb against Mac-1, whereas a blocking mAb against LFA-1 or p150,95 did not significantly affect cell adhesion (Figure 2A). To further investigate the participation of K1-3 and K4 in these interactions, we studied adhesion of THP-1 cells to immobilized fragments of angiostatin. Adhesion to immobilized K1-3 was abolished by a blocking mAb against β1- and α4-integrin, whereas anti–β2-integrin antibodies were ineffective. In contrast, adhesion to immobilized K4 was reduced by a blocking mAb against β2-integrin and mAb against Mac-1, whereas blocking mAb against β1-integrins was ineffective (Figure 2B-C). Furthermore, adhesion of THP-1 cells to immobilized K1-4, K1-3, and K4 was totally abolished by ϵ-aminocaproic acid (EACA), indicating that lysine-binding sites in angiostatin are required for interaction with integrins (Figure 2A-C). Similar results were also observed when adhesion of peripheral blood neutrophils was tested (not shown). Moreover, these data were corroborated by testing the adhesion of nontransfected K562 cells or K562 cells that were transfected with Mac-1, LFA-1, or p150,95 to the 3 immobilized forms of angiostatin (data not shown). Taken together, these data indicate that angiostatin interacts with leukocyte integrins, in particular, K1-3 and K4 interact with α4β1-integrin and Mac-1, respectively, thereby blocking the function of the integrins.
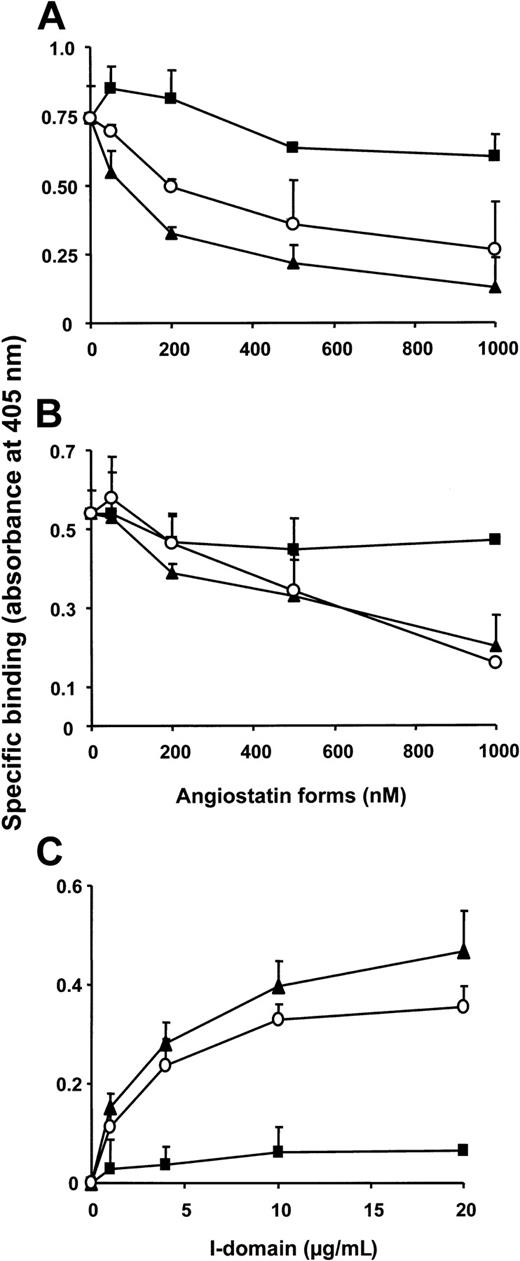
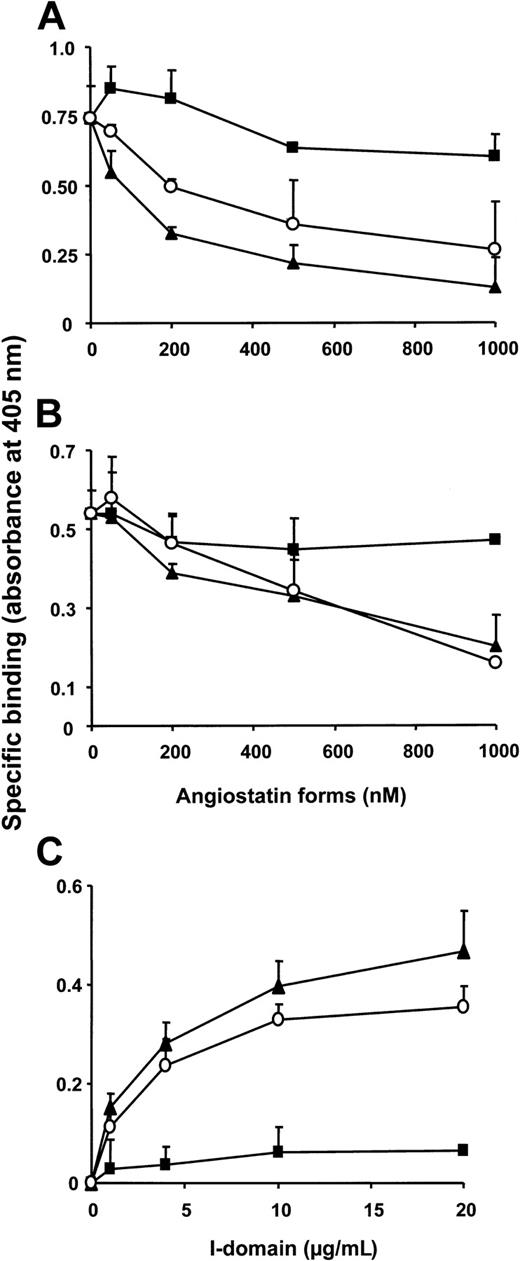
Direct interaction between K1-4, K4, and Mac-1
The previous observations implicated that K1-4 and the portion of K4 could directly bind to the β2-integrin Mac-1. Therefore, these angiostatin forms were tested for their interference with the interaction of other Mac-1 ligands. In a purified system, K1-4 and K4 but not K1-3 inhibited the binding of FBG and ICAM-1 to immobilized Mac-1 (Figure 3A-B), whereas binding of ICAM-1 to LFA-1 was not affected (data not shown). A specific and saturable binding of K1-4 (but not K1-3) to immobilized Mac-1 (but not LFA-1) was also observed (data not shown). We then tested whether angiostatin binds to the major ligand-binding I domain of Mac-1, and a direct saturable binding of biotinylated I-domain to immobilized K1-4 or K4 (but not to K1-3) was observed (Figure 3C). These data indicate that K1-4 and particularly K4 directly interact with Mac-1, and this binding may be attributed at least in part to the ligand binding I-domain of the integrin α-chain.
Direct interaction of angiostatin with Mac-1. The binding of fibrinogen (A) or ICAM-1 (B) to immobilized Mac-1 is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). (C) Dose-dependent specific binding of the isolated I-domain of Mac-1 to immobilized K1-4 (▴), K1-3 (▪), or K4 (○). Specific binding is expressed as absorbance at 405 nm. Data are mean ± SD (n = 3) of a typical experiment; similar results were observed in 3 separate experiments.
Direct interaction of angiostatin with Mac-1. The binding of fibrinogen (A) or ICAM-1 (B) to immobilized Mac-1 is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). (C) Dose-dependent specific binding of the isolated I-domain of Mac-1 to immobilized K1-4 (▴), K1-3 (▪), or K4 (○). Specific binding is expressed as absorbance at 405 nm. Data are mean ± SD (n = 3) of a typical experiment; similar results were observed in 3 separate experiments.
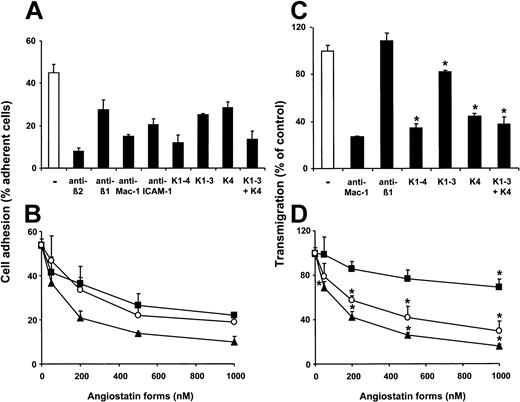
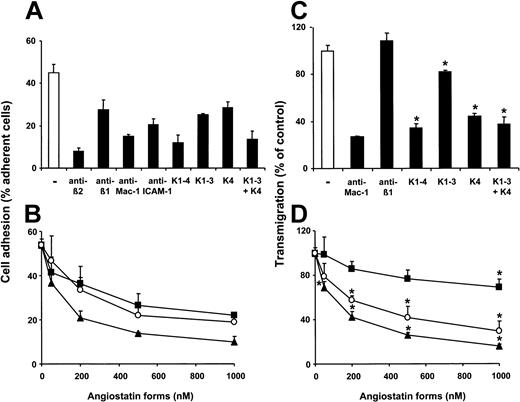
Inhibition of leukocyte adhesion to endothelial cells and transendothelial migration by angiostatin
The binding between Mac-1 and ICAM-1 as well as the binding between α4β1 and VCAM-1 participate in leukocyte-endothelial interactions. We therefore investigated whether angiostatin interferes with the adhesion of peripheral blood neutrophils to endothelial cells. Neutrophil adhesion to endothelial cells was mediated by β2-integrins and to a lesser extent by β1-integrins, as it was inhibited by blocking mAb against β2 and especially blocking mAb against Mac-1 as well as by blocking mAb against β1. The presence of K1-4 significantly reduced adhesion of neutrophils to endothelial cells to the level of inhibition obtained with blocking mAb against Mac-1. Both K1-3 and K4 significantly blocked neutrophil adhesion to the endothelium, and upon coincubation their inhibitory effect was comparable with the antiadhesive function of K1-4 (Figure 4A). The effect of K1-4, K1-3, and K4 on neutrophil adhesion to HUVECs was also dose dependent (Figure 4B). The median inhibitory concentrations (IC50) of K1-4, K1-3, and K4 were 150 nM, 500 nM, and 400 nM, respectively.
Influence of angiostatin on neutrophil–endothelial cell interactions. (A) PMA-stimulated adhesion of human neutrophils to endothelial cells is shown in the absence (–) or presence of blocking mAb to β2-integrin, β1-integrin, Mac-1, ICAM-1 (each antibody at 20 μg/mL), K1-4, K1-3, K4, or a combination of K4 with K1-3 (each angiostatin form at 1000 nM). (B) PMA-stimulated adhesion of human neutrophils to endothelial cells is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). Cell adhesion is represented as percentage of adherent cell to total added cells. (C) The trans-endothelial migration of human neutrophils in response to 50 ng/mL MCP-1 is shown in the absence (–) or presence of mAb to Mac-1, mAb to β1-integrin (each antibody at 20 μg/mL), K1-4, K1-3, K4, or a combination of K4 with K1-3 (each angiostatin form at 1000 nM). (D) The trans-endothelial migration of human neutrophils in response to 50 ng/mL MCP-1 is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). Transmigration is presented as percent of control (only MCP-1, in the absence of competitor). Data are mean ± SD (n = 3) of a typical experiment, similar results were obtained in 3 separate experiments. *P < .001, compared with control.
Influence of angiostatin on neutrophil–endothelial cell interactions. (A) PMA-stimulated adhesion of human neutrophils to endothelial cells is shown in the absence (–) or presence of blocking mAb to β2-integrin, β1-integrin, Mac-1, ICAM-1 (each antibody at 20 μg/mL), K1-4, K1-3, K4, or a combination of K4 with K1-3 (each angiostatin form at 1000 nM). (B) PMA-stimulated adhesion of human neutrophils to endothelial cells is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). Cell adhesion is represented as percentage of adherent cell to total added cells. (C) The trans-endothelial migration of human neutrophils in response to 50 ng/mL MCP-1 is shown in the absence (–) or presence of mAb to Mac-1, mAb to β1-integrin (each antibody at 20 μg/mL), K1-4, K1-3, K4, or a combination of K4 with K1-3 (each angiostatin form at 1000 nM). (D) The trans-endothelial migration of human neutrophils in response to 50 ng/mL MCP-1 is shown in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○). Transmigration is presented as percent of control (only MCP-1, in the absence of competitor). Data are mean ± SD (n = 3) of a typical experiment, similar results were obtained in 3 separate experiments. *P < .001, compared with control.
In contrast, neutrophil transendothelial migration was predominantly mediated by Mac-1, while mAb against β1-integrin exhibited no inhibitory activity. Consistent with the previous observation that K4 predominantly interacts with Mac-1 and K1-3 with β1-integrin, monocyte chemoattractant protein-1 (MCP-1)–stimulated neutrophil transmigration through endothelial cells was prevented in the presence of K1-4 or K4, whereas a weak (about 25%-30%) inhibition of neutrophil transmigration was provided only by the highest concentration of K1-3 (1000 nM; Figure 4C-D). Together, angiostatin can block neutrophil adhesion to and transmigration through the endothelium in vitro.
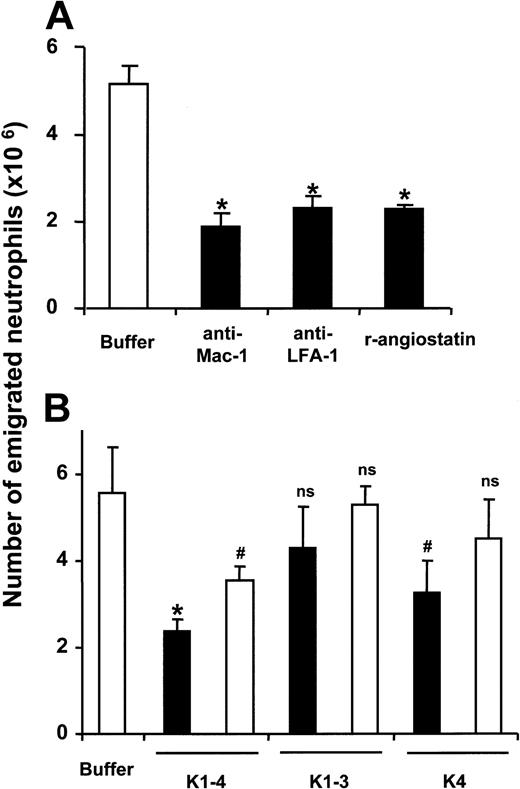
Inhibition of neutrophil recruitment by angiostatin in acute peritonitis in mice
To test whether angiostatin interferes with leukocyte recruitment in vivo, we studied its role in a mouse model of acute inflammation. Peritonitis was induced by thioglycollate injection, and after 4 hours there was the expected increase in the total leukocyte count in the peritoneum, mostly attributable to emigrated neutrophils: The portion of neutrophils among all leukocytes after 4 hours was 50% to 60%.34,35,37 The use of blocking antibodies against LFA-1, Mac-1, or ICAM-1 30 minutes prior to the induction of peritonitis resulted in a 60% to 75% inhibition of neutrophil extravasation into the inflamed peritoneum at 4 hours following thioglycollate injection (Figure 5A) (data with antibody against ICAM-1 not shown). Also, application of recombinant angiostatin (100 μg) resulted in a significant inhibition of neutrophil extravasation (Figure 5A). We then compared the effects of 40 or 100 μg (2 or 5 mg/kg, respectively) of each of K1-4, K1-3, and K4 to block neutrophil recruitment. In mice that were pretreated with these forms of angiostatin, K1-4 provided the maximal inhibition (> 60%) with the higher dose administered (Figure 5B), while also significant inhibition of neutrophil recruitment (about 40%-50%) was observed after pretreatment of mice with the lower dose of K1-4 or the higher dose of isolated K4, whereas K1-3 exhibited no significant inhibition at both doses tested (Figure 5B).
Inhibition of inflammatory reactions in vivo by angiostatin. Following thioglycollate injection into the mouse peritoneum to induce acute inflammation, the number of neutrophils in the peritoneal lavage was analyzed after 4 hours: (A) Prior to thioglycollate administration, separate mice were treated by intraperitoneal injection with PBS-buffer only (▦; –), with a blocking mAb against Mac-1, or with a blocking mAb against LFA-1 or recombinant angiostatin (K1-4) (each 100 μg) as indicated. *P < .001 compared with control (only buffer). (B) Prior to thioglycollate administration, separate mice were treated by intraperitoneal injection with PBS buffer (▦) , with K1-4, K1-3, or K4 (▪ 100 μg; □ 40 μg). *P < .001; #P < .05; ns indicates not significant, compared with control (only buffer). Data are mean ± SD (n = 8-10 mice per treatment).
Inhibition of inflammatory reactions in vivo by angiostatin. Following thioglycollate injection into the mouse peritoneum to induce acute inflammation, the number of neutrophils in the peritoneal lavage was analyzed after 4 hours: (A) Prior to thioglycollate administration, separate mice were treated by intraperitoneal injection with PBS-buffer only (▦; –), with a blocking mAb against Mac-1, or with a blocking mAb against LFA-1 or recombinant angiostatin (K1-4) (each 100 μg) as indicated. *P < .001 compared with control (only buffer). (B) Prior to thioglycollate administration, separate mice were treated by intraperitoneal injection with PBS buffer (▦) , with K1-4, K1-3, or K4 (▪ 100 μg; □ 40 μg). *P < .001; #P < .05; ns indicates not significant, compared with control (only buffer). Data are mean ± SD (n = 8-10 mice per treatment).
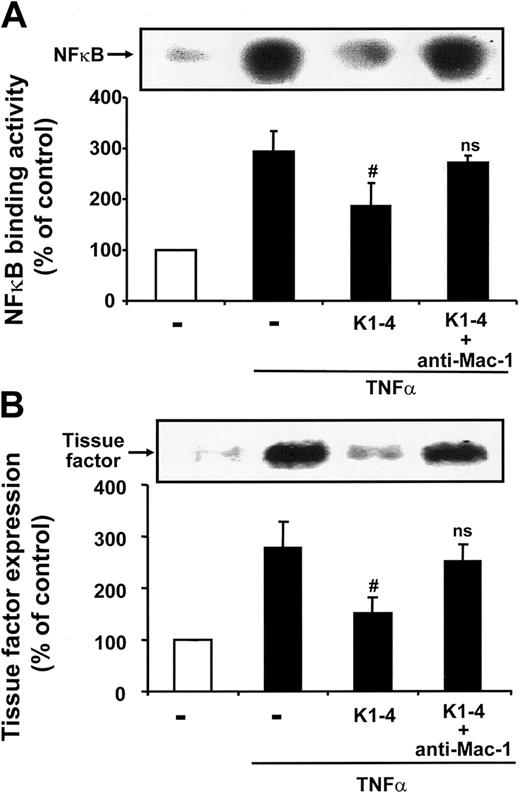
Inhibition of the activity of the transcription factor nuclear factor-κB (NF-κB) in leukocytes by angiostatin
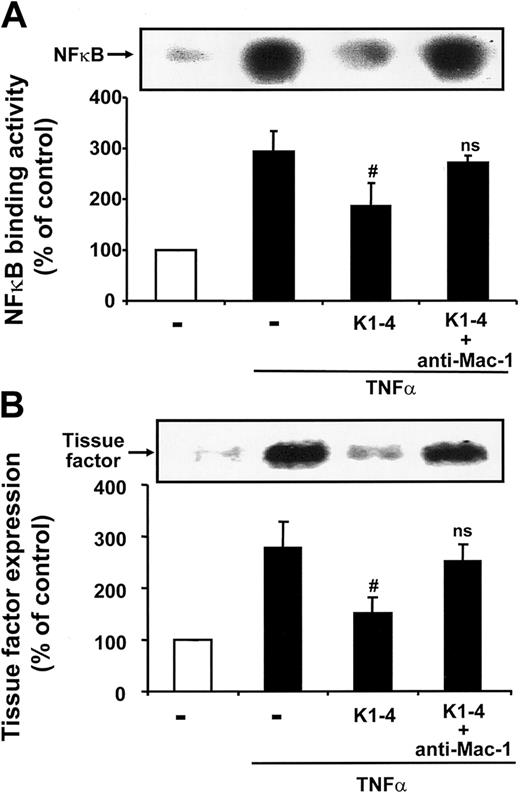
The transcription factor NF-κB has been proposed as a critical molecular bridge between inflammatory, infectious, or other stressful stimuli and gene expression,8-10 and ligation and activation of Mac-1 can result in the activation of this transcription factor.5-7 Based on our findings, angiostatin has an inhibitory function on Mac-1, and we tested the effect of K1-4 on the NFκB binding activity in THP-1 cells as assessed by EMSA. As shown in Figure 6A, K1-4 significantly inhibited tumor necrosis factor-α–induced NFκB activity, whereas in the presence of blocking mAb against Mac-1 this inhibitory activity of K1-4 was largely prevented. Since NFκB is central in the regulation of the expression of inflammatory mediators on leukocytes such as tissue factor, and tissue factor has been previously shown to be up-regulated in monocytes upon Mac-1 ligation,40-42 we studied whether angiostatin could inhibit tumor necrosis factor-α–induced tissue factor up-regulation. Indeed, coincubation of THP-1 cells with K1-4 significantly reduced tissue factor expression in THP-1 cells (Figure 6B). Again, the inhibitory effect of K1-4 on tissue factor expression was prevented in the presence of mAb against Mac-1, which was shown before (Figure 2A) to block the interaction between Mac-1 and K1-4.
Angiostatin reduces activity of NFκB and tissue factor expression. The DNA binding activity of NFκB as assessed by EMSA (A) as well as the expression of tissue factor as assessed by Western blot (B) are shown in the absence (–; open bar) or presence of TNFα (▪) without or together with K1-4 (500 nM) or K1-4 + mAb to Mac-1 (10 μg/mL), as indicated. The inserts demonstrate a typical EMSA for NFκB DNA binding activity (A) and a typical blot with staining for tissue factor (B). Densitometric data are presented as percentage of control (in the absence of TNFα or competitor) and are mean ± SD of 3 separate experiments, each performed in triplicate. #P < .05; ns indicates not significant, compared with TNFα alone.
Angiostatin reduces activity of NFκB and tissue factor expression. The DNA binding activity of NFκB as assessed by EMSA (A) as well as the expression of tissue factor as assessed by Western blot (B) are shown in the absence (–; open bar) or presence of TNFα (▪) without or together with K1-4 (500 nM) or K1-4 + mAb to Mac-1 (10 μg/mL), as indicated. The inserts demonstrate a typical EMSA for NFκB DNA binding activity (A) and a typical blot with staining for tissue factor (B). Densitometric data are presented as percentage of control (in the absence of TNFα or competitor) and are mean ± SD of 3 separate experiments, each performed in triplicate. #P < .05; ns indicates not significant, compared with TNFα alone.
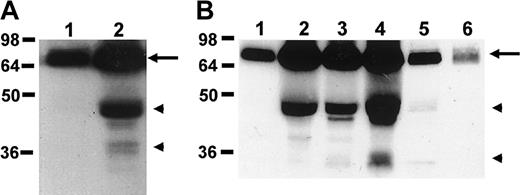
Generation of angiostatin during inflammation
We then went on to investigate whether angiostatin can be generated physiologically during inflammation. We therefore performed Western blot analysis to detect angiostatin forms in wound homogenisates from mice. In the normal mouse cutaneous tissue, only plasminogen but no angiostatin forms were detectable. In contrast, angiostatin forms were detected during wound healing (Figure 7A). In this model, wound healing is complete after 8 to 9 days. In order to study the kinetics of angiostatin generation in wound healing, wounds were extracted at days 0, 1, 3, 7, and 10 after generation of the wounds. Interestingly, plasminogen and angiostatin forms were expressed even at day 1 and day 3 after generation of the wounds (ie, at the initial phase of wound healing). The expression of angiostatin forms peaked at the last phase of wound healing (day 7 after generation of the wounds), and almost disappeared after wound healing was complete at day 10 (Figure 7B). Furthermore, we detected angiostatin forms in the fluid from human wounds (data not shown). Thus, angiostatin can be generated during inflammation and wound healing where it is likely to exert its anti-inflammatory and antiangiogenic effects.
Generation of angiostatin during wound healing. (A) The expression of plasminogen (arrow) and angiostatin forms (arrowheads) in normal cutaneous tissue (lane 1) as well as in a 5-day-old wound (lane 2) is shown. (B). The expression of plasminogen (arrow) and angiostatin forms (arrowheads) in wounds that were extracted at day 0 (lane 1), day 1 (lane 2), day 3 (lane 3), day 7 (lane 4), or day 10 (lane 5) after wound generation. Lane 6 indicates purified plasminogen (0.5 μg).
Generation of angiostatin during wound healing. (A) The expression of plasminogen (arrow) and angiostatin forms (arrowheads) in normal cutaneous tissue (lane 1) as well as in a 5-day-old wound (lane 2) is shown. (B). The expression of plasminogen (arrow) and angiostatin forms (arrowheads) in wounds that were extracted at day 0 (lane 1), day 1 (lane 2), day 3 (lane 3), day 7 (lane 4), or day 10 (lane 5) after wound generation. Lane 6 indicates purified plasminogen (0.5 μg).
Discussion
Leukocyte activation and adhesion to the endothelium and the subsequent transendothelial migration are pivotal steps in the recruitment of cells to the inflamed tissue. This highly coordinated multistep process requires tight regulation of adhesive events including the induction of genes coding for adhesion receptors, their change in avidity, as well as the modification of ligand-binding affinities due to, for example, adhesion receptor clustering.1,4 Uncontrolled activation of leukocytes and/or endothelial cells results in pathologic chronic inflammation during atherosclerosis, rheumatoid arthritis, and other disorders. The present report demonstrates that the antiangiogenic factor angiostatin has an as-yet-uncovered potent anti-inflammatory function by interacting with leukocyte integrins and inhibiting leukocyte recruitment in vitro and in vivo. Our data show that angiostatin serves as novel ligand for the β2-integrin Mac-1, and we have confirmed the previously described interaction of angiostatin with β1-integrins.24 Angiostatin thereby serves as an antiadhesive factor. These findings can also provide novel insights into the mechanisms of action of angiostatin as a potent antiangiogenic substance.
The following features are consistent with a specific interaction particularly of K4 of angiostatin with Mac-1 and K1-3 with α4β1: (1) K1-4 and the isolated K4 specifically inhibited Mac-1–dependent adhesion of neutrophils and myelomonocytic cells to immobilized FBG or ICAM-1, whereas α4β1-dependent adhesion to FN and VCAM-1 was blocked by K1-4 and K1-3. (2) Neutrophils and THP-1 cells directly adhered to K4 and K1-3 in a Mac-1– and α4β1-dependent manner, respectively. Our data are in accordance with the previous report by Tarui et al24 showing an interaction between angiostatin and β1-integrins. Adhesion to K1-4 was predominantly mediated by Mac-1, with α4β1 mediating adhesion to a lesser extent. These data were corroborated when adhesion of K562 cells transfected with different β2-integrins to immobilized different forms of angiostatin was tested; thereby it was further established that K1-4 and K4 interact with Mac-1 but not with LFA-1. (3) In a purified system, K1-4 and K4 directly interfered with the interaction of Mac-1 with its ligands ICAM-1 and FBG. Moreover, a direct binding of K4 or K1-4 to Mac-1 but not to LFA-1 was observed. K1-4 and K4 directly interacted with the major ligand-binding I-domain of Mac-1, however, whether the predominant binding site for angiostatin lies within the I-domain of Mac-1 or other sites of the molecule might be involved, needs further experimentation. (4) Based on their interaction with Mac-1, K1-4 and K4 to a lesser extent inhibited leukocyte recruitment in vivo, as we observed in the model of thioglycollate-induced acute peritonitis, in which acute neutrophil emigration is predominantly mediated by Mac-1 and LFA-1. Together, these data clearly define angiostatin as an antiadhesive and anti-inflammatory factor for leukocytes.
The transcription factor NFκB has been proposed as a critical bridge between oxidant stress and gene expression.8-10 Exposure of cells to inflammatory, infectious, or other stressful stimuli results in rapid phosphorylation and degradation of IκBα and the subsequent release and translocation of NFκB into the nucleus.8-10 The activation of the transcription factor NFκB modulates the expression of several proinflammatory factors, such as interleukin-1b, interleukin-6, or tissue factor.8-10 In addition, NFκB activation can also result upon Mac-1 ligation and activation,5-7 and tissue factor expression has been previously reported to be up-regulated upon β2-integrin ligation.41-43 We demonstrate here that angiostatin inhibits tumor necrosis factor-α–induced NFκB activation as well as tissue factor up-regulation in a Mac-1–dependent manner, since a mAb against Mac-1, which interferes with angiostatin binding, prevented the inhibitory effect of angiostatin. Thus, the anti-inflammatory action of angiostatin extends also to events that are downstream to integrin-dependent adhesion, such as blockade of NFκB activity. Moreover, since tissue factor is a major initiator of hemostasis after vascular injury, inhibition of its expression by angiostatin indicates that angiostatin serves a further yet-unrecognized function as a local regulator of the coagulatory activity in the tissue. Strikingly, tissue factor was recently reported to block the angiostatin-mediated inhibition of endothelial cell proliferation.44 This observation together with the present finding that angiostatin inhibits tissue factor expression may lead to the intriguing conclusion that down-regulation of tissue factor expression by angiostatin provides a feedback mechanism that prolongs the local activity of angiostatin in the tissue. Further studies are needed to address this issue in detail.
Our findings revealed that K4 of angiostatin entails the central region of the polypeptide that serves as integrin ligand with antiadhesive activity. This is in accordance with previous studies demonstrating that K4, which has only marginal antiproliferative activity on endothelial cells, is the most potent fragment in inhibiting endothelial cell migration with an IC50 similar to values presented here. In contrast, kringle 1-3, which is equivalent to angiostatin in inhibiting endothelial cell proliferation, manifests only a modest antimigratory effect.21-23 Further studies are needed to characterize the functional differences of these kringle fragments despite their high conformational uniformity and nearly 50% sequence identity.
The present study extends previous findings that angiostatin specifically interacts with β1-integrins and αvβ3-integrin on endothelial cells in an Arg-Gly-Asp (RGD)–dependent manner,24 thereby interfering with the interaction between plasmin and αvβ3-integrin and inhibiting plasmin-induced endothelial cell migration.45 In accordance with the previous works, we find here that binding of angiostatin to Mac-1 or α4β1-integrin was also blocked by EACA, a lysine analog. The respective lysine-binding sites are present in kringle domains 1, 2, and 4 of angiostatin, and further characterization of integrin-binding sites within the kringle domains is required to determine the contact sites between angiostatin and integrins.
Previous studies on the function of angiostatin in vascular biology were limited to endothelial cells, but are extended to leukocytes as described here. Consequently, the interaction of angiostatin with different integrins provides new insights not only for its mechanistic role in angiogenesis as related to αvβ3-integrin–mediated signaling, but also for its antiadhesive and anti-inflammatory function. Together, on the basis of angiostatin interaction with leukocyte integrins a better understanding about angiogenic events related to (chronic) inflammation will be possible.
Moreover, angiostatin is generated during inflammation, as we detected angiostatin forms during wound healing in humans and mice. Strikingly, substantial amounts of angiostatin were detected during the early phase of wound healing, indicating that angiostatin generation during inflammation is fast. The generation of angiostatin forms peaked at the last phase of wound healing. Thus, angiostatin is likely to be a central player in inflammation and wound healing, and in particular, angiostatin probably regulates the termination of wound healing by modulating the local inflammatory and angiogenic balance of the inflamed/injured tissue. In the inflamed tissue, angiostatin might counteract the angiogenic potential of the inflammatory cells by inhibiting integrin-mediated leukocyte recruitment and activation. For example, monocytes are a source for vascular endothelial growth factor, basic fibroblast growth factor, and metalloproteinases and can modulate angiogenesis and arteriogenesis.46,47 Moreover, neutrophils produce proangiogenic growth factors such as heparin-binding epidermal growth factor, vascular endothelial growth factor, interleukin-8, or tumor necrosis factor-α48,49 and are an abundant source of proteinases such as matrix metalloproteinase 9 (MMP-9), which controls the angiogenic switch during (tumor) neovascularization.50,51 Our present findings gain additional importance in view of the fact that neutrophil-derived elastase can generate angiostatin.26 Thus, hypothesizing that the overall contribution of inflammatory cells to angiogenesis regulation most likely depends upon a fine balance of proangiogenic and antiangiogenic factors, which are secreted by recruited leukocytes depending on the environmental stimuli, the antiadhesive and anti-inflammatory action of angiostatin on leukocytes, presented here, represents a novel negative feedback loop counteracting further recruitment of inflammatory cells and angiogenesis at a site of inflammation or vascular injury.
Angiostatin might thereby be a crucial player linking inflammation and angiogenesis under both physiologic conditions such as wound healing and pathologic situations such as in rheumatoid arthritis, psoriasis, diabetic retinopathy, or atherosclerosis. Chemokines have potent angiogenic activities,27 and a previous report indicated that angiostatin inhibits inflammation-related angiogenesis independent of the inducing agent (ie, CXC chemokine receptor 2 [CXCR2] agonists, formyl-Met-Leu-Phe, or lipopolysaccharide [LPS]), suggesting that it interferes with a downstream pathway common to these stimulants,27 and we here provide evidence for a likely mechanism underlying this phenomenon. Finally, in a very recent study, administration of angiostatin reduced lesion progression and the infiltration of macrophages into atheromas,52 which might be not only an indirect consequence of reduced plaque neovascularization but also due to a direct effect of angiostatin on inflammatory cells according to our present data. In essence, by affecting leukocytes and endothelial cells, angiostatin plays a crucial role at the interface between inflammation and angiogenesis, and our data are meant to stimulate our thinking about novel therapeutic applications for this endogenous molecule.
Prepublished online as Blood First Edition Paper, September 21, 2004; DOI 10.1182/blood-2004-01-0166.
Supported by grants from the Deutsche Forschungsgemeinschaft to T.C. (Ch279/1-1, Ch279/2-1, and SFB405) and to K.T.P. (Pr327/18-1), as well as by a grant from Novartis Foundation for Therapeutical Research to T.C. and K.T.P. T.C. is a recipient of the Stolzenberg-Prize of the Justus-Liebig Universität, Giessen, Germany.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The excellent technical assistance of Yvonne Mueller and Hanno Welker is gratefully acknowledged. The authors also acknowledge the aminoterminal sequencing by Dr D. Linder (Giessen, Germany).

![Figure 1. Angiostatin interferes with leukocyte adhesion. The adhesion of PMA-stimulated THP-1 cells to immobilized vitronectin (A), fibrinogen (B), ICAM-1 (C), fibronectin (D), or VCAM-1 (E) in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○) in the soluble phase is shown. (F) The adhesion of PMA-stimulated human neutrophils to immobilized fibrinogen (▪) or immobilized fibronectin (▦]) is shown in the absence (–) or presence of inhibitory mAb (anti-Mac-1 or anti-β1, respectively, each 20 μg/mL), K1-4, K1-3, K4 (each 1000 nM), or a combination of K1-3 and K4, as indicated. Cell adhesion is represented as absorbance at 590 nm. All data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/105/3/10.1182_blood-2004-01-0166/6/m_zh80030573340001.jpeg?Expires=1768125178&Signature=446fW0WtBK2obihkP1HWlO4kscFIzy39kw49euuOWIav8ikkcD8x2SSgWm-Y4i1FpAQ9bzxdoAdhSW5qwg6AF2d3D7MmHJZucJBIV6g3JQnDh~VI5caFcLasvFWGcycxxqAIHTdwm8St-B~WiFO4BlXGpzOqnmaTiMGJzRhvSNiHpZxiXIDkD4n6utWfxhmUlOwIhzgZsNaKvHo7hWk55eK9wf-E5xMcshJ3cII7GSklke0FzKexRnbVuS6FjM-lQLngTxayQ-0apVenMOoABTuI1~fGNUYGbQLf5i-fxbcxr82SVEBQhN9TLMg96lCvZ-cok6N-p2glRLa1x9UpmQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Figure 1. Angiostatin interferes with leukocyte adhesion. The adhesion of PMA-stimulated THP-1 cells to immobilized vitronectin (A), fibrinogen (B), ICAM-1 (C), fibronectin (D), or VCAM-1 (E) in the absence or presence of increasing concentrations of K1-4 (▴), K1-3 (▪), or K4 (○) in the soluble phase is shown. (F) The adhesion of PMA-stimulated human neutrophils to immobilized fibrinogen (▪) or immobilized fibronectin (▦]) is shown in the absence (–) or presence of inhibitory mAb (anti-Mac-1 or anti-β1, respectively, each 20 μg/mL), K1-4, K1-3, K4 (each 1000 nM), or a combination of K1-3 and K4, as indicated. Cell adhesion is represented as absorbance at 590 nm. All data are mean ± SD (n = 3) of a typical experiment; similar results were obtained in 3 separate experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/105/3/10.1182_blood-2004-01-0166/6/m_zh80030573340001.jpeg?Expires=1768606561&Signature=Xzv6zkXDscbms5Dr5d0p1NLhZb5ppDNmZVdd6ZFdLG311PGBKipcYCmMOC7GIW1rffuKZLIoRLXA~~6Viv83jAOOs6TBh3uk3wSZSJj30~Nata~44TyNYpDG5A4fyV2Mz2gK31k8m~i1OR9zHOHviREbyoJoe55VgmxzDa9yiXYnMPvI1uZHiBdZ5MBpTwH9OMTD32Z3pdeMszYcFcQPidypYSSNZwh1V~NNP-623pzMBcaieu8InTcI3bC7jyFS1Sy8XsMZbXesYgxeATlX0SEvTFdEkq2ZUh6W2Q1K2bIOkeCIC9spjK64f2UIWku3~dEyvT1Y85LDGdahrI8pdA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)