Abstract
Chronic myeloid leukemia (CML) is sustained by a rare population of primitive, quiescent, BCR-ABL+ cells and represents an excellent example of a malignancy in which tumor-initiating cells represent the key to disease eradication. CML is also the first malignancy for which targeted therapy has replaced conventional chemotherapy. Within a vast excess of proliferating progenitor cells that express breakpoint cluster region-abelson (BCR-ABL) and are exquisitely sensitive to the tyrosine kinase inhibitor imatinib mesylate (IM) resides a small population of quiescent leukemic cells that, despite higher levels of BCR-ABL transcripts, exhibits innate insensitivity to IM. These cells remain after IM therapy, even when apparently complete responses are achieved, and they probably explain molecular disease persistence. Although it can be argued that patients may survive for many years with low levels of leukemia still present, it is possible to achieve disease clearance at the molecular level following an allogeneic stem cell transplantation. The emergence of drug resistance with IM monotherapy also argues in favor of complete disease eradication that we believe should remain the ultimate therapeutic goal in CML. New approaches to the elimination of these primitive CML cells may thus be crucial to the development of curative strategies.
Introduction
In chronic myeloid leukemia (CML) the expanded clone is believed to be initiated, in a pluripotent hemopoietic stem cell, by the chance occurrence of a rare mutational event, the translocation of t(9;22), giving rise to the Philadelphia (Ph) chromosome and expression of the oncogenic tyrosine kinase breakpoint cluster region-abelson (BCR-ABL).1 Although the oncoprotein has transforming activity in vitro and in vivo,2,3 the growth advantage conferred upon the Ph+ stem cell is relatively subtle, as evidenced by disease only manifesting some 6 to 7 years following radiation exposure, as calculated from follow-up of atomic bomb survivors in Japan at the end of World War II.4 Despite the introduction, in 1998, of a highly effective tyrosine kinase inhibitor imatinib mesylate (IM),5,6 allogeneic stem cell transplantation following myeloablative conditioning remains the only proven curative treatment for CML.7 The identification of therapies directed specifically and selectively at the leukemic stem cell compartment has remained elusive.
Normal hemopoietic stem cells
Normal hemopoietic stem cells have characteristic, measurable properties. They are rare, representing only 1 in 104 to 105 total bone marrow cells, and their numbers are tightly regulated. Although generally quiescent, they are capable of extensive self-renewal and multilineage differentiation and are transplantable.8 Using flow cytometry stem cells show low forward scatter, indicating small size, express CD34 but do not express lineage or activation markers such as CD38 or HLA-DR.9 The expression of adenosine triphosphate (ATP) binding cassette (ABC) transporter proteins at the cell surface10 confers strong efflux potential for rhodamine, Hoechst, and pyronin Y11 and is responsible for the side profile (SP) phenotype.12
Ph+ BCR-ABL+ stem cell
The earliest suggestion that CML arises in a pluripotent stem cell came in 1951 when it was recognized that mature cells derived from more than a single lineage were involved in the leukemic process.13 These findings were later corroborated by studies using cytogenetic, fluorescence in situ hybridization (FISH), and X-linked markers to prove clonal expansion in multiple lineages.14 More recent work by Gunsilius et al15 may place the level of the BCR-ABL mutation within a hemangioblast.
Leukemia-initiating cell in CML
The ability of CML stem cells to engraft humans was first shown by accident following granulocyte transfusions in the 1960s and 1970s.16,17 These observations were later formally confirmed by gene marking studies in 1994,18 and the evidence was further strengthened by results of clinical autografting programs and experimental work using immunodeficient mice as xenotransplantation models.19,20 These clinical observations confirmed the existence of transplantable leukemia, initiating cells in chronic-phase CML. However, more recent studies in acute myeloid leukemia (AML) and CML suggest a leukemic stem cell hierarchy, with both short- and long-term repopulating cells,21 and convincing evidence that more mature myeloid progenitors can acquire self-renewal capacity and stem cell-like functions, particularly in more advanced phase disease.22,23 It has been difficult to determine an accurate frequency for the leukemia-initiating cell in CML in chronic phase; however, most studies suggest this is lower than in normal hemopoiesis.24 Such frequency estimates have been further complicated by the finding that engraftment or seeding potential of normal stem cells fluctuates according to their cell-cycle status.25 This is relevant because it has been recognized for many years that the proportion of proliferating primitive CML progenitors is much higher than that of their normal counterparts, and these progenitors may, therefore, show compromised engraftment potential.26
Candidate quiescent CML stem cells
Since CML in chronic phase is sustained by pluripotent Ph+ stem cells, our efforts to characterize this population have focused on the identification and isolation of CML cells that are primitive, quiescent and remain cytokine nonresponsive for several days in culture.27,28 In growth factor–supplemented serum-free cultures, using carboxyfluorescein diacetate succinimidyl ester (CFSE) to track cell division, CD34 to track differentiation, and annexin V to track apoptosis, we have determined the frequency of nonproliferating CD34+ CML cells to be approximately 0.5% of the total CD34+ compartment. This frequency is very close to that measured by efflux studies combining Hoechst 33342 and pyronin Y or cells expressing CD34 but negative for CD38. These purification strategies appear to isolate CML cells that remain heterogeneous in terms of quiescence, consisting both of cells transiting G0/G1, which are susceptible to the antiproliferative effects of many drugs, and cells in deep G0, which may be the more clinically relevant subset. Relatively low numbers of such cells are able to engraft nonobese diabetic/severe combined immunodeficient (NOD/SCID) mice and to produce detectable leukemic progeny 6 to 8 weeks later.27 These experiments also confirmed that their quiescence is a temporary phenomenon and reversible in vivo, thus demonstrating the importance of this population as a therapeutic target.28 The existence of such primitive, transiently quiescent CML cells also provides a probable explanation for the failure of intensive (but nonmyeloablative) chemotherapy to eradicate CML and for late relapse many years after transplantation.
Stem cell targeting
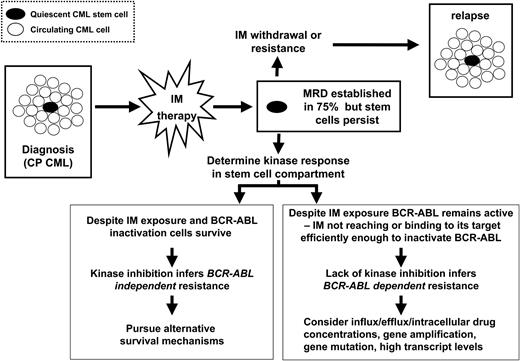
If, as we propose, only this rare subset of CML CD34+ cells sustains the disease in patients, then the challenge is to fully understand their survival mechanisms and then to develop therapies that induce leukemia stem cell–specific apoptosis (Figure 1). Conventional chemotherapies kill proliferating cells, which may be irrelevant for the persistence and propagation of the disease, in a nonselective manner. Current strategies for treatment do not take account of the potentially great difference in drug sensitivity, and, for therapies such as IM, relative expression of the target that have been shown to exist between proliferating and primitive quiescent cell populations.29
Toward targeted cancer stem cell therapy in chronic myeloid leukemia. • indicates quiescent CML stem cell; ○, circulating CML cell. CP indicates chronic phase; MRD indicates minimal residual disease.
Toward targeted cancer stem cell therapy in chronic myeloid leukemia. • indicates quiescent CML stem cell; ○, circulating CML cell. CP indicates chronic phase; MRD indicates minimal residual disease.
Primitive quiescent CML cells are insensitive to IM in vitro
Our previous findings and those of others have demonstrated that primitive populations of progenitor cells in patients with CML are sensitive to the antiproliferative effects of IM but, unlike more mature proliferating Ph+ cells, do not readily undergo apoptosis.30 High concentrations of IM, significantly greater than achievable in vivo, fail to eliminate the most quiescent cells even after 6 days of continuous drug exposure. Recent data from our group also confirm the unique resistance of these cells to several rationally selected drug combinations, including 1-β-d-arabinofuranosylcytosine (Ara-C), 2-(4-morpholinyl)-8-phenyl-4H-1-benzopyran-4-one (LY294002), and 17-(Allylamino)-17-demethoxygeldanamycin (17AAG) with IM.31 The isolated cells include a subset which accumulates in G0/G1 in the presence of IM or other antiproliferative agents but can be eradicated by carefully scheduled pulsed therapies. However, a further subset appears deeply quiescent and inherently resistant to IM. These latter cells likely share biologic properties with their normal counterparts, perhaps more related to their stem cell phenotype than the transformation process per se, making them poor targets for IM therapy.
Molecular disease persistence in vivo
Currently, therapeutic endpoints, such as complete hematologic response, complete cytogenetic response (CCR), and 3-log depletion of BCR-ABL transcripts,29 rely on rapid reduction in overall, rather than stem cell–specific, leukemic burden. Despite short follow-up with IM relative to the natural history of CML, these surrogate markers of response have so far proven predictive for progression-free survival. However, clinicians should be cautious before broadening the correlation between CCR achieved with interferon (IFN) therapy and survival to IM therapy. There is mounting evidence that CML stem cells are not eliminated by IM in vivo, with patients in CCR having easily detectable Ph+ CD34+ cells, colony-forming cells (CFCs) and long-term culture-initiating cells (LTC-ICs).32,33 Furthermore, only 4% of patients in the IRIS (International Randomized IFN versus STI571) trial achieved sequential negative reverse transcription–polymerase chain reaction (RT-PCR) tests by 30 months on therapy.29 These results are indeed reminiscent of IFN studies in which patients in CCR and even molecular remission were shown to have residual disease within the CFC compartment.34 However, the slow but durable responses to IFN backed by laboratory studies35 suggested the primary activity of IFN may be at the stem cell level. However, the very rapid early IM responses and the suggestion that patients who have achieved excellent responses may now be showing evidence of disease progression36 imply that IM may target a different and more mature CML cell population. Furthermore, mutations leading to drug resistance are a prominent problem with IM therapy, again arguing in favor of disease eradication if this can be achieved.37,38
This persistent disease has raised concern and prompted further interest in novel strategies to achieve disease eradication without resorting to stem cell transplantation. Current knowledge suggests that drug resistance of primitive CML cells is likely to be multifactorial. Although mutations in the kinase domain of BCR-ABL have been assumed to be of greater clinical relevance in patients with advanced disease, some of these have been detected in new cases of CML who achieve CCR with IM, suggesting that eventual selective outgrowth of preexisting clones could become commonplace.39-41 Our own calculations suggest that the average patient harbors 5 × 107 Ph+ quiescent CD34+ cells. Given the demonstrated insensitivity of these cells to IM in vitro, it is plausible that they would become the dominant persisting population of CML cells remaining after IM treatment. Whether quiescent CML cells with wild-type BCR-ABL sequence coexist with clones expressing BCR-ABL kinase mutations and both contribute to IM resistance in most chronic phase patients is currently unknown.
Target expression and inhibition by IM
Our previous animal studies demonstrated that primitive quiescent CML cells engraft NOD/SCID mice and produce BCR-ABL+ progeny in vivo.27 Similarly, single-cell RT-PCR analyses confirmed that quiescent CML cells express BCR-ABL mRNA with more recent quantitative analyses, suggesting higher transcript levels in the most primitive CML cells.42 Fluorescence in situ hybridization (FISH) studies show that only a single copy of BCR-ABL is found in these rare primitive cells and thus eliminate gene amplification as an explanation for their resistance (unpublished data). What is not yet certain is whether their resistance is BCR-ABL dependent, meaning that despite exposure to IM BCR-ABL remains active with phosphorylation of downstream proteins such as Crk-like protein (CRKL). Bhatia's group (Chu et al41 ) has recently demonstrated that, upon exposure to IM for 16 hours, total CD34+ cells from patients with CML show almost total dephosphorylation of CRKL by Western blotting. However, as the quiescent fraction represents less than 1% of the total CD34 population, any lack of response by these cells would be masked in such experiments. Our own preliminary experiments suggest that the picture is very different for either total CD34+ cells cultured with IM for 72 hours, at which time point only resistant cells remain, or for more primitive CD34+ CD38– cells at either 16 or 72 hours. Under these experimental conditions CRKL remains fully phosphorylated, suggesting that in primitive progenitors IM is not reaching or binding to its target efficiently enough to inactivate BCR-ABL (Elrick et al61 ). These results require further confirmation and have prompted additional experiments to investigate intracellular drug concentrations and to search for mutations of the kinase domain in these primitive cells.41 Such experiments will prove challenging, given the rarity of the quiescent population.
Novel investigative and therapeutic approaches
To address the limitations of IM monotherapy many groups have investigated drug combinations with IM. In addition, since IM binding to the BCR-ABL kinase domain is known to be conformation sensitive,43 the newer generation dual SRC/BCR-ABL kinase inhibitors are of great interest, since they appear to be, not only more potent than IM, but also able to bind to conformations of BCR-ABL that confer IM resistance.44,45 However, as before, most recent work with these agents has been carried out in cell lines with limited studies on primary CML cell populations. It is timely, therefore, to highlight the importance of testing novel agents on the subset of primary leukemic cells that are most likely to determine long-term outcome in vivo. Furthermore, most current screening methods for novel agents measure success by overall tumor cell kill, leading to drastic but misleading effects, whereas a drug that selectively targets primitive cells would be overlooked or interpreted as a failure and abandoned prematurely. In the future genomic and proteomic approaches should focus on highly enriched normal versus leukemic populations, using RNA amplification to optimize results for small cell numbers, in an effort to identify novel diagnostic and therapeutic targets.
Future approaches in CML will require confirmation of target expression in the immature cells and recognition that acquired secondary mutations may lead to BCR-ABL–independent resistance46 and may enable more mature progenitor cells to self-renew and drive blast crisis. However, in chronic-phase disease our biggest challenge may be to overcome the inherent properties of stem cells that make the target inaccessible or no longer relevant. Investigators should focus on disease pathogenesis and biology rather than just the specific target, and it must be understood that standard clinical parameters may overestimate (eg, IM therapy) or underestimate (eg, IFN therapy) effects on the rare stem cell population in CML. Until meaningful endpoints are decided for IM, survival should remain the primary proof of therapeutic efficacy.
There are definite grounds for optimism regarding CML therapy. In our drug combination studies, only IM with lonafarnib produced a decrease in quiescent, primitive CML cells in vitro, suggesting that this combination may be more effective than IM monotherapy.31 Synergy between IM and lonafarnib has been shown previously on IM-sensitive and -resistant CML cell lines47 and may reflect lonafarnib's dual activity as a modulator of subcellular localization of Ras48 and an inhibitor of ABC transporter molecules.49 These efflux proteins may be particularly important for primitive cell populations in which expression levels would be anticipated to be high. Very recently it has been confirmed that IM is a substrate for ABCG2 (ABC transporter G2), an active ABC transporter expressed on normal and leukemia stem cells,50 and IM has also been shown to undergo active transport into CML cells via the drug transporter organic cation transporter type 1 (OCT1).51 Expression levels for ABCG2 and OCT1 on primitive CML cells have yet to be determined. We have also shown that extending the period of drug exposure in vitro is no more effective, in terms of eliminating primitive quiescent cells, than a short exposure followed by a drug-free interval, supporting the concept of pulsed regimens to effectively target primitive leukemic cells that require an exposure break to allow their entry into cycle and reinstatement of a drug-sensitive state. Future approaches will focus on ways to break quiescence of CML cells and/or to antagonize the strong antiproliferative effects of IM and many other novel agents being investigated for CML therapy.
Implications for other leukemias and solid cancers
Over the past 5 to 10 years there has been a shift in focus toward identifying disease-specific intracellular or extracellular markers and using these as targets for novel therapy. This approach has been most successful in the field of hematologic malignancy, leading to development of rituximab, gemtuzumab ozogamicin (Mylotarg), alemtuzumab (Campath), IM, all-trans retinoic acid (ATRA), Flt-3 inhibitors, and others. These agents produce rapid and spectacular effects in terms of depletion of tumor cells, offering good debulking and apparent regression of disease. However, our experience with IM suggests that these responses will be neither complete nor durable, and minimal residual disease will remain in most instances.
In parallel to the work in CML, Dick and others have identified a common phenotype for the leukemia-initiating cell in AML52-54 and further studies are in progress for acute lymphoblastic leukemia (ALL).55 In all these cases (CML, AML, ALL), although the leukemia-initiating cell phenotype is very similar to that of normal hemopoietic stem cells, subtle differences exist that must be elucidated and exploited to gain selective therapeutic advantage in terms of induction of leukemia stem cell–specific apoptosis. This has already been achieved to some degree for AML in elegant studies by Jordan's group (Guzman et al56 ). By combining cell stress, induced by idarubicin, with inhibition of a survival signal (nuclear factor-κB [NF-kB]and downstream targets), by a proteasome inhibitor, robust leukemia stem cell–specific apoptosis was observed in AML and confirmed in an in vivo mouse model. Further models combining hyperthermia and phosphatidylinositol 3 (PI3) kinase inhibition, differentiation therapies, novel leukemia stem cell–specific targets, and modulation of self-renewal are explored in the recent review by Jordan and Guzman.57 In the solid-tumor field, it is becoming increasingly recognized that cancer is a stem cell disorder; cancer stem cells have now been identified in prostate, breast, and brain tumors.58-60 The same messages hold true for all these diseases. We need to identify and isolate cancer stem cells for each of these disorders, to develop sophisticated cancer stem cell experimental systems, and stem cell–screening methodology, to identify stem cell–specific targets and apoptotic stimuli. In this manner we should be able to optimize stem cell–directed therapies and hope to achieve eradication of disease.
Prepublished online as Blood First Edition Paper, November 4, 2004; DOI 10.1182/blood-2004-08-3373.