Abstract
Background: IM was proven to be superior to IFN+Ara-C for newly diagnosed pts with CML-CP (O’Brien et al, NEJM 2003). At 42-months of follow-up, 75% of the 553 pts randomized to IM remain on treatment. Of the 553 pts randomized to IFN+Ara-C only 4% are still on IFN+Ara-C. This update analysis is focused on IM pts.
Methods: Evaluation included complete hematologic response (CHR), major/complete cytogenetic response (MCyR/CCyR) - defined as 0-35% Ph+ and 0% Ph+ metaphases respectively, major molecular response (MMR) - defined as ≥3 log reduction of bcr-abl transcripts from the standardized baseline, time to progression - defined as loss of CHR/MCyR or evolution to accelerated phase/blast crisis (AP/BC) or death due to any cause, time to AP/BC - defined as evolution to AP/BC or death due to CML, and overall survival.
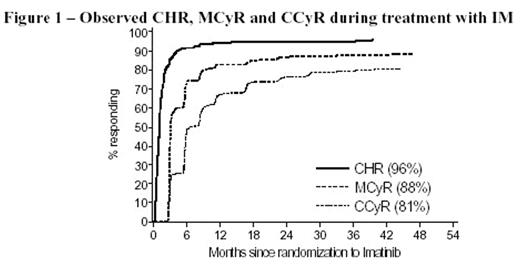
Results: With an average duration of 38 months of IM treatment, the best observed rates of CHR, MCyR and CCyR are 96%, 88% and 81%, respectively. Although the majority of MCyRs were achieved within the first 3 to 9 months, some pts achieved a MCyR and some even a CCyR after more than one year of treatment (Figure 1). The estimated MMR rate at 12 months is 40%.
Observed CHR, MCyR and CCyR during treatment with IM
The estimated progression-free rate at 42 months is 84%; additionally 94% are estimated free of progression to AP/BC (97% of the pts with CCyR and 73% of the pts without CCyR during study, p<0.001). The risk of relapse remains low with no apparent increased risk over time. The yearly hazard for progression to AP/BC is about 2% in each of the 4 years.
The overall estimated survival at 42 months is 91% (considering all deaths). The estimated survival was lowest in pts with high risk Sokal score (84%) as compared to 91% in the intermediate risk pts and 94% in the low risk pts (p<0.001). Similarly, the best observed CCyR in the high, intermediate, and low risk groups were 69%, 80% and 88% respectively (p=0.002). In the subset of pts with CCyR the estimated survival at 42 months was 92%, 93% and 97% in the high to low risk groups (p=0.30), indicating that once pts achieve a CCyR, their survival is not significantly different between the Sokal risk groups.
Of the 509 pts who were still on treatment at 12 months and had achieved a MCyR by then (n=436), the rate without progression to AP/BC at 42 months was 97% whereas it was only 83% for the 73 pts who did not achieve a MCyR at 12 months (p<0.001). The estimated survival rates at 42 months were 95% and 83% in these two response groups, respectively (p<0.001).
Furthermore, for pts who had achieved a MMR at 12 months, the probability of remaining free from progression to AP/BC was 100% at 42 months compared to 95% for pts in CCyR but not in MMR, and 91% for pts not in CCyR at 12 months (p=0.0013). Conclusions: The follow-up confirms the beneficial effect of cytogenetic and molecular responses on long-term outcomes with IM. These results will be further updated using data cut-off of 31-July 2005 to reflect additional 12-months of data (i.e., 54-month follow-up).
Author notes
Corresponding author