Abstract
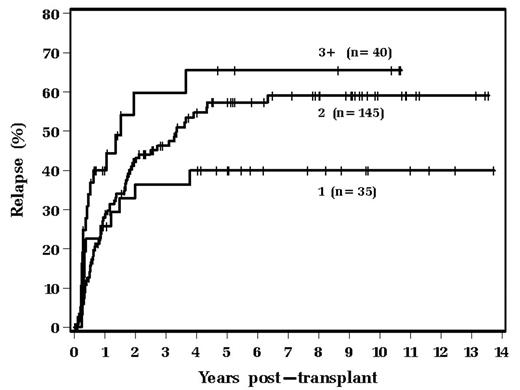
Long-term results of conventional therapy of Hodgkin’s disease (HD) has demonstrated the importance of long-term and ongoing follow-up given the potential for later complications after curative therapy. While many transplant series report follow-up of several years after ABMT, few report a 15-year experience from a single institution. This report examines the outcomes of 220 patients receiving high-dose chemotherapy and autologous stem cell transplant (ABMT) at The Cleveland Clinic Foundation from January 1990 through June 2005. Median age was 33 years (range, 14–70 years); median time from diagnosis to transplant was 19 months; 47% received prior radiation therapy; 82% had nodular sclerosis histologic subtype; number of courses of prior chemotherapy were: 1 (16%), 2 (66%), 3 (14%), 4 or more (4%). All patients received salvage therapy prior to transplant: 29% were in a complete remission (CR), 55% in a partial remission (PR), and 16% refractory. All patients received a chemotherapy-only preparative regimen, most commonly Bu/Cy/VP (73%), followed by CBV (17%). 78% received peripheral stem cells alone; 22% received either autologous bone marrow or a combination of bone marrow plus peripheral stem cells. At the present time 60% of patients are alive. Of the 88 patients who died, the most common cause of death is relapse (69% of deaths). Secondary malignancy occurred in 11 patients (5%); 9 of these cases were secondary AML/MDS and 5 of these patients with secondary malignancies have died. 44% of the entire cohort has relapsed, at a median of 9 months post-transplant (range, 1.4–76 months). 10-year overall survival is 47%. A multivariable analysis showed that the two significant variables that correlated with post-BMT relapse were the number of prior chemotherapies (p = 0.011), and patients treated in remission vs. those not in remission (p = 0.002). Of patients receiving 2 or more prior courses of chemotherapy, 60% have relapsed 8 years post-transplant, compared to 40% of those receiving one course of prior chemotherapy. The risk of relapse by the number of prior chemotherapy courses is shown graphically below:
In conclusion, this very large series of ABMT for recurrent HD with long-term follow-up demonstrates the importance of timely autografting in relapsed HD patients. The optimal time to proceed with ABMT is after failing one, and only one, course of chemotherapy. Delaying transplant for unrealistic long-term salvage with other courses of traditional chemotherapy will negatively affect the outcome of subsequent ABMT.
Author notes
Corresponding author